World Journal of Emergency Medicine ›› 2025, Vol. 16 ›› Issue (2): 136-143.doi: 10.5847/wjem.j.1920-8642.2025.036
• Original Articles • Previous Articles Next Articles
Peili Chen, Yan Ge, Huiqiu Sheng, Wenwu Sun, Jiahui Wang, Li Ma( ), Enqiang Mao(
), Enqiang Mao( )
)
Received:2024-11-20
Accepted:2025-01-15
Online:2025-03-19
Published:2025-03-01
Contact:
Li Ma, Email: Peili Chen, Yan Ge, Huiqiu Sheng, Wenwu Sun, Jiahui Wang, Li Ma, Enqiang Mao. The role of early changes in routine coagulation tests in predicting the occurrence and prognosis of sepsis[J]. World Journal of Emergency Medicine, 2025, 16(2): 136-143.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2025.036
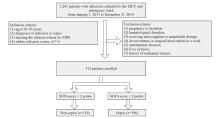
Figure 1.
The flowchart of this study. Clinical diagnoses: upon admission, the patient was diagnosed by the clinician with organ infection or sepsis. SIRS: systemic inflammatory response syndrome, defined as the presence of two or more of the following: (1) temperature <36 °C or >38 °C; (2) heart rate >90 beats/min; (3) respiratory rate >20 breaths/min or PaCO2 < 32 mmHg; and (4) white blood cell count≥12,000 cells/mm3 or≤4,000 cells/mm3. SOFA: based on six different scores, one for each of the respiratory, cardiovascular, hepatic, coagulation, renal and neurological systems and allocates a score of 0-4 with an increasing score reflecting worsening organ dysfunction.
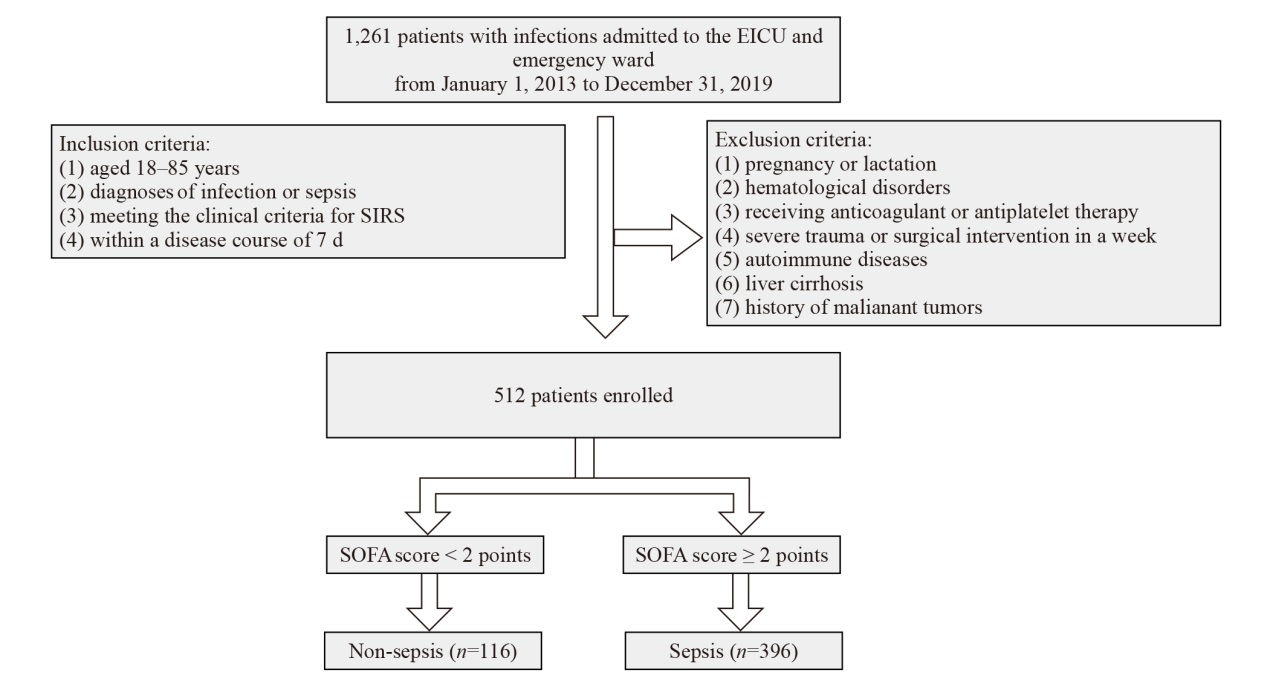
Table 1.
