INTRODUCTION
The Beijing 2022 Olympic Winter Games was the second Games held amid the COVID-19 pandemic,[1] a situation that has impacted millions of lives in every nation. Moreover, to a certain extent, the pandemic has altered the way sporting activities operate. In the context of the spread of the Omicron variant of SARS-CoV-2 and high virus transmissibility during the winter months, it is important to ensure athletes’ health, safety, and ability to compete. Although recent data exist concerning injuries and illnesses from the Winter Olympic Games held in Sochi 2014[2] and PyeongChang in 2018,[3] injury and illness prevention and the protection of athletes’ health are key mandates for the International Olympic Committee. Systematic monitoring of trends in injury and illness over time can provide epidemiological data that are invaluable in maintaining the health of athletes.[4] Each venue in Beijing, Yanqing, and Zhangjiakou set up a clinic and was equipped with ambulances to provide a variety of medical services. In general, injuries reported in winter sports are classified according to injury site, type, incidence, and severity.[5⇓-7] Illnesses are classified and reported according to type, symptoms, and cause. However, there is a lack of knowledge on injury risk and illness occurrence among elite winter sport athletes during the COVID-19 pandemic. Thus, the aim of the present study was to evaluate the characteristics and frequencies of injury and illnesses occurring among all athletes during the Beijing 2022 Olympic Winter Games.
METHODS
We conducted a retrospective study encompassing multiple sports events. A total of 231 ambulances were available in the Beijing, Yanqing, and Zhangjiakou competition areas to provide 24-hour emergency services. We collected information for all athletes treated for injuries and illnesses in the polyclinic and all other medical venues operated by Beijing 2022 medical staff between 4 and 20 February 2022, as well as information on ambulance transfers. These data were collected using an electronic medical record system.
Implementation
After the Winter Olympics, we analyzed all the case data, clarified the statistical criteria, and separated the missing items to ensure the accuracy of the data analysis.
Definitions of injury and illness
Injuries and illnesses were defined as new cases (presently existing, without full recovery) or recurring cases (occurrence after fully taking part in the Games) of incidents such as musculoskeletal complaints or concussions. We included athletes who were undergoing medical treatment incurred in competition or training, regardless of the consequences of their absence from competition or training. [8] In cases with several diagnoses involving multiple body parts injured during the same incident or multiple types of injury or illness occurring in the same or different parts of the body, only the most severe injuries/illnesses were registered.
Injury and illness report form
In terms of injuries, we recorded the following information: athletes’ accreditation number, sport/event (whether the injury occurred in competition or training, whether the athlete was transferred), time of injury, injured body part, injury type, cause of injury, and estimated time lost from competition or training. We also recorded the following information for illnesses: athletes’ accreditation number, affected system(s), and main symptom(s).
Confidentiality and ethical approval
We used the athletes’ accreditation number to query the athlete database to collect information on the athletes’ age, sex, and nationality. We treated all information with strict confidence and anonymized our medical database at the end of the Games.
This study was approved by the Ethics Committee of Beijing Emergency Medical Center (No. 2022-4-003), and written informed consent was waived.
Data analysis
We calculated injury and illness incidence as the number of injuries or illnesses occurring during competition or training, respectively, with incidence presented as injuries/illnesses per 100 athlete-days. Data were compared between male group and female group with respect to injury and illness risk using the Student’s t-test for continuous variables. We calculated the risk ratio (RR) of the number of injuries or illnesses between the two groups, assuming a constant hazard per group. We present injury and illness incidence with 95% confidence intervals (CIs). We considered two-tailed P values ≤0.05 as statistically significant.
RESULTS
Incidence and distribution of injuries and illnesses
In total, 2,897 athletes from 91 nations experienced injuries or illnesses. Among them, 1,593 were men, and 1,304 were women. Beijing 2022 medical staff reported 326 injuries and 80 illnesses. Thus, there were 11.3 injuries (95%CI: 10.1-12.4) and 2.8 illnesses (95%CI: 2.2-3.4) per 100 athletes over the 17-day period. Altogether, 11% of athletes incurred at least one injury, and 2% incurred at least one illness. Whereas most injured athletes experienced one injury, a total of 11 athletes had two or more injuries. The number of injured athletes was the highest in the skating sports (n=104), followed by alpine skiing (n=53), ice track (n=37), freestyle skiing (n=36), and ice hockey (n=35), and was the lowest in the Nordic skiing disciplines (n=20); no athletes were injured in the curling events. In terms of injuries by gender, 13.3% of women and 9.5% of men experienced at least one injury (RR=1.40, 95%CI: 1.14 -1.72, P=0.001), resulting in an incidence of 13.3 (95%CI: 11.5-15.2) injuries per 100 female athletes and 9.5 (95%CI: 8.1-11.0) injuries per 100 male athletes. With regard to illnesses by gender, 3.5% of women and 2.1% of men experienced an illness (RR=1.65, 95%CI: 1.07-2.56, P=0.023), with an incidence of 3.5 (95%CI: 2.5-4.5) illnesses per 100 female athletes and 2.1 (95%CI: 1.4-2.8) illnesses per 100 male athletes. Illnesses were reported in a variety of sports. The sports with more than 10 illness cases were skating sports (n=33) and Nordic skiing (n=22) (Table 1).
