World Journal of Emergency Medicine ›› 2024, Vol. 15 ›› Issue (3): 197-203.doi: 10.5847/wjem.j.1920-8642.2024.047
• Original Articles • Previous Articles Next Articles
Subi Abudurexiti1, Shihai Xu2, Zhangping Sun3, Yi Jiang4, Ping Gong2( )
)
Received:2023-11-12
Accepted:2024-03-06
Online:2024-05-15
Published:2024-05-01
Contact:
Ping Gong, Email: Subi Abudurexiti, Shihai Xu, Zhangping Sun, Yi Jiang, Ping Gong. Glucose metabolic reprogramming-related parameters for the prediction of 28-day neurological prognosis and all-cause mortality in patients after cardiac arrest: a prospective single-center observational study[J]. World Journal of Emergency Medicine, 2024, 15(3): 197-203.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2024.047
Table 1.
Baseline characteristics of the enrolled participants on ICU admission
| Parameters | Healthy volunteers (n=40) | Survivors (n=38) | Non-survivors (n=82) | P-valuea |
|---|---|---|---|---|
| Age, years, median (IQR) | 58.9 (39.8-72.0) | 64.5 (51.3-77.8) | 73.0 (60.0-82.2) | 0.608 |
| Male, n (%) | 21 (52.5) | 24 (63.2) | 47 (57.3) | 0.690 |
| Comorbidities, n (%) | ||||
| Diabetes | — | 10 (26.3) | 31 (37.8) | 0.301 |
| Hypertension | — | 16 (42.1) | 39 (47.6) | 0.694 |
| Coronary heart disease | — | 9 (23.7) | 18 (21.9) | 0.210 |
| Cerebrovascular disease | — | 5 (13.2) | 15 (18.3) | 0.603 |
| Chronic pulmonary disease | — | 4 (10.5) | 4 (4.9) | 0.261 |
| Chronic kidney disease | — | — | 6 (7.3) | — |
| CA causes, n (%) | ||||
| Cardiac | — | 24 (63.2) | 42 (51.2) | 0.243 |
| Respiratory | — | 2 (5.3) | 9 (11.0) | 0.499 |
| Septic | — | 5 (13.2) | 13 (15.9) | 0.790 |
| Cerebral | — | 3 (7.9) | 13 (15.9) | 0.386 |
| Others | — | 4 (10.5) | 5 (6.1) | 0.462 |
| Out-of-hospital CA, n (%) | — | 10 (26.3) | 34 (41.5) | 0.154 |
| Witnessed CA, n (%) | — | 33 (86.8) | 55 (67.1) | 0.027 |
| Bystander CPR, n (%) | — | 34 (89.5) | 59 (72.0) | 0.036 |
| Initial cardiac rhythm, n (%) | ||||
| VT | — | 1 (2.6) | 4 (4.9) | 0.492 |
| VF | — | 10 (26.3) | 10 (12.2) | 0.047 |
| Asystole and pulseless activity | — | 16 (42.1) | 17 (20.7) | 0.027 |
| Unknown | — | 11 (28.9) | 51 (62.2) | 0.001 |
| CPR time, min, median (IQR) | — | 10.0 (5.0-25.0) | 15.0 (6.5 -28.5) | 0.016 |
| Length of ICU stay, d, median (IQR) | — | 8 (5-12) | 5 (2-11) | 0.003 |
| Laboratory findings, median (IQR) | ||||
| WBC, ×109/L | 6.82 (5.45-8.49) | 12.40 (8.74-18.60) | 14.88 (10.42-20.08) | 0.201 |
| Neutrophil ratio, % | 57.3 (50.2-63.4) | 84.3 (76.6-90.2) | 87.7 (82.9-91.3) | 0.084 |
| PCT, ng/mL | 0.15 (0.01-0.33) | 1.82 (0.91-5.67) | 4.59 (0.83-11.00) | 0.159 |
| Creatinine, μmol/L | 64.5 (57.2-79.2) | 103.0 (85.5-178.0) | 137.0 (91.8-231.3) | 0.183 |
| High sensitivity troponin I, μg/L | 0.01 (0.00-0.03) | 0.22 (0.09-3.93) | 0.94 (0.21-8.57) | 0.112 |
| BNP, pg/mL | 30.8 (22.3-45.9) | 371.0 (119.7-1120.0) | 787.8 (233.1-1988.5) | 0.070 |
| PO2/FiO2, mmHg | 460.0 (410.8-482.0) | 320.0 (240.5-398.3) | 229.0 (157.0-335.3) | 0.259 |
| Blood glucose, μmol/L | 5.2 (4.7-5.7) | 8.6 (4.7-9.7) | 8.7 (6.0-13.2) | 0.342 |
| APACHE II score, median (IQR) | — | 14.0 (9.8-20.0) | 23.0 (19.0-26.0) | <0.01 |
| SOFA score, median (IQR) | — | 5.5 (4.0-7.8) | 12.0 (10.0-14.5) | <0.01 |
Table 2.