Logistics regression analysis of predictive markers for sepsis
| Variables | Univariate regression | Multivariate regression | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95%CI | P-value | ||
| Gender | 0.94 | 0.617-1.434 | 0.788 | ||||
| Age | 0.99 | 0.982-1.004 | 0.242 | ||||
| APECHEII | 1.04 | 1.016-1.071 | 0.002 | 0.984 | 0.931-1.040 | 0.564 | |
| SAPS II | 0.99 | 0.967-1.024 | 0.710 | ||||
| Pulmonary infection | 0.28 | 0.015-1.574 | 0.235 | ||||
| APTT | 1.02 | 0.997-1.058 | 0.105 | ||||
| PT | 1.42 | 1.248-1.645 | <0.001 | 0.930 | 0.749-1.154 | 0.510 | |
| TT | 1.06 | 0.991-1.143 | 0.136 | ||||
| Fg | 0.89 | 0.788-0.995 | 0.040 | 1.006 | 0.759-1.333 | 0.968 | |
| FDP | 1.32 | 1.243-1.403 | <0.001 | 1.144 | 1.029-1.272 | <0.001 | |
| D-dimer | 1.90 | 1.671-2.194 | <0.001 | 1.452 | 1.122-1.880 | 0.008 | |
| Platelet count | 1.00 | 0.998-1.002 | 0.930 | ||||
| Vasopressor | 28.50 | 8.862-174.336 | <0.001 | 1.569 | 0.185-13.346 | 0.680 | |
| Ventilator | 27.86 | 8.661-170.416 | <0.001 | 7.443 | 0.874-63.397 | 0.006 | |
| CRRT | 14735 | 0.051-61108 | 0.974 | ||||
| Operation | 2.12 | 1.069-4.714 | 0.044 | 1.538 | 0.440-5.381 | 0.500 | |
| PCT | 1.11 | 1.073-1.167 | <0.001 | 1.056 | 1.025-1.102 | 0.003 | |
| Bile acids | 1.03 | 1.012-1.067 | 0.013 | 1.005 | 0.959-1.053 | 0.834 | |
| Lactate | 3.16 | 2.247-4.613 | <0.001 | 2.274 | 1.473-3.651 | <0.001 | |
| CRP | 1.01 | 1.003-1.008 | <0.001 | 1.007 | 0.724-1.812 | 0.325 | |
| Chronic disease | 0.48 | 0.024-3.219 | 0.513 | ||||

Figure 2.
The nomogram of the presdictive model of sepsis occurrence. The nomogram was developed by visualizing graphical representations, wherein each factor was assigned a score based on its respective value. Subsequently, the total score was calculated by summing the individual scores, enabling the assessment of clinical risks. For instance, a patient admitted to the hospital presented with a lactate level of 1.94 mmol/L and a procalcitonin (PCT) level of 23 ng/mL without mechanical ventilation. Additionally, coagulation parameters revealed that fibrin degradation products (FDP) levels at 8.1 mg/L and D-dimer levels at 3 mg/L. These parameters were assigned β (X-m) scores of 0, 0.66, 0, -1.85 and -2.52, respectively. The final total score calculated amounted to -3.71 which corresponds to a predicted probability of sepsis at approximately 82.8%.
