World Journal of Emergency Medicine ›› 2021, Vol. 12 ›› Issue (4): 303-308.doi: 10.5847/wjem.j.1920-8642.2021.04.009
• Orginal Articles • Previous Articles Next Articles
Ji-yang Ling1, Chun-sheng Li2( ), Yun Zhang1, Xiao-li Yuan1, Bo Liu3, Yong Liang3, Qiang Zhang3
), Yun Zhang1, Xiao-li Yuan1, Bo Liu3, Yong Liang3, Qiang Zhang3
Received:2020-12-15
Accepted:2021-05-26
Online:2021-09-01
Published:2021-08-17
Contact:
Chun-sheng Li
E-mail:lcscyyy@163.com
Ji-yang Ling, Chun-sheng Li, Yun Zhang, Xiao-li Yuan, Bo Liu, Yong Liang, Qiang Zhang. Protective effect of extracorporeal membrane pulmonary oxygenation combined with cardiopulmonary resuscitation on post-resuscitation lung injury[J]. World Journal of Emergency Medicine, 2021, 12(4): 303-308.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2021.04.009

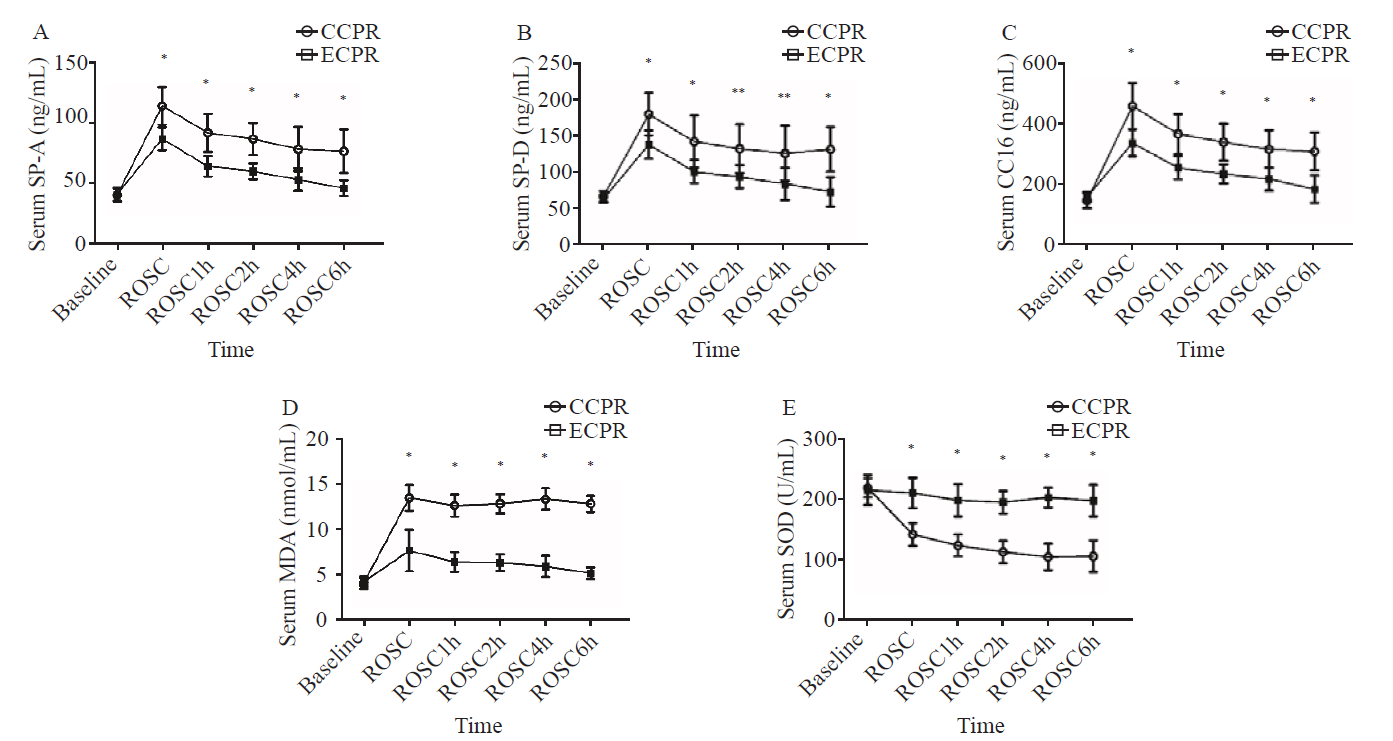
Figure 1.