Baseline characteristics of the enrolled participants on ICU admission according to neurological outcome
| Parameters | Healthy volunteers (n=40) | Good neurological outcome (n=23) | Poor neurological outcome (n=97) | P-valuea |
|---|---|---|---|---|
| Age, years, median (IQR) | 58.9 (39.8-72.0) | 66.0 (55.0-80.0) | 75.0 (54.0-82.3) | 0.141 |
| Male, n (%) | 21 (52.5) | 16 (69.6) | 55 (56.7) | 0.584 |
| Comorbidities, n (%) | ||||
| Diabetes | — | 9 (39.1) | 33 (34.0) | 0.841 |
| Hypertension | — | 10 (43.5) | 46 (47.4) | 0.871 |
| Coronary heart disease | — | 8 (34.8) | 34 (35.1) | 0.681 |
| Cerebrovascular disease | — | 4 (17.4) | 17 (17.5) | 0.523 |
| Chronic pulmonary disease | — | 3 (13.0) | 7 (7.2) | 0.379 |
| Chronic kidney disease | — | — | 6 (6.2) | 0.114 |
| CA causes, n (%) | ||||
| Cardiac | — | 14 (60.8) | 48 (49.4) | 0.320 |
| Respiratory | — | 4 (17.4) | 9 (9.2) | 0.621 |
| Septic | — | 3 (13.0) | 9 (9.2) | 0.606 |
| Cerebral | — | 1 (4.3) | 14 (14.4) | 0.224 |
| Others | — | 1 (4.3) | 17 (19.6) | 0.162 |
| Out-of-hospital CA, n (%) | — | 10 (43.4) | 42 (43.2) | 0.302 |
| Witnessed CA, n (%) | — | 13 (56.5) | 62 (63.9) | 0.042 |
| Bystander CPR, n (%) | — | 12 (52.2) | 66 (68.0) | 0.033 |
| Initial cardiac rhythm, n (%) | ||||
| VT | — | 2 (8.7) | 6 (6.2) | 0.607 |
| VF | — | 7 (30.4) | 13 (13.4) | 0.050 |
| Asystole and pulseless activity | — | 3 (13.0) | 20 (20.6) | 0.456 |
| Unknown | — | 11 (47.8) | 59 (60.8) | 0.258 |
| CPR time, min, median (IQR) | — | 5.0 (3.0-25.0) | 17.0 (10.0 -30.0) | 0.016 |
| Length of ICU stay, d, median (IQR) | — | 7.0 (4.0-14.0) | 5.0 (2.0-15.0) | 0.268 |
| Laboratory findings, median (IQR) | ||||
| WBC, ×109/L | 6.82 (5.45-8.49) | 12.50 (9.90-20.40) | 14.30 (9.40-19.70) | 0.792 |
| Neutrophil ratio, % | 57.3 (50.2-63.4) | 84.5 (76.0-90.2) | 87.2 (81.6-91.2) | 0.198 |
| PCT, ng/mL | 0.15 (0.01-0.33) | 1.00 (0.41-3.67) | 4.50 (0.83-8.91) | 0.156 |
| Creatinine, μmol/L | 64.5 (57.2-79.2) | 85.5 (62.3-137.5) | 139.0 (95.0-232.0) | 0.158 |
| High sensitivity troponin I, μg/L | 0.01 (0.00-0.03) | 0.17 (0.07-1.13) | 0.78 (0.18-7.97) | 0.081 |
| BNP, pg/mL | 30.8 (22.3-45.9) | 444.3 (83.6-1154.0) | 702.0 (185.1-2066.3) | 0.270 |
| PO2/FiO2, mmHg | 460.0 (410.8-482.0) | 347.0 (262.9-402.6) | 214.0 (152.0-360.0) | 0.314 |
| Blood glucose, μmol/L | 5.2 (4.7-5.7) | 7.1 (4.2-9.9) | 10.6 (6.1-13.6) | 0.128 |
| APACHE II score, median (IQR) | — | 13.0 (9.0-18.0) | 23.0 (18.0-25.0) | <0.01 |
| SOFA score, median (IQR) | — | 6.0 (2.0-9.3) | 12.0 (10.0-14.0) | 0.011 |

Figure 1.
