World Journal of Emergency Medicine ›› 2025, Vol. 16 ›› Issue (3): 231-238.doi: 10.5847/wjem.j.1920-8642.2025.055
• Original Article • Previous Articles Next Articles
Jie Chen1,2, Zhonghao Li3,2, Xiaoyu Liu1, Tianpeng Hu2, Nan Gao1, Weijian Zhang1, Guoqiang Zhang2( )
)
Received:2024-11-20
Accepted:2025-03-25
Online:2025-05-19
Published:2025-05-01
Contact:
Guoqiang Zhang, Email: Jie Chen, Zhonghao Li, Xiaoyu Liu, Tianpeng Hu, Nan Gao, Weijian Zhang, Guoqiang Zhang. Potential common key genes associated with myocardial dysfunction and brain injury following cardiac arrest resuscitation in a rat model[J]. World Journal of Emergency Medicine, 2025, 16(3): 231-238.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2025.055

Figure 1.
CA/CPR-induced transcriptional alterations in the hippocampus and LV. A: heatmap showing up-regulated or down-regulated DEGs in hippocampal tissue induced by CA/CPR; B: the top ten hub genes of the PPI network diagram of CA/CPR-induced 217 DEG alterations in the hippocampus; C: heatmap showing up-regulated or down-regulated DEGs in the LV induced by CA/CPR; D: the top ten hub genes of the PPI network diagram of CA/CPR-induced 80 DEG alterations in the LV. The more reddish and darker the color of the gene is, the higher the PPI network score. n=3. Con-1, Con-2, Con-3: rat 1, 2, 3 in the control group; Mod-1, Mod-2, Mod-3: rat 1, 2, 3 in the CA/CPR group; TPM: transcripts per million; CRP: cardiopulmonary resuscitation; CA: cardiac arrest; LV: left ventricular; DEG: differentially expressed genes; PPI: protein-protein interaction.
