World Journal of Emergency Medicine ›› 2023, Vol. 14 ›› Issue (3): 186-192.doi: 10.5847/wjem.j.1920-8642.2023.052
• Original Articles • Previous Articles Next Articles
Meng-meng An1,2, Chen-xi Liu2, Ping Gong3( )
)
Received:2022-12-22
Online:2023-04-28
Published:2023-05-01
Contact:
Ping Gong
E-mail:gongp828@sina.cn
Meng-meng An, Chen-xi Liu, Ping Gong. Effects of continuous renal replacement therapy on inflammation-related anemia, iron metabolism and prognosis in sepsis patients with acute kidney injury[J]. World Journal of Emergency Medicine, 2023, 14(3): 186-192.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2023.052
Table 1.
Baseline characteristics
| Parameters | Control group (n=50) | CRRT group (n=39) | P-valuea |
|---|---|---|---|
| Age, years | 76.0 (68.2, 85.1) | 74.5 (65.0, 83.3) | 0.489 |
| Male gender, n (%) | 29 (58.0) | 18 (46.2) | 0.292 |
| Infection sites, n (%) | |||
| Lung | 21 (42.0) | 12 (30.8) | 0.377 |
| Abdomen | 13 (26.0) | 17 (43.6) | 0.114 |
| Biliary system | 9 (18.0) | 6 (15.4) | 0.784 |
| Soft skin tissue | 9 (18.0) | 4 (10.2) | 0.375 |
| Comorbidities, n (%) | |||
| Hypertension | 28 (56.0) | 20 (51.3) | 0.675 |
| Diabetes mellitus | 20 (40.0) | 11 (28.2) | 0.271 |
| Stroke Acute myocardial infarction Deep venous thrombosis | 1 (2.0) 2 (4.0) 4 (8.0) | 0 (0) 0 (0) 1 (2.6) | 1.000 0.502 0.380 |
| Post-operative patients, n (%) | 7 (14.0) | 3 (7.7) | 0.503 |
| Patients using vasopressors, n (%) | 27 (54.0) | 20 (51.5) | 0.833 |
| Patients with mechanical ventilation, n (%) | 26 (52.0) | 17 (43.6) | 0.523 |
| Length of mechanical ventilation, h | 102.0 (75.8, 136.0) | 117.0 (79.0, 151.0) | 0.386 |
| PaO2/FiO2, mmHg | 216.5 (175.8, 245.0) | 217.0 (192.0, 244.0) | 0.579 |
| Serum procalcitonin, ng/mL | 7.32 (2.45, 10.23) | 5.00 (1.16, 16.90) | 0.993 |
| Serum lactate, mmol/L | 4.05 (2.28, 5.53) | 3.10 (1.80, 4.90) | 0.101 |
| Serum creatinine, µmol/L | 242.0 (181.8, 261.3) | 247.0 (209.0, 265.0) | 0.721 |
| Urine output, mL/(kg·h) | 0.32 (0.28, 0.49) | 0.37 (0.29, 0.48) | 0.735 |
| Serum potassium, mmol/L | 4.16 (3.84, 4.58) | 4.36 (3.96, 4.65) | 0.186 |
| Reticulocytes, ×109/L | 66.0 (43.3, 81.3) | 50.0 (38.0, 65.0) | 0.083 |
| Mean corpuscular volume, fL | 88.5 (82.0, 93.0) | 88.0 (85.0, 93.0) | 0.967 |
| Mean corpuscular hemoglobin, pg | 32.0 (30.0, 34.0) | 32.0 (29.0, 34.0) | 0.800 |
| MCHC, g/L | 334.5 (320.8, 347.0) | 333.0 (314.0, 348.0) | 0.628 |

Figure 1.
Comparison of parameters correlated to anemia in patients with sepsis between the CRRT and control groups. The normal range of HB and RDW detected by an automatic blood cell analyzer was 130-175 g/L and <15%, respectively. The asterisks, circles, and numbers beside these denote the outliers, and were defined in the usual manner as points above (and below) 1.5 times the interquartile range. CRRT: continuous renal replacement therapy; ICU: intensive care unit; HB: hemoglobin; RDW: red blood cell distribution width; EPO: erythropoietin; IL-6: interleukin-6.