Comparisons of the serum LDH (A), lactate (B), pyruvate (C), lactate/pyruvate ratio (D), NSE (E), IL-6 (F), APACHE II (G) and SOFA (H) scores among healthy volunteers, survivors and non-survivors. LDH: lactate dehydrogenase; NSE: neuron-specific enolase; IL-6: interleukin-6; APACHE II: Acute Physiology and Chronic Health Evaluation II; SOFA: Sequential Organ Failure Assessment; ROSC: restoration of spontaneous circulation; *P<0.05 versus healthy volunteers; #P<0.05 versus survivors.
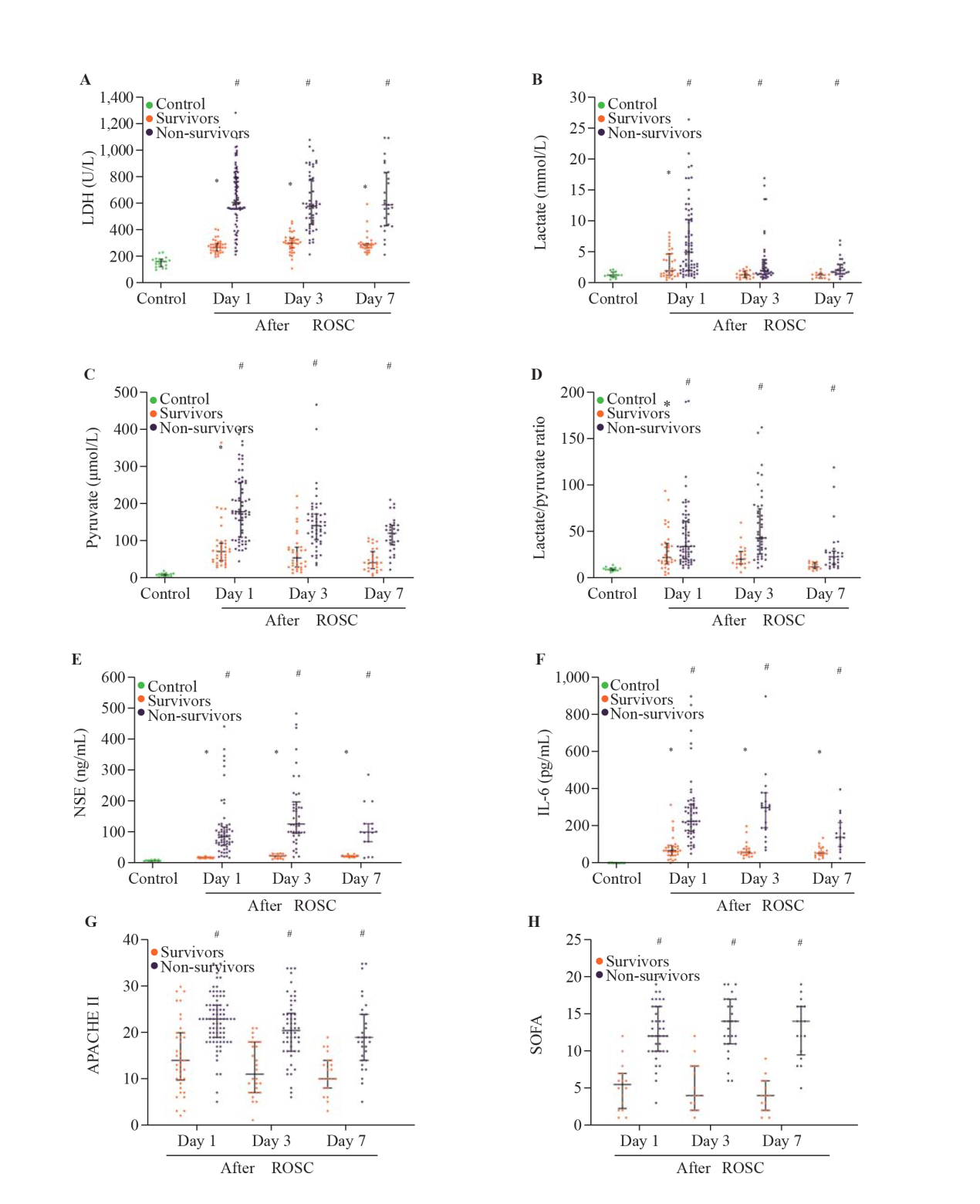
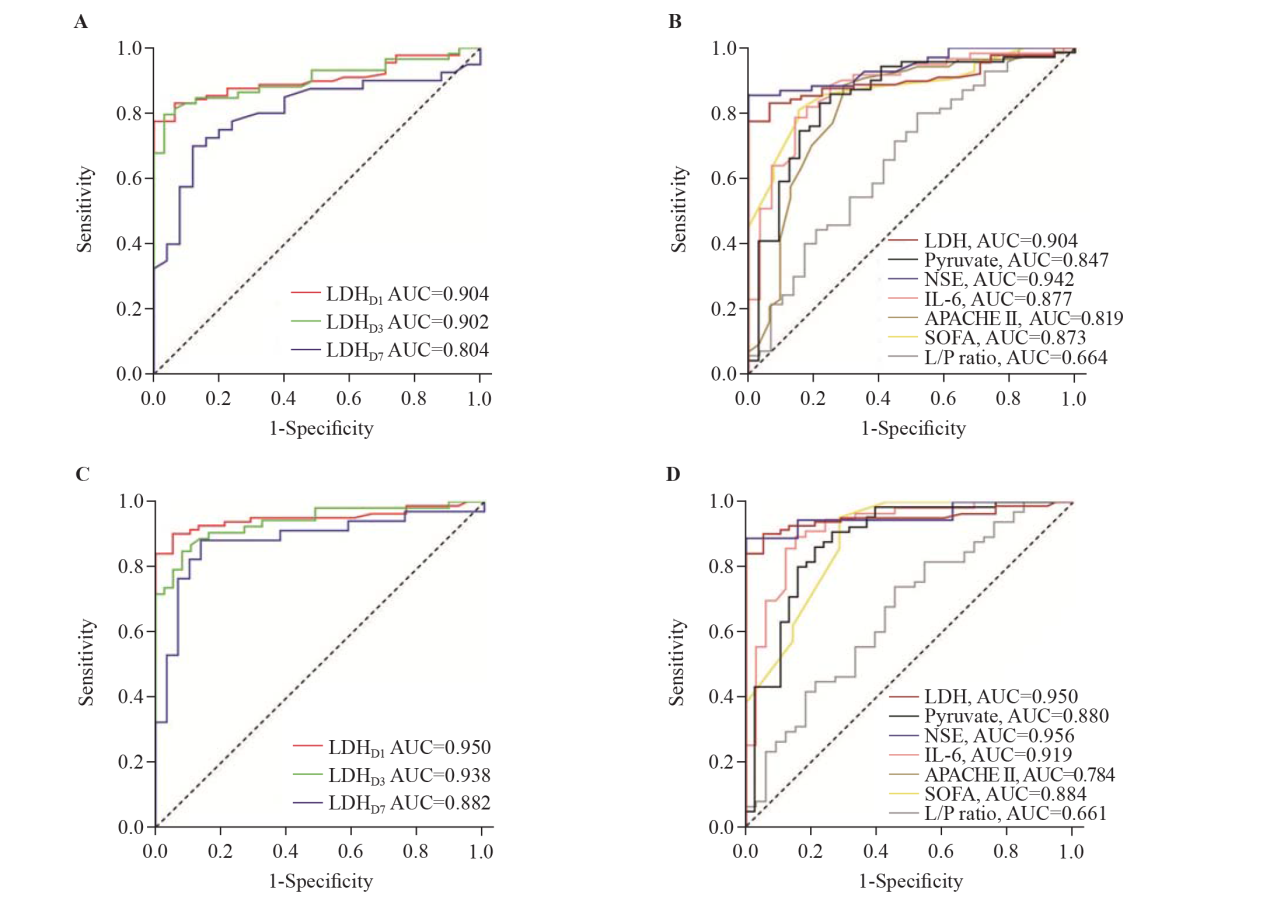
Figure 2.
