World Journal of Emergency Medicine ›› 2024, Vol. 15 ›› Issue (2): 91-97.doi: 10.5847/wjem.j.1920-8642.2024.026
• Original Article • Previous Articles Next Articles
Qing Zhao1, Jinfu Ma2, Jianguo Xiao3, Zhe Feng4, Hui Liu3( )
)
Received:2023-05-29
Accepted:2023-11-20
Online:2024-03-11
Published:2024-03-01
Contact:
Hui Liu, Email: Qing Zhao, Jinfu Ma, Jianguo Xiao, Zhe Feng, Hui Liu. Data driven analysis reveals prognostic genes and immunological targets in human sepsis-associated acute kidney injury[J]. World Journal of Emergency Medicine, 2024, 15(2): 91-97.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2024.026

Figure 1.
Flowchart of the identification and bioinformatics analysis of the key genes related to sepsis-associated acute kidney injury (SA-AKI). The co-differentially expressed genes (co-DEGs) were identified and used to search for hub genes. Immune association and disease association were evaluated, and functional annotation of hub genes was performed. AKI: acute kidney injury; WGCNA: weighted gene coexpression network analysis; GWAS: genome-wide association study; GSEA: gene set enrichment analysis.
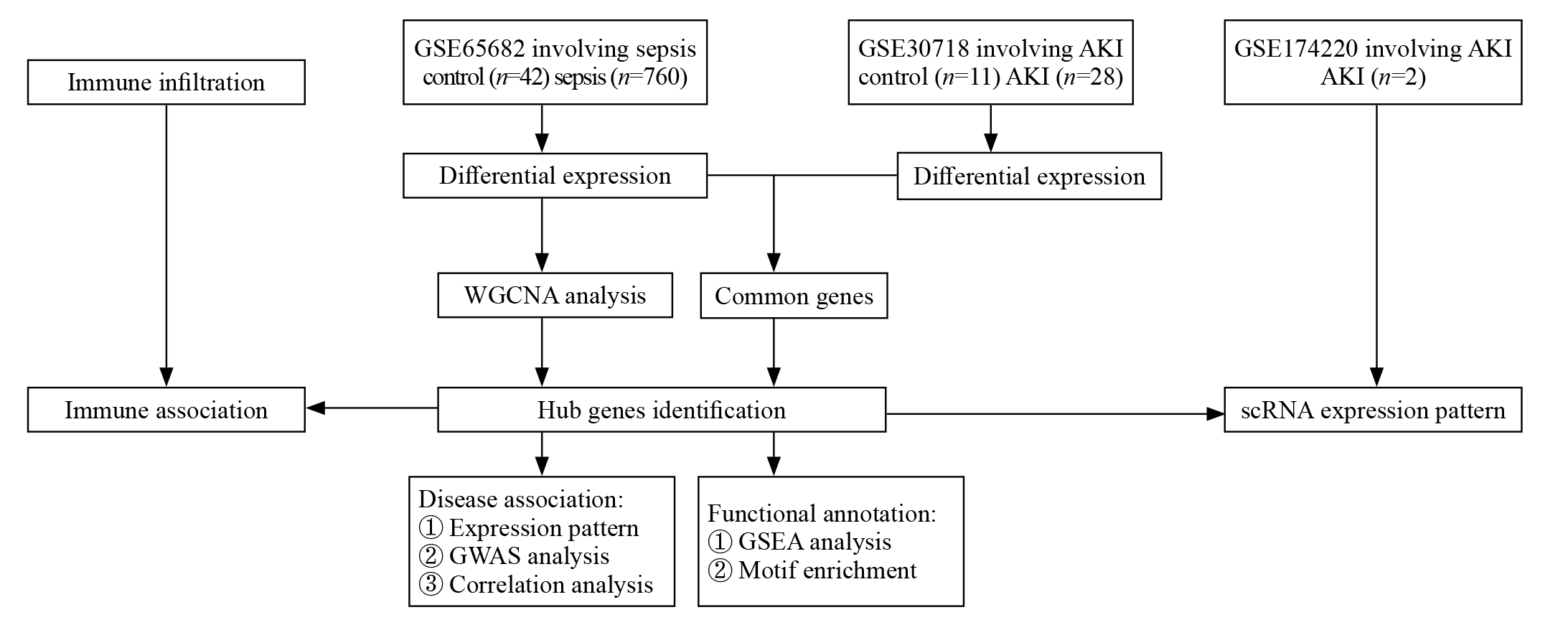

Figure 2.
