Dear editor,
In many cases, ST-segment changes on electrocardiogram (ECG) are suggestive of acute coronary syndrome, but there may be other causes,[1,2] such as stress-induced cardiomyopathy. However, reports of such changes in patients with pneumothorax are very rare.[3,4,5,6,7,8,9,10,11] Here, we report a case of ST-segment elevation due to stress-induced cardiomyopathy in a patient with pneumothorax.
CASE
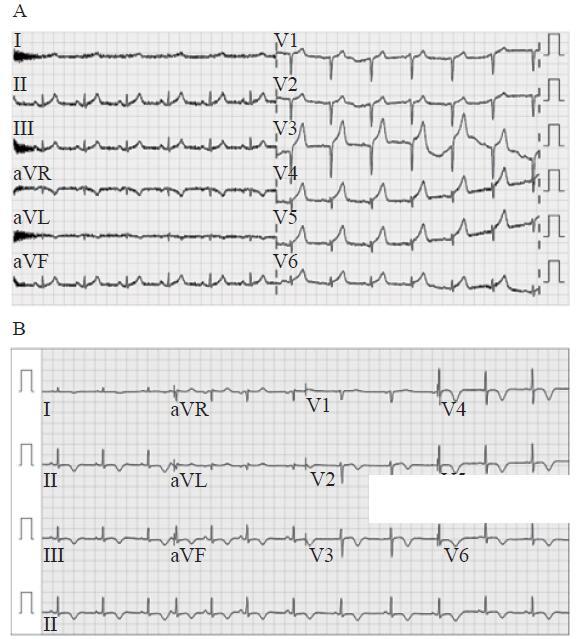
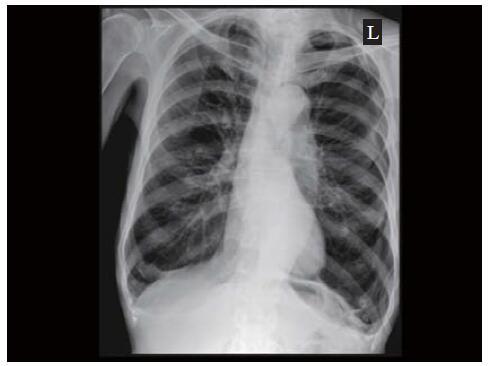
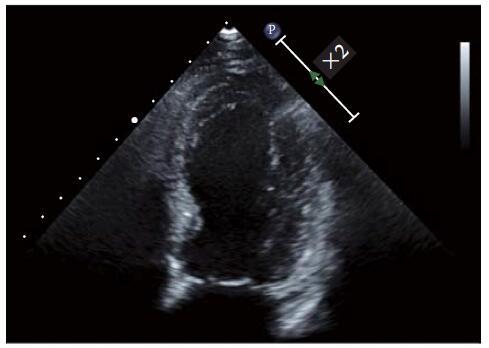
An 81-year-old man was brought to the emergency department (ED) with dyspnea lasting for several hours. He had complained of chest discomfort 2 days before and had a history of hypertension and chronic obstructive pulmonary disease (COPD). Two years prior, he had developed iatrogenic left pneumothorax from an acupuncture needle and had undergone closed thoracostomy. Additionally, he had undergone surgery for gastric cancer 7 years ago. Initially, his blood pressure was 130/80 mmHg, pulse 84/minute, respiration 22/minute, and body temperature 37.2 °C. His oxygen saturation when breathing room air was 92%. Laboratory examination in the ED revealed creatine kinase myocardial band (CK-MB) 1.8 ng/mL (normal 3.6 ng/mL), troponin T high-sensitive (troponin T-hs) test <0.01 ng/mL (normal 0.1 ng/mL), and pro-B-type natriuretic peptide 132.0 pg/mL (normal 32.6-219.9 pg/mL). However, from an initial ECG, ST-segment elevation was seen in the leads II, III, aVF, V3, V4, V5, and V6 (Figure 1), and follow-up assessment of cardiac enzyme showed that CK-MB and troponin T-hs had increased to 5.5 ng/mL and 0.3 ng/mL, respectively. Chest radiography revealed left pneumothorax (Figure 2). Chest computed tomography (CT) revealed an overall emphysematous change in both the lungs. Acute coronary syndrome was suspected, and pneumothorax was resolved by performing closed thoracostomy with 24 Fr chest tube. Although coronary angiography was planned, a coronary CT scan was performed due to the patient’s strong refusal to an angiography. The CT scan did not reveal any specific stenosis, except for calcification of the left anterior descending artery. Transthoracic echocardiography showed hypokinesia of the mid- and apical- segments with sparing movements of the basal segment as typical characteristics of stress-induced cardiomyopathy (Figure 3). The patient was admitted to the general ward and received supportive treatment with chest underwater drainage system in the left pleural space. On follow-up laboratory examinations, cardiac enzymes showed a decreasing tendency with peak CK-MB and high-sensitivity troponin T levels at 7.0 ng/mL and 0.3 ng/mL, respectively, one day after admission to the general ward. The ECG showed changes in the ST-segment elevation to diffuse T-wave inversion. On the 9th day of admission, echocardiography showed that cardiac wall motion returned to be normal. On the 4th day of hospitalization, the chest tube was removed after confirmation of no air leak; however, minimal pneumothorax developed and was absorbed. Finally, the patient was discharged on the 17th day of hospitalization. Further treatments, including pleurodesis, were not considered as it may exacerbate the stress-induced cardiomyopathy.
Figure 1.
Figure 1.
ECG findings at the initial (A) and last follow-up (B).
Figure 2.
Figure 2.
Chest radiography shows the left pneumothorax.
Figure 3.
Figure 3.
Echocardiography shows preserved movement of the basal segment of the left ventricle with decreased movement of apical- and mid-segments, a characteristic sign of stress-induced cardiomyopathy.
DISCUSSION
Stress-induced cardiomyopathy was first introduced in Japan in 1990,[12] and ever since many studies have been conducted.[2] Although the precise pathophysiology remains unclear, catecholamine cardiotoxicity is considered as the most important, with a prevalence of 1.7%-2.2% of patients with acute coronary syndrome.[13] The Mayo Clinic diagnostic criteria were used to diagnose stress-induced cardiomyopathy. These criteria included: new ECG changes or elevated cardiac troponin; absence of coronary artery disease, recent significant head trauma, intracranial bleeding, pheochromocytoma, myocarditis, or hypertrophic cardiomyopathy; and transiently decreased ventricular systolic function extending beyond a single coronary artery.