Receiver operating characteristic curves of serum LDH on days 1, 3, and 7 after ROSC as well as LDH, pyruvate, NSE, IL-6, APACHE II score, SOFA score, and L/P ratio on day 1 after ROSC for the prediction of poor 28-day neurological prognosis (A, B) and 28-day all-cause mortality (C, D). AUC: area under the curve; LDH: lactate dehydrogenase; NSE: neuron-specific enolase; IL-6: interleukin-6; APACHE II: Acute Physiology and Chronic Health Evaluation II; SOFA: Sequential Organ Failure Assessment; L/P ratio: lactate/pyruvate ratio.
| 1 |
Birkun A. Understanding the epidemiology and outcomes of out-of-hospital cardiac arrest in the former Union of Soviet Socialist Republics: observations from the Crimean peninsula. World J Emerg Med. 2022; 13(1):67-8.
doi: 10.5847/wjem.j.1920-8642.2022.009 pmid: 35003419 |
| 2 | Yan SJ, Chen M, Wen J, Fu WN, Song XY, Chen HJ, et al. Global research trends in cardiac arrest research: a visual analysis of the literature based on CiteSpace. World J Emerg Med. 2022; 13(4):290-6. |
| 3 |
Martin E, Rosenthal RE, Fiskum G. Pyruvate dehydrogenase complex: metabolic link to ischemic brain injury and target of oxidative stress. J Neurosci Res. 2005; 79(1-2): 240-7.
pmid: 15562436 |
| 4 |
Suetrong B, Walley KR. Lactic acidosis in sepsis: it’s not all anaerobic: implications for diagnosis and management. Chest. 2016; 149(1):252-61.
doi: 10.1378/chest.15-1703 pmid: 26378980 |
| 5 | van Wyngene L, Vandewalle J, Libert C. Reprogramming of basic metabolic pathways in microbial sepsis: therapeutic targets at last? EMBO Mol Med. 2018; 10(8): e8712. |
| 6 | Vaupel P, Multhoff G. Revisiting the Warburg effect: historical dogma versus current understanding. J Physiol. 2021; 599(6):1745-57. |
| 7 |
Schöder H, Knight RJ, Kofoed KF, Schelbert HR, Buxton DB. Regulation of pyruvate dehydrogenase activity and glucose metabolism in post-ischaemic myocardium. Biochim Biophys Acta. 1998; 1406(1):62-72.
pmid: 9545535 |
| 8 | Callaway CW, Soar J, Aibiki M, Böttiger BW, Brooks SC, Deakin CD, et al. Part 4: advanced life support: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015; 132(16 Suppl 1):S84-S145. |
| 9 |
Soar J, Berg KM, Andersen LW, Böttiger BW, Cacciola S, Callaway CW, et al. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020; 156:A80-A119.
doi: 10.1016/j.resuscitation.2020.09.012 pmid: 33099419 |
| 10 |
Hellmann F, Verdi M, Schlemper BR Jr, Caponi S. 50th anniversary of the Declaration of Helsinki: the double standard was introduced. Arch Med Res. 2014; 45(7):600-1.
doi: 10.1016/j.arcmed.2014.10.005 pmid: 25450586 |
| 11 |
Lu J, Wei ZH, Jiang H, Cheng L, Chen QH, Chen MQ, et al. Lactate dehydrogenase is associated with 28-day mortality in patients with sepsis: a retrospective observational study. J Surg Res. 2018; 228:314-21.
doi: S0022-4804(18)30198-7 pmid: 29907227 |
| 12 | Kalogeris T, Baines CP, Krenz M, Korthuis RJ. Ischemia/reperfusion. Compr Physiol. 2016; 7(1):113-70. |
| 13 |
Issa MS, Grossestreuer AV, Patel H, Ntshinga L, Coker A, Yankama T, et al. Lactate and hypotension as predictors of mortality after in-hospital cardiac arrest. Resuscitation. 2021; 158:208-14.
doi: 10.1016/j.resuscitation.2020.10.018 pmid: 33289651 |
| 14 |
Li ZF, Zhang B, Yao WL, Zhang CH, Wan L, Zhang Y. APC-Cdh1 regulates neuronal apoptosis through modulating glycolysis and pentose-phosphate pathway after oxygen-glucose deprivation and reperfusion. Cell Mol Neurobiol. 2019; 39(1):123-35.
