World Journal of Emergency Medicine ›› 2023, Vol. 14 ›› Issue (4): 265-272.doi: 10.5847/wjem.j.1920-8642.2023.070
• Original Article • Previous Articles Next Articles
Qiang Zhou1, Xuejie Dong2, Wei Zhang3, Rengyu Wu1, Kaizhu Chen1, Hongjuan Zhang1, Zhijie Zheng2, Lin Zhang4,5( )
)
Received:2022-10-28
Accepted:2023-02-20
Online:2023-06-30
Published:2023-07-01
Contact:
Lin Zhang
E-mail:zhanglynn@sjtu.edu.cn
Qiang Zhou, Xuejie Dong, Wei Zhang, Rengyu Wu, Kaizhu Chen, Hongjuan Zhang, Zhijie Zheng, Lin Zhang. Effect of a low-cost instruction card for automated external defibrillator operation in lay rescuers: a randomized simulation study[J]. World Journal of Emergency Medicine, 2023, 14(4): 265-272.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2023.070
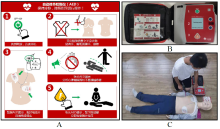
Figure 1.
The illustration of AED self-instruction card in use. A: design of the AED self-instruction card; ① turn on AED immediately; ② fully bare the chest; ③ correctly place electrodes and then plug the connector into the AED; ④ keep clear when analyzing the rhythm and delivering shock and ⑤ click the button and resume CPR after shock. B: illustration of the placement of self-instruction card in the AED pocket.C: illustration of rescuer using AED with the self-instruction card in simulated cardiac arrest scenario. AED: automated external defibrillator; CPR: cardiopulmonary resuscitation.

Table 1.
Demographic characteristics of participants
| Characteristics | Baseline and post-training | 3-month follow-up | |||||
|---|---|---|---|---|---|---|---|
| Card group (n=83) | Control group (n=82) | P-value | Card group (n=75) | Control group (n=77) | P-value | ||
| Male, n (%) | 38 (45.8) | 37 (45.1) | 0.71 | 36 (48.0) | 36 (46.7) | 0.91 | |
| Age group, n (%) | 0.89 | 0.78 | |||||
| 18-24 years | 30 (45.8) | 29 (35.4) | 29 (38.7) | 28 (36.4) | |||
| 25-54 years | 29 (34.9) | 30 (36.6) | 24 (32.0) | 29 (37.7) | |||
| 55-65 years | 24 (28.9) | 23 (28.0) | 22 (29.3) | 20 (26.0) | |||
| Education status, n (%) | 0.26 | 0.19 | |||||
| High school/ Junior college and below | 37 (44.6) | 27 (32.9) | 33 (44.0) | 26 (33.8) | |||
| College/ University | 40 (48.2) | 44 (53.6) | 36 (48.0) | 42 (54.5) | |||
| Master and above | 6 (7.2) | 11 (13.4) | 6 (8.0) | 9 (11.7) | |||
Table 2.
Comparison of laypeople AED operation skills between card group and control group, n (%)
| Operation skills | Total | 18-24 years | 25-54 years | 55-65 years | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Card group | Control group | P-valuec | Card group | Control group | P-value | Card group | Control group | P-value | Card group | Control group | P-value | |||||
| Fully baring the chest | ||||||||||||||||