Table 1. Number (n) and proportion (%) of injuries and illnesses in different sports in the Beijing 2022 Olympic Winter Games
| Sports | Injuries | Illnesses | |||||
|---|---|---|---|---|---|---|---|
| Female | Male | Total | Female | Male | Total | ||
| Ice sports | |||||||
| Curling | - | - | - | - | - | - | |
| Ice hockey | 10 | 25 | 35 | 2 | 3 | 5 | |
| Skating | |||||||
| Figure | 2 | 4 | 6 | 1 | 2 | 3 | |
| Short track | 8 | 6 | 14 | 8 | 3 | 11 | |
| Speed | 26 | 7 | 33 | 6 | 5 | 11 | |
| Information on sport/event missing * | 42 | 9 | 51 | 3 | 5 | 8 | |
| Ice track | |||||||
| Bobsleigh | 5 | 18 | 23 | 3 | 2 | 5 | |
| Luge | 1 | 9 | 10 | 1 | 1 | 2 | |
| Skeleton | 3 | 1 | 4 | 2 | 1 | 3 | |
| Snow sports | |||||||
| Alpine skiing | |||||||
| Technology (Downhill, super-G) | 11 | 18 | 29 | 2 | 1 | 3 | |
| Speed (Giant Slalom, Slalom ) | 13 | 11 | 24 | - | 2 | 2 | |
| Freestyle skiing | |||||||
| Aerials | - | 2 | 2 | 1 | - | 1 | |
| Halfpipe | 3 | 3 | 6 | - | - | - | |
| Moguls | - | - | - | - | - | - | |
| Ski cross | 2 | 2 | 4 | - | - | - | |
| Slopestyle | 9 | 6 | 15 | 1 | - | 1 | |
| Big air | 9 | 0 | 9 | - | - | - | |
| Snowboarding | |||||||
| Halfpipe | 0 | 3 | 3 | - | - | - | |
| Slopestyle | 5 | 3 | 8 | 1 | - | 1 | |
| Snowboard cross | 6 | 3 | 9 | - | - | - | |
| Slalom | 0 | 1 | 1 | - | - | - | |
| Big air | 5 | 2 | 7 | 1 | - | 1 | |
| Nordic skiing | |||||||
| Biathlon | 0 | 1 | 1 | 7 | 2 | 9 | |
| Cross-country skiing | 5 | 11 | 16 | 6 | 5 | 11 | |
| Nordic combined | - | - | - | - | 1 | 1 | |
| Ski jumping | - | 3 | 3 | 1 | 1 | 1 | |
| Other* | 9 | 4 | 13 | - | 1 | 1 | |
| Total | 174 | 152 | 326 | 46 | 34 | 80 | |
*Partial data missing.
Location and type of injuries
The most affected injury locations were the knee (22.1%), followed by the lumbar spine (10.4%) and thigh (9.2%) (Table 2). The incidence of knee injuries was roughly the same in ice and snow sports. Muscle strains (29.1%), impingement (16.6%), and contusion (12.6%) were the most common types of injury (Table 2).
Table 2. The information of injuries in sports scheduled during the Beijing 2022 Olympic Winter Games
| Injuries | Ice sports | Snow sports | Other (n=13) | Total (n=326) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ice hockey (n=35) | Skating (n=104) | Ice track (n=37) | Alpine skiing (n=53) | Freestyle skiing (n=36) | Snowboarding (n=28) | Nordic skiing (n=20) | ||||
| Injury location | ||||||||||
| Face (including eye, ear, nose) | 2 | 1 | 1 | 3 | 6 | - | - | 2 | 15 (4.6) | |
| Head | 2 | 1 | - | - | 3 | 3 | 3 | - | 12 (3.7) | |
| Neck/cervical spine | 1 | 2 | 2 | 1 | 1 | 1 | - | - | 8 (2.5) | |
| Thoracic spine/upper back | - | 4 | - | 1 | - | - | - | - | 5 (1.5) | |
| Sternum/ribs | 2 | - | - | - | 2 | - | - | - | 4 (1.2) | |
| Lumbar spine/lower back | - | 9 | 5 | 9 | 1 | 3 | 5 | 2 | 34 (10.4) | |
| Abdomen | - | - | - | - | - | - | - | - | 0 (0) | |
| Pelvis/sacrum/buttock | - | 1 | 1 | 1 | - | 2 | - | - | 5 (1.5) | |
| Shoulder/clavicle | 12 | 1 | - | 1 | 4 | 2 | 1 | 1 | 22 (6.8) | |
| Elbow | - | 4 | - | 3 | - | 2 | - | 1 | 10 (3.1) | |
