World Journal of Emergency Medicine ›› 2022, Vol. 13 ›› Issue (3): 189-195.doi: 10.5847/wjem.j.1920-8642.2022.040
• Original Articles • Previous Articles Next Articles
Peng-chao Guo1, Nan Li2( ), Hui-ming Zhong1, Guang-feng Zhao1
), Hui-ming Zhong1, Guang-feng Zhao1
Received:2021-08-29
Accepted:2022-01-10
Online:2022-05-13
Published:2022-05-01
Contact:
Nan Li
E-mail:2515141@zju.edu.cn
Peng-chao Guo, Nan Li, Hui-ming Zhong, Guang-feng Zhao. Clinical effectiveness of a pneumatic compression device combined with low-molecular-weight heparin for the prevention of deep vein thrombosis in trauma patients: A single-center retrospective cohort study[J]. World Journal of Emergency Medicine, 2022, 13(3): 189-195.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2022.040

Figure 1.
Comparison of PLT, FIB, PT, and APTT between groups. Compared with before surgery within the two groups, *P<0.05; compared with after surgery between the two groups, #P<0.05. PLT: platelet; FIB: fibrinogen; PT: plasma prothrombin time; APTT: plasma activated partial thromboplastin time.
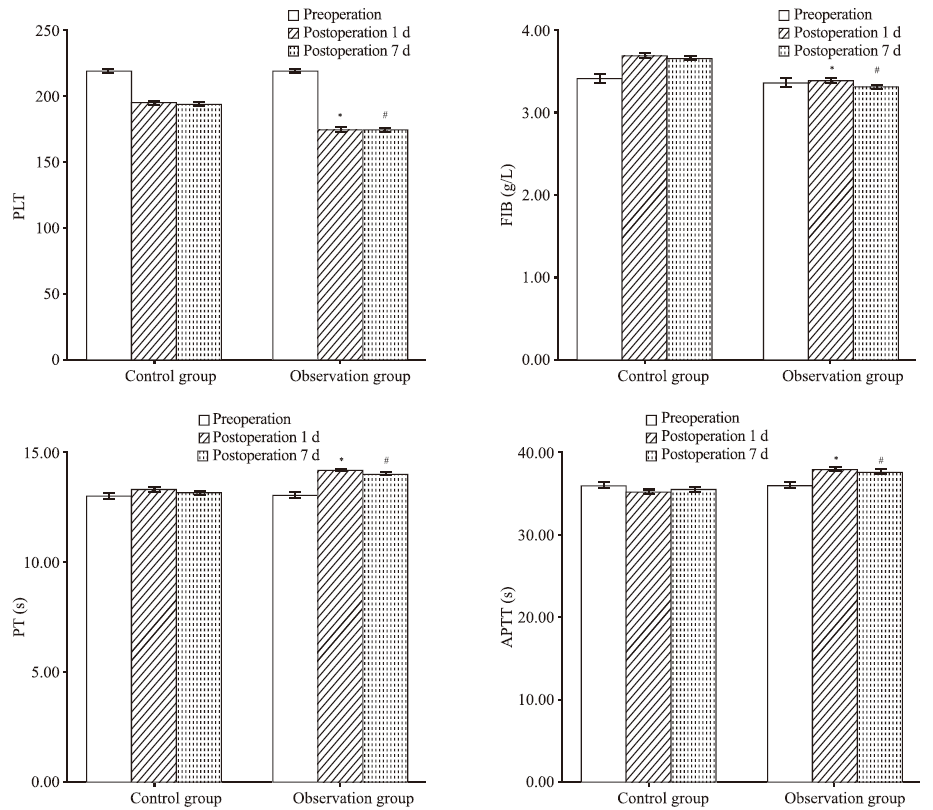
Table 1.