| Baseline a | 72 (88.9) | 52 (63.4) | <0.001 | 27 (90.0) | 24 (82.8) | 0.47 | 26 (89.7) | 22 (73.3) | 0.11 | 19 (79.2) | 6 (26.1) | <0.001 | ||||
| Post-training a | 83 (100) | 82 (100) | - | 30 (100) | 29 (100) | - | 29 (100) | 30 (100) | - | 24 (100) | 23 (100) | - | ||||
| Follow-up b | 61 (96.8) | 71 (92.2) | 0.29 | 29 (100) | 27 (96.4) | 0.49 | 12 (100) | 27 (93.1) | 1.0 | 20 (90.9) | 17 (85.0) | 0.66 | ||||
| Correct electrodes placement | ||||||||||||||||
| Baseline | 27 (32.5) | 14 (17.1) | 0.03 | 13 (43.3) | 9 (31.0) | 0.33 | 9 (31.0) | 3 (10.0) | 0.04 | 5 (20.8) | 2 (8.7) | 0.42 | ||||
| Post-training | 63 (75.9) | 61 (74.4) | 0.82 | 25 (83.3) | 23 (79.3) | 0.69 | 22 (75.9) | 21 (70.0) | 0.61 | 16 (66.7) | 17 (73.9) | 0.59 | ||||
| Follow-up | 37 (58.7) | 36 (46.8) | 0.16 | 18 (62.1) | 15 (53.6) | 0.52 | 7 (58.3) | 18 (62.1) | 1.0 | 12 (54.5) | 3 (15.0) | 0.01 | ||||
| Clearing while AED analyzes the rhythm | ||||||||||||||||
| Baseline | 70 (84.3) | 63 (76.8) | 0.22 | 27 (90.0) | 24 (82.8) | 0.47 | 23 (79.3) | 23 (76.7) | 0.81 | 20 (83.3) | 16 (69.6) | 0.32 | ||||
| Post-training | 81 (97.6) | 74 (90.2) | 0.06 | 30 (100) | 25 (86.2) | 0.035 | 28 (96.6) | 28 (93.3) | 1.0 | 23 (95.8) | 21 (91.3) | 0.61 | ||||
| Follow-up | 62 (98.4) | 71 (92.2) | 0.13 | 29 (100) | 25 (89.3) | 0.11 | 12 (100) | 29 (100) | - | 21 (95.5) | 17 (85.0) | 0.33 | ||||
| Clearing while AED delivers the shock | ||||||||||||||||
| Baseline | 78 (94.0) | 75 (91.5) | 0.57 | 28 (93.3) | 28 (96.6) | 1.0 | 28 (96.6) | 29 (96.7) | 1.0 | 22 (91.7) | 18 (78.3) | 0.25 | ||||
| Post-training | 82 (98.8) | 81 (98.8) | 1.0 | 30 (100) | 29 (100) | - | 28 (96.6) | 30 (100) | 0.49 | 24 (100) | 22 (95.7) | 0.49 | ||||
| Follow-up | 63 (100) | 74 (96.1) | 0.25 | 29 (100) | 28 (100) | - | 12 (100) | 29 (100) | - | 22 (100) | 17 (85.0) | 0.10 | ||||
| Successful defibrillation d | ||||||||||||||||
| Baseline | 26 (31.1) | 13 (15.9) | 0.03 | 13 (43.3) | 8 (27.6) | 0.21 | 8 (27.6) | 3 (10.0) | 0.08 | 5 (20.8) | 2 (8.7) | 0.42 | ||||
| Post-training | 63 (75.9) | 61 (74.4) | 0.83 | 25 (83.3) | 23 (79.3) | 0.69 | 22 (75.9) | 21 (70.0) | 0.61 | 16 (66.7) | 17 (73.9) | 0.59 | ||||
| Follow-up | 37 (58.7) | 36 (46.8) | 0.16 | 18 (62.1) | 15 (53.6) | 0.52 | 7 (58.3) | 18 (62.1) | 1.0 | 12 (54.5) | 3 (15.0) | 0.01 | ||||
| Resuming CPR after shock | ||||||||||||||||
| Baseline | 60 (72.3) | 8 (9.8) | <0.001 | 18 (60.0) | 3 (10.3) | <0.001 | 23 (79.3) | 3 (10.0) | <0.001 | 19 (79.2) | 2 (8.7) | <0.001 | ||||
| Post-training | 83 (100) | 71 (86.6) | 0.001 | 30 (100) | 26 (89.7) | 0.11 | 29 (100) | 26 (86.7) | 0.11 | 24 (100) | 19 (82.6) | 0.13 | ||||
| Follow-up | 62 (98.4) | 44 (57.1) | <0.001 | 29 (100) | 20 (71.4) | 0.002 | 12 (100) | 21 (72.4) | 0.08 | 21 (95.5) | 3 (15.0) | <0.001 | ||||
Table 3.