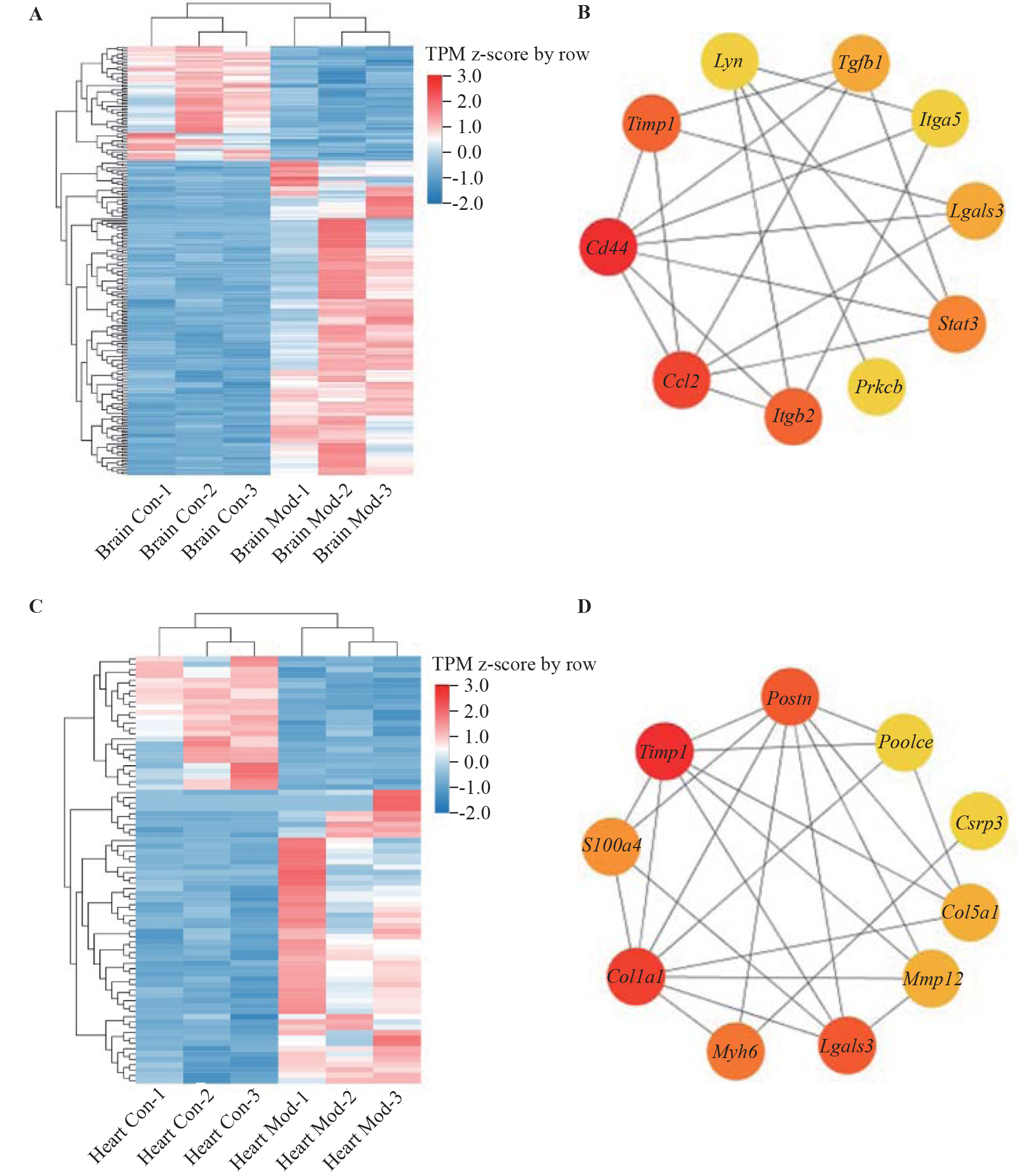
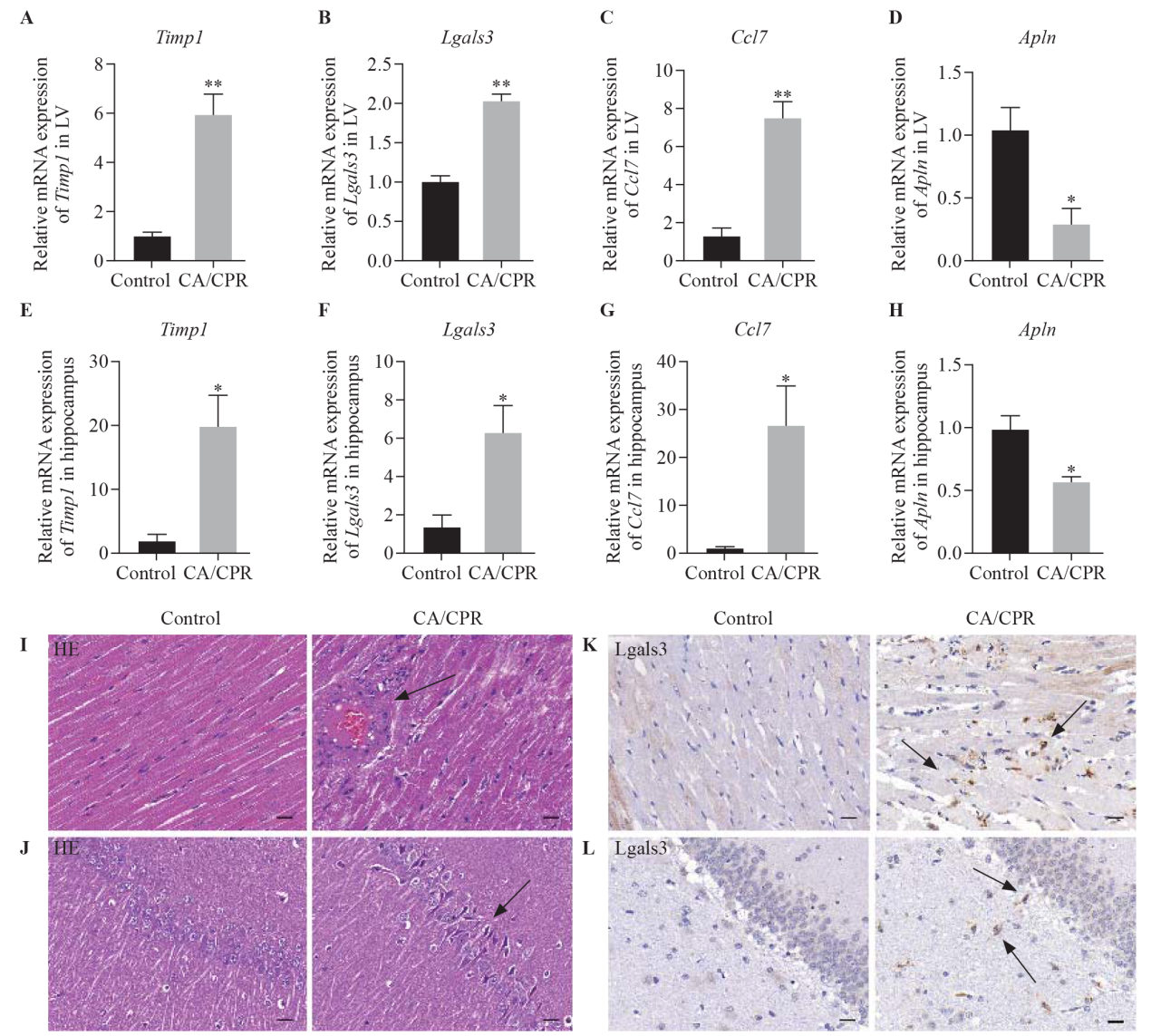
Figure 3.
CA/CPR-induced myocardial and brain injury in rats and expression validation of common genes in the LV and hippocampus. A-H: relative mRNA expression of Timp1, Lgals3, Ccl7 and Apln in LV and hippocampal tissues; values are presented as the means±SEMs. I and J: representative morphological alterations in cardiomyocytes in the LV and hippocampal regions determined by HE staining; K, L: representative immunohistochemical images of Lgals3 expression in the LV and hippocampal regions; scale bar=20 μm; LV: left ventricle; CA/CPR: cardiac arrest/cardiopulmonary resuscitation; compared with the control group, *P<0.05, **P<0.01.
| 1 | Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020; 141(9): e139-e596. |
| 2 |
Kang C, You Y, Park JS, Park BK, Lee JK, Lee BK. Utilization of biomarkers for the prognostic prediction of cardiac arrest survivors using a multi-modal approach. World J Emerg Med. 2024; 15(2):131-4.
doi: 10.5847/wjem.j.1920-8642.2024.029 pmid: 38476538 |
| 3 |
Punniyakotty B, Ong XL, Ahmad M, Kirresh A. Improving mortality in pediatric out-of-hospital cardiac arrest events requires a multifactorial approach. JACC Asia. 2023; 3(1):166.
doi: 10.1016/j.jacasi.2022.11.011 pmid: 36873764 |
| 4 | Cunningham CA, Coppler PJ, Skolnik AB. The immunology of the post-cardiac arrest syndrome. Resuscitation. 2022; 179: 116-23. |
| 5 |