| Arm | 2 | 3 | 2 | 2 | - | - | - | - | 9 (2.8) | |
| Wrist | 2 | 2 | - | 3 | 1 | 3 | - | - | 11 (3.4) | |
| Hand | 3 | 4 | - | 3 | 1 | 2 | - | - | 13 (4.0) | |
| Finger | 1 | - | 2 | - | 3 | - | 1 | 1 | 8 (2.5) | |
| Hip | - | 1 | - | - | - | - | - | 1 | 2 (0.6) | |
| Groin | - | - | 2 | - | - | - | - | - | 2 (0.6) | |
| Thigh | - | 18 | 3 | 4 | 3 | - | 1 | 1 | 30 (9.2) | |
| Knee | 4 | 18 | 15 | 17 | 10 | 4 | 1 | 3 | 72 (22.1) | |
| Lower leg | - | 9 | 1 | 4 | 1 | - | - | - | 15 (4.6) | |
| Ankle | 2 | 11 | - | - | - | 5 | 5 | - | 23 (7.1) | |
| Foot/toe | 2 | 15 | 3 | 1 | - | 1 | 3 | 1 | 26 (8.0) | |
| Injury type | ||||||||||
| Concussion | 2 | 1 | - | - | 2 | 3 | 3 | - | 11 (3.4) | |
| Fracture (trauma, stress, other bone injuries) | 1 | 2 | 2 | 7 | 6 | 3 | 4 | 1 | 26 (8.0) | |
| Sprain (dislocation, subluxation, ligamentous rupture) | 2 | 6 | - | - | 5 | 5 | 2 | 1 | 21 (6.4) | |
| Strain (muscle rupture, tear, tendon rupture) | 1 | 52 | 13 | 17 | 3 | 2 | 5 | 2 | 95 (29.1) | |
| Meniscus, cartilage | - | - | 3 | - | - | - | - | - | 3 (0.9) | |
| Contusion, haematoma, brusie | 4 | 8 | 4 | 7 | 9 | 5 | - | 4 | 41 (12.6) | |
| Tendinosis, tendinapathy | - | - | 4 | - | - | - | - | - | 4 (1.2) | |
| Arthritis, synovitis, brusitis | - | - | 2 | - | - | - | - | - | 2 (0.6) | |
| Impingement | 22 | 2 | 2 | 10 | 8 | 7 | 2 | 1 | 54 (16.6) | |
| Laceration, abrasion, skin lesion | 3 | 5 | 7 | 8 | 1 | 1 | 2 | 1 | 28 (8.6) | |
| Dental injury, broken tooth | - | - | - | 1 | 2 | - | - | 1 | 4 (1.2) | |
| Muscle cramps, spasm | - | 26 | - | 3 | - | 1 | 1 | - | 31 (9.5) | |
| Other (nerve, spinal cord, fasciitis) | 2 | - | - | - | 1 | 1 | 2 | 6 (1.8) | ||
Number of injuries
Injury circumstances and severity of injury
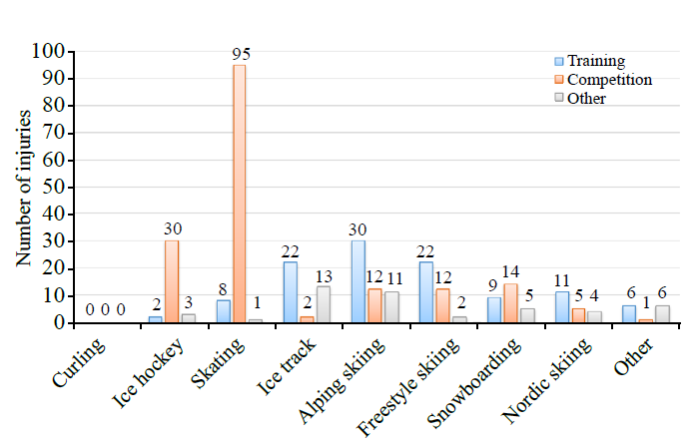
In total, slightly more than half of the 326 injuries occurred during competition (n=171, 52.5%), 110 injuries (33.7%) happened during training, and 45 injuries (13.8%) happened during other sports-related activities, such as during warm-up exercises (Figure 1).
Figure 1.
Figure 1.
Number of injuries in different circumstances for different sports.
Of the 326 injuries, 14 (4.3%) led to an estimated absence from training or competition of more than 1 week. The injuries included 10 cases of strain/muscle rupture/tear/tendon rupture (1 neck/cervical spine, 1 thoracic spine/upper back, 4 lumbar spine/lower back, 1 thigh, 2 knee, 1 foot/toe), 2 meniscus/cartilage injuries (2 knee), 1 case of tendinosis/tendinopathy (foot/toe), and 1 case of impingement (knee).
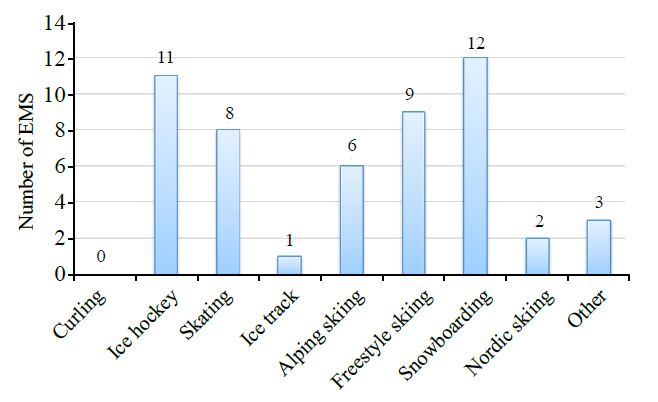
Emergency medical services (EMS) of injury
Among the 326 injuries, 52 (16%) athletes were transferred to hospitals for further care, and 12.8% of the 406 athletes had an injury or illness. The rate of EMS was the highest for snowboarding (n=12, 42.9 injuries [95% CI: 22.3-62.4] per 100 athletes), ice hockey (n=11, 31.4 injuries [95%CI: 15.2-47.6] per 100 athletes), and freestyle skiing (n=9, 25.0 injuries [95%CI: 10.1-39.9] per 100 athletes) (Table 3 and Figure 2).