Comparison of time intervals in successful defibrillation between card group and control group by age, s, M(P25-P75)
| Variables | Total | 18-24 years | 25-54 years | 55-65 years | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Card group | Control group | P-value | Card group | Control group | P-value | Card group | Control group | P-value | Card group | Control group | P-value | |||||||||||||
| n | Time intervals | n | Time intervals | n | Time intervals | n | Time intervals | n | Time intervals | n | Time intervals | n | Time intervals | n | Time intervals | |||||||||
| Time to power-on a | ||||||||||||||||||||||||
| Baseline | 26 | 35 (18-89) | 13 | 51 (17-107) | 0.79 | 13 | 74 (34-109) | 8 | 80 (42-172) | 0.45 | 8 | 21 (14-78) | 3 | 23 (12-72) | 0.83 | 5 | 18 (10-30) | 2 | 18, 39 | 0.33 | ||||
| Post-training | 63 | 28 (11-48) | 61 | 22 (11-51) | 0.96 | 25 | 36 (16-50) | 23 | 29 (11-52) | 0.48 | 22 | 34 (17-44) | 21 | 17 (9-43) | 0.08 | 16 | 9 (6-14) | 17 | 33 (12-58) | 0.019 | ||||
| Follow-up | 37 | 36 (17-52) | 36 | 28 (16-50) | 0.49 | 18 | 40 (20-52) | 15 | 31 (19-53) | 0.72 | 7 | 54 (35-71) | 18 | 31 (17-50) | 0.07 | 12 | 27 (9-38) | 3 | 15 (10-31) | 0.67 | ||||
| Time to shock a | ||||||||||||||||||||||||
| Baseline | 26 | 113 (92-146) | 13 | 107 (101-131) | 0.25 | 13 | 125 (113-171) | 8 | 129 (103-198) | 0.72 | 8 | 91 (80-140) | 3 | 109 (102-122) | 0.38 | 5 | 95 (72-112) | 2 | 85, 92 | 1 | ||||
| Post-training | 63 | 72 (63-78) | 61 | 80 (69-88) | <0.001 | 25 | 75 (66-80) | 23 | 74 (64-88) | 0.59 | 22 | 68 (63-78) | 21 | 81 (70-90) | 0.009 | 16 | 65 (56-74) | 17 | 79 (77-86) | 0.001 | ||||
| Follow-up | 37 | 74 (66-87) | 36 | 80 (71-94) | 0.05 | 18 | 76 (68-83) | 15 | 81 (69-92) | 0.31 | 7 | 100 (77-143) | 18 | 78 (69-93) | 0.05 | 12 | 68 (60-74) | 3 | 92 (75-106) | 0.006 | ||||
| Time to resume CPR after shock b | ||||||||||||||||||||||||
| Baseline | 23 | 10 (7-13) | 5 | 12 (11-15) | 0.06 | 10 | 8 (5-13) | 2 | 10, 11 | 0.39 | 8 | 13 (10-14) | 2 | 12, 15 | 0.60 | 5 | 8 (5-10) | 1 | 16 | 0.14 | ||||
| Post-training | 63 | 7 (3-10) | 51 | 10 (8-11) | <0.001 | 25 | 4 (2-8) | 16 | 9 (6-10) | 0.003 | 22 | 10 (6-11) | 21 | 9.5 (8-11) | 0.87 | 16 | 6 (3-9) | 14 | 10 (7-12) | 0.002 | ||||
| Follow-up | 36 | 9 (8-12) | 27 | 9 (7-12) | 0.33 | 18 | 11 (9-14) | 10 | 8 (6-19) | 0.36 | 7 | 9 (8-16) | 16 | 9 (8-12) | 0.66 | 11 | 9 (8-10) | 1 | 9 | 0.88 | ||||
| 1 |
Bækgaard JS, Viereck S, Møller TP, Ersbøll AK, Lippert F, Folke F. The effects of public access defibrillation on survival after out-of-hospital cardiac arrest: a systematic review of observational studies. Circulation. 2017; 136(10): 954-65.
doi: 10.1161/CIRCULATIONAHA.117.029067 pmid: 28687709 |
| 2 |
Deakin CD. The chain of survival: not all links are equal. Resuscitation. 2018; 126: 80-2.
doi: S0300-9572(18)30080-7 pmid: 29471008 |
| 3 |
Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, Olasveengen T, et al. European Resuscitation Council Guidelines for Resuscitation 2015: section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015; 95: 81-99.
doi: 10.1016/j.resuscitation.2015.07.015 pmid: 26477420 |
| 4 | Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(18 Suppl 2): S414-S435. |
| 5 |
Agerskov M, Nielsen AM, Hansen CM, Hansen MB, Lippert FK, Wissenberg M, et al. Public access defibrillation: great benefit and potential but infrequently used. Resuscitation. 2015; 96: 53-8.
doi: 10.1016/j.resuscitation.2015.07.021 pmid: 26234893 |
| 6 |
Deakin CD, Shewry E, Gray HH. Public access defibrillation remains out of reach for most victims of out-of-hospital sudden cardiac arrest. Heart. 2014; 100(8): 619-23.