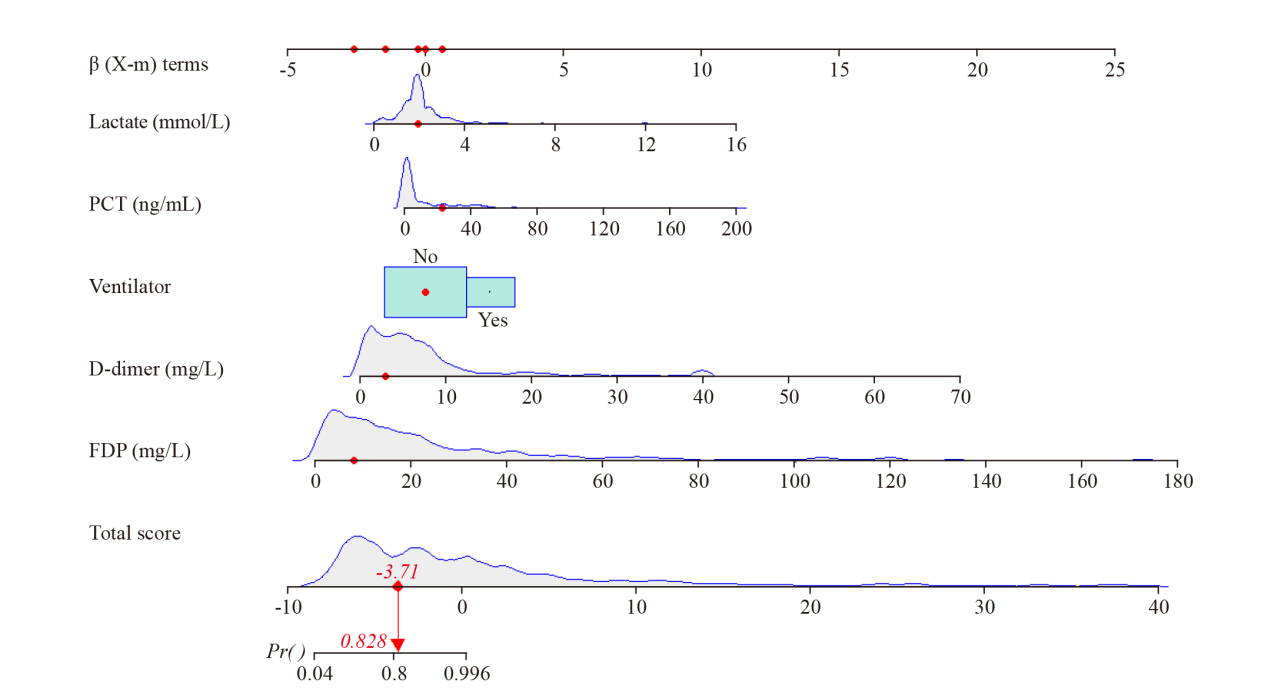
Figure 4.
The calibration plot of the sepsis prediction model. The dot line represents the model’s predicted fit, while the solid line represents the bias-corrected fit from 40 bootstrap resamples. The proximity of these curves to the reference line (dashed line) indicates strong alignment between predicted and actual values.
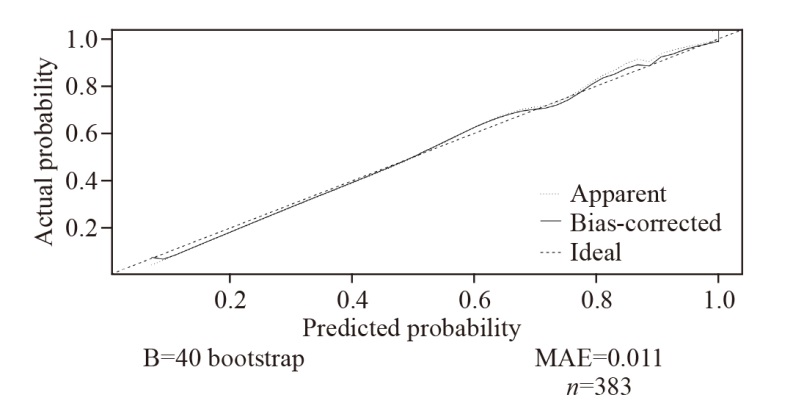
Figure 5.