Table 3. Information on the 52 athletes in emergency medical service
| Injury types | Sports with the highest number |
|---|---|
| Concussion | 2 in snowboard cross, 1 in skating sports, 1 in snowboarding big air, 1 in ice hockey |
| Fracture | 4 in alpine skiing, 1 in figure skating, 1 in aerials, 1 in other |
| Sprain (dislocation, subluxation, ligamentous rupture) | 2 in ski cross, 1 in figure skating, 1 in short track skating, 1 in freestyle skiing slopestyle, 1 in freestyle skiing big air, 1 in snowboarding halfpipe, 1 in snowboarding slopestyle, 1 in snowboard cross,1 in cross-country skiing, 1 in other, 1 in ice hockey |
| Strain (muscle rupture, tear, tendon rupture) | 2 in speed skating, 1 in short tract skating |
| Contusion, haematoma, brusie | 2 in other, 2 in ice hockey, 1 in snowboarding slopestyle |
| Impingement | 7 in ice hockey, 2 in snowboarding slopestyle, 2 in snowboard cross, 1 in short tract skating, 1 in aerials, 1 in freestyle skiing slopestyle, 1 in ski jumping |
| Laceration, abrasion, skin lesion | 2 in alpine skiing, 1 in short tract skating, 1 in freestyle skiing big air |
| Other (nerve, spinal cord, fasciitis) | 1 in snowboard cross |
Figure 2.
Figure 2.
Number of emergency medical service (EMS) in different sports.
Affected system, symptoms, cause, and severity of illnesses
The number of athletes with illnesses (n=80) was the highest in skating (n=33) and Nordic skiing (n=22). A total of 50 illnesses (62.5%) involved dentistry (n=28) and ophthalmology/otolaryngology (n=22) and were mostly observed in skating venues (n=29), Nordic skiing (n=8), and ice track (n=6) (Table 4). The cause of illness was most often classified as other (preexisting, drugs) (n=52, 65%), followed by infection (n=22, 27.5%). The most commonly reported symptoms were dehydration/anaphylaxis/lethargy/dizziness/asymptomatic (other; n=53, 66.3%) and pain (n=23, 28.8%). A total of 6 (7.6%) illness cases were exercise-induced or caused by environmental factors (Table 4). Approximately 5% (n=4) of illnesses were expected to result in absence from further training or competition. Of those, one case of illness was expected to result in an estimated time loss of more than 7 d (arrhythmia, dizziness).
Table 4. The information of illnesses in sports scheduled during the Beijing 2022 Olympic Winter Games
| Illnesses | Ice hockey (n=5) | Skating (n=33) | Ice track (n=10) | Alpine skiing (n=5) | Freestyle skiing (n=2) | Snowboarding (n=2) | Nordic skiing (n=22) | Other (n=1) | Total n (%) |
|---|---|---|---|---|---|---|---|---|---|
| Illness affected system | |||||||||
| Gastrointestinal | 1 | 1 | 1 | - | 1 | - | 2 | - | 6 (7.5) |
| Respiratory | 1 | - | - | - | - | 1 | 1 | - | 3 (3.8) |
| Allergic, immunologica | - | - | - | - | - | - | 1 | - | 1 (1.3) |
| Metabolic, endocrinological | - | - | - | - | - | - | 1 | - | 1 (1.3) |
| Dermatological | - | 1 | - | - | - | - | - | - | 1 (1.3) |
| Dental | 1 | 12 | 4 | 3 | 1 | - | 6 | 1 | 28 (35.0) |
| Ophthalmological, otolaryngological | 1 | 17 | 2 | - | - | - | 2 | - | 22 (27.5) |
| Other (urogenital, gynaecological, cardiovascular, neurological, psychiatric, musculoskeletal) | 1 | 2 | 3 | 2 | - | 1 | 9 | - | 18 (22.5) |
| Illness symptoms | |||||||||
| Fever | - | - | - | - | - | - | - | - | - |
| Pain | 2 | 7 | 6 | 1 | 1 | - | 6 | - | 23 (28.8) |
| Diarrhoea, vomiting | - | - | - | - | - | - | 1 | - | 1 (1.3) |
| Dyspnoea, cough | 1 | - | 1 | - | - | - | 1 | - | 3 (3.8) |
| Other (dehydration, anaphylaxis, lethargy, dizziness, asymptomatic) | 2 | 26 | 3 | 4 | 1 | 2 | 14 | 1 | 53 (66.3) |
| Illness cause | |||||||||
| Infection | 3 | 5 | 3 | 3 | 1 | 1 | 6 | - | 22 (27.5) |
| Environmental | - | - | - | 1 | - | 1 | 3 | - | 5 (6.3) |
| Exercise-induced | - | - | - | - | - | - | 1 | - | 1 (1.3) |
| Other (preexisting, medicine) | 2 | 28 | 7 | 1 | 1 | - | 12 | 1 | 52 (65.0) |
Number of EMS
DISCUSSION
The aim of this study was to describe, analyze, and evaluate the incidence of injuries and illnesses among athletes competing in the Beijing 2022 Olympic Winter Games. The main findings of this retrospective study were that 11.3% and 2.8% of the 2,897 athletes experienced at least one injury or illness, respectively. This resulted in 11.3 injuries and 2.8 illnesses per 100 athletes during the Games. Furthermore, the characteristics of injuries and illnesses varied greatly according to sport event and athletes’ sex.