[14] Stress-induced cardiomyopathy shows various patterns on an ECG, and ST-segment elevation is the most common change. T-wave changes, Q-wave, and prolongation of QT interval are also observed. In patients with pneumothorax, changes in the ST-segment in the ECG have been reported for a very long time, even without tension pneumothorax.[3,4,5,6,7,8,9,10,11] Although the mechanism of the ECG changes in pneumothorax has not been clearly identified, there are several hypotheses to explain ECG alterations.[3,4] Pneumothorax may cause a change in the heart position, which can cause ECG changes. More specifically, the air in the retrosternal space can change the distance between the heart and chest wall, which weakens electric conductivity. Alteration of cardiac contraction due to air between the heart and its surroundings also affects ECG baseline voltage, resulting in ST-segment elevation. Most mechanisms described in previous studies elucidated it as the increase in intrathoracic pressure at the time of pneumothorax leading to a decrease in the venous return and increase in the pulmonary vascular resistance, which results in decreasing stroke volume that induces tachycardia with an increased oxygen demand in the myocardium; this makes it similar to ischemic heart disease.
The cause of ST-segment elevation in such patients remains unclear. Although the abnormalities of the ECG are resolved within a short time after resolution of the pneumothorax, as in previously reported cases,[4-8] it may be different for cases in which abnormality of the ECG persisted for a long time, as in our case. Chan et al[11] have reported that only 27% of right-sided pneumothorax recovered to normal ST-segment after closed thoracostomy in 25% of left-sided pneumothorax. Therefore, it may be difficult to identify the reason simply from changes in the ECG. With respect to myocardial enzymes in pneumothorax, normal category values have been reported for most cases.[3-8] Although myocardial enzymes are elevated in some cases of pneumothorax,[10,11] in our case, it could also be due to stress-induced cardiomyopathy. Considering the clinical situation of our case, myocardial enzyme levels were elevated for more than one week, indicating that ST-segment elevation was due to stress-induced cardiomyopathy rather than pneumothorax, as it would have resolved within a short time in the latter case.
Cases of combined pneumothorax and stress-induced cardiomyopathy are rarely reported. After searching in the English literature, only six cases were found to be reported.[13,15-19] A brief analysis of these cases showed that, unlike in our case, all patients were women, with ages ranging from 58.0 to 83.0 years (average 69.5 years). Among these, three had tension pneumothorax, and four had pneumothorax on the right side. All these patients had a history of lung-related diseases. Three patients had COPD, one had asthma, and one had bronchogenic carcinoma. The other one was the oldest patient, aged 83 years old, and had a history of closed thoracostomy with pneumothorax, which occurred more than 50 years prior. All were expected to have limited lung function.
Although there is no scientifically proven mechanism between pneumothorax and stress-induced cardiomyopathy, the possibility of stress and hypoxemia occurring due to pneumothorax can affect the heart.[17] Stress and hypoxemia may induce catecholamine release, which can in turn contribute to cardiac dysfunction. Particularly, stress-induced cardiomyopathy can occur in patients with limited pulmonary function owing to conditions such as COPD, even without tension pneumothorax.
CONCLUSIONS
In conclusion, serial echocardiographic evaluations and a thorough laboratory test for myocardial enzymes are required, and ST-segment elevation in patients with pneumothorax can be caused not only from pneumothorax but also from other heart problems, especially in cases of limited pulmonary function.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: No disclosure.
Contributors: JWC proposed the study and wrote the first draft. Both authors read and approved the final version of the paper.
Reference
ST-segment elevation in conditions other than acute myocardial infarction
DOI:10.1056/NEJMra022580 URL PMID:14645641 [Cited within: 1]
Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review
DOI:10.1093/eurheartj/ehl032
URL
PMID:16720686
[Cited within: 2]