Comparison of serum markers at each time point between the two groups. Data were expressed as mean±standard deviation (n=8); CCPR: conventional cardiopulmonary resuscitation; ECPR: extracorporeal cardiopulmonary resuscitation; SP-A: surfactant protein A; SP-D: surfactant protein D; CC16: Clara cell protein 16; MDA: malondialdehyde; SOD: superoxide dismutase; ROSC: return of spontaneous circulation; ROSC1h/2h/4h/6h: 1, 2, 4, and 6 hours after ROSC; compared with baseline, *P<0.01, **P <0.05.
| 1 |
Lin MH, Peng LN, Chen LK, Chen TJ, Hwang SJ. Cardiopulmonary resuscitation for hospital inpatients in Taiwan: an 8-year nationwide survey. Resuscitation. 2012; 83(3):343-6.
doi: 10.1016/j.resuscitation.2011.09.006 |
| 2 |
Nehme Z, Andrew E, Bernard S, Smith K. Impact of cardiopulmonary resuscitation duration on survival from paramedic witnessed out-of-hospital cardiac arrests: an observational study. Resuscitation. 2016; 100:25-31.
doi: 10.1016/j.resuscitation.2015.12.011 |
| 3 | Chen YS, Chao A, Yu HY, Ko WJ, Wu IH, Chen RJC, et al. Analysis and results of prolonged resuscitation in cardiac arrest patients rescued by extracorporeal membrane oxygenation. J Am Coll Cardiol. 2003; 41(2):197-203. |
| 4 |
Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008; 372(9638):554-61.
doi: 10.1016/S0140-6736(08)60958-7 |
| 5 |
Ortega-Deballon I, Hornby L, Shemie SD, Bhanji F, Guadagno E. Extracorporeal resuscitation for refractory out-of-hospital cardiac arrest in adults: a systematic review of international practices and outcomes. Resuscitation. 2016; 101:12-20.
doi: 10.1016/j.resuscitation.2016.01.018 pmid: 26836946 |
| 6 |
Kim SJ, Kim HJ, Lee HY, Ahn HS, Lee SW. Comparing extracorporeal cardiopulmonary resuscitation with conventional cardiopulmonary resuscitation: a meta-analysis. Resuscitation. 2016; 103:106-16.
doi: 10.1016/j.resuscitation.2016.01.019 |
| 7 |
Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation. 2007; 116(15):1693-700.
pmid: 17893278 |
| 8 |
Ding CQ, Zhang YP, Wang YW, Yang MF, Wang S, Cui NQ, et al. Death and do-not-resuscitate order in the emergency department: A single-center three-year retrospective study in the Chinese mainland. World J Emerg Med. 2020; 11(4):231-7.
doi: 10.5847/wjem.j.1920-8642.2020.04.005 |
| 9 |
Menegazzi JJ, Salcido DD, Housler GJ, Logue ES. Feasibility of initiating extracorporeal life support during mechanical chest compression CPR: a porcine pilot study. Resuscitation. 2012; 83(1):130-3.
doi: 10.1016/j.resuscitation.2011.07.030 pmid: 21835144 |
| 10 |
Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. 2015; 86:88-94.