doi: 10.1007/s10571-018-0638-x pmid: 30460429 |
| 15 |
Dienel GA, Cruz NF. Aerobic glycolysis during brain activation: adrenergic regulation and influence of norepinephrine on astrocytic metabolism. J Neurochem. 2016; 138(1):14-52.
doi: 10.1111/jnc.13630 pmid: 27166428 |
| 16 |
Seppet E, Gruno M, Peetsalu A, Gizatullina Z, Nguyen HP, Vielhaber S, et al. Mitochondria and energetic depression in cell pathophysiology. Int J Mol Sci. 2009; 10(5):2252-303.
doi: 10.3390/ijms10052252 pmid: 19564950 |
| 17 |
Bas-Orth C, Tan YW, Lau D, Bading H. Synaptic activity drives a genomic program that promotes a neuronal Warburg effect. J Biol Chem. 2017; 292(13):5183-94.
doi: 10.1074/jbc.M116.761106 pmid: 28196867 |
| 18 | Cheng SC, Joosten LA, Netea MG. The interplay between central metabolism and innate immune responses. Cytokine Growth Factor Rev. 2014; 25(6):707-13. |
| 19 | Adrie C, Adib-Conquy M, Laurent I, Monchi M, Vinsonneau C, Fitting C, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002; 106(5):562-8. |
| 20 |
Haas SA, Lange T, Saugel B, Petzoldt M, Fuhrmann V, Metschke M, et al. Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med. 2016; 42(2):202-10.
doi: 10.1007/s00134-015-4127-0 pmid: 26556617 |
| 21 |
Mahmoodpoor A, Shadvar K, Saghaleini SH, Koleini E, Hamishehkar H, Ostadi Z, et al. Which one is a better predictor of ICU mortality in septic patients? Comparison between serial serum lactate concentrations and its removal rate. J Crit Care. 2018; 44:51-6.
doi: S0883-9441(17)31348-5 pmid: 29065350 |
| 22 |
Parsikia A, Bones K, Kaplan M, Strain J, Leung PS, Ortiz J, et al. The predictive value of initial serum lactate in trauma patients. Shock. 2014; 42(3):199-204.
doi: 10.1097/SHK.0000000000000208 pmid: 24978889 |
| 23 |
Nishioka N, Kobayashi D, Izawa J, Irisawa T, Yamada T, Yoshiya K, et al. Association between serum lactate level during cardiopulmonary resuscitation and survival in adult out-of-hospital cardiac arrest: a multicenter cohort study. Sci Rep. 2021; 11(1): 1639.
doi: 10.1038/s41598-020-80774-4 pmid: 33452306 |
| 24 |
Lee DH, Cho IS, Lee SH, Min YI, Min JH, Kim SH, et al. Correlation between initial serum levels of lactate after return of spontaneous circulation and survival and neurological outcomes in patients who undergo therapeutic hypothermia after cardiac arrest. Resuscitation. 2015; 88:143-9.
doi: 10.1016/j.resuscitation.2014.11.005 pmid: 25450570 |
| 25 |
Punniyakotty B, Ong XL, Ahmad M, Kirresh A. Improving mortality in pediatric out-of-hospital cardiac arrest events requires a multifactorial approach. JACC Asia. 2023; 3(1):166.
doi: 10.1016/j.jacasi.2022.11.011 pmid: 36873764 |
| 26 |
Starodub R, Abella BS, Grossestreuer AV, Shofer FS, Perman SM, Leary M, et al. Association of serum lactate and survival outcomes in patients undergoing therapeutic hypothermia after cardiac arrest. Resuscitation. 2013; 84(8):1078-82.
doi: 10.1016/j.resuscitation.2013.02.001 pmid: 23402966 |
| 27 | Lee TR, Kang MJ, Cha WC, Shin TG, Sim MS, Jo IJ, et al. Better lactate clearance associated with good neurologic outcome in survivors who treated with therapeutic hypothermia after out-of-hospital cardiac arrest. Crit Care. 2013; 17(5): R260. |
| 28 | Riske L, Thomas RK, Baker GB, Dursun SM. Lactate in the brain:an update on its relevance to brain energy, neurons, glia and panic disorder. Ther Adv Psychopharmacol. 2017; 7(2): 85-9. |
| 29 |
Ji J, Qian SY, Liu J, Gao HM. Occurrence of early epilepsy in children with traumatic brain injury: a retrospective study. World J Pediatr. 2022; 18(3):214-21.