The Kaplan-Meier survival analysis of septic patients with differences in the expression of IL32. IL32 was identified as an intersection gene of sepsis and AKI. The results showed that IL32 had significant survival differences in septic patients. A higher expression of IL32 was associated with a better prognosis in survival probability.

| 1 |
Peerapornratana S, Manrique-Caballero CL, Gómez H, Kellum JA. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int. 2019; 96(5): 1083-99.
doi: S0085-2538(19)30601-5 pmid: 31443997 |
| 2 |
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005; 294(7): 813-8.
doi: 10.1001/jama.294.7.813 pmid: 16106006 |
| 3 |
Bouchard J, Acharya A, Cerda J, Maccariello ER, Madarasu RC, Tolwani AJ, et al. A prospective international multicenter study of AKI in the intensive care unit. Clin J Am Soc Nephrol. 2015; 10(8): 1324-31.
doi: 10.2215/CJN.04360514 |
| 4 | Mehta RL, Bouchard J, Soroko SB, Ikizler TA, Paganini EP, Chertow GM, et al. Sepsis as a cause and consequence of acute kidney injury: Program to Improve Care in Acute Renal Disease. Intensive Care Med. 2011; 37(2): 241-8. |
| 5 |
Fani F, Regolisti G, Delsante M, Cantaluppi V, Castellano G, Gesualdo L, et al. Recent advances in the pathogenetic mechanisms of sepsis-associated acute kidney injury. J Nephrol. 2018; 31(3): 351-9.
doi: 10.1007/s40620-017-0452-4 pmid: 29273917 |
| 6 |
Gu Y, Huang F, Wang YL, Chen CJ, Wu S, Zhou SL, et al. Connexin32 plays a crucial role in ROS-mediated endoplasmic reticulum stress apoptosis signaling pathway in ischemia reperfusion-induced acute kidney injury. J Transl Med. 2018; 16(1): 117.
doi: 10.1186/s12967-018-1493-8 pmid: 29728112 |
| 7 |
Huen SC, Cantley LG. Macrophages in renal injury and repair. Annu Rev Physiol. 2017; 79: 449-69.
doi: 10.1146/annurev-physiol-022516-034219 pmid: 28192060 |
| 8 |
Zhang QY, Yang X, Peng M, Mi SL, Wang YL, Li XY, et al. Post-treatment with irisin attenuates acute kidney injury in sepsis mice through anti-ferroptosis via the SIRT1/Nrf2 pathway. Front Pharmacol. 2022; 13: 857067.
doi: 10.3389/fphar.2022.857067 |
| 9 | Poston JT, Koyner JL. Sepsis associated acute kidney injury. BMJ. 2019; 364: k4891. |
| 10 |
Kellum JA, Chawla LS, Keener C, Singbartl K, Palevsky PM, Pike FL, et al. The effects of alternative resuscitation strategies on acute kidney injury in patients with septic shock. Am J Respir Crit Care Med. 2016; 193(3): 281-7.
doi: 10.1164/rccm.201505-0995OC |
| 11 |
Manrique-Caballero CL, Del Rio-Pertuz G, Gomez H. Sepsis-associated acute kidney injury. Crit Care Clin. 2021; 37(2): 279-301.
doi: 10.1016/j.ccc.2020.11.010 pmid: 33752856 |
| 12 |
Kuwabara S, Goggins E, Okusa MD. The pathophysiology of sepsis-associated AKI. Clin J Am Soc Nephrol. 2022; 17(7): 1050-69.
doi: 10.2215/CJN.00850122 |
| 13 |
Zhang WY, Chen ZH, An XX, Li H, Zhang HL, Wu SJ, et al. Analysis and validation of diagnostic biomarkers and immune cell infiltration characteristics in pediatric sepsis by integrating bioinformatics and machine learning. World J Pediatr. 2023; 19(11):1094-103.
doi: 10.1007/s12519-023-00717-7 |
| 14 |
Gautam A, Pandit B. IL32: the multifaceted and unconventional cytokine. Hum Immunol. 2021; 82(9): 659-67.