Decision curve analysis (DCA) curve of the sepsis prediction model. The X-axis represents threshold probability, while the Y-axis represents the standard net benefit. The All line represents the net benefit of predicting that all patients will develop sepsis, while the None line represents the net benefit of predicting that none of the patients will develop sepsis. The decision curve for the sepsis prediction model lies between the All and None line and above the All line, indicating that the model provides an enhanced clinical decision-making.

Table 2.
Cox regression analysis for the mortality of sepsis
| Variables | Coefficient | Hazard ratio | 95% CI | P-value |
|---|---|---|---|---|
| Age | 0.021 | 1.021 | 1.008-1.034 | 0.021 |
| Prothrombin time | 0.042 | 1.043 | 1.011-1.077 | 0.008 |
| Vasopressor | 1.833 | 6.250 | 3.403-11.479 | <0.001 |
| Ventilator | 0.675 | 1.964 | 1.179-3.272 | 0.009 |
| Lactate | 0.164 | 1.178 | 1.074-1.291 | 0.004 |
| 1 |
Weng L, Zeng XY, Yin P, Wang LJ, Wang CY, Jiang W, et al. Sepsis-related mortality in China: a descriptive analysis. Intensive Care Med. 2018; 44(7): 1071-80.
doi: 10.1007/s00134-018-5203-z pmid: 29846748 |
| 2 |
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003; 31(4): 1250-6.
doi: 10.1097/01.CCM.0000050454.01978.3B pmid: 12682500 |
| 3 | Du LZ. Early diagnosis and management of neonatal sepsis: a perspective. World J Pediatr. 2024; 20(4):303-6. |
| 4 |
Iba T, Levi M, Levy JH. Sepsis-induced coagulopathy and disseminated intravascular coagulation. Semin Thromb Hemost. 2020; 46(1): 89-95.
doi: 10.1055/s-0039-1694995 pmid: 31443111 |
| 5 | Czempik PF, Wiórek A. Management strategies in septic coagulopathy: a review of the current literature. Healthcare (Basel). 2023; 11(2): 227. |
| 6 | Tsai HJ, Tsao CM, Liao MH, Ka SM, Liaw WJ, Wu CC. Application of thrombelastography in liver injury induced by endotoxin in rat. Blood Coagul Fibrinolysis. 2012; 23(2): 118-26. |
| 7 |
Spiel AO, Mayr FB, Firbas C, Quehenberger P, Jilma B. Validation of rotation thrombelastography in a model of systemic activation of fibrinolysis and coagulation in humans. J Thromb Haemost. 2006; 4(2): 411-6.
pmid: 16420574 |
| 8 | Daudel F, Kessler U, Folly H, Lienert JS, Takala J, Jakob SM. Thromboelastometry for the assessment of coagulation abnormalities in early and established adult sepsis: a prospective cohort study. Crit Care. 2009; 13(2): R42. |
| 9 | Müller MC, Meijers JCM, Vroom MB, Juffermans NP. Utility of thromboelastography and/or thromboelastometry in adults with sepsis: a systematic review. Crit Care. 2014; 18(1): R30. |
| 10 |
Marik PE, Taeb AM. SIRS, qSOFA and new sepsis definition. J Thorac Dis. 2017; 9(4): 943-5.
doi: 10.21037/jtd.2017.03.125 pmid: 28523143 |
| 11 |
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al.Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013; 39(2): 165-228.