Injuries in the Olympic sports
The incidence of injuries in the Beijing 2022 Olympics (11%) was slightly lower than those in PyeongChang 2018 (12%)[3] and Sochi 2014 (12%)[2] but comparable to those of Vancouver 2010 (11%)[9] and London 2012 (11%)[10] and slightly higher than those in Beijing 2008 (10%)[11] and Rio 2016 (8%).[12] Furthermore, 13.3% of women and 9.5% of men had at least one injury. The injury rate among female athletes was similar to their counterparts in PyeongChang 2018 (13.7%) whereas this rate among male athletes was slightly lower (11.9% in PyeongChang 2018). Injury rates in Beijing 2022 among both female and male athletes were lower than those in Sochi 2014 (14.9% and 13.2%, respectively). Thus, it can be concluded that the difference in the ratios of injuried males and females has increased in comparison with previous years. With seven new sport events in Beijing 2022, including women’s single bobsled, short track mixed team relay, mixed team ski jump, freestyle skiing big air (men’s and women’s), mixed team freestyle skiing aerials, and mixed team snowboarding cross, the proportion of female athletes was increased (45%) and athletes were more evenly distributed between men and women in comparison with past Games. This may have led to an increase in injury rates among female athletes. The frequency of injuries could not be obtained because of a lack of data on the number of athletes participating in each sport. However, the events with the most and least injuries were skating sports and curling, respectively.
Location and type of injuries
For the location of the injury, similar to the PyeongChang 2018 Olympic Winter Games[3] and the Vancouver 2010 Olympic Winter Games,[9] the site most frequently injured during Beijing 2022 was the knee (22.1%). In total, 50 of 72 (69.4%) knee injuries occurred among athletes from skating sports, alpine skiing, and ice track. According to previous studies, knee injuries mainly occur in snow sports. The incidence of knee injuries in snow sports was 77.4% in the PyeongChang 2018 Olympic Winter Games.[3] Similarly, Flørenes et al[13] reported that the knee was the most frequently injured body region among athletes in the World Cup tournament, with incidences of 36% in alpine skiing, 29% in freestyle skiing, and 19% in snowboarding. Interestingly, the incidence of knee injuries was roughly the same for ice and snow sports in Beijing 2022, which can be inferred as a consequence of changes in environmental factors, venue or track design disparities, competition rules, or changes in equipment.
In approximately 60% of injuries during Beijing 2022, strain, impingement, and contusion were diagnosed as the top three injury types. In the PyeongChang 2018 Olympic Winter Games, the top three injury types were contusion, sprain, and laceration, accounting for approximately 28.5%, 13.0%, and 9.8% of all injuries, respectively.[3] We found that skating sports caused the highest number of injuries, regardless of whether the knee was the primary injury location or strain was the primary injury type. Moreover, injuries during competition (n=95, 91.4%) accounted for the largest proportion of skating sports. High-speed sports, such as short track skating and speed skating, in which multiple athletes participated at the same time, were competitive and led to a higher risk of injury.
Injury surroundings and severities
Injuries were unevenly distributed between training and competition (33.7% vs. 52.5%), and the results differed from those of PyeongChang 2018 (48% vs. 46%), Sochi 2014 (63% vs. 35%), and Vancouver 2010 (54% vs. 46%). Ice hockey was the only sport in Sochi 2014 and PyeongChang 2018 in which injuries occurred more commonly in competition than in training, as was the case in Beijing 2022. These results correspond with earlier findings.[14-15] Ice hockey is a team sport with a lot of physical contact, and its intensity, speed, and likelihood of causing fatigue are much higher in competition than in training, resulting in athletes needing much time for recovery.
In a major sporting event such as the Olympic Games, any injury or illness, even if minor in severity and with no time lost, can lead to performance disorders and prevent athletes from achieving their goals, so they are very careful to avoid injuries. Athletes in Beijing 2022 incurred fewer severe injuries (4.3% of injuries were estimated to result in an absence of more than 7 d) than athletes in PyeongChang 2018 and Sochi 2014 (13% and 16%, respectively). These results are comparable to those of Vancouver 2010; however, there was a high percentage of missing data on injury severity in Vancouver 2010.[9] The vast majority of athletes with an absence of more than 7 d had knee and spinal injuries. As knee and spinal injuries often result in long absences from training and competition, the prevention of spinal cord injury, spinal fracture, and severe knee ligament sprains, including injuries of the anterior cruciate ligament, is important.
EMS of injury
An important task of medical services in sports events is to establish transportation and treatment systems for severely injured athletes. The reported rates of transportation to a hospital by ambulance during the Olympic Winter Games were 1.5% in Calgary 1998, 3.2% in Salt Lake City 2002, and 2.8% in Torino 2006.[16⇓-18] In the Sapporo AWG, the rate of athlete transportation was 9.3%.[19] The frequency of ambulance transfer in Beijing 2022 was significantly increased (12.8%, 52 of 406) compared with previous Games. All 52 athletes transported by ambulance were injured, and none were transported owing to illness. The most frequently transferred athletes were snowboard players, followed by ice hockey players. These events were covered by an emergency medical system, which ensured that ambulances were available 24 hours a day at each venue to provide appropriate treatment for all transferred athletes. The risk of injury varies for different sporting events; therefore, these data provide a basis for emergency medical treatment at major sporting events.