Comparison of basic data between groups
| Variables | Control group (n=126) | Observation group (n=126) | t/Z/χ2 | P-value |
|---|---|---|---|---|
| Sex Female, n (%) Male, n (%) | 59 (46.8) | 72 (57.1) | 0.910a | 0.340 |
| 67 (53.2) | 54 (42.9) | |||
| Age, years, mean±SD | 48.3±6.4 | 53.7±5.9 | 0.219b | 0.873 |
| Hypertension, n | 21 (16.7) | 24 (19.1) | 0.311a | 0.771 |
| Diabetes, n | 7 (5.6) | 6 (4.8) | 1.279a | 0.204 |
| Antiplatelet therapy, n | 13 (10.3) | 14 (11.1) | 0.584a | 0.445 |
| Oral anticoagulant, n | 15 (11.9) | 11 (8.7) | 0.727a | 0.469 |
| Caprini risk scores, n High risk (3-4) Highest risk (≥5) | 59 (46.8) 67 (53.2) | 53 (42.1) 73 (57.9) | -0.759a | 0.448 |
| Glasgow Coma Scale score, n 13 14 15 | 22 (17.5) 31 (24.6) | 26 (20.6) 29 (23.1) | -0.408c | 0.684 |
| 73 (57.9) | 71 (56.3) | |||
| Clavicle fracture type, n Mid fracture Acromion fracture | 74 (58.7) 52 (41.3) | 87 (69.1) 39 (30.9) | -1.702a | 0.089 |
Table 2.
Multivariate logistic regression analysis results of DVT in trauma patients
| Variables | β | S.E. | Wald | Sig. | OR | 95% CI |
|---|---|---|---|---|---|---|
| Sex | 0.505 | 0.463 | 1.189 | 0.276 | 1.657 | 0.669-4.106 |
| Age | -0.016 | 0.015 | 1.075 | 0.300 | 0.984 | 0.955-1.014 |
| Baseling disease | -0.117 | 0.555 | 0.045 | 0.833 | 0.889 | 0.300-2.638 |
| Caprini risk score | 0.017 | 0.088 | 0.039 | 0.844 | 1.017 | 0.856-1.210 |
| Length of stay | 0.121 | 0.082 | 2.189 | 0.139 | 1.129 | 0.961-1.325 |
| GCS | 0.156 | 0.279 | 0.314 | 0.576 | 1.169 | 0.676-2.021 |
| Blood loss | 0.006 | 0.017 | 0.130 | 0.719 | 1.006 | 0.973-1.041 |
| Drugs | 0.300 | 0.806 | 0.139 | 0.709 | 1.350 | 0.278-6.550 |
| APTT | 0.032 | 0.052 | 0.379 | 0.538 | 1.033 | 0.932-1.144 |
| PLT | -0.016 | 0.010 | 2.785 | 0.095 | 0.984 | 0.965-1.003 |
| PCD | 1.764 | 0.598 | 8.701 | 0.003* | 5.833 | 1.807-18.828 |
| Fracture type | -0.145 | 0.507 | 0.081 | 0.775 | 0.865 | 0.321-2.335 |
Table 3.
ROC curve analysis of variables in the prevention of deep vein thrombosis by PCD
| Variables | Cut-off | Sensitivity | Specificity | Youden Index | AUC (95% CI) | P-value |
|---|---|---|---|---|---|---|
| APTT | 37.5 s | 0.849 | 0.857 | 0.378 | 0.628 (0.407-0.849) | <0.05 |
| Caprini risk score | 6.5 | 0.454 | 0.286 | 0.168 | 0.520 (0.291-0.750) | 0.257 |
| Length of stay | 7.5 d | 0.429 | 0.286 | 0.143 | 0.466 (0.248-0.683) | 0.602 |
| GCS | 13.5 | 0.647 | 0.857 | -0.210 | 0.354 (0.156-0.552) | 0.196 |
| Blood loss | 35.5 mL | 0.387 | 0.286 | 0.101 | 0.441 (0.256-0.627) | 0.076 |
| Infection rate | 38.85% | 0.244 | 0.429 | -0.185 | 0.297 (0.076-0.518) | 0.072 |
| PLT | 124×109/L | 0.924 | 0.571 | 0.353 | 0.700 (0.495-0.904) | <0.05 |
| 1 |
Mesa Galan LA, Egea-Guerrero JJ, Quintana Diaz M, Vilches-Arenas A. The effectiveness and safety of pharmacological prophylaxis against venous thromboembolism in patients with moderate to severe traumatic brain injury: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2016; 81(3):567-74.
doi: 10.1097/TA.0000000000001134 |
| 2 |
Ginzburg E, Cohn SM, Lopez J, Jackowski J, Brown M, Hameed SM, et al. Randomized clinical trial of intermittent pneumatic compression and low molecular weight heparin in trauma. Br J Surg. 2003; 90(11):1338-44.
doi: 10.1002/bjs.4309 |
| 3 |
Selby R, Geerts W, Ofosu FA, Craven S, Dewar L, Phillips A, et al. Hypercoagulability after trauma: hemostatic changes and relationship to venous thromboembolism. Thromb Res. 2009; 124(3):281-7.