Sandroni C, Cronberg T, Sekhon M. Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis. Intensive Care Med. 2021; 47(12): 1393-414.
doi: 10.1007/s00134-021-06548-2 pmid: 34705079 |
| 6 | Jentzer JC, Chonde MD, Dezfulian C. Myocardial dysfunction and shock after cardiac arrest. Biomed Res Int. 2015; 2015: 314796. |
| 7 |
Kohlhauer M, Panel M, Roches MVD, Faucher E, Abi Zeid Daou Y, Boissady E, et al. Brain and myocardial mitochondria follow different patterns of dysfunction after cardiac arrest. Shock. 2021; 56(5): 857-64.
doi: 10.1097/SHK.0000000000001793 pmid: 33978607 |
| 8 | Choudhary RC, Kuschner CE, Kazmi J, McDevitt L, Espin BB, Essaihi M, et al. The role of phospholipid alterations in mitochondrial and brain dysfunction after cardiac arrest. Int J Mol Sci. 2024; 25(9): 4645. |
| 9 | Benghanem S, Sharshar T, Gavaret M, Dumas F, Diehl JL, Brechot N, et al. Heart rate variability for neuro-prognostication after CA: insight from the Parisian registry. Resuscitation. 2024; 202: 110294. |
| 10 | Endoh H, Kamimura N, Honda H, Nitta M. Early prognostication of neurological outcome by heart rate variability in adult patients with out-of-hospital sudden cardiac arrest. Crit Care. 2019; 23(1): 323. |
| 11 | Lamoureux L, Radhakrishnan J, Gazmuri RJ. A rat model of ventricular fibrillation and resuscitation by conventional closed-chest technique. J Vis Exp. 2015(98): 52413. |
| 12 |
Li RQ, Li YR, Kristiansen K, Wang J. SOAP: short oligonucleotide alignment program. Bioinformatics. 2008; 24(5): 713-4.
