INTRODUCTION
Trauma is a major medical and public health problem in many countries, and at least 5.8 million people die due to severe trauma every year.[1] Troponin I (TnI) is a specific indicator of myocardial injury, and up to 70% of patients with blunt chest trauma have increased levels of TnI, which plays an important role in blunt cardiac injury (BCI) diagnosis; however, there are various reasons for its increase, including hypotensive shock, traumatic brain injury, hypoxemia, and others.[2] Therefore, BCI diagnosis cannot be solely based on an increase in the TnI level. Nevertheless, the TnI has a high value in the screening and excluding BCI, and the Eastern Association for the Surgery of Trauma guidelines recommends patients suspected of BCI to undergo electrocardiogram (ECG) and TnI assessment.[3] However, the trend of TnI changes in trauma patients is rarely reported, and there is no regulation regarding the monitoring time of TnI. There is a controversy regarding the prognostic value of TnI.[4,5] Briefly, there is no conclusion on the changes and clinical values of TnI; therefore, we aim to explore the changes and clinical significance of serum TnI in trauma patients.
METHODS
Study participants
This study was a retrospective analysis. The inclusion criterion was as follows: consecutive trauma patients admitted to our trauma center between July 1, 2017 and July 31, 2020.
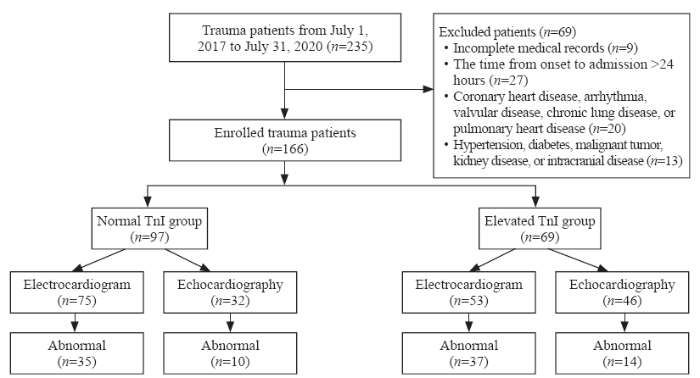
Exclusion criteria were as follows: (1) incomplete records; (2) time from onset to admission >24 hours; (3) previous cardiac diseases, such as coronary heart disease, arrhythmia, valvular disease, pulmonary heart disease; and (4) hypertension, diabetes, malignant tumors, kidney disease, and intracranial disease (Figure 1).
Figure 1.
Figure 1.
Flowchart showing the enrollment and exclusion processes.
Study design
Data on the general demographic characteristics, Injury Severity Score (ISS), TnI levels within 7 days after trauma, other laboratory examinations, ECG, echocardiography, computed tomography or magnetic resonance imaging, length of intensive care admission and hospitalization, mechanical ventilation time, and outcome of patients, along with other aspects, were collected.
ECG abnormalities included the following factors: arrhythmia (sinus bradycardia/bradycardia, premature beats, supraventricular tachycardia, atrial fibrillation, bundle branch block, and QT interval prolongation), ST-segment depression or elevation >1 mm, and T wave flat and/or inversion.[4] Echocardiographic abnormalities included the following factors: pericardial effusion, local ventricular wall motion abnormalities, acute valve dysfunction, ventricular enlargement, ventricular septal rupture, and heart thrombosis.[6] In our study, patients with elevated TnI and abnormal ECG and/or echocardiography findings were diagnosed with BCI.
Patients were divided into elevated and normal TnI groups according to whether they had increased TnI levels (≥0.04 ng/mL) within 24 hours of admission. Clinical characteristics were subsequently compared and analyzed. A graph depicting a change in trend was drawn according to TnI levels on admission, on reaching a peak point, and 7 days after admission. Patients were divided into survival and death groups. The age, sex, ISS, lactic acid level, creatinine level, diagnosis of BCI, TnI level on admission, and abnormal TnI on day 7 were included in the comparative study, and significant differences were found. Finally, we analyzed the independent correlation factors related to in-hospital mortality.
Statistical analyses
SPSS statistical software (version 22.0; IBM Corp, USA) was used for data processing. Data are presented as mean±standard deviation. Two independent sample t-tests were used to compare parameters between the groups. Furthermore, the Chi-square test was used to compare both groups, and a logistic regression analysis was performed to analyze factors related to binary variables. The P-value <0.05 was considered statistically significant.