doi: 10.1007/s00134-012-2769-8 pmid: 23361625 |
| 12 | Lu Y, Song L. Clinical significance of procalcitonin, lactic acid, and endotoxin testing for children with severe pneumonia and sepsis. Altern Ther Health Med. 2023; 29(3): 218-23. |
| 13 | Garcia-Alvarez M, Marik P, Bellomo R. Sepsis-associated hyperlactatemia. Crit Care. 2014; 18(5): 503. |
| 14 | Takeuchi M, Tachibana K. Mechanical ventilation for ARDS patients—for a better understanding of the 2012 Surviving Sepsis Campaign Guidelines. Cardiovasc Hematol Disord Drug Targets. 2015; 15(1): 41-5. |
| 15 |
Innocenti F, Gori AM, Giusti B, Tozzi C, Donnini C, Meo F, et al. Prognostic value of sepsis-induced coagulation abnormalities: an early assessment in the emergency department. Intern Emerg Med. 2019; 14(3):459-66.
doi: 10.1007/s11739-018-1990-z pmid: 30535649 |
| 16 |
Simmons J, Pittet JF. The coagulopathy of acute sepsis. Curr Opin Anaesthesiol. 2015; 28(2): 227-36.
doi: 10.1097/ACO.0000000000000163 pmid: 25590467 |
| 17 | Scarlatescu E, Tomescu D, Arama SS. Anticoagulant therapy in sepsis. the importance of timing. J Crit Care Med (Targu Mures). 2017; 3(2): 63-9. |
| 18 | Dhainaut JF, Shorr AF, Macias WL, Kollef MJ, Levi M, Reinhart K, et al. Dynamic evolution of coagulopathy in the first day of severe sepsis: relationship with mortality and organ failure. Crit Care Med. 2005; 33(2): 341-8. |
| 19 | Semeraro F, Colucci M, Caironi P, Masson S, Ammollo CT, Teli R, et al. Platelet drop and fibrinolytic shutdown in patients with sepsis. Crit Care Med. 2018; 46(3): e221-8. |
| 20 | Ito T, Thachil J, Asakura H, Levy JH, Iba T. Thrombomodulin in disseminated intravascular coagulation and other critical conditions-a multi-faceted anticoagulant protein with therapeutic potential. Crit Care. 2019; 23(1): 280. |
| 21 |
Colucci M, Semeraro N. Thrombin activatable fibrinolysis inhibitor: at the nexus of fibrinolysis and inflammation. Thromb Res. 2012; 129(3): 314-9.
doi: 10.1016/j.thromres.2011.10.031 pmid: 22113149 |
| 22 |
Totoki T, Ito T, Kakuuchi M, Yashima N, Maruyama I, Kakihana Y. An evaluation of circulating activated TAFI in septic DIC: a case series and review of the literature. Thromb J. 2022; 20(1): 6.
doi: 10.1186/s12959-022-00364-4 pmid: 35130927 |
| [1] | Chunxue Wang, Dianyin Yang, Yuxin Zhu, Qian Yang, Tong Liu, Xiandong Liu, Dongyang Zhao, Xiaowei Bao, Tiancao Dong, Li Shao, Lunxian Tang. Circulating circular RNAs act as potential novel biomarkers for sepsis secondary to pneumonia: a prospective cohort study [J]. World Journal of Emergency Medicine, 2025, 16(2): 144-152. |
| [2] | Azzah S Alharbi, Raghad Hassan Sanyi, Esam I Azhar. Bacteria and host: what does this mean for sepsis bottleneck? [J]. World Journal of Emergency Medicine, 2025, 16(1): 10-17. |
| [3] | Tianpeng Hu, Yan Li, Shengtao Yan, Lichao Sun, Rui Lian, Jieqiong Yu, Jie Chen, Xiaoyu Liu, Guoqiang Zhang. Application of myxovirus resistance protein A in the etiological diagnosis of infections in adults [J]. World Journal of Emergency Medicine, 2025, 16(1): 35-42. |
| [4] | Chao Gong, Shengyong Xu, Youlong Pan, Shigong Guo, Joseph Harold Walline, Xue Wang, Xin Lu, Shiyuan Yu, Mubing Qin, Huadong Zhu, Yanxia Gao, Yi Li. Effects of probiotic treatment on the prognosis of patients with sepsis: a systematic review [J]. World Journal of Emergency Medicine, 2025, 16(1): 18-27. |