doi: 10.1016/j.resuscitation.2014.09.010 |
| 11 | Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: adult advanced cardiovascular life support 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(18 Suppl 2):S444-64. |
| 12 | Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: post-cardiac arrest care 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(18 Suppl 2):S465-82. |
| 13 |
Giannoni E, Sawa T, Allen L, Wiener-Kronish J, Hawgood S. Surfactant proteins A and D enhance pulmonary clearance of Pseudomonas aeruginosa. Am J Respir Cell Mol Biol. 2006; 34(6):704-10.
doi: 10.1165/rcmb.2005-0461OC |
| 14 |
Bridges JP, Davis HW, Damodarasamy M, Kuroki Y, Howles G, Hui DY, et al. Pulmonary surfactant proteins A and D are potent endogenous inhibitors of lipid peroxidation and oxidative cellular injury. J Biol Chem. 2000; 275(49):38848-55.
pmid: 10969075 |
| 15 |
Goto H, Ledford JG, Mukherjee S, Noble PW, Williams KL, Wright JR. The role of surfactant protein A in bleomycin-induced acute lung injury. Am J Respir Crit Care Med. 2010; 181(12):1336-44.
doi: 10.1164/rccm.200907-1002OC |
| 16 |
Belhaj A, Boven C, Dewachter L, Ruiz Patino M, Sokolow Y, Rondelet B. Influence of donor lung surfactant-A and -B protein expression on the development of primary graft dysfunction after lung transplantation: a pilot study. Ann Transplant. 2017; 22:361-9.
doi: 10.12659/AOT.903313 |
| 17 |
Fan YW, Jiang SW, Chen JM, Wang HQ, Liu D, Pan SM, et al. A pulmonary source of infection in patients with sepsis-associated acute kidney injury leads to a worse outcome and poor recovery of kidney function. World J Emerg Med. 2020; 11(1):18-26.
doi: 10.5847/wjem.j.1920-8642.2020.01.003 |
| 18 |
Sato A, Whitsett JA, Scheule RK, Ikegami M. Surfactant protein D inhibits lung inflammation caused by ventilation in premature newborn lambs. Am J Respir Crit Care Med. 2010; 181(10):1098-105.
doi: 10.1164/rccm.200912-1818OC |
| 19 |
Thacker S, Moran AN, Lionakis M, Mastrangelo MAA, Halder T, Huby MDP, et al. Restoration of lung surfactant protein D by IL-6 protects against secondary pneumonia following hemorrhagic shock. J Infect. 2014; 68(3):231-41.
doi: 10.1016/j.jinf.2013.11.010 |
| 20 |
Duda I, Grzybowska K, Jędrzejowska-Szypułka H, Lewin-Kowalik J. The sitting position during neurosurgical procedures does not influence serum biomarkers of pulmonary parenchymal injury. BMC Surg. 2012; 12:24.
doi: 10.1186/1471-2482-12-24 |
| 21 |
Kurt A, Turut H, Acipayam A, Kirbas A, Yuce S, Cumhur Cure M, et al. Investigation of surfactant protein-D and interleukin-6 levels in patients with blunt chest trauma with multiple rib fractures and pulmonary contusions: a cross-sectional study in Black Sea Region of Turkey. BMJ Open. 2016; 6(10):e011797.
doi: 10.1136/bmjopen-2016-011797 |
| 22 |
Ware LB, Koyama T, Billheimer DD, Wu W, Bernard GR, Thompson BT, et al. Prognostic and pathogenetic value of combining clinical and biochemical indices in patients with acute lung injury. Chest. 2010; 137(2):288-96.
doi: 10.1378/chest.09-1484 |
| 23 |
Wen MN, Zhao G, Zhang JY, Zhao YH. Clinical study on the changes of lung-specific proteins: CC16 after lung contusion. Exp Ther Med. 2017; 14(3):2733-6.