RESULTS
During our study, there were 235 trauma patients; 36 patients were excluded because they had incomplete data or the time from onset to admission was over 24 hours; 33 patients with a history of cardiac and other chronic diseases were also excluded. Finally, 166 trauma patients were included. Sixty-nine (41.57%) patients had elevated TnI levels, whereas 97 patients had normal TnI values. Compared with the normal TnI group, the ISS and lactic acid level were higher, the heart rate was faster, and systolic blood pressure was lower in the elevated TnI group (Table 1).
Table 1 Baseline characteristics of patients with trauma
| Parameters | Elevated TnI group (n=69) | Normal TnI group (n=97) | Statistics | P |
|---|---|---|---|---|
| Age, years | 47.59±19.12 | 50.33±15.08 | 6.55 | 0.325 |
| Male, n (%) | 58 (84.04) | 65 (67.01) | 6.10 | 0.010 |
| Injury Severity Score | 31.62±14.55 | 19.16±8.26 | 25.26 | 0.000 |
| Injury type, n (%) | ||||
| Traumatic brain injury | 30 (43.47) | 37 (38.14) | 0.48 | 0.298 |
| Traumatic chest injury | 49 (71.01) | 50 (51.54) | 6.34 | 0.009 |
| Traumatic abdominal injury | 26 (37.68) | 23 (23.71) | 3.46 | 0.046 |
| Traumatic bone injury | 52 (75.36) | 56 (57.73) | 4.78 | 0.021 |
| Heart rate, beats/minute | 98.94±25.43 | 82.40±15.30 | 27.80 | 0.000 |
| Systolic blood pressure, mmHg | 115.43±32.51 | 129.85±20.67 | 21.10 | 0.001 |
| Hemoglobin, g/L | 115.94±29.48 | 131.13±21.06 | 11.76 | 0.000 |
| Creatinine, µmol/L | 96.54±42.02 | 70.53±31.89 | 10.88 | 0.000 |
| Lactic acid, mmol/L | 3.56±2.96 | 1.49±0.98 | 43.61 | 0.000 |
| Troponin, ng/mL | 0.57±1.34 | 0.01±0.01 | 28.13 | 0.000 |
| Creatine kinase-myocardial band, ng/mL | 30.13±35.55 | 10.19±21.615 | 26.75 | 0.000 |
| Myoglobin, ng/mL | 1,196.30±1,289.60 | 269.38±321.65 | 97.38 | 0.000 |
| ST-T changes, n | 7 | 10 | 0.00 | 0.984 |
| Right bundle branch block, n | 2 | 5 | 0.50 | 0.478 |
| QT interval prolongation, n | 2 | 2 | 0.13 | 0.723 |
| Supraventricular tachycardia, n | 3 | 0 | 4.35 | 0.069 |
| Atrial fibrillation, n | 2 | 1 | 0.81 | 0.760 |
| Sinus bradycardia, n | 7 | 6 | 0.92 | 0.337 |
| Sinus tachycardia, n | 18 | 8 | 11.97 | 0.001 |
| Premature beats, n | 3 | 3 | 0.19 | 0.989 |
| Valve regurgitation, n | 13 | 10 | 0.08 | 0.776 |
| Ventricular wall motion abnormalities, ventricular enlargement, n | 2 | 0 | 1.43 | 0.510 |
| Pericardial effusion, n | 1 | 0 | 0.71 | 0.401 |
| Hospitalization, days | 23.39±26.08 | 13.15±8.54 | 18.84 | 0.000 |
| Intensive care duration, days | 20.70±26.06 | 7.89±6.83 | 20.11 | 0.000 |
| Ventilator use time, hours | 222.78±319.92 | 42.15±125.50 | 26.01 | 0.000 |
| In-hospital mortality, n (%) | 10 (14.49) | 0 (0) | 14.81 | 0.000 |
Abnormal ECGs were found in 56.25% (72/128) of the trauma patients and were more frequent in the elevated TnI group than in the normal TnI group (69.81% vs. 46.67%, P<0.05). Arrhythmia (48.43%, 62/128) was the most common cardiac disease among the patients in this study, followed by ST-T abnormalities (13.28%, 17/128). Nevertheless, there were no significant differences in the rate of echocardiographic abnormalities between the groups (30.43% [14/46] in TnI elevated group vs. 31.25% [10/32] in normal TnI group, P>0.05). Valve regurgitation was the leading abnormal finding on bedside echocardiography, but there was no hemodynamic instability caused by acute valve dysfunction, which required emergency surgery.