doi: 10.1093/bioinformatics/btn025 pmid: 18227114 |
| 13 |
Langmead B, Salzberg SL. Fast gapped-read alignment with bowtie 2. Nat Methods. 2012; 9(4): 357-9.
doi: 10.1038/nmeth.1923 pmid: 22388286 |
| 14 | Li B, Dewey CN. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinformatics. 2011; 12: 323. |
| 15 | Ye H, Ye L, Kang H, Zhang D, Tao L, Tang K, et al. HIT: linking herbal active ingredients to targets. Nucleic Acids Res. 2011; 39(database issue): D1055-D1059. |
| 16 | Szklarczyk D, Kirsch R, Koutrouli M, Nastou K, Mehryary F, Hachilif R, et al. The STRING database in 2023:protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 2023; 51(D1): D638-D646. |
| 17 |
Pitkin SL, Maguire JJ, Bonner TI, Davenport AP. International Union of Basic and Clinical Pharmacology. LXXIV. Apelin receptor nomenclature, distribution, pharmacology, and function. Pharmacol Rev. 2010; 62(3): 331-42.
doi: 10.1124/pr.110.002949 pmid: 20605969 |
| 18 |
Pisarenko OI, Lankin VZ, Konovalova GG, Serebryakova LI, Shulzhenko VS, Timoshin AA, et al. Apelin-12 and its structural analog enhance antioxidant defense in experimental myocardial ischemia and reperfusion. Mol Cell Biochem. 2014; 391(1-2): 241-50.
doi: 10.1007/s11010-014-2008-4 pmid: 24599747 |
| 19 |
Khaksari M, Aboutaleb N, Nasirinezhad F, Vakili A, Madjd Z. Apelin-13 protects the brain against ischemic reperfusion injury and cerebral edema in a transient model of focal cerebral ischemia. J Mol Neurosci. 2012; 48(1): 201-8.
doi: 10.1007/s12031-012-9808-3 pmid: 22638858 |
| 20 |
Dawkins E, Small DH. Insights into the physiological function of the amyloid-β precursor protein: beyond Alzheimer’s disease. J Neurochem. 2014; 129(5): 756-69.
doi: 10.1111/jnc.12675 pmid: 24517464 |
| 21 |
Ishikawa J, Harada K. Heart and brain failure: the vicious cycle of the heart-brain interaction. JACC Asia. 2023; 3(1):120-1.
doi: 10.1016/j.jacasi.2022.10.009 pmid: 36873757 |
| 22 |
Greco S, Zaccagnini G, Fuschi P, Voellenkle C, Carrara M, Sadeghi I, et al. Increased BACE1-AS long noncoding RNA and β-amyloid levels in heart failure. Cardiovasc Res. 2017; 113(5): 453-63.
doi: 10.1093/cvr/cvx013 pmid: 28158647 |
| 23 |
Stamatelopoulos K, Sibbing D, Rallidis LS, Georgiopoulos G, Stakos D, Braun S, et al. Amyloid-beta (1-40) and the risk of death from cardiovascular causes in patients with coronary heart disease. J Am Coll Cardiol. 2015; 65(9): 904-16.
doi: 10.1016/j.jacc.2014.12.035 pmid: 25744007 |
| 24 |
Janata A, Magnet IAM, Uray T, Stezoski JP, Janesko-Feldman K, Tisherman SA, et al. Regional TNFα mapping in the brain reveals the striatum as a neuroinflammatory target after ventricular fibrillation cardiac arrest in rats. Resuscitation. 2014; 85(5): 694-701.