doi: 10.1007/s12519-021-00502-4 pmid: 35150398 |
| 30 |
Hosmann A, Schober A, Gruber A, Sterz F, Testori C, Warenits A, et al. Cerebral and peripheral metabolism to predict successful reperfusion after cardiac arrest in rats: a microdialysis study. Neurocrit Care. 2016; 24(2):283-93.
doi: 10.1007/s12028-015-0214-x pmid: 26582187 |
| 31 |
Mölström S, Nielsen TH, Nordström CH, Forsse A, Möller S, Venö S, et al. Bedside microdialysis for detection of early brain injury after out-of-hospital cardiac arrest. Sci Rep. 2021; 11(1):15871.
doi: 10.1038/s41598-021-95405-9 pmid: 34354178 |
| 32 |
Suistomaa M, Ruokonen E, Kari A, Takala J. Time-pattern of lactate and lactate to pyruvate ratio in the first 24 hours of intensive care emergency admissions. Shock. 2000; 14(1):8-12.
pmid: 10909886 |
| 33 |
Jha MK, Lee IK, Suk K. Metabolic reprogramming by the pyruvate dehydrogenase kinase-lactic acid axis: linking metabolism and diverse neuropathophysiologies. Neurosci Biobehav Rev. 2016; 68:1-19.
doi: S0149-7634(16)30102-6 pmid: 27179453 |
| 34 | Fukuda T, Ohashi-Fukuda N, Sekiguchi H, Inokuchi R, Kukita I. Survival from pediatric out-of-hospital cardiac arrest during nights and weekends: an updated japanese registry-based study. JACC Asia. 2022; 2(4):433-43. |
| 35 |
Henry BM, Aggarwal G, Wong J, Benoit S, Vikse J, Plebani M, et al. Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: a pooled analysis. Am J Emerg Med. 2020; 38(9):1722-6.
doi: S0735-6757(20)30436-8 pmid: 32738466 |
| 36 | Khalilov RA, Dzhafarova AM, Khizrieva SI. Effect of hypothermia on kinetic characteristics of lactate dehydrogenase in rat brain under conditions of global ischemia and reperfusion. Bull Exp Biol Med. 2017; 163(3):334-7. |
| [1] | Rashed Alremeithi, Quincy K. Tran, Megan T. Quintana, Soroush Shahamatdar, Ali Pourmand. Approach to traumatic cardiac arrest in the emergency department: a narrative literature review for emergency providers [J]. World Journal of Emergency Medicine, 2024, 15(1): 3-9. |
| [2] | Jing Yang, Hanqi Tang, Shihuan Shao, Feng Xu, Yangyang Fu, Shengyong Xu, Chen Li, Yan Li, Yang Liu, Joseph Harold Walline, Huadong Zhu, Yuguo Chen, Xuezhong Yu, Jun Xu. A novel predictor of unsustained return of spontaneous circulation in cardiac arrest patients through a combination of capnography and pulse oximetry: a multicenter observational study [J]. World Journal of Emergency Medicine, 2024, 15(1): 16-22. |
| [3] | Jiale Yang, Fanghe Gong, Xuezhi Shi, Fanfan Wang, Jing Qian, Lulu Wan, Yi Chen, Huaisheng Chen, Huasheng Tong. A nomogram based on lymphocyte percentage for predicting hospital mortality in exertional heatstroke patients: a 13-year retrospective study [J]. World Journal of Emergency Medicine, 2023, 14(6): 434-441. |
| [4] | Gannan Wang, Zhe Wang, Yi Zhu, Zhongman Zhang, Wei Li, Xufeng Chen, Yong Mei. The neuro-prognostic value of the ion shift index in cardiac arrest patients following extracorporeal cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2023, 14(5): 354-359. |
| [5] | Yue Li, Yong-peng Xie, Xiao-min Li, Tao Lu. Effects of early standardized enteral nutrition on preventing acute muscle loss in the acute exacerbation of chronic obstructive pulmonary disease patients with mechanical ventilation [J]. World Journal of Emergency Medicine, 2023, 14(3): 193-197. |