In this study, 40 patients met the diagnosis of BCI, with an incidence rate of 24.10% (40/166), and 8 patients had abnormalities on ECG and echocardiography. The all-cause mortality in these patients was 25%. Compared with the normal TnI group, the average hospital stays, intensive care time, and mechanical ventilation time were longer, and the in-hospital mortality was higher in the elevated TnI group (Table 1).
The TnI level of trauma patients gradually increased after admission (1.346±0.569 ng/mL), peaked at 48 hours (7.804±1.537 ng/mL), and gradually decreased within 7 days after trauma (0.579±0.159 ng/mL), but the TnI levels of some patients (n=13) did not return to baseline values. TnI levels of patients in the normal TnI group did not elevate within 24 hours and continued to be normal for 1 week (supplementary Figure 1).
All trauma patients were divided into survival and death groups, and there were differences in ISS, abnormal TnI on day 7, lactic acid level, creatinine level, and whether BCI was diagnosed between the two groups (P<0.05) (Table 2). Further, logistic regression analysis revealed that TnI abnormality on day 7 and the lactic acid level were independently correlated with in-hospital mortality, but the TnI level on admission did not play a role in predicting the prognosis (Table 3).
Table 2 Comparative analysis of possible death-related factors in trauma patients
| Parameters | Death group (n=10) | Survival group (n=156) | Statistics | P |
|---|---|---|---|---|
| Age, years | 45.50±23.35 | 49.34±16.51 | 1.92 | 0.488 |
| Male, n (%) | 8 (80.00) | 115 (73.71) | 0.17 | 0.973 |
| ISS score | 41.56±21.23 | 23.18±11.88 | 9.87 | 0.000 |
| Hemoglobin, g/L | 112.90±34.17 | 126.07±25.09 | 1.49 | 0.117 |
| Creatinine, µmol/L | 122.00±75.75 | 77.94±33.41 | 27.60 | 0.000 |
| Lactic acid, mmol/L | 7.53±5.08 | 2.05±1.58 | 84.92 | 0.000 |
| Troponin on admission, ng/mL | 0.62±1.08 | 0.22±0.89 | 2.41 | 0.117 |
| Abnormal troponin after 7 days, n | 6 | 7 | 40.12 | 0.000 |
| Number of blunt cardiac injury patients, n | 10 | 30 | 33.52 | 0.000 |
Table 3 Factors related to in-hospital mortality
| Parameters | B value | Wald value | Odds ratio | 95% confidence interval | P |
|---|---|---|---|---|---|
| Abnormal troponin at 7 days | -2.896 | 8.133 | 0.055 | 0.008-0.404 | 0.004 |
| Troponin on admission | -3.263 | 1.253 | 0.038 | 0.000-11.604 | 0.263 |
| Lactic acid level | 0.466 | 0.212 | 1.594 | 1.053-2.413 | 0.028 |
DISCUSSION
In our study, patients with elevated TnI had higher ISS and lactic acid levels, faster heart rate, and lower systolic blood pressure on admission, reflecting that the patients in this group were more serious. Hajsadeghi et al[7] found that critically ill patients were more likely to be exposed to shock, anemia, tachycardia, and other factors that may cause myocardial hypoxia, which led to the release of TnI. They considered that critically ill patients had an increased risk of cardiomyocyte damage; our research also reflected indirectly that the risk and degree of cardiomyocyte damage in severely traumatized patients were high.
BCI can damage the cardiac conduction system and cause structural damage.[8] The clinical manifestations of BCI vary, ranging from asymptomatic ECG changes to life-threatening cardiac complications, and there is no gold standard for diagnosis, making early identification difficult. According to a previous study,[9] the incidence of BCI ranged from 8% to 76%, largely owing to the different diagnostic criteria. In this study, the incidence rate of BCI was 24.10%, and the all-cause in-hospital mortality rate was 25%. The diagnosis rate of BCI in the death group was significantly higher than that in surviving patients, but further regression analysis did not show that it was independently related to the in-hospital death. In BCI patients with high ISS and abnormal cardiac structure, once clinical hemodynamic and malignant arrhythmia occurred, even if they could be successfully transported to the hospital, their mortality rate was as high as 80%.[10] However, for patients whose BCI was diagnosed by abnormal TnI and/or ECG, the prognosis was usually good.[11] The majority of patients in this study did not have acute and severe cardiac structural abnormalities; therefore, the overall prognosis was good, and BCI was not an independent risk factor affecting in-hospital death.