doi: 10.1016/j.humimm.2021.05.002 pmid: 34024634 |
| 15 |
Kim SJ, Lee S, Kwak A, Kim E, Jo S, Bae S, et al. Interleukin-32γ transgenic mice resist LPS-mediated septic shock. J Microbiol Biotechnol. 2014; 24(8): 1133-42.
doi: 10.4014/jmb.1404.04012 |
| 16 |
Shen W, Bian L, Ma Y, Yin X. Serum IL-6 as a marker of disease progression in interstitial nephritis. Am J Transl Res. 2022; 14(5): 3189-97.
pmid: 35702112 |
| 17 |
Zhang M, Wu LL, Deng YY, Peng F, Wang TT, Zhao YH, et al. Single cell dissection of epithelial-immune cellular interplay in acute kidney injury microenvironment. Front Immunol. 2022; 13: 857025.
doi: 10.3389/fimmu.2022.857025 |
| 18 |
You RL, Heyang ZG, Ma YX, Xia P, Zheng H, Lin JF, et al. Identification of biomarkers, immune infiltration landscape, and treatment targets of ischemia-reperfusion acute kidney injury at an early stage by bioinformatics methods. Hereditas. 2022; 159(1): 24.
doi: 10.1186/s41065-022-00236-x pmid: 35658960 |
| 19 |
Conway BR, O’Sullivan ED, Cairns C, O’Sullivan J, Simpson DJ, Salzano A, et al. Kidney single-cell atlas reveals myeloid heterogeneity in progression and regression of kidney disease. J Am Soc Nephrol. 2020; 31(12): 2833-54.
doi: 10.1681/ASN.2020060806 pmid: 32978267 |
| 20 |
Lee K, Jang HR. Role of T cells in ischemic acute kidney injury and repair. Korean J Intern Med. 2022; 37(3): 534-50.
doi: 10.3904/kjim.2021.526 pmid: 35508946 |
| 21 |
Rudman-Melnick V, Adam M, Potter A, Chokshi SM, Ma Q, Drake KA, et al. Single-cell profiling of AKI in a murine model reveals novel transcriptional signatures, profibrotic phenotype, and epithelial-to-stromal crosstalk. J Am Soc Nephrol. 2020; 31(12): 2793-814.
doi: 10.1681/ASN.2020010052 pmid: 33115917 |
| 22 |
Kaminski H, Couzi L, Eberl M. Unconventional T cells and kidney disease. Nat Rev Nephrol. 2021; 17(12): 795-813.
doi: 10.1038/s41581-021-00466-8 pmid: 34446934 |
| 23 |
Han L, Chen SY, Chen ZY, Zhou BQ, Zheng YX, Shen LS. Interleukin 32 promotes Foxp3+ treg cell development and CD8+ T cell function in human esophageal squamous cell carcinoma microenvironment. Front Cell Dev Biol. 2021; 9: 704853.
doi: 10.3389/fcell.2021.704853 |
| 24 |
Sharma R. Harnessing endogenous T-regulatory cells in acute kidney injury. Nephron. 2020; 144(12): 626-8.
doi: 10.1159/000508503 |
| 25 |
Sharma R, Kinsey GR. Regulatory T cells in acute and chronic kidney diseases. Am J Physiol Renal Physiol. 2018; 314(5): F679-F698.