Illnesses in the Olympic sports
The incidence of illnesses in Beijing 2022 was significantly lower than those of PyeongChang 2018 and Sochi 2014 (2.8% of all athletes affected in Beijing vs. 9% in PyeongChang and 8% in Sochi[2-3]). Furthermore, the PyeongChang illness incidence differed between female and male athletes, with slightly more women (57.5%, 46 of 80) than men (42.5%, 34 of 80) competing but with women in PyeongChang experiencing 61% more illnesses than men. These disproportionate rates have previously been reported in the Rio 2016 Paralympic Games[20] and the 2009 Athletics and Aquatics World Championships.[21,22]
Regarding the type of illnesses, according to previous reports, respiratory infections have accounted for a high proportion of illnesses in other elite sport events over the years.[2,3,20⇓⇓⇓⇓⇓⇓⇓-28] However, there were only three cases of respiratory problems in Beijing 2022. A total of 50 illnesses (62.5%) were attributed to dentistry and ophthalmology/otolaryngology. Beijing 2022 was the second Games held amid the COVID-19 pandemic. To prevent the transmission of COVID-19 during the Games, organizers of Beijing 2022 formulated scientifically sound and pragmatic countermeasures. In particular, an innovative “closed loop” system[29] was used; participants and venues were classified according to high, medium, and low risk levels and 12 stringent countermeasures were formulated. These included: a) requiring participants to be fully vaccinated at least 14 d prior to their departure for China and b) mandatory 21-day quarantine for those not fully vaccinated upon arrival in Beijing. As a result, the incidence of respiratory diseases, such as respiratory infections, declined significantly. We consider that this was also the main reason for the decrease in medical treatment of athletes owing to illnesses during the Beijing 2022 Games.
Limitations
Regarding study limitations, such as the statistical classification of the preliminary design data not being detailed enough and the training of data entry personnel not being comprehensive enough due to the COVID-19 epidemic, some data were missing, which influenced the findings.
CONCLUSIONS
In summary, 11% of competing athletes had a reported medical encounter for a new or recurrent injury, and nearly 3% had at least one illness during the Beijing 2022 Olympic Winter Games. The incidence and characteristics of injuries and illnesses in training and competition varied greatly among different sports. Our results indicate that the type and distribution of injuries and illnesses among athletes changed owing to the COVID-19 pandemic. Our findings provide the basis for further studies on the etiology of injuries and illnesses among elite athletes. Moreover, as the COVID-19 pandemic continues around the world, the “closed loop” system also provides a reference for large-scale sporting events in the future.
ACKNOWLEDGMENT
We thank all the medical staff for their efforts to save the patient during the Beijing 2022 Olympic Winter Games, and we thank all patients involved in this study.
Funding: This study was supported by the Beijing Municipal Science and Technology Project (Z191100004419003), Capital’s Funds for Health Improvement and Research (2022-1-3031, 2022-2-3033), and Beijing Public Health High-level Scholars Development Program (2022-1-001).
Ethical approval: The study was approved by the Ethics Committee of Beijing Emergency Medical Center (No. 2022-4-003) and the requirement for written informed consent was waived. Under the terms of the approval, studies must undergo independent scientific review. Following approval, members of the research team were authorized to access the raw data for this study, which was granted permission by the Ethics Committee of Beijing Emergency Medical Center. The data used in this study were anonymized before use.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Contributors: PDH, DG and JL (Jie Liu) contributed equally to this work. JJZ conceived the study idea for this article; PDH, DG and JL (Jie Liu) wrote the first draft; JL (Jing Luo), LXZ, and HXL collected data; SJT and SMN analyzed data; JJZ and YW suggested critical revisions. All authors were dedicated to the emergency medical services of the Beijing 2022 Olympic Winter Games. All authors have read and approved the final version of the manuscript and agreed with the order of presentation of the authors.
Reference
Sports injuries and illnesses in the Sochi 2014 Olympic Winter Games
DOI:10.1136/bjsports-2014-094538 URL [Cited within: 3]
Sports injury and illness incidence in the PyeongChang 2018 Olympic Winter Games: a prospective study of 2914 athletes from 92 countries
DOI:10.1136/bjsports-2018-100236 URL [Cited within: 6]
More data needed on injury risk among young elite athletes
DOI:10.1136/bjsm.2010.073833 URL
Major trauma in winter sports: an international trauma database analysis
Vascular injury is associated with increased mortality in winter sports trauma
DOI:10.1016/j.avsg.2014.10.003
PMID:25449983
[Cited within: 1]

Trauma is the leading cause of injury and death for individuals aged 1-44 years. Up to 8% of the US population participates in winter sports, and although vascular injuries are uncommon in these activities, little is published in this area. We sought to identify the incidence, injury patterns, and outcomes of vascular injuries resulting from winter sports trauma.Patients with winter sports trauma and the subset with vascular injuries were identified by accessing the National Trauma Data Bank querying years 2007-2010. Patients with and without vascular injuries were then compared. Admission variables included transport time, emergency department hypotension (systolic blood pressure < 90), Glasgow Coma Scale ≤ 8, Injury Severity Score ≥ 25, fractures, solid organ injury, and vascular injury. Outcomes were analyzed and associations with vascular injuries were determined.A total of 2,298 patients were identified with winter sports-related trauma and 28 (1.2%) had associated vascular injuries. Overall, the top 3 injuries were head trauma (16.7%), thoracic vertebral fractures (5.5%), and lumbar vertebral fractures (5.1%). The most common associated vascular injures were to the popliteal artery (17.7%), splenic artery (14.7%), and brachial blood vessels (14.7%). In the entire cohort, 1 patient (0.04%) suffered an amputation and 15 patients (0.7%) died. There were no amputations in the vascular injury group. Mortality was 0.6% in patients without a vascular injury compared with 7.1% of those with a vascular injury (P = 0.01).Although vascular injury is an uncommon associated finding in winter sports trauma, it is associated with a significant increase in mortality. These findings highlight the need for rapid identification of traumatic vascular injuries, which predicts worse overall outcomes in this patient population.Copyright © 2015 Elsevier Inc. All rights reserved.