| [5] | Qingliu Zheng, Changyun Liu, Lingying Le, Qiqi Wu, Zhihong Xu, Jiyan Lin, Qiuyun Chen. ICU-acquired weakness in critically ill patients at risk of malnutrition: risk factors, biomarkers, and early enteral nutrition impact [J]. World Journal of Emergency Medicine, 2025, 16(1): 51-56. |
| [6] | Jingyuan Xie, Jiandong Gao, Mutian Yang, Ting Zhang, Yecheng Liu, Yutong Chen, Zetong Liu, Qimin Mei, Zhimao Li, Huadong Zhu, Ji Wu. Prediction of sepsis within 24 hours at the triage stage in emergency departments using machine learning [J]. World Journal of Emergency Medicine, 2024, 15(5): 379-385. |
| [7] | Juexian Wei, Hengzong Mo, Yuting Zhang, Wenmin Deng, Siqing Zheng, Haifeng Mao, Yang Ji, Huilin Jiang, Yongcheng Zhu. Evolutionary trend analysis and knowledge structure mapping of endothelial dysfunction in sepsis: a bibliometrics study [J]. World Journal of Emergency Medicine, 2024, 15(5): 386-396. |
| [8] | Payush Chatta, Brian Diep, Jakrin Kewcharoen, Daniel Rossie, Cory Toomasian, Purvi Parwani, Dmitry Abramov. The diagnostic yield for computed tomography pulmonary angiography in patients with anticoagulation [J]. World Journal of Emergency Medicine, 2024, 15(4): 251-255. |
| [9] | Rex Pui Kin Lam, Zonglin Dai, Eric Ho Yin Lau, Carrie Yuen Ting Ip, Ho Ching Chan, Lingyun Zhao, Tat Chi Tsang, Matthew Sik Hon Tsui, Timothy Hudson Rainer. Comparing 11 early warning scores and three shock indices in early sepsis prediction in the emergency department [J]. World Journal of Emergency Medicine, 2024, 15(4): 273-282. |
| [10] | Huixin Zhao, Yiming Dong, Sijia Wang, Jiayuan Shen, Zhenju Song, Mingming Xue, Mian Shao. Comparison between sepsis-induced coagulopathy and sepsis-associated coagulopathy criteria in identifying sepsis-associated disseminated intravascular coagulation [J]. World Journal of Emergency Medicine, 2024, 15(3): 190-196. |
| [11] | A-ling Tang, Yan Li, Li-chao Sun, Xiao-yu Liu, Nan Gao, Sheng-tao Yan, Guo-qiang Zhang. Xuebijing improves intestinal microcirculation dysfunction in septic rats by regulating the VEGF-A/PI3K/Akt signaling pathway [J]. World Journal of Emergency Medicine, 2024, 15(3): 206-213. |
| [12] | Qing Zhao, Jinfu Ma, Jianguo Xiao, Zhe Feng, Hui Liu. Data driven analysis reveals prognostic genes and immunological targets in human sepsis-associated acute kidney injury [J]. World Journal of Emergency Medicine, 2024, 15(2): 91-97. |
| [13] | Weichao Ding, Wei Zhang, Juan Chen, Mengmeng Wang, Yi Ren, Jing Feng, Xiaoqin Han, Xiaohang Ji, Shinan Nie, Zhaorui Sun. Protective mechanism of quercetin in alleviating sepsis-related acute respiratory distress syndrome based on network pharmacology and in vitro experiments [J]. World Journal of Emergency Medicine, 2024, 15(2): 111-120. |
| [14] | Wei Zhou, Maiying Fan, Xiang Li, Fang Yu, En Zhou, Xiaotong Han. Molecular mechanism of Xuebijing in treating pyogenic liver abscess complicated with sepsis [J]. World Journal of Emergency Medicine, 2024, 15(1): 35-40. |
| [15] | Jingyi Wang, Li Weng, Jun Xu, Bin Du. Blood gas analysis as a surrogate for microhemodynamic monitoring in sepsis [J]. World Journal of Emergency Medicine, 2023, 14(6): 421-427. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