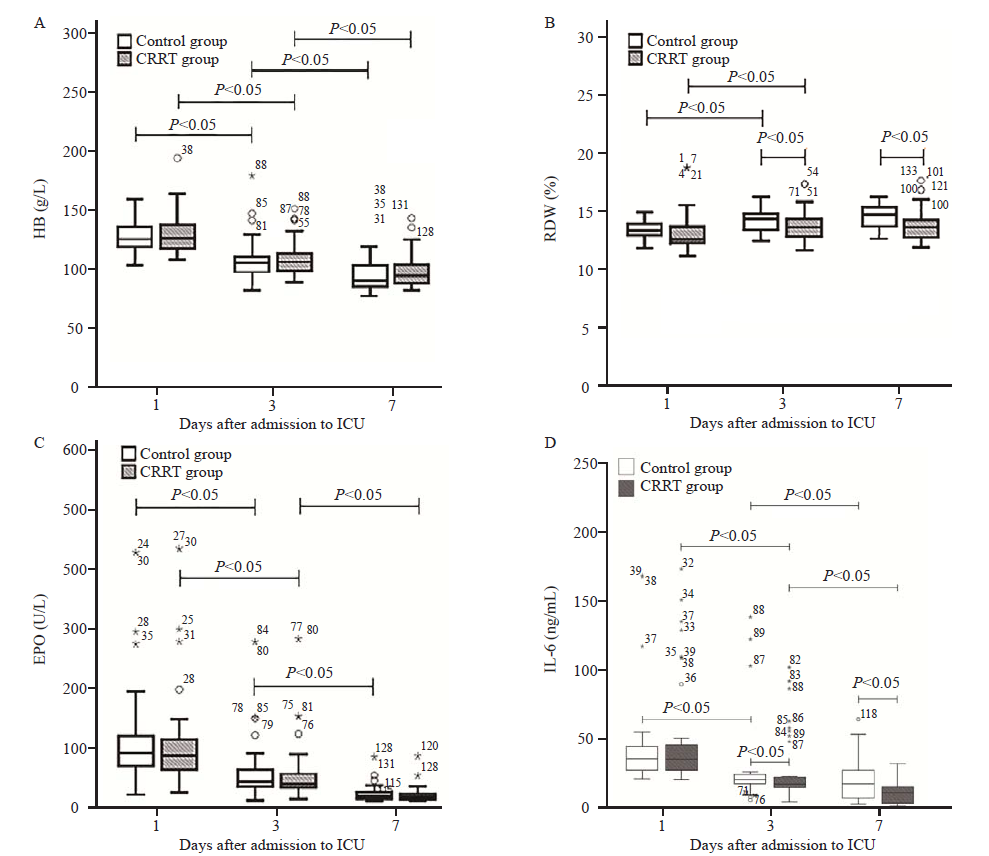
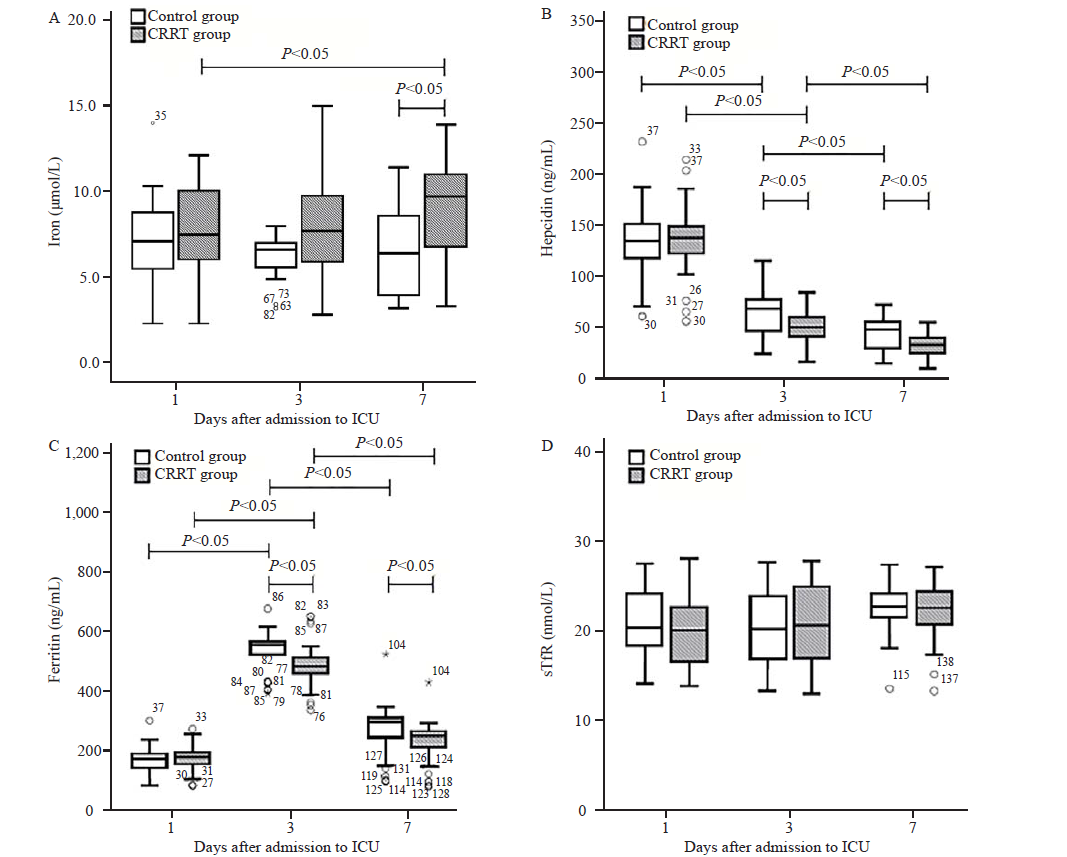
Figure 2.
Comparison of parameters correlated to iron metabolism in sepsis patients between the CRRT and control groups. The asterisks, circles, and numbers beside these denote the outliers, and were defined in the usual manner as points above (and below) 1.5 times the interquartile range. CRRT: continuous renal replacement therapy; ICU: intensive care unit; sTfR: soluble transferrin receptor.
| [1] |
Vincent JL, Marshall JC, Namendys-Silva SA, Francois B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014; 2(5):380-86.
doi: 10.1016/S2213-2600(14)70061-X |
| [2] |
Hu H, Jiang JY, Yao N. Comparison of different versions of the quick sequential organ failure assessment for predicting in-hospital mortality of sepsis patients: A retrospective observational study. World J Emerg Med. 2022; 13(2):114-9.
doi: 10.5847/wjem.j.1920-8642.2022.027 pmid: 35237364 |
| [3] |
Jiang Y, Jiang FQ, Kong F, An MM, Jin BB, Cao D, Gong P. Inflammatory anemia-associated parameters are related to 28-day mortality in patients with sepsis admitted to the ICU: a preliminary observational study. Ann Intensive Care. 2019; 9(1):67.