Injuries in men’s international ice hockey: a 7-year study of the International Ice Hockey Federation Adult World Championship Tournaments and Olympic Winter Games
DOI:10.1136/bjsports-2014-093688 URL [Cited within: 1]
Injury surveillance in multi-sport events: the International Olympic Committee approach
DOI:10.1136/bjsm.2008.046631 URL [Cited within: 1]
Sports injuries and illnesses during the Winter Olympic Games 2010
DOI:10.1136/bjsm.2010.076992 URL [Cited within: 2]
Sports injuries and illnesses during the London Summer Olympic Games 2012
DOI:10.1136/bjsports-2013-092380 URL [Cited within: 1]
Sports injuries during the summer Olympic games 2008
DOI:10.1177/0363546509339357
PMID:19783812
[Cited within: 1]

Standardized assessment of sports injuries provides important epidemiological information and also directions for injury prevention.To analyze the frequency, characteristics, and causes of injuries incurred during the Summer Olympic Games 2008.Descriptive epidemiology study.The chief physicians and/or chief medical officers of the national teams were asked to report daily all injuries newly incurred during the Olympic Games on a standardized injury report form. In addition, injuries were reported daily by the physicians at the medical stations at the different Olympic venues and at the polyclinic in the Olympic Village.Physicians and/or therapists of 92 national teams covering 88% of the 10,977 registered athletes took part in the study. In total, 1055 injuries were reported, resulting in an incidence of 96.1 injuries per 1000 registered athletes. Half of the injuries (49.6%) were expected to prevent the athlete from participating in competition or training. The most prevalent diagnoses were ankle sprains and thigh strains. The majority (72.5%) of injuries were incurred in competition. One third of the injuries were caused by contact with another athlete, followed by overuse (22%) and noncontact incidences (20%). Injuries were reported from all sports, but their incidence and characteristics varied substantially. In relation to the number of registered athletes, the risk of incurring an injury was highest in soccer, taekwondo, hockey, handball, weightlifting, and boxing (all >or=15% of the athletes) and lowest for sailing, canoeing/kayaking, rowing, synchronized swimming, diving, fencing, and swimming.The data indicate that the injury surveillance system covered almost all of the participating athletes, and the results highlight areas of high risk for sport injury such as the in-competition period, the ankle and thigh, and specific sports. The identification of these factors should stimulate future research and subsequent policy change to prevent injury in elite athletes.
Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic Summer Games: a prospective study of 11274 athletes from 207 countries
DOI:10.1136/bjsports-2017-097956 URL [Cited within: 1]
Injuries among World Cup ski and snowboard athletes
DOI:10.1111/j.1600-0838.2010.01147.x URL [Cited within: 1]
A prospective study of concussions among National Hockey League players during regular season games: the NHL-NHLPA Concussion Program
DOI:10.1503/cmaj.092190
PMID:21502355

In 1997, the National Hockey League (NHL) and NHL Players' Association (NHLPA) launched a concussion program to improve the understanding of this injury. We explored initial postconcussion signs, symptoms, physical examination findings and time loss (i.e., time between the injury and medical clearance by the physician to return to competitive play), experienced by male professional ice-hockey players, and assessed the utility of initial postconcussion clinical manifestations in predicting time loss among hockey players.We conducted a prospective case series of concussions over seven NHL regular seasons (1997-2004) using an inclusive cohort of players. The primary outcome was concussion and the secondary outcome was time loss. NHL team physicians documented post-concussion clinical manifestations and recorded the date when a player was medically cleared to return to play.Team physicians reported 559 concussions during regular season games. The estimated incidence was 1.8 concussions per 1000 player-hours. The most common postconcussion symptom was headache (71%). On average, time loss (in days) increased 2.25 times (95% confidence interval [CI] 1.41-3.62) for every subsequent (i.e., recurrent) concussion sustained during the study period. Controlling for age and position, significant predictors of time loss were postconcussion headache (p < 0.001), low energy or fatigue (p = 0.01), amnesia (p = 0.02) and abnormal neurologic examination (p = 0.01). Using a previously suggested time loss cut-point of 10 days, headache (odds ratio [OR] 2.17, 95% CI 1.33-3.54) and low energy or fatigue (OR 1.72, 95% CI 1.04-2.85) were significant predictors of time loss of more than 10 days.Postconcussion headache, low energy or fatigue, amnesia and abnormal neurologic examination were significant predictors of time loss among professional hockey players.