doi: 10.3892/etm.2017.4842 |
| 24 | Wutzler S, Lehnert T, Laurer H, Lehnert M, Becker M, Henrich D, et al. Circulating levels of Clara cell protein 16 but not surfactant protein D identify and quantify lung damage in patients with multiple injuries. J Trauma. 2011; 71(2):E31-6. |
| 25 |
Determann RM, Millo JL, Waddy S, Lutter R, Garrard CS, Schultz MJ. Plasma CC16 levels are associated with development of ALI/ARDS in patients with ventilator-associated pneumonia: a retrospective observational study. BMC Pulm Med. 2009; 9(1):1-9.
doi: 10.1186/1471-2466-9-1 |
| 26 |
Marikovsky M, Ziv V, Nevo N, Harris-Cerruti C, Mahler O. Cu/Zn superoxide dismutase plays important role in immune response. J Immunol. 2003; 170(6):2993-3001.
pmid: 12626552 |
| 27 |
Jung O, Marklund SL, Geiger H, Pedrazzini T, Busse R, Brandes RP. Extracellular superoxide dismutase is a major determinant of nitric oxide bioavailability: in vivo and ex vivo evidence from ecSOD-deficient mice. Circ Res. 2003; 93(7):622-9.
doi: 10.1161/01.RES.0000092140.81594.A8 |
| 28 |
Karaiskos T, Tomos P, Asouhidou I, Nikiteas N, Kontakiotis T, Papalois A. Oxidative and pre-inflammatory stress in wedge resection of pulmonary parenchyma using the radiofrequency ablation technique in a swine model. J Cardiothorac Surg. 2012; 7:7.
doi: 10.1186/1749-8090-7-7 |
| 29 |
Meng L, Li LY, Lu S, Li K, Su ZB, Wang YY, et al. The protective effect of dexmedetomidine on LPS-induced acute lung injury through the HMGB1-mediated TLR4/NF-κB and PI3K/Akt/mTOR pathways. Mol Immunol. 2018; 94:7-17.
doi: S0161-5890(17)30601-6 pmid: 29241031 |
| 30 |
Şener G, Paskaloǧlu K, Toklu H, Kapucu C, Ayanoglu-Dulger G, Kacmaz A, et al. Melatonin ameliorates chronic renal failure-induced oxidative organ damage in rats. J Pineal Res. 2004; 36(4):232-41.
doi: 10.1111/jpi.2004.36.issue-4 |
| 31 |
Klebanoff SJ. Myeloperoxidase: friend and foe. J Leukoc Biol. 2005; 77(5):598-625.
doi: 10.1189/jlb.1204697 |
| 32 |
El Kebir D, József L, Pan WL, Wang LL, Petasis NA, Serhan CN, et al. 15-epi-lipoxin A4Inhibits myeloperoxidase signaling and enhances resolution of acute lung injury. Am J Respir Crit Care Med. 2009; 180(4):311-9.
doi: 10.1164/rccm.200810-1601OC |
| 33 |
Lv H, Liu QM, Wen ZM, Feng HH, Deng XM, Ci XX. Xanthohumol ameliorates lipopolysaccharide (LPS)-induced acute lung injury via induction of AMPK/GSK3β-Nrf2 signal axis. Redox Biol. 2017; 12:311-24.