doi: 10.1136/heartjnl-2013-305030 pmid: 24553390 |
| 7 |
Kitamura T, Kiyohara K, Sakai T, Matsuyama T, Hatakeyama T, Shimamoto T, et al. Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med. 2016; 375(17): 1649-59.
doi: 10.1056/NEJMsa1600011 |
| 8 |
Hawkes C, Booth S, Ji C, Brace-McDonnell SJ, Whittington A, Mapstone J, et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation. 2017; 110: 133-40.
doi: S0300-9572(16)30547-0 pmid: 27865775 |
| 9 |
Dong XJ, Zhang L, Yu YL, Shi SX, Yang XC, Zhang XQ, et al. The general public’s ability to operate automated external defibrillator: a controlled simulation study. World J Emerg Med. 2020; 11(4): 238-45.
doi: 10.5847/wjem.j.1920-8642.2020.04.006 |
| 10 |
Yeung J, Okamoto D, Soar J, Perkins GD. AED training and its impact on skill acquisition, retention and performance - A systematic review of alternative training methods. Resuscitation. 2011; 82(6): 657-64.
doi: 10.1016/j.resuscitation.2011.02.035 |
| 11 |
Maes F, Marchandise S, Boileau L, Le Polain de Waroux JB, Scavée C. Evaluation of a new semiautomated external defibrillator technology: a live cases video recording study. Emerg Med J. 2015; 32(6): 481-5.
doi: 10.1136/emermed-2013-202962 pmid: 25082717 |
| 12 |
Foster AG, Deakin CD. Accuracy of instructional diagrams for automated external defibrillator pad positioning. Resuscitation. 2019; 139: 282-8.
doi: S0300-9572(19)30150-9 pmid: 31063839 |
| 13 | Carballo-Fazanes A, Jorge-Soto C, Abelairas-Gómez C, Bello-Rodríguez J, Fernández-Méndez F, Rodríguez-Núñez A. Could mobile apps improve laypeople AED use? Resuscitation. 2019;140: 159-60. |
| 14 |
Andersen LW, Holmberg MJ, Granfeldt A, James LP, Caulley L. Cost-effectiveness of public automated external defibrillators. Resuscitation. 2019; 138: 250-8.
doi: S0300-9572(19)30097-8 pmid: 30926453 |
| 15 | Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, et al. European Resuscitation Council Guidelines for Resuscitation 2015: section 3. Adult advanced life support. Resuscitation. 2015;95: 100-47. |
| 16 |
Mosesso VN Jr, Shapiro AH, Stein K, Burkett K, Wang H. Effects of AED device features on performance by untrained laypersons. Resuscitation. 2009; 80(11): 1285-9.
doi: 10.1016/j.resuscitation.2009.07.016 pmid: 19720444 |
| 17 |
Roccia WD, Modic PE, Cuddy MA. Automated external defibrillator use among the general population. J Dent Educ. 2003; 67(12): 1355-61.
pmid: 14733268 |
| 18 |
Bødtker H, Rosendahl D. Automated external defibrillators and defibrillation electrodes from major manufactures depict placement of the left apical defibrillation electrode poorly!. Resuscitation. 2018; 125: e11-e12.
doi: 10.1016/j.resuscitation.2018.01.046 |
| 19 |
Bødtker H, Rosendahl D. Correct AED electrode placement is rarely achieved by laypersons when attaching AED electrodes to a human thorax. Resuscitation. 2018; 127: e12-e13.
doi: 10.1016/j.resuscitation.2018.04.002 |
| 20 |
Kiyohara K, Kitamura T, Sakai T, Nishiyama C, Nishiuchi T, Hayashi Y, et al. Public-access AED pad application and outcomes for out-of-hospital cardiac arrests in Osaka, Japan. Resuscitation. 2016; 106: 70-5.
doi: 10.1016/j.resuscitation.2016.06.025 pmid: 27373223 |
| 21 |
Savastano S, Vanni V, Burkart R, Raimondi M, Canevari F, Molinari S, et al. Comparative performance assessment of commercially available automatic external defibrillators: a simulation and real-life measurement study of hands-off time. Resuscitation. 2017; 110: 12-7.
doi: S0300-9572(16)30509-3 pmid: 27780740 |
| 22 |
Nurmi J, Castrén M. Layperson positioning of defibrillation electrodes guided by pictorial instructions. Resuscitation. 2005; 64(2): 177-80.