The epidemiology of professional ice hockey injuries: a prospective report of six NHL seasons
Level of medical care required for mass gatherings: the XV Winter Olympic Games in Calgary, Canada
The epidemiology of illness and injury at the alpine venues during the Salt Lake City 2002 Winter Olympic Games
PMID:16567258
[Cited within: 1]

The Emergency Medicine literature has described levels of medical care for mass gatherings in the United States, including for the Los Angeles 1984 Summer and Calgary 1988 Winter Olympic Games. However, there are limited data to describe the type and number of illness or injury that may occur during mass gatherings in an alpine winter environment. To describe the epidemiology of illness and injury seen among spectators at the alpine and snowboarding venues during the Salt Lake City 2002 Winter Olympic Games, we conducted a retrospective review of the Salt Lake City 2002 Olympic Medical Care database for all patient encounters during the operational period of the Games at the alpine and snowboarding venues. The three venues included were: Deer Valley Resort (DVR), Park City Mountain Resort (PCM), and Snowbasin Resort (SBA). Each venue had a medical clinic located on site for spectators and another for athletes. Physicians, nurses, emergency medical technicians, and therapists staffed the clinics. The database was created by Inter-mountain Health Care (IHC) in conjunction with Salt Lake City 2002 Winter Olympic staff and consisted of descriptive reports of all patient encounters from all venues including demographic, epidemiology, and outcome information. IHC maintains the database, and was the sole medical provider for the Games. Each venue had at least 6 days of competition events. Over the 19 days of the Olympiad, a total of 410,160 spectators and 3,961 competitive athletes attended the three venues. There were 841 spectators evaluated and treated at the venue clinics, and mobile medical staff treated 262 spectators. The top five spectator clinic diagnostic categories were: sprain/strain (n=108), miscellaneous trauma (n=103), respiratory (n=88), miscellaneous medical (n=69), and digestive (n=52). Fifty spectators required transport to a hospital for additional care: 27 required transfer by ground ambulance and the remainder were transported by private vehicle. The overall spectator medical utilization rate was 26.9. In conclusion, the rate and acuity of patients seen at the alpine venues during the 2002 Winter Olympic Games was low. Nevertheless, we recommend full on-site physician and nurse staffing with advanced trauma and cardiac life support available during similar events.
Torino 2006 Winter Olympic Games: highlight on health services organization
DOI:10.1016/j.jemermed.2009.08.028
PMID:19879085
[Cited within: 1]

Mass gatherings require attention toward planning and execution of dedicated medical care.The aims were to describe the organization and provision of medical care in the Torino 2006 Winter Olympic Games in light of the epidemiology of illnesses and injuries among athletes during this event.The organization integrated 18 medical centers operating at Olympic venues, three polyclinics inside the Olympic Villages, and 13 pre-existing Olympic Hospitals. The design was a retrospective study, with review of medical records at Olympic medical facilities. All the athletes who attended any medical center or polyclinic were eligible. The main outcomes included type of injuries and illnesses affecting athletes, incidence of injuries and illnesses by provenance and discipline, and rate of hospital admissions.A total of 330 athletes received medical care and 676 medical encounter forms were documented, with an overall medical utilization rate of 12.66%. Skeleton, snowboard, bobsleigh, and alpine and freestyle skiing had the highest medical attendance rate relative to other disciplines (p < 0.001). The majority of injuries and illnesses were of a minor nature. A total of 23 visits required hospital admissions (3.40%).The described model of medical coverage for such events seemed to be practical and efficient for the athletes, without depleting services to the general population. The risk of severe injury and illness seemed to be low. These data could be useful for planning medical services in future mass gatherings.Copyright © 2010 Elsevier Inc. All rights reserved.
Medical services at the 2017 Sapporo Asian winter games: injury and illness epidemiology at a 34 -nation multisport event
DOI:10.1136/bjsports-2018-099061 URL [Cited within: 1]
Sport, sex and age increase risk of illness at the Rio 2016 Summer Paralympic Games: a prospective cohort study of 51 198 athlete days
DOI:10.1136/bjsports-2017-097962 URL [Cited within: 2]
Occurrence of injuries and illnesses during the 2009 IAAF World Athletics Championships
DOI:10.1136/bjsm.2010.078030 URL [Cited within: 2]
Sports injuries and illnesses in the 2009 FINA World Championships (Aquatics)
DOI:10.1136/bjsm.2010.071720 URL [Cited within: 2]
Illness data from the US open tennis championships from 1994 to 2009
Sport injuries and illnesses during the first Winter Youth Olympic Games 2012 in Innsbruck, Austria
DOI:10.1136/bjsports-2012-091534 URL [Cited within: 1]
Elite athletes travelling to international destinations >5 time zone differences from their home country have a 2-3-fold increased risk of illness
DOI:10.1136/bjsports-2012-091395 URL [Cited within: 1]
Illness during the 2010 Super 14 Rugby Union tournament - a prospective study involving 22 676 player days
DOI:10.1136/bjsports-2012-091046 URL [Cited within: 1]
Illness and injuries in elite football players—a prospective cohort study during the FIFA Confederations Cup 2009
DOI:10.1097/JSM.0b013e31828b0a10 URL [Cited within: 1]
Sports injuries and illnesses during the second Asian Beach Games
DOI:10.1136/bjsports-2011-090852 URL [Cited within: 1]
Risk management strategies for the 2022 Olympic Winter Games: the Beijing scheme
DOI:10.1016/j.jshs.2022.02.006 URL [Cited within: 1]