doi: 10.1016/j.thromres.2008.10.002 pmid: 19041119 |
| 4 |
Moumneh T, Riou J, Douillet D, Henni S, Mottier D, Tritschler T, et al. Validation of risk assessment models predicting venous thromboembolism in acutely ill medical inpatients: a cohort study. J Thromb Haemost. 2020; 18(6):1398-407.
doi: 10.1111/jth.14796 pmid: 32168402 |
| 5 | Mehta R, Chinthapalli K. Glasgow Coma Scale explained. BMJ. 2019; 365:l1296. |
| 6 |
Williams DH, Levin HS, Eisenberg HM. Mild head injury classification. Neurosurgery. 1990; 27(3):422-8.
doi: 10.1097/00006123-199009000-00014 pmid: 2234336 |
| 7 |
Kane RL, Bershadsky B, Rockwood T, Saleh K, Islam NC. Visual analog scale pain reporting was standardized. J Clin Epidemiol. 2005; 58(6):618-23.
doi: 10.1016/j.jclinepi.2004.11.017 |
| 8 |
Fröhlich M, Lefering R, Probst C, Paffrath T, Schneider MM, Maegele M, et al. Epidemiology and risk factors of multiple-organ failure after multiple trauma: an analysis of 31,154 patients from the trauma register DGU. J Trauma Acute Care Surg. 2014; 76(4):921-7; discussion 927-8.
doi: 10.1097/TA.0000000000000199 |
| 9 |
Ropars M, Thomazeau H, Huten D. Clavicle fractures. Orthop Traumatol Surg Res. 2017; 103(1S):S53-9.
doi: 10.1016/j.otsr.2016.11.007 |
| 10 |
Khorana AA. Risk assessment for cancer-associated VTE: diversifying the evidence base. JACC: Asia. 2021; 1(2):271-3.
doi: 10.1016/j.jacasi.2021.07.007 |
| 11 |
Eppsteiner RW, Shin JJ, Johnson J, van Dam RM. Mechanical compression versus subcutaneous heparin therapy in postoperative and posttrauma patients: a systematic review and meta-analysis. World J Surg. 2010; 34(1):10-9.
doi: 10.1007/s00268-009-0284-z pmid: 20020289 |
| 12 |
Jenkins R, Morris NA, Haac B, Besien RV, Stein DM, Badjatia N, et al. Outcome predictors for severely brain-injured patients directly admitted or transferred from emergency departments to a trauma center. World J Emerg Med. 2020; 11(2):120-1.
doi: 10.5847/wjem.j.1920-8642.2020.02.010 pmid: 32076479 |
| 13 | Bilotta F, Rosa G. Saline or albumin for fluid resuscitation in traumatic brain injury. N Engl J Med. 2007; 357(25):2635. |
| 14 | Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia:recognition, treatment, and prevention:the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126(3 Suppl):311S-37S. |
| 15 |
Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004; 350(22):2257-64.
doi: 10.1056/NEJMoa032274 |
| 16 |
Reed CR, Ferguson RA, Peng YM, Collier BR, Bradburn EH, Toms AR, et al. Contact isolation is a risk factor for venous thromboembolism in trauma patients. J Trauma Acute Care Surg. 2015; 79(5): 833-7.
doi: 10.1097/TA.0000000000000835 |
| 17 |
Haut ER, Garcia LJ, Shihab HM, Brotman DJ, Stevens KA, Sharma R, et al. The effectiveness of prophylactic inferior vena cava filters in trauma patients. JAMA Surg. 2014; 149(2):194.
doi: 10.1001/jamasurg.2013.3970 |
| 18 | Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS; Bratton SL, Chestnut RM, et al. Guidelines for the management of severe traumatic brain injury. V. deep vein thrombosis prophylaxis. J Neurotrauma. 2007; 24 Suppl 1:S32-6. |
| 19 |
Phelan HA. Pharmacologic venous thromboembolism prophylaxis after traumatic brain injury: a critical literature review. J Neurotrauma. 2012; 29(10):1821-8.
doi: 10.1089/neu.2012.2459 |
| 20 |
Che XR, Wang YJ, Zheng HY. Prognostic value of intracranial pressure monitoring for the management of hypertensive intracerebral hemorrhage following minimally invasive surgery. World J Emerg Med. 2020; 11(3):169-73.
doi: 10.5847/wjem.j.1920-8642.2020.03.007 |
| 21 |
Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited. Lancet. 2009; 373(9658):155-66.