doi: 10.1186/s13613-019-0542-7 pmid: 31183575 |
| [4] | Carson JL, Stanworth SJ, Roubinian N, Fergusson DA, Triulzi D, Doree C, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2016; 10:CD002042. |
| [5] |
Heming N, Montravers P, Lasocki S. Iron deficiency in critically ill patients: highlighting the role of hepcidin. Crit Care. 2011; 15(2):210.
doi: 10.1186/cc9992 |
| [6] |
Romagnoli S, Ricci Z, Ronco C. CRRT for sepsis-induced acute kidney injury. Curr Opin Crit Care. 2018; 24(6):483-92.
doi: 10.1097/MCC.0000000000000544 pmid: 30239411 |
| [7] |
Putzu A, Fang MX, Boscolo Berto M, Belletti A, Cabrini L, Cassina T, et al. Blood purification with continuous veno-venous hemofiltration in patients with sepsis or ARDS: a systematic review and meta-analysis. Minerva Anestesiol. 2017; 83(8):867-77.
doi: 10.23736/S0375-9393.17.11946-2 pmid: 28607338 |
| [8] |
Venkataraman R, Subramanian S, Kellum JA. Clinical review: extracorporeal blood purification in severe sepsis. Crit Care. 2003; 7(2):139-45.
doi: 10.1186/cc1889 pmid: 12720560 |
| [9] |
Bellomo R, Ronco C. Continuous haemofiltration in the intensive care unit. Crit Care. 2000; 4(6):339-45.