doi: 10.1016/j.redox.2017.03.001 |
| [1] | Wei-jing Shao, Ting-ting Shu, Shuang Xu, Li-cai Liang, Jehane Michael Le Grange, Yu-ran Zhou, He Huang, Yu Cai, Qing Zhang, Peng Sun. Left-sided vagus nerve stimulation improves cardiopulmonary resuscitation outcomes in rats as effectively as right-sided vagus nerve stimulation [J]. World Journal of Emergency Medicine, 2021, 12(4): 309-316. |
| [2] | Xue-jie Dong, Lin Zhang, Yue-lin Yu, Shu-xiao Shi, Xiao-chen Yang, Xiao-qian Zhang, Shuang Tian, Helge Myklebust, Guo-hong Li, Zhi-jie Zheng. The general public’s ability to operate automated external defibrillator: A controlled simulation study [J]. World Journal of Emergency Medicine, 2020, 11(4): 238-245. |
| [3] | Yun-fei Jiang, Jian Kang, Pei-pei Huang, Jia-xi Yao, Zhong-he Wang, Lei Jiang, Jun Wang, Li Qiao, Bao-li Zhu, Hao Sun, Jin-song Zhang. Evaluation of gastric lavage efficiency and utility using a rapid quantitative method in a swine paraquat poisoning model [J]. World Journal of Emergency Medicine, 2020, 11(3): 174-181. |
| [4] | Ye-cheng Liu, Yan-meng Qi, Hui Zhang, Joseph Walline, Hua-dong Zhu. A survey of ventilation strategies during cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2019, 10(4): 222-227. |
| [5] | Alexei Birkun, Yekaterina Kosova. Social attitude and willingness to attend cardiopulmonary resuscitation training and perform resuscitation in the Crimea [J]. World Journal of Emergency Medicine, 2018, 9(4): 237-248. |
| [6] | Alexei Birkun, Maksim Glotov, Herman Franklin Ndjamen, Esther Alaiye, Temidara Adeleke, Sergey Samarin. Pre-recorded instructional audio vs. dispatchers’ conversational assistance in telephone cardiopulmonary resuscitation: A randomized controlled simulation study [J]. World Journal of Emergency Medicine, 2018, 9(3): 165-171. |
| [7] | Alexei Birkun, Maksim Glotov. Education in cardiopulmonary resuscitation in Russia: A systematic review of the available evidence [J]. World Journal of Emergency Medicine, 2017, 8(4): 245-252. |
| [8] | Chennappa Kalvatala Krishna, Hakim Irfan Showkat, Meenakshi Taktani, Vikram Khatri. Out of hospital cardiac arrest resuscitation outcome in North India — CARO study [J]. World Journal of Emergency Medicine, 2017, 8(3): 200-205. |
| [9] | Ji Ung Na, Sang Kuk Han, Pil Cho Choi, Dong Hyuk Shin. Effect of metronome rates on the quality of bag-mask ventilation during metronome-guided 30:2 cardiopulmonary resuscitation: A randomized simulation study [J]. World Journal of Emergency Medicine, 2017, 8(2): 136-140. |
| [10] | Gan-nan Wang, Xu-feng Chen, Li Qiao, Yong Mei, Jin-ru Lv, Xi-hua Huang, Bin Shen, Jin-song Zhang. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A meta-analysis of 2 260 patients with cardiac arrest [J]. World Journal of Emergency Medicine, 2017, 8(1): 5-11. |
| [11] | Marion Leary, David G. Buckler, Daniel J. Ikeda, Daiane A. Saraiva, Robert A. Berg, Vinay M. Nadkarni, Audrey L. Blewer, Benjamin S. Abella. The association of layperson characteristics with the quality of simulated cardiopulmonary resuscitation performance [J]. World Journal of Emergency Medicine, 2017, 8(1): 12-18. |
| [12] | Chik Leung Ho, Ka Wai Cheng, Tze Hang Ma, Yau Hang Wong, Ka Lok Cheng, Chak Wah Kam. Characterization of available automated external defibrillators in the market based on the product manuals in 2014 [J]. World Journal of Emergency Medicine, 2016, 7(2): 138-146. |
| [13] | Audrey L. Blewer, David G. Buckler, Jiaqi Li, Marion Leary, Lance B. Becker, Judy A. Shea, Peter W. Groeneveld, Mary E. Putt, Benjamin S. Abella. Impact of the 2010 resuscitation guidelines training on layperson chest compressions [J]. World Journal of Emergency Medicine, 2015, 6(4): 270-276. |
| [14] | Jian-ping Gao, Ke-jing Ying. Thrombolysis during extended cardiopulmonary resuscitation for autoimmune-related pulmonary embolism [J]. World Journal of Emergency Medicine, 2015, 6(2): 153-156. |
| [15] | Shou-quan Chen. Advances in clinical studies of cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2015, 6(2): 85-93. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