Cardiac TnI is an important component of myocardial cell contraction and a specific indicator of heart injury; therefore, it has become a specific biomarker for the clinical diagnosis of myocardial infarction.[12] However, elevated TnI levels are related to many factors, including sex, age, renal insufficiency, heart failure, and trauma.[13] Although the diagnostic criteria for BCI are currently not uniform, TnI greatly contributes to BCI diagnosis, and previous clinical studies depicted that if ECG findings and TnI levels were normal, the predicted value was 100% for clinical exclusion of severe BCI.[14] The current guidelines recommended TnI monitoring for trauma patients with suspected cardiac injury,[3] but the specific monitoring time and clinical significance were still unclear, and there are few reports on the trend of TnI changes in trauma patients. Our study showed that the peak of TnI appeared about 48 hours after admission, and then gradually decreased. Most patients returned to normalcy within 7 days after admission. In contrast, trauma patients whose TnI did not increase within 24 hours continued to be normal in the next week. Therefore, we recommend that for patients with normal TnI immediately after admission, TnI should be monitored for 24 hours. If TnI continues to be normal, the possibility of an increase of TnI is minor. If TnI rises within 24 hours, continued monitoring of TnI levels for 7 days is recommended.
The prognostic value of TnI is still controversial, and a previous clinical study[4] has reported that the release of TnI is not related to the prognosis of trauma patients. However, the retrospective clinical study of Martin et al[15] found that increases in serum TnI were related to the patient’s overall degree of injury and that elevated TnI levels were an independent predictor of mortality in trauma patients admitted to the intensive care unit. Keskpaik et al[16] conducted a clinical study on high-sensitivity cardiac troponin T (hs-cTnT) and found that patients with elevated hs-cTnT levels had a higher ISS, higher lactic acid levels, and lower systolic blood pressure than those with normal TnT on admission. Moreover, vasopressor support was needed during treatment, and hs-cTnT >14 ng/L was associated with increased in-hospital mortality, ventilator use, and longer intensive care time. However, neither our study nor the study by Keskpaik et al[16] could prove that elevated TnI was independently related to poor prognosis, because there were differences in severity between groups. Therefore, we further found the difference between death and survival patients. Through regression analysis, we found that abnormal TnI on day 7 was independently associated with in-hospital mortality. In retrospect, the patients whose TnI levels were still abnormal after 7 days of admission usually had severe trauma; their condition worsened or more severe systemic inflammatory reaction appeared 7 days later, leading to aggravation of ischemia and hypoxia. Therefore, their risk of death was comparatively higher. We believe that changes in TnI but not the baseline TnI level play an important role in predicting the prognosis. The clinical study about TnT in intensive care conducted by Hajsadeghi et al,[7] which monitored the changes of TnT, found that the level of TnT on day 7 could predict the poor prognosis of critically ill patients. These results are in line with the results of our study.
BCI can cause various arrhythmias.[17] We found that 56.25% of patients had abnormal ECG findings. The possible mechanisms of arrhythmia included abnormal perfusion, ischemia, hypoxia, abnormal vagus/sympathetic reflex, and impaired myocardial conduction.[18] ST-T changes were also common in trauma patients,[19] which was caused by local myocardial damage as well as non-traumatic heart disease, hypoxia, electrolyte imbalance, and disease deterioration.[20]
Echocardiography is the first choice for trauma patients who are suspected to have cardiac injury, especially in patients with hemodynamic instability.[3] In our study, valvular regurgitation was a major finding. Because most patients did not have basic echocardiographic data, we could not determine it as trauma-induced valvular regurgitation, especially in patients with no relevant clinical manifestations. Speckle tracking echocardiography is a new technology that can comprehensively evaluate myocardial movement and detect subclinical myocardial injury at the early stages of development, which may improve the positive findings.[21]
This study has some limitations. First, this was a single-center retrospective clinical study with a small amount of data. Second, it was an observational study, and we recommend that further clinical studies be conducted to confirm the findings of this study.
CONCLUSIONS
Elevated TnI is common among trauma patients; TnI has great value in the diagnosis and exclusion of BCI. Trauma patients with elevated TnI levels have longer hospital stays and higher in-hospital mortality. If the TnI does not increase within 24 hours on admission, the chance of increase within 7 days is less, unless the condition worsens. In patients with elevated TnI within 24 hours, the peak occurs at 48 hours after admission, and most patients return to normalcy within 7 days. Failure to recover may be related to an increased risk of death in the hospital. Therefore, we recommend monitoring TnI levels in all trauma patients for 24 hours after admission. If TnI levels increase within 24 hours, monitoring must be continued for 7 days. If TnI does not recover after 7 days, there is a high risk of in-hospital death. Monitoring the changes in serum TnI is very important among trauma patients.