doi: 10.1186/cc718 pmid: 11123877 |
| [10] |
Kellum JA, Lameire N. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013; 17(1):204.
doi: 10.1186/cc11454 |
| [11] |
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017; 43(3):304-77.
doi: 10.1007/s00134-017-4683-6 pmid: 28101605 |
| [12] |
Rodriguez RM, Corwin HL, Gettinger A, Corwin MJ, Gubler D, Pearl RG. Nutritional deficiencies and blunted erythropoietin response as causes of the anemia of critical illness. J Crit Care. 2001; 16(1):36-41.
doi: 10.1053/jcrc.2001.21795 pmid: 11230723 |
| [13] |
van Eijk LT, Kroot JJ, Tromp M, van der Hoeven JG, Swinkels DW, Pickkers P. Inflammation-induced hepcidin-25 is associated with the development of anemia in septic patients: an observational study. Crit Care. 2011; 15(1):R9.
doi: 10.1186/cc9408 |
| [14] |
Emans ME, van der Putten K, van Rooijen KL, Kraaijenhagen RJ, Swinkels D, van Solinge WW, et al. Determinants of red cell distribution width (RDW) in cardiorenal patients: RDW is not related to erythropoietin resistance. J Card Fail. 2011; 17(8):626-33.
doi: 10.1016/j.cardfail.2011.04.009 pmid: 21807323 |
| [15] |
French C. Erythropoietin in critical illness and trauma. Crit Care Clin. 2019; 35(2):277-87.
doi: S0749-0704(18)30785-1 pmid: 30784609 |
| [16] |
Chen J, Chen G, Xiao D, Peng W, Yu G, Lin Y, et al. Continuous venovenous hemofiltration decreases mortality and ameliorates acute lung injury in canine model of severe salt water drowning. Scand J Trauma Resusc Emerg Med. 2016; 24:40.
doi: 10.1186/s13049-016-0224-5 |
| [17] |
Ganz T, Nemeth E. Hepcidin and iron homeostasis. Biochim Biophys Acta. 2012; 1823(9):1434-43.
doi: 10.1016/j.bbamcr.2012.01.014 pmid: 22306005 |
| [18] |
Darveau M, Denault AY, Blais N, Notebaert E. Bench-to-bedside review: iron metabolism in critically ill patients. Crit Care. 2004; 8(5):356-62.
doi: 10.1186/cc2862 |
| [19] |
Silvester W. Mediator removal with CRRT: complement and cytokines. Am J Kidney Dis. 1997; 30(5 Suppl 4):S38-43.
doi: 10.1016/S0272-6386(97)90541-2 |
| [20] |
Zaritsky J, Young B, Gales B, Wang HJ, Rastogi A, Westerman M, et al. Reduction of serum hepcidin by hemodialysis in pediatric and adult patients. Clin J Am Soc Nephrol. 2010; 5(6):1010-4.
doi: 10.2215/CJN.08161109 |
| [1] | Jue-xian Wei, Hui-lin Jiang, Xiao-hui Chen. Endothelial cell metabolism in sepsis [J]. World Journal of Emergency Medicine, 2023, 14(1): 10-16. |
| [2] | Hui Liu, Jie Hu, Jian-guo Xiao, Hong-jun Kang, Fei-hu Zhou. The procalcitonin-to-cortisol ratio is a potential prognostic predictor in sepsis with abdominal source: a retrospective observational study [J]. World Journal of Emergency Medicine, 2022, 13(6): 441-447. |
| [3] | Ralph Bou Chebl, Nadim Kattouf, Mohamad Assaf, Saadeddine Haidar, Gilbert Abou Dagher, Sarah Abdul Nabi, Rana Bachir, Mazen El Sayed. Comparing the demographic data and outcomes of septic shock patients presenting to teaching or non-teaching metropolitan hospitals in the United States [J]. World Journal of Emergency Medicine, 2022, 13(6): 433-440. |
| [4] | Shi-yuan Yu, Zeng-zheng Ge, Jun Xiang, Yan-xia Gao, Xin Lu, Joseph Harold Walline, Mu-bing Qin, Hua-dong Zhu, Yi Li. Is rosuvastatin protective against sepsis-associated encephalopathy? A secondary analysis of the SAILS trial [J]. World Journal of Emergency Medicine, 2022, 13(5): 367-372. |