doi: 10.1016/S0140-6736(09)60040-4 |
| 22 |
Theusinger OM, Baulig W, Seifert B, Müller SM, Mariotti S, Spahn DR. Changes in coagulation in standard laboratory tests and ROTEM in trauma patients between on-scene and arrival in the emergency department. Anesth Analg. 2015; 120(3):627-35.
doi: 10.1213/ANE.0000000000000561 pmid: 25545751 |
| 23 |
Chiasson TC, Manns BJ, Stelfox HT. An economic evaluation of venous thromboembolism prophylaxis strategies in critically ill trauma patients at risk of bleeding. PLoS Med. 2009; 6(6):e1000098.
doi: 10.1371/journal.pmed.1000098 |
| 24 |
Jacobs BN, Cain-Nielsen AH, Jakubus JL, Mikhail JN, Fath JJ, Regenbogen SE, et al. Unfractionated heparin versus low-molecular-weight heparin for venous thromboembolism prophylaxis in trauma. J Trauma Acute Care Surg. 2017; 83(1):151-8.
doi: 10.1097/TA.0000000000001494 |
| 25 |
DiGiorgio AM, Tsolinas R, Alazzeh M, Haefeli J, Talbott JF, Ferguson AR, et al. Safety and effectiveness of early chemical deep venous thrombosis prophylaxis after spinal cord injury: pilot prospective data. Neurosurg Focus. 2017; 43(5):E21.
doi: 10.3171/2017.8.FOCUS17437 |
| 26 |
Geerts WH, Jay RM, Code KI, Chen E, Szalai JP, Saibil EA, et al. A comparison of low-dose heparin with low-molecular-weight heparin as prophylaxis against venous thromboembolism after major trauma. N Engl J Med. 1996; 335(10):701-7.
doi: 10.1056/NEJM199609053351003 |
| 27 |
Zacà V, Marcucci R, Parodi G, Limbruno U, Notarstefano P, Pieragnoli P, et al. Management of antithrombotic therapy in patients undergoing electrophysiological device surgery. Europace. 2015; 17(6):840-54.
doi: 10.1093/europace/euu357 |
| 28 |
Droege ME, Mueller EW, Besl KM, Lemmink JA, Kramer EA, Athota KP, et al. Effect of a dalteparin prophylaxis protocol using anti-factor Xa concentrations on venous thromboembolism in high-risk trauma patients. J Trauma Acute Care Surg. 2014; 76(2):450-6.
doi: 10.1097/TA.0000000000000087 pmid: 24458050 |
| 29 |
Kurtoglu M, Yanar H, Bilsel Y, Guloglu R, Kizilirmak S, Buyukkurt D, et al. Venous thromboembolism prophylaxis after head and spinal trauma: intermittent pneumatic compression devices versus low molecular weight heparin. World J Surg. 2004; 28(8):807-11.
pmid: 15457363 |
| 30 | Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P. Antithrombotic and thrombolytic therapy for ischemic stroke:American College of Chest Physicians Evidence-based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133(6 Suppl): 630S-69S. |
| 31 |
Cushman JG, Agarwal N, Fabian TC, Garcia V, Nagy KK, Pasquale MD, et al. Practice management guidelines for the management of mild traumatic brain injury: the EAST practice management guidelines work group. J Trauma. 2001; 51(5):1016-26.
doi: 10.1097/00005373-200111000-00034 |
| 32 |
Kearon C, Akl EA, Comerota AJ, Prandoni P, Kahn SR. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th Ed: American College of Chest Physicians Evidence-based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e419S-94S.