Funding: The study was supported by a grant from the National Key R&D Program of China (2018YFF0301103).
Ethical approval: This study was approved by the Ethics Committee of Peking University People’s Hospital.
Conflicts of interests: The authors declare that they have no competing interests.
Contributors: LWD and TBW conceived, designed the study, analyzed the data, and wrote the paper. JHZ and ZD contributed to data acquisition and analysis.
Reference
Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017
DOI:10.1016/S0140-6736(18)32203-7 URL [Cited within: 1]
Cardiac troponin I as an early prognosis biomarker after trauma: a retrospective cohort study
DOI:S0007-0912(18)30237-X
PMID:29793582
[Cited within: 1]

The significance of cardiac troponin I (cTnI) elevation after trauma is debated. We therefore explored the association between cTnI elevation at admission after trauma and ICU mortality.We performed a retrospective analysis from a prospectively constituted database, of patients admitted to ICU after trauma at a single centre, over a 36 month period. According to cTnI plasma concentration at admission, patients were categorised into three groups: normal (<0.05 ng ml), intermediate (0.05-0.99 ng ml), or high concentration (≥1.0 ng ml). Associations of pre-hospital conditions or cTnI elevation and mortality were analysed by multivariate logistic regression.Among the 994 patients, 177 (18%) had cTnI elevation at ICU admission. Of this total, 114 (11%) patients died in the ICU. The cTnI release was an independent predictor of ICU mortality with a concentration-response relationship [odds ratio (OR) 4.90 (2.19-11.16) and 14.83 (4.68-49.90) for intermediate and high concentrations, respectively] and Day 2 mortality [OR 2.23 (1.18-5.80) and 7.49 (2.77-20.12) for intermediate and high concentrations, respectively]. The severity of thoracic trauma [OR 2.25 (1.07-4.55) and 3.23 (2.00-5.27) for Abbreviated Injury Scale scores 1-2 and ≥3, respectively], out-of-hospital maximal heart rate ≥120 beats min [OR 2.22 (1.32-3.69)], and out-of-hospital shock [OR 2.02 (1.20-3.38)] were independently associated with cTnI elevation.Release of cTnI was an independent predictor of ICU mortality, suggesting that this biomarker can be used in daily practice for early stratification of the risk of ICU death. Thoracic trauma was strongly associated with cTnI elevation.Copyright © 2018 British Journal of Anaesthesia. Published by Elsevier Ltd. All rights reserved.
Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline
DOI:10.1097/TA.0b013e318270193a URL [Cited within: 3]
Incidence and significance of cardiac troponin I release in severe trauma patients
PMID:15564931
[Cited within: 3]

The incidence and significance of troponin I release and its mechanism are unknown in severe trauma patients. The characteristics of this release were prospectively studied in such patients and correlated with presence of shock, existence of myocardial contusion, and outcome.During a 24-month period, serial electrocardiogram recordings and troponin I measurements were performed in all trauma patients admitted at a surgical intensive care unit. The diagnosis of a significant myocardial contusion was made on electrocardiographic criteria. According to the time course of troponin I, three groups of patients were defined a priori: very transient (</= 12 h) and limited release (troponin I < 2 microg/l), transient (</= 36 h) and significant release (troponin I >/= 2 microg/l), and sustained (> 36 h) and significant release (troponin I > 2 microg/l). In the last group, coronary artery angiography was performed.The incidence of troponin I release was 12% (95% confidence interval [CI], 9.6-14.4%) in 728 patients. A significant myocardial contusion was found in 35 patients (5%; 95% CI, 3.4-6.6%) and may occur in the absence of chest trauma and without troponin I release. Sensitivity, specificity, and positive and negative predictive values of troponin I for the diagnosis of myocardial contusion were 63, 98, 40, and 98%, respectively. Troponin I release was observed in 54 early (> 48 h) survivors (7%; 95% CI, 5.6-9.6%) without preexisting coronary artery disease. A sustained and significant release of troponin I (17 patients) was frequently associated with chest trauma (82%) and constantly with electrocardiographic abnormalities. A coronary artery injury was found in 7 patients (2 major and 5 minor vascular injuries) (1% of the whole group; 95% CI, 0.4-2.0%). Mortality was similar in early survivors with (15%; 95% CI, 7-27%) or without (12%; 95% CI, 9-14%) troponin I release. The odds ratio for late mortality was 1.32 (95% CI, 0.61-2.85) in patients with troponin I release.Serial electrocardiogram recordings and troponin I assessments may be proposed for initial screening in high-risk trauma patients to detect anatomical cardiac injuries through the time course of circulating protein. Troponin I release does not have a prognosis value in trauma patients.