doi: 10.1016/j.resuscitation.2014.01.033 pmid: 24530249 |
| 25 |
Bonetti NR, Diaz-Cañestro C, Liberale L, Crucet M, Akhmedov A, Merlini M, et al. Tumour necrosis factor-α inhibition improves stroke outcome in a mouse model of rheumatoid arthritis. Sci Rep. 2019; 9(1): 2173.
doi: 10.1038/s41598-019-38670-z pmid: 30778120 |
| 26 |
Van Damme J, Proost P, Lenaerts JP, Opdenakker G. Structural and functional identification of two human, tumor-derived monocyte chemotactic proteins (MCP-2 and MCP-3) belonging to the chemokine family. J Exp Med. 1992; 176(1): 59-65.
doi: 10.1084/jem.176.1.59 pmid: 1613466 |
| 27 |
Sun YY, Pinto C, Camus S, Duval V, Alayrac P, Zlatanova I, et al. Splenic marginal zone B lymphocytes regulate cardiac remodeling after acute myocardial infarction in mice. J Am Coll Cardiol. 2022; 79(7): 632-47.
doi: 10.1016/j.jacc.2021.11.051 pmid: 35177192 |
| 28 |
Ries C. Cytokine functions of TIMP-1. Cell Mol Life Sci. 2014; 71(4): 659-72.
doi: 10.1007/s00018-013-1457-3 pmid: 23982756 |
| 29 | Barton PJR, Birks EJ, Felkin LE, Cullen ME, Koban MU, Yacoub MH. Increased expression of extracellular matrix regulators TIMP1 and MMP1 in deteriorating heart failure. J Heart Lung Transplant. 2003; 22(7): 738-44. |
| 30 |
Angus McQuibban G, Gong JH, Wong JP, Wallace JL, Clark-Lewis I, Overall CM. Matrix metalloproteinase processing of monocyte chemoattractant proteins generates CC chemokine receptor antagonists with anti-inflammatory properties in vivo. Blood. 2002; 100(4): 1160-7.
pmid: 12149192 |
| 31 |
Venkatraman A, Hardas S, Patel N, Singh Bajaj N, Arora G, Arora P. Galectin-3: an emerging biomarker in stroke and cerebrovascular diseases. Eur J Neurol. 2018; 25(2): 238-46.
doi: 10.1111/ene.13496 pmid: 29053903 |
| 32 |
Shirakawa K, Endo J, Kataoka M, Katsumata Y, Yoshida N, Yamamoto T, et al. IL (interleukin)-10-STAT3-galectin-3 axis is essential for osteopontin-producing reparative macrophage polarization after myocardial infarction. Circulation. 2018; 138(18): 2021-35.
doi: 10.1161/CIRCULATIONAHA.118.035047 pmid: 29967195 |
| [1] | Rui Shao, Chenchen Hang, Xingsheng Wang, Luying Zhang, Fei Shao, Ziren Tang. The “SOOTEST-ICU” bundle for optimizing cerebral hypoxia and reperfusion to minimize brain injury after resuscitation from cardiac arrest [J]. World Journal of Emergency Medicine, 2025, 16(3): 206-211. |
| [2] | George Briassoulis, Mina Argyrakopoulou, Dafni Korela, Sotiria Labrinaki, Artemis Nikiforou, Antonios Papoutsakis, Panagiotis Briassoulis, Marianna Miliaraki, George Notas, Stavroula Ilia. Lifelong training, retraining, reskilling, upskilling and knowledge gaps in emergency medicine: a cross-sectional survey study [J]. World Journal of Emergency Medicine, 2025, 16(3): 212-219. |
| [3] | Tingting Xu, Shaokun Wang, Liqiang Zhao, Jiawen Wang, Jihong Xing. A two-sample Mendelian randomization study on the relationship of body weight, body mass index, and waist circumference with cardiac arrest [J]. World Journal of Emergency Medicine, 2025, 16(2): 129-135. |
| [4] | Wachira Wongtanasarasin, Daniel K. Nishijima, Wanrudee Isaranuwatchai, Jeffrey S. Hoch. Real-world cost-effectiveness of targeted temperature management in out-of-hospital cardiac arrest survivors: results from an academic medical center [J]. World Journal of Emergency Medicine, 2025, 16(1): 28-34. |