AIMS: To clarify the major features of the apical ballooning syndrome, we performed a systematic review of the existing literature. METHODS AND RESULTS: Review of all relevant case series using the MEDLINE and EMBASE databases resulted in the identification of 14 studies. These studies suggest that the apical ballooning syndrome accounts for approximately 2.0% of ST-segment elevation infarcts, with most cases described in post-menopausal women. The most common clinical presentations are chest pain and dyspnoea, reported in 67.8 and 17.8% of the patients, respectively. Cardiogenic shock (4.2% of the patients) and ventricular fibrillation (1.5%) were not infrequent. ST-segment elevation was reported in 81.6% of the patients, T wave abnormalities in 64.3%, and Q waves in 31.8%. Cardiac biomarkers were usually mildly elevated, as reported in 86.2% of the patients. Typically, patients had left ventricular (LV) dysfunction on admission, with mean ejection fraction ranging from 20 to 49%. However, over a period of days to weeks, all patients experienced dramatic improvement in LV function. The onset of symptoms was often preceded by emotional (26.8%) or physical stress (37.8%). Norepinephrine concentration was elevated in 74.3% of the patients. Prognosis was generally excellent, with full recovery in most patients. In-hospital mortality was 1.1%. Only 3.5% of the patients experienced a recurrence. CONCLUSION: Clinicians should consider this syndrome in the differential diagnosis of patients presenting with chest pain, especially in post-menopausal women with a recent history of emotional or physical stress.
Electrocardiographic changes in spontaneous pneumothorax
DOI:10.1016/j.ijcard.2011.08.057 URL PMID:21911271 [Cited within: 4]
Minimal pneumothorax with dynamic changes in ST-segment similar to myocardial infarction
URL PMID:28438445 [Cited within: 4]
Transient ST elevation associated with tension pneumothorax
DOI:10.1016/s0361-1124(79)80442-6
URL
PMID:533960
[Cited within: 2]