Identifying the broken heart: predictors of mortality and morbidity in suspected blunt cardiac injury
DOI:10.1016/j.amjsurg.2015.10.027 URL [Cited within: 1]
Diagnosing cardiac contusion: old wisdom and new insights
PMID:12695446
[Cited within: 1]

Cardiac contusion is usually caused by blunt chest trauma and therefore is frequently suspected in patients involved in car or motorcycle accidents. The diagnosis of a myocardial contusion is difficult because of non-specific symptoms and the lack of an ideal test to detect myocardial damage. Cardiac contusion can cause life threatening arrhythmias and cardiac failure. Many diagnostic methods, such as ECG, biochemical cardiac markers, transthoracic and transoesophageal echocardiography, and radionuclide imaging studies, have been investigated to determine their use in predicting such complications. Recently, cardiac troponin I and T were found to be highly sensitive for myocardial injury. Troponin I and T have also proved to be useful in the stratification of patients at risk for complications. Nevertheless, diagnosis of a cardiac contusion and identification of patients at risk remain a challenge. In this review the current diagnostic tests will be discussed. Also, based on these diagnostic tests, a screening strategy containing data from the latest studies is presented, with the intention of detecting patients at risk.
Association between troponin T and ICU mortality, a changing trend
DOI:10.5830/CVJA-2011-034
PMID:22614659
[Cited within: 2]

Initially elevated levels of troponin predict adverse outcomes in patients admitted to the intensive care unit (ICU). No research team has investigated the changes in concentration of cardiac troponin T (cTnT) during ICU stay and their association with patient outcome.We investigated whether the change in cTnT levels during ICU stay could predict outcomes (death or survival).In this cohort study, all patients admitted to the medical ICU (10 beds) from January to July 2008 were enrolled. Troponin levels were evaluated within the first 24 hours of ICU admission and on the fourth, seventh and 10th days after admission.The study population (135 patients) had a mean age of 60.9 ± 21.5 years. The outcome was significantly different with regard to normal or elevated cTnT concentrations on the first and seventh days of follow up (p = 0.03 and 0.023, respectively). This difference was non-significant for cTnT levels on the fourth and 10th days after admission (p = 0.69 and 0.78, respectively). The change in cTnT levels was not significantly different between the deceased and discharged patients (p = 0.4).Changes in cTnT levels during ICU stay did not show a significant trend (power: 0.26). Patients whose cTnT levels were increased on the first and seventh days of ICU stay had a worse survival, which could be associated with cardiac events on admission or at specific times during the stay in ICU.
Blunt cardiac trauma review
DOI:10.1016/j.ccl.2017.08.010 URL [Cited within: 1]
Cardiac injuries caused by trauma: review and case reports
DOI:S1752-928X(17)30127-0
PMID:28850860
[Cited within: 1]

Assessment of suspected cardiac injuries in a trauma setting is a challenging and time-critical matter, with clinical and imaging findings having complementary roles in the formation of an accurate diagnosis. In this article, we review the supporting literature for the pathophysiology, classification and evaluation of cardiac injuries caused by trauma. We also describe 4 cardiac trauma patients seen at a tertiary referral hospital.Copyright © 2017 Elsevier Ltd and Faculty of Forensic and Legal Medicine. All rights reserved.
Survival following nonpenetrating traumatic rupture of cardiac chambers
PMID:3314758
[Cited within: 1]

We report the cases of 3 patients who survived cardiac chamber rupture resulting from blunt external trauma. All were drivers in motor vehicle collisions. All were seen with signs of pericardial tamponade and were treated by pericardiocentesis followed by emergency thoracotomy performed in the operating room. Ruptures of the right atrium and right and left ventricles were repaired by manual suture techniques without cardiopulmonary bypass. The cases of 37 previously reported patients who survived this injury are reviewed. We believe that patients with cardiac rupture who reach the hospital alive can often be saved by prompt diagnosis and immediate surgical treatment.