| [5] | Subi Abudurexiti, Shihai Xu, Zhangping Sun, Yi Jiang, Ping Gong. Glucose metabolic reprogramming-related parameters for the prediction of 28-day neurological prognosis and all-cause mortality in patients after cardiac arrest: a prospective single-center observational study [J]. World Journal of Emergency Medicine, 2024, 15(3): 197-203. |
| [6] | Jing Yang, Hanqi Tang, Shihuan Shao, Feng Xu, Yangyang Fu, Shengyong Xu, Chen Li, Yan Li, Yang Liu, Joseph Harold Walline, Huadong Zhu, Yuguo Chen, Xuezhong Yu, Jun Xu. A novel predictor of unsustained return of spontaneous circulation in cardiac arrest patients through a combination of capnography and pulse oximetry: a multicenter observational study [J]. World Journal of Emergency Medicine, 2024, 15(1): 16-22. |
| [7] | Rashed Alremeithi, Quincy K. Tran, Megan T. Quintana, Soroush Shahamatdar, Ali Pourmand. Approach to traumatic cardiac arrest in the emergency department: a narrative literature review for emergency providers [J]. World Journal of Emergency Medicine, 2024, 15(1): 3-9. |
| [8] | Shuang Xu, Lang Guo, Weijing Shao, Licai Liang, Tingting Shu, Yuhan Zhang, He Huang, Guangqi Guo, Qing Zhang, Peng Sun. Vagus nerve stimulation protects against cerebral injury after cardiopulmonary resuscitation by inhibiting inflammation through the TLR4/NF-κB and α7nAChR/JAK2 signaling pathways [J]. World Journal of Emergency Medicine, 2023, 14(6): 462-470. |
| [9] | Gannan Wang, Zhe Wang, Yi Zhu, Zhongman Zhang, Wei Li, Xufeng Chen, Yong Mei. The neuro-prognostic value of the ion shift index in cardiac arrest patients following extracorporeal cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2023, 14(5): 354-359. |
| [10] | Guang-qi Guo, Yan-nan Ma, Shuang Xu, Hong-rong Zhang, Peng Sun. Effect of post-rewarming fever after targeted temperature management in cardiac arrest patients: a systematic review and meta-analysis [J]. World Journal of Emergency Medicine, 2023, 14(3): 217-223. |
| [11] | Gan-nan Wang, Zhong-man Zhang, Wen Chen, Xiao-quan Xu, Jin-song Zhang. Timing of brain computed tomography for predicting neurological prognosis in comatose cardiac arrest survivors: a retrospective observational study [J]. World Journal of Emergency Medicine, 2022, 13(5): 349-354. |
| [12] | Shi-jiao Yan, Mei Chen, Jing Wen, Wen-ning Fu, Xing-yue Song, Huan-jun Chen, Ri-xing Wang, Mei-ling Chen, Xiao-tong Han, Chuan-zhu Lyu. Global research trends in cardiac arrest research: a visual analysis of the literature based on CiteSpace [J]. World Journal of Emergency Medicine, 2022, 13(4): 290-296. |
| [13] | Hong-li Xiao, Lian-xing Zhao, Jun Yang, Nan Tong, Le An, Guo-xing Wang, Miao-rong Xie, Chun-sheng Li. Increasing angiotensin-converting enzyme (ACE) 2/ACE axes ratio alleviates early pulmonary vascular remodeling in a porcine model of acute pulmonary embolism with cardiac arrest [J]. World Journal of Emergency Medicine, 2022, 13(3): 208-214. |
| [14] | Chao-yu Lei, Heng-wei Qin, Xue-jie Dong, Jia-lin You, Lin Zhang. Layperson’s performance on an unconversant type of AED device: A prospective crossover simulation experimental study [J]. World Journal of Emergency Medicine, 2022, 13(2): 98-105. |
| [15] | Ryan W. Horton, Kian R. Niknam, Viveta Lobo, Kathryn H. Pade, Drew Jones, Kenton L. Anderson. A cadaveric model for transesophageal echocardiography transducer placement training: A pilot study [J]. World Journal of Emergency Medicine, 2022, 13(1): 18-22. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