doi: 10.1152/ajprenal.00236.2017 |
| 26 | Sidletskaya KA, Vitkina TI, Denisenko YK, Mineeva EE. Role of toll-like receptor 2 in regulation of T-helper immune response in chronic obstructive pulmonary disease. Can Respir J. 2021; 2021: 5596095. |
| [1] | Weichao Ding, Wei Zhang, Juan Chen, Mengmeng Wang, Yi Ren, Jing Feng, Xiaoqin Han, Xiaohang Ji, Shinan Nie, Zhaorui Sun. Protective mechanism of quercetin in alleviating sepsis-related acute respiratory distress syndrome based on network pharmacology and in vitro experiments [J]. World Journal of Emergency Medicine, 2024, 15(2): 111-120. |
| [2] | Wei Zhou, Maiying Fan, Xiang Li, Fang Yu, En Zhou, Xiaotong Han. Molecular mechanism of Xuebijing in treating pyogenic liver abscess complicated with sepsis [J]. World Journal of Emergency Medicine, 2024, 15(1): 35-40. |
| [3] | Jingyi Wang, Li Weng, Jun Xu, Bin Du. Blood gas analysis as a surrogate for microhemodynamic monitoring in sepsis [J]. World Journal of Emergency Medicine, 2023, 14(6): 421-427. |
| [4] | Saifeng Chen, Xuewei Hao, Guo Chen, Guorong Liu, Xiaoyan Yuan, Peiling Shen, Dongfeng Guo. Effects of mesencephalic astrocyte-derived neurotrophic factor on sepsis-associated acute kidney injury [J]. World Journal of Emergency Medicine, 2023, 14(5): 386-392. |
| [5] | Mubing Qin, Yanxia Gao, Shigong Guo, Xin Lu, Qian Zhao, Zengzheng Ge, Huadong Zhu, Yi Li. Establishment and evaluation of animal models of sepsis-associated encephalopathy [J]. World Journal of Emergency Medicine, 2023, 14(5): 349-353. |
| [6] | Meng-meng An, Chen-xi Liu, Ping Gong. Effects of continuous renal replacement therapy on inflammation-related anemia, iron metabolism and prognosis in sepsis patients with acute kidney injury [J]. World Journal of Emergency Medicine, 2023, 14(3): 186-192. |
| [7] | Jue-xian Wei, Hui-lin Jiang, Xiao-hui Chen. Endothelial cell metabolism in sepsis [J]. World Journal of Emergency Medicine, 2023, 14(1): 10-16. |
| [8] | Hui Liu, Jie Hu, Jian-guo Xiao, Hong-jun Kang, Fei-hu Zhou. The procalcitonin-to-cortisol ratio is a potential prognostic predictor in sepsis with abdominal source: a retrospective observational study [J]. World Journal of Emergency Medicine, 2022, 13(6): 441-447. |
| [9] | Ralph Bou Chebl, Nadim Kattouf, Mohamad Assaf, Saadeddine Haidar, Gilbert Abou Dagher, Sarah Abdul Nabi, Rana Bachir, Mazen El Sayed. Comparing the demographic data and outcomes of septic shock patients presenting to teaching or non-teaching metropolitan hospitals in the United States [J]. World Journal of Emergency Medicine, 2022, 13(6): 433-440. |
| [10] | Shi-yuan Yu, Zeng-zheng Ge, Jun Xiang, Yan-xia Gao, Xin Lu, Joseph Harold Walline, Mu-bing Qin, Hua-dong Zhu, Yi Li. Is rosuvastatin protective against sepsis-associated encephalopathy? A secondary analysis of the SAILS trial [J]. World Journal of Emergency Medicine, 2022, 13(5): 367-372. |
| [11] | A-ling Tang, Mei-jia Shen, Guo-qiang Zhang. Intestinal microcirculation dysfunction in sepsis: pathophysiology, clinical monitoring, and therapeutic interventions [J]. World Journal of Emergency Medicine, 2022, 13(5): 343-348. |
| [12] | Xiao-kang Dai, Zhen-xing Ding, Yuan-yuan Tan, Hua-rui Bao, Dong-yao Wang, Hong Zhang. Neutrophils inhibit CD8+ T cells immune response by arginase-1 signaling in patients with sepsis [J]. World Journal of Emergency Medicine, 2022, 13(4): 266-273. |
| [13] | Xuan Fu, Xue Lin, Samuel Seery, Li-na Zhao, Hua-dong Zhu, Jun Xu, Xue-zhong Yu. Speckle-tracking echocardiography for detecting myocardial dysfunction in sepsis and septic shock patients: A single emergency department study [J]. World Journal of Emergency Medicine, 2022, 13(3): 175-181. |
| [14] | Mei-jia Shen, Li-chao Sun, Xiao-yu Liu, Meng-chen Xiong, Shan Li, A-ling Tang, Guo-qiang Zhang. Trichostatin A improves the inflammatory response and liver injury in septic mice through the FoxO3a/autophagy signaling pathway [J]. World Journal of Emergency Medicine, 2022, 13(3): 182-188. |
| [15] | Cheng Hang, Li-jun Liu, Zhao-yun Huang, Jian-liang Zhu, Bao-chun Zhou, Xiao-zhen Li. Optimal indicator for changing the filter during the continuous renal replacement therapy in intensive care unit patients with acute kidney injury: A crossover randomized trial [J]. World Journal of Emergency Medicine, 2022, 13(3): 196-201. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