In a 52-year-old man, a spontaneous right tension pneumothorax was associated with transient bradycardia, hypotension and electrocardiogram (ECG) changes consisting of precordial ST elevation suggestive of acute myocardial injury. Immediately after chest tube placement, the ECG reverted to near normal. Serial cardiac enzymes and isoenzymes showed no evidence of myocardial infarction. To our knowledge, this is the first reported case of this association. The ECG changes may be related to the hypotensive state induced by the tension pneumothorax with resulting decreased coronary artery blood flow and myocardial ischemia that resolved without infarction.
Severe transmyocardial ischemia in a patient with tension pneumothorax
DOI:10.1097/00003246-200005000-00065
URL
PMID:10834727
[Cited within: 2]

OBJECTIVE: To report tension pneumothorax (TP) as a cause of severe myocardial ischemia. DESIGN: Clinical case report. SETTING: Medical intensive care unit of a university hospital. PATIENTS: One patient with severe shock attributable to right TP after unsuccessful percutaneous central venous catheterization. INTERVENTIONS: Blood pressure, electrocardiogram (ECG), chest radiograph, and echocardiography during and after shock. MEASUREMENTS AND MAIN RESULTS: On admission the patient was in profound state of shock (heart rate 140 beats/min, blood pressure 65/30 mm Hg). Twelve-lead ECG showed pronounced ST segment elevation in leads II, III, aVF, and V4-V6. Chest radiograph revealed right TP with complete displacement of the mediastinum and the heart to the left side. Immediate right-sided tube thoracostomy resulted in reexpansion of the lung followed by instantaneous hemodynamic and respiratory improvement as well as nearly complete resolution of the ECG changes. Peak value of the creatine phosphokinase was 4140 U/L without significant elevation of the MB isoenzyme at any time. Moreover, the initial hypokinesia of the posterior and lateral left ventricular wall resolved completely, as demonstrated by echocardiography. CONCLUSION: The specific condition of TP may lead to impaired systolic and diastolic coronary artery blood flow affecting ventricular repolarization and T-wave configuration in ECG indicative of transmyocardial ischemia. General symptoms, namely hypotension, tachycardia, and hypoxemia, are likewise typical for cardiogenic shock attributable to myocardial infarction. Yet any therapeutic measure directed toward revascularization, such as thrombolysis or even percutaneous transluminal coronary angioplasty, would have had devastating consequences. Therefore, thorough physical examination of our patient was pivotal in disclosing the true origin of profound shock.
Novel electrocardiographic changes associated with iatrogenic pneumothorax
URL PMID:16823020 [Cited within: 2]
Left spontaneous pneumothorax presenting with ST-segment elevations: a case report and review of the literature
DOI:10.1016/j.hrtlng.2010.09.007
URL
PMID:21320674
[Cited within: 4]

Common electrocardiogram (ECG) changes associated with left-sided pneumothorax include right axis deviation, reduced R-wave amplitude in precordial leads, QRS alterations (amplitude changes), and T-wave inversions. Few reports exist of ST-segment elevations or changes suggestive of acute myocardial infarction (AMI), and these involve older patients with tension pneumothorax and previous coronary heart disease. We report on a young man with no significant medical history, presenting with left-sided spontaneous pneumothorax and ECG changes that included ST-segment elevations and T-wave inversions in the precordial leads, reminiscent of AMI. All changes resolved after decompression of the pneumothorax. On the basis of the patient's presenting symptoms, response to therapy, and our review of the literature, we propose a number of possible mechanisms explaining his electrocardiographic findings.
Changes in electrocardiographic findings after closed thoracostomy in patients with spontaneous pneumothorax
DOI:10.15441/ceem.16.154
URL
PMID:28435901
[Cited within: 2]

OBJECTIVE: We aimed to describe electrocardiographic (ECG) findings in spontaneous pneumothorax patients before and after closed thoracostomy. METHODS: This is a retrospective study which included patients with spontaneous pneumothorax who presented to an emergency department of a tertiary urban hospital from February 2005 to March 2015. The primary outcome was a difference in ECG findings between before and after closed thoracostomy. We specifically investigated the following ECG elements: PR, QRS, QTc, axis, ST segments, and R waves in each lead. The secondary outcomes were change in ST segment in any lead and change in axis after closed thoracostomy. RESULTS: There were two ECG elements which showed statistically significant difference after thoracostomy. With right pneumothorax volume of greater than 80%, QTc and the R waves in aVF and V5 significantly changed after thoracostomy. With left pneumothorax volume between 31% and 80%, the ST segment in V2 and the R wave in V1 significantly changed after thoracostomy. However, majority of ECG elements did not show statistically significant alteration after thoracostomy. CONCLUSION: We found only minor changes in ECG after closed thoracostomy in spontaneous pneumothorax patients.
Transient ST-segment elevation resembling acute myocardial infarction in a patient with a right secondary spontaneous pneumothorax
DOI:10.1016/j.hlc.2012.06.006
URL
PMID:22796089
[Cited within: 3]