Blunt cardiac trauma: a review of the current knowledge and management
DOI:10.1016/j.athoracsur.2014.04.043
PMID:25069684
[Cited within: 1]

Blunt cardiac injuries are highly lethal. A review of the world's English literature on the topic reveals a lack of Level 1 Evidence and few cohesive guidelines for the management of these patients. An online database query was performed using the PubMed medical database. All relevant articles from the past 20 years were reviewed. Conclusions are presented with their corresponding Levels of Evidence.Copyright © 2014 The Society of Thoracic Surgeons. Published by Elsevier Inc. All rights reserved.
Fourth universal definition of myocardial infarction (2018)
The meaning of elevated troponin I levels: not always acute coronary syndromes
DOI:10.1016/j.ajem.2015.09.037
PMID:26508391
[Cited within: 1]

Troponin elevation can be caused by etiologies other than acute coronary syndromes (ACS). Our hypothesis was that elevated troponins occur more frequently in non-ACS cases but that ACS cases (type 1 ST-elevation myocardial infarction [STEMI] and type 1 non-STEMI [NSTEMI]) have significantly higher troponin elevations.This was a cross-sectional cohort analysis of a random subset of all patients with elevated troponins (defined as ≥0.06 ng/mL) over a 1-year period from July 2013 to June 2014. The first positive troponin I and the peak were used in this study. All included patients had medical record reviews looking for whether our cardiologists or hospitalists attributed the elevated troponin to an ACS (NSTEMI or STEMI) or non-ACS cause. Non-ACS causes were categorized as infection, cancer, renal diseases, cardiovascular disease, pulmonary disease, trauma, cardiac arrest, neurologic disease, hypertension, or other. Data were extracted by 2 investigators on the cause of the elevated troponin. Three sessions to educate data extractors were arranged and methods of data extraction discussed, then a 5% sample was reevaluated by the other extractor to determine interrater agreement measures. Parametric data were evaluated with t test and analysis of variance. Dichotomous variables were compared using χ(2) test. Troponin data were evaluated using nonparametric Kruskal-Wallis or Mann-Whitney U. A logistic regression model was created with variables selected a priori to evaluate the predictive ability of these variables in differentiating ACS vs non-ACS causes of elevated troponin.We evaluated 458 randomly selected patients from 1317 unique cases of all patients with initial elevated troponins at least 0.06 mg/mL during the study period. There was 84% interrater agreement in the 5% sampling. Seventy-nine percent had a non-ACS cause of elevated troponin, and the average initial positive troponin I level was significantly lower in the non-ACS cases (0.14; 95% confidence interval [CI], 0.08-0.37) than those with documented STEMI (10.2; 95% CI, 0.75-20.1) or NSTEMIs (0.4; 95% CI, 0.13-1.7). In the non-ACS group, the median initial troponin was 0.14 ng/mL (0.08-0.37 ng/mL). Peak troponin levels were highest in STEMI, next NSTEMI, and lowest in non ACS causes. The most frequent subgroups in the non-ACS group were non-ACS cardiovascular, infectious, renal, or hypertensive causes. In a linear regression model adjusting for age and sex, higher troponin levels had higher odds of being related to ACS causes (adjusted odds ratio, 1.4; 95% CI, 1.2-1.6) than non-ACS causes.The etiology for most initial elevated troponin I levels in a randomly selected population is the result of non-ACS causes. As initial + troponin levels increased, they were more likely associated with ACS causes than with non-ACS causes. Average initial + and peak troponin values were highest in STEMIs, next highest in NSTEMIs, and lowest overall in non-ACS causes.Copyright © 2015. Published by Elsevier Inc.
Stress-induced cardiomyopathy with electrocardiographic ST-segment elevation in a patient with pneumothorax
DOI:10.5847/wjem.j.1920-8642.2020.04.010 URL [Cited within: 1]
Troponin increases in the critically injured patient: mechanical trauma or physiologic stress?