doi: 10.1378/chest.11-2301 |
| [1] | Li-wen Dou, Zhe Du, Ji-hong Zhu, Tian-bing Wang. Changes and significance of serum troponin in trauma patients: A retrospective study in a level I trauma center [J]. World Journal of Emergency Medicine, 2022, 13(1): 27-31. |
| [2] | Patrizio Petrone, Sofía Espinoza-Villalobos, Gerard A. Baltazar, Kjetil Søreide, Adam Stright, Collin E.M. Brathwaite, D’Andrea K. Joseph. Fatal and non-fatal injuries due to suspension trauma syndrome: A systematic review of definition, pathophysiology, and management controversies [J]. World Journal of Emergency Medicine, 2021, 12(4): 253-260. |
| [3] | Gui-long Feng, Miao-miao Zheng, Shi-hong Yao, Yin-qi Li, Shao-jun Zhang, Wei-jing Wen, Kai Fan, Jia-li Zhang, Xiao Zhang. Risk factors and predictive model of adrenocortical insufficiency in patients with traumatic brain injury [J]. World Journal of Emergency Medicine, 2021, 12(3): 179-184. |
| [4] | Yong Liang, Hong Zeng, Yu-geng Liu, Ai-min Xu, Wen-hong Liu. Prevalence of post-traumatic stress disorder after earthquakes among the elderly in China: A meta-analysis [J]. World Journal of Emergency Medicine, 2021, 12(2): 137-142. |
| [5] | Samantha Shwe, Lauren Witchey, Shadi Lahham, Ethan Kunstadt, Inna Shniter, John C. Fox. Retrospective analysis of eFAST ultrasounds performed on trauma activations at an academic level-1 trauma center [J]. World Journal of Emergency Medicine, 2020, 11(1): 12-17. |
| [6] | Elaine Situ-LaCasse, Helpees Guirguis, Lucas Friedman, Asad E. Patanwala, Seth E. Cohen, Srikar Adhikari. Can emergency physicians perform extended compression ultrasound for the diagnosis of lower extremity deep vein thrombosis? [J]. World Journal of Emergency Medicine, 2019, 10(4): 205-209. |
| [7] | Linda C. Chokotho, Wakisa Mulwafu, Mulinda Nyirenda, Foster J. Mbomuwa, Hemant G. Pandit, Grace Le, Christopher Lavy. Establishment of trauma registry at Queen Elizabeth Central Hospital (QECH), Blantyre, Malawi and mapping of high risk geographic areas for trauma [J]. World Journal of Emergency Medicine, 2019, 10(1): 33-41. |
| [8] | Hojat Sheikh Motahar Vahedi, Hadi Hajebi, Elnaz Vahidi, Amir Nejati, Morteza Saeedi. Comparison between intravenous morphine versus fentanyl in acute pain relief in drug abusers with acute limb traumatic injury [J]. World Journal of Emergency Medicine, 2019, 10(1): 27-32. |
| [9] | Bianca M. Wahlen, Ayman El-Menyar, Mohammad Asim, Hassan Al-Thani. Rapid sequence induction (RSI) in trauma patients: Insights from healthcare providers [J]. World Journal of Emergency Medicine, 2019, 10(1): 19-26. |
| [10] | Brian G. Cornelius, Elizabeth Webb, Angela Cornelius, Kenneth W.G. Smith, Srdan Ristic, Jay Jain, Urska Cvek, Marjan Trutschl. Effect of sedative agent selection on morbidity, mortality and length of stay in patients with increase in intracranial pressure [J]. World Journal of Emergency Medicine, 2018, 9(4): 256-261. |
| [11] | Suresh Kumar Arumugam, Insolvisagan Mudali, Gustav Strandvik, Ayman El-Menyar, Ammar Al-Hassani, Hassan Al-Thani. Risk factors for ventilator-associated pneumonia in trauma patients: A descriptive analysis [J]. World Journal of Emergency Medicine, 2018, 9(3): 203-210. |
| [12] | Ahmed El Muntasar, Ethan Toner, Oddai A. Alkhazaaleh, Danaradja Arumugam, Nikhil Shah, Shahab Hajibandeh, Shahin Hajibandeh. Effect of angioembolisation versus surgical packing on mortality in traumatic pelvic haemorrhage: A systematic review and meta-analysis [J]. World Journal of Emergency Medicine, 2018, 9(2): 85-92. |
| [13] | Saeed Mahmood, Omaima Mahmood, Ayman El-Menyar, Mohammad Asim, Hassan Al-Thani. Predisposing factors, clinical assessment, management and outcomes of agitation in the trauma intensive care unit [J]. World Journal of Emergency Medicine, 2018, 9(2): 105-112. |
| [14] | Kasim Turgut, Mehmet Ediz Sarihan, Cemil Colak, Taner Güven, Ali Gür, Sükrü Gürbüz. Falls from height: A retrospective analysis [J]. World Journal of Emergency Medicine, 2018, 9(1): 46-50. |
| [15] | Salima Kerai, Omrana Pasha, Uzma Khan, Muhammad Islam, Nargis Asad, Junaid Razzak. Association of post-traumatic stress disorder and work performance: A survey from an emergency medical service, Karachi, Pakistan [J]. World Journal of Emergency Medicine, 2017, 8(3): 214-222. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