| [6] | Guang-qi Guo, Yan-nan Ma, Shuang Xu, Hong-rong Zhang, Peng Sun. Effect of post-rewarming fever after targeted temperature management in cardiac arrest patients: a systematic review and meta-analysis [J]. World Journal of Emergency Medicine, 2023, 14(3): 217-223. |
| [7] | Xiao-guang Zhu, Jia-mei Jiang, Yong-xia Li, Jing Gao, Wei Wu, Qi-ming Feng. Development and validation of a nomogram for predicting survival in patients with acute pancreatitis [J]. World Journal of Emergency Medicine, 2023, 14(1): 44-48. |
| [8] | Gan-nan Wang, Zhong-man Zhang, Wen Chen, Xiao-quan Xu, Jin-song Zhang. Timing of brain computed tomography for predicting neurological prognosis in comatose cardiac arrest survivors: a retrospective observational study [J]. World Journal of Emergency Medicine, 2022, 13(5): 349-354. |
| [9] | Fei Shao, Xian Shi, Shu-hua Huo, Qing-yu Liu, Ji-xue Shi, Jian Kang, Ping Gong, Sheng-tao Yan, Guo-xing Wang, Li-jie Qin, Fei Wang, Ke Feng, Feng-ying Chen, Yong-jie Yin, Tao Ma, Yan Li, Yang Wu, Hao Cui, Chang-xiao Yu, Song Yang, Wei Gan, Sai Wang, Liu-ye-zi Du, Ming-chen Zhao, Zi-ren Tang, Shen Zhao. Development and evaluation of a predictive nomogram for survival in heat stroke patients: a retrospective cohort study [J]. World Journal of Emergency Medicine, 2022, 13(5): 355-360. |
| [10] | Shi-jiao Yan, Mei Chen, Jing Wen, Wen-ning Fu, Xing-yue Song, Huan-jun Chen, Ri-xing Wang, Mei-ling Chen, Xiao-tong Han, Chuan-zhu Lyu. Global research trends in cardiac arrest research: a visual analysis of the literature based on CiteSpace [J]. World Journal of Emergency Medicine, 2022, 13(4): 290-296. |
| [11] | Hong-li Xiao, Lian-xing Zhao, Jun Yang, Nan Tong, Le An, Guo-xing Wang, Miao-rong Xie, Chun-sheng Li. Increasing angiotensin-converting enzyme (ACE) 2/ACE axes ratio alleviates early pulmonary vascular remodeling in a porcine model of acute pulmonary embolism with cardiac arrest [J]. World Journal of Emergency Medicine, 2022, 13(3): 208-214. |
| [12] | Chao-yu Lei, Heng-wei Qin, Xue-jie Dong, Jia-lin You, Lin Zhang. Layperson’s performance on an unconversant type of AED device: A prospective crossover simulation experimental study [J]. World Journal of Emergency Medicine, 2022, 13(2): 98-105. |
| [13] | Ji-yang Ling, Chun-sheng Li, Yun Zhang, Xiao-li Yuan, Bo Liu, Yong Liang, Qiang Zhang. Protective effect of extracorporeal membrane pulmonary oxygenation combined with cardiopulmonary resuscitation on post-resuscitation lung injury [J]. World Journal of Emergency Medicine, 2021, 12(4): 303-308. |
| [14] | Wei-jing Shao, Ting-ting Shu, Shuang Xu, Li-cai Liang, Jehane Michael Le Grange, Yu-ran Zhou, He Huang, Yu Cai, Qing Zhang, Peng Sun. Left-sided vagus nerve stimulation improves cardiopulmonary resuscitation outcomes in rats as effectively as right-sided vagus nerve stimulation [J]. World Journal of Emergency Medicine, 2021, 12(4): 309-316. |
| [15] | Yu-ming Wang, Yan-jun Zheng, Ying Chen, Yun-chuan Huang, Wei-wei Chen, Ran Ji, Li-li Xu, Zhi-tao Yang, Hui-qiu Sheng, Hong-ping Qu, En-qiang Mao, Er-zhen Chen. Effects of fluid balance on prognosis of acute respiratory distress syndrome patients secondary to sepsis [J]. World Journal of Emergency Medicine, 2020, 11(4): 216-222. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