| [5] | A-ling Tang, Mei-jia Shen, Guo-qiang Zhang. Intestinal microcirculation dysfunction in sepsis: pathophysiology, clinical monitoring, and therapeutic interventions [J]. World Journal of Emergency Medicine, 2022, 13(5): 343-348. |
| [6] | Xiao-kang Dai, Zhen-xing Ding, Yuan-yuan Tan, Hua-rui Bao, Dong-yao Wang, Hong Zhang. Neutrophils inhibit CD8+ T cells immune response by arginase-1 signaling in patients with sepsis [J]. World Journal of Emergency Medicine, 2022, 13(4): 266-273. |
| [7] | Xuan Fu, Xue Lin, Samuel Seery, Li-na Zhao, Hua-dong Zhu, Jun Xu, Xue-zhong Yu. Speckle-tracking echocardiography for detecting myocardial dysfunction in sepsis and septic shock patients: A single emergency department study [J]. World Journal of Emergency Medicine, 2022, 13(3): 175-181. |
| [8] | Mei-jia Shen, Li-chao Sun, Xiao-yu Liu, Meng-chen Xiong, Shan Li, A-ling Tang, Guo-qiang Zhang. Trichostatin A improves the inflammatory response and liver injury in septic mice through the FoxO3a/autophagy signaling pathway [J]. World Journal of Emergency Medicine, 2022, 13(3): 182-188. |
| [9] | Cheng Hang, Li-jun Liu, Zhao-yun Huang, Jian-liang Zhu, Bao-chun Zhou, Xiao-zhen Li. Optimal indicator for changing the filter during the continuous renal replacement therapy in intensive care unit patients with acute kidney injury: A crossover randomized trial [J]. World Journal of Emergency Medicine, 2022, 13(3): 196-201. |
| [10] | Hai Hu, Jing-yuan Jiang, Ni Yao. Comparison of different versions of the quick sequential organ failure assessment for predicting in-hospital mortality of sepsis patients: A retrospective observational study [J]. World Journal of Emergency Medicine, 2022, 13(2): 114-119. |
| [11] | Stella Ng, Qi-feng Zhu, Ju-bo Jiang, Chun-hui Liu, Jia-qi Fan, Ye-ming Xu, Xian-bao Liu, Jian-an Wang. Anemia and risk of periprocedural cerebral injury detected by diffusion-weighted magnetic resonance imaging in patients undergoing transcatheter aortic valve replacement [J]. World Journal of Emergency Medicine, 2022, 13(1): 32-39. |
| [12] | Li-wei Duan, Jin-long Qu, Jian Wan, Yong-hua Xu, Yi Shan, Li-xue Wu, Jin-hao Zheng, Wei-wei Jiang, Qi-tong Chen, Yan Zhu, Jian Zhou, Wen-bo Yu, Lei Pei, Xi Song, Wen-fang Li, Zhao-fen Lin. Effects of viral infection and microbial diversity on patients with sepsis: A retrospective study based on metagenomic next-generation sequencing [J]. World Journal of Emergency Medicine, 2021, 12(1): 29-35. |
| [13] | Hai-jiang Zhou, Tian-fei Lan, Shu-bin Guo. Outcome prediction value of National Early Warning Score in septic patients with community-acquired pneumonia in emergency department: A single-center retrospective cohort study [J]. World Journal of Emergency Medicine, 2020, 11(4): 206-215. |
| [14] | Yu-ming Wang, Yan-jun Zheng, Ying Chen, Yun-chuan Huang, Wei-wei Chen, Ran Ji, Li-li Xu, Zhi-tao Yang, Hui-qiu Sheng, Hong-ping Qu, En-qiang Mao, Er-zhen Chen. Effects of fluid balance on prognosis of acute respiratory distress syndrome patients secondary to sepsis [J]. World Journal of Emergency Medicine, 2020, 11(4): 216-222. |
| [15] | Miao Yuan, Ding-yi Yan, Fang-shi Xu, Yi-di Zhao, Yang Zhou, Long-fei Pan. Effects of sepsis on hippocampal volume and memory function [J]. World Journal of Emergency Medicine, 2020, 11(4): 223-230. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