The role of elevated high-sensitivity cardiac troponin on outcomes following severe blunt chest trauma
DOI:S0020-1383(19)30833-2
PMID:31955863
[Cited within: 2]

Blunt cardiac injuries (BCI) result in poor outcomes following chest trauma. Admission ECG and troponin levels are frequently obtained in patients with suspected BCI, nevertheless, the prognostic value of cardiac troponins remains controversial. The purpose of the current study was to review the prognostic value of elevated high-sensitivity cardiac troponin T (hs-cTnT) in patients with severe blunt chest injuries. We hypothesized that elevated hs-cTnT result in poor outcomes in this subgroup of severe trauma patients.After IRB approval, all consecutive patients with Injury Severity Score (ISS) > 15 and chest Abbreviated Injury Scale (AIS) score ≥3 admitted to the major trauma centers between 1/2015 and 6/2017 were retrospectively reviewed. Primary outcomes were in-hospital and one-year mortality. Secondary outcomes included ventilator days and Glasgow Outcome Scale (GOS) score at hospital discharge.Overall, 147 patients were included. Mean age was 49.0 (19.1) years and 75% were male. Serum troponin levels on admission were accrued in 82 (56%) patients with elevated and normal hs-cTnT levels found in 54 (66%) and in 28 (34%) patients, respectively. Elevated hs-cTnT group had significantly higher ISS and lactate level, and lower systolic blood pressure on admission. In-hospital mortality was significantly higher in patients with elevated hs-cTnT levels compared to patients with normal hs-cTnT levels (26% vs. 4%, p = 0.02). Hs-cTnT level > 14 ng/L was significantly associated with extended ventilator days and lower GOS score at hospital discharge.Blunt chest trauma victims with elevated hs-cTnT levels experience significantly poorer adjusted outcomes compared to patients with normal levels. Compliance with EAST practice management guidelines following severe blunt chest trauma was not fully complied in our study cohort that warrants prospective performance improvement measures.Copyright © 2020 Elsevier Ltd. All rights reserved.
Evaluation of noninvasive tests of cardiac damage in suspected cardiac contusion
PMID:6284407
[Cited within: 1]

Nonpenetrating trauma to the chest can result in cardiac damage that may be overlooked because of associated injuries and the lack of obvious thoracic injury. The clinical diagnosis of important cardiac damage in this setting is difficult. We evaluated noninvasive tests for detecting myocardial damage in 100 patients with severe, nonpenetrating chest trauma. The noninvasive tests included serial ECG, serial total CPK and CPK-MB enzymes, continuous Holter monitor recording to detect dysrhythmia, and technetium-99m pyrophosphate scintigraphy. Peak CPK-MB elevations occurred in 72 patients. ECG abnormalities were noted in 70 patients, and 27 patients had Lown grade 3 or greater dysrhythmias. Fifteen patients died and all had autopsies. The noninvasive abnormalities were nonspecific and did not reflect myocardial contusion that led to clinically important cardiac complications.
Inter-ethnic differences in cardiovascular disease: impact on therapies and outcomes
DOI:10.1016/j.jacasi.2021.05.001 URL [Cited within: 1]
Electrocardiographic changes following primary blast injury to the thorax
PMID:11346922
[Cited within: 1]

Profound physiological changes occur following primary blast exposure but the contribution of cardiac arrhythmias is unknown. Thirteen rats, under intravenous anaesthesia, were exposed to a blast wave directed at the thorax (Group II); 10 other animals underwent abdominal blast (Group III) and nine animals acted as controls (Group I). Animals were monitored before, during and after blast exposure. Group II animals demonstrated apnoea, bradycardia and hypotension. No significant physiological changes were seen in Groups I or III. Group II displayed a variety of ECG disturbances, from ventricular extrasystoles to ventricular fibrillation. All abnormalities reverted to sinus rhythm within minutes except in fatally injured animals. These ECG changes probably result from stress wave injury. Significant disturbances might account for some fatalities following primary blast exposure and may exacerbate the triad of apnoea, bradycardia and hypotension. Such observations may have important consequences for the management of blast casualties.
ECG findings in nonpenetrating chest trauma: a review
PMID:3323297
[Cited within: 1]

Significant ECG findings frequently accompany blunt chest trauma. Surface ECG in conjunction with creatinine phosphokinase (CPK) isoenzyme assay, has been an accepted standard for diagnosis of posttraumatic cardiac dysfunction, or "cardiac contusion." Studies employing recently developed noninvasive cardiac imaging techniques have called this practice into question and have shed new light on the pathophysiology of this clinical entity. As a result, it is appropriate to review the ECG manifestations of blunt chest trauma and to reappraise the utility of the ECG in its evaluation. This article will concern itself solely with nonpenetrating cardiac injuries not requiring initial surgical management, since clinical presentation, course, and prognosis differ when operative therapy is indicated.
Speckle tracking analysis of left ventricular systolic function following traumatic brain injury: a pilot prospective observational cohort study
DOI:10.1097/ANA.0000000000000578 URL [Cited within: 1]