A rare cause of ST-segment elevation mimicking myocardial infarction has been reported in the setting of acute pneumothorax. We present a middle-aged woman with a right-sided secondary pneumothorax who developed severe chest pain associated with ST-segment elevation suggestive of acute myocardial infarction. Symptoms resolved immediately after advancement of the dislodged chest drain. A subsequent coronary angiogram was normal. This case highlights an uncommon electrocardiographic alteration and discusses possible pathophysiological mechanisms.
ECG changes with elevated troponin I in a patient with tension pneumothorax
DOI:10.1097/SMJ.0b013e3181aeda06
URL
PMID:19668050
[Cited within: 4]

An 86-year-old man presented with sudden onset of dyspnea during hospitalization. Initial electrocardiography (ECG) showed poor R-wave progression of precordial leads with elevation of troponin I. Tension pneumothorax was subsequently diagnosed and the ECG returned to normal after resolution of clinical compromise.
Takotsubo-type cardiomyopathy due to multivessel spasm
Takotsubo cardiomyopathy in the setting of tension pneumothorax
DOI:10.1155/2015/536931
URL
PMID:26366307
[Cited within: 2]

Background. Takotsubo cardiomyopathy is defined as a transient left ventricular dysfunction, usually accompanied by electrocardiographic changes. The literature documents only two other cases of Takotsubo cardiomyopathy in the latter setting. Methods. A 78-year-old female presented to the ED with severe shortness of breath, hypertension, and tachycardia. On physical exam, heart sounds (S1 and S2) were regular and wheezing was noticed bilaterally. We found laboratory results with a WBC of 20.0 (103/muL), troponin of 16.52 ng/mL, CK-mb of 70.6%, and BNP of 177 pg/mL. The patient was intubated for acute hypoxemic respiratory failure. A chest X-ray revealed a large left-sided tension pneumothorax. Initial echocardiogram showed apical ballooning with a LVEF of 10-15%. A cardiac angiography revealed normal coronary arteries with no coronary disease. After supportive treatment, the patient's condition improved with a subsequent echocardiogram showing a LVEF of 60%. Conclusion. The patient was found to have Takotsubo cardiomyopathy in the setting of a tension pneumothorax. The exact mechanisms of ventricular dysfunction have not been clarified. However, multivessel coronary spasm or catecholamine cardiotoxicity has been suggested to have a causative role. We suggest that, in our patient, left ventricular dysfunction was induced by the latter mechanism related to the stress associated with acute pneumothorax.
Apical ballooning syndrome: an important differential diagnosis of acute myocardial infarction
DOI:10.1161/CIRCULATIONAHA.106.669341 URL PMID:17283269 [Cited within: 1]
Reversible left ventricular dysfunction “takotsubo” cardiomyopathy associated with pneumothorax
DOI:10.1136/heart.87.2.e1
URL
PMID:11796564
[Cited within: 1]

An 83 year old woman presented to the emergency department with chest pain and dyspnoea. Chest radiography showed pneumothorax of the left lung. Arteries were normal on coronary angiography. Left ventriculography showed asynergy of apical akinesis and basal hyperkinesis. Within 18 days, the asynergy improved without any specific treatment. In the present case the left ventricular dysfunction may have been induced by altered catecholamine dynamics as a result of pneumothorax.
Broken lung and broken heart: a case of right pneumothorax resulting in Takotsubo cardiomyopathy
Takotsubo cardiomyopathy secondary to spontaneous right-sided pneumothorax
DOI:10.1136/bcr-2020-236677 URL PMID:32878839 [Cited within: 1]
An unusual presentation of takotsubo cardiomyopathy in a setting of tension pneumothorax
Tension pneumothorax-induced Takotsubo syndrome: A case report
DOI:10.1097/MD.0000000000015190 URL [Cited within: 1]