pmid: 15680526 |
| 23 |
Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010; 3(1): 63-81.
doi: 10.1161/CIRCOUTCOMES.109.889576 |
| 24 |
Ringh M, Hollenberg J, Palsgaard-Moeller T, Svensson L, Rosenqvist M, Lippert FK, et al. The challenges and possibilities of public access defibrillation. J Intern Med. 2018; 283(3): 238-56.
doi: 10.1111/joim.12730 pmid: 29331055 |
| 25 |
Zhang L, Li BY, Zhao XF, Zhang YQ, Deng YT, Zhao AQ, et al. Public access of automated external defibrillators in a metropolitan city of China. Resuscitation. 2019; 140: 120-6.
doi: S0300-9572(19)30184-4 pmid: 31129230 |
| 26 | Medicine CSoE. Expert consensus on AED layout and launch in China. Chin J Emerg Med. 2020; 29(8):1025-31. |
| 27 | Global Resuscitation Alliance. Public Access Defibrillation Program in Shenzhen, China. Ten Programs. Available at: https://www.globalresuscitationalliance.org/wp-content/uploads/2019/12/China_PAD.pdf |
| 28 |
Lei CY, Qin HW, Dong XJ, You JL, Zhang L. Layperson’s performance on an unconversant type of AED device: a prospective crossover simulation experimental study. World J Emerg Med. 2022; 13(2): 98-105.
doi: 10.5847/wjem.j.1920-8642.2022.024 |
| [1] | Chao-yu Lei, Heng-wei Qin, Xue-jie Dong, Jia-lin You, Lin Zhang. Layperson’s performance on an unconversant type of AED device: A prospective crossover simulation experimental study [J]. World Journal of Emergency Medicine, 2022, 13(2): 98-105. |
| [2] | Xin Lu, Shi Feng, Shi-gong Guo, Mu-bing Qin, Xiang-ning Liu, Shi-yuan Yu, Li-na Zhao, Zeng-zheng Ge, Jing-jing Chai, Sheng-yong Xu, Di Shi, Ji-hai Liu, Hua-dong Zhu, Yi Li. Development of an intensive simulating training program in emergency medicine for medical students in China [J]. World Journal of Emergency Medicine, 2022, 13(1): 23-26. |
| [3] | Ryan W. Horton, Kian R. Niknam, Viveta Lobo, Kathryn H. Pade, Drew Jones, Kenton L. Anderson. A cadaveric model for transesophageal echocardiography transducer placement training: A pilot study [J]. World Journal of Emergency Medicine, 2022, 13(1): 18-22. |
| [4] | Xue-jie Dong, Lin Zhang, Yue-lin Yu, Shu-xiao Shi, Xiao-chen Yang, Xiao-qian Zhang, Shuang Tian, Helge Myklebust, Guo-hong Li, Zhi-jie Zheng. The general public’s ability to operate automated external defibrillator: A controlled simulation study [J]. World Journal of Emergency Medicine, 2020, 11(4): 238-245. |
| [5] | Avir Mitra, Asaf Gave, Kelsey Coolahan, Thomas Nguyen. Confirmation of endotracheal tube placement using disposable fiberoptic bronchoscopy in the emergent setting [J]. World Journal of Emergency Medicine, 2019, 10(4): 210-214. |
| [6] | Israel Olatunji Gabriel, Joel O. Aluko. Theoretical knowledge and psychomotor skill acquisition of basic life support training programme among secondary school students [J]. World Journal of Emergency Medicine, 2019, 10(2): 81-87. |
| [7] | Mario Kobras, Sascha Langewand, Christina Murr, Christiane Neu, Jeannette Schmid. Short lessons in basic life support improve self-assurance in performing cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2016, 7(4): 255-262. |
| [8] | Chik Leung Ho, Ka Wai Cheng, Tze Hang Ma, Yau Hang Wong, Ka Lok Cheng, Chak Wah Kam. Characterization of available automated external defibrillators in the market based on the product manuals in 2014 [J]. World Journal of Emergency Medicine, 2016, 7(2): 138-146. |
| [9] | Endale Gebreegziabher, Adugna Aregawi, Habtamu Getinet. Knowledge and skills of neonatal resuscitation of health professionals at a university teaching hospital of Northwest Ethiopia [J]. World Journal of Emergency Medicine, 2014, 5(3): 196-202. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
