World Journal of Emergency Medicine ›› 2023, Vol. 14 ›› Issue (4): 294-301.doi: 10.5847/wjem.j.1920-8642.2023.055
• Original Article • Previous Articles Next Articles
Fady Y. Hijji1, Andrew D. Schneider1, Matthew D. Thomas1, Joseph G. Lyons1( ), Daniel D. Bohl2, Jennifer L. Jerele1, Michael J. Prayson1
), Daniel D. Bohl2, Jennifer L. Jerele1, Michael J. Prayson1
Received:2022-08-29
Accepted:2023-02-02
Online:2023-06-30
Published:2023-07-01
Contact:
Joseph G. Lyons
E-mail:joseph.g.lyons@wright.edu
Fady Y. Hijji, Andrew D. Schneider, Matthew D. Thomas, Joseph G. Lyons, Daniel D. Bohl, Jennifer L. Jerele, Michael J. Prayson. Knowledge of radiation exposure associated with common trauma imaging modalities among orthopaedic surgeons, emergency medicine physicians, and general surgeons in the United States[J]. World Journal of Emergency Medicine, 2023, 14(4): 294-301.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2023.055
Table 1.
Physician characteristics (n=218)
| Variables | Number | Percent |
|---|---|---|
| Specialty | ||
| Orthopaedic surgery | 88 | 40.4% |
| Resident | 60 | |
| Attending | 28 | |
| Emergency medicine | 102 | 46.8% |
| Resident | 80 | |
| Attending | 22 | |
| General surgery | 28 | 12.8% |
| Resident | 27 | |
| Attending | 1 | |
| Years in practice | ||
| ≤5 | 164 | 75.2% |
| 6-10 | 11 | 5.1% |
| >10 | 43 | 19.7% |
| Fellowship trained | ||
| No | 187 | 85.8% |
| Yes | 31 | 14.2% |
| Resident education* | ||
| Not involved | 0 | 0.0% |
| Involved | 51 | 100.0% |
| Practice setting | ||
| Academic | 118 | 54.1% |
| Community | 32 | 14.7% |
| Mixed | 68 | 31.2% |
| Region | ||
| East Coast | 83 | 38.1% |
| Midwest | 94 | 43.1% |
| West Coast | 41 | 18.8% |
| Population | ||
| Greater than 3 million | 17 | 7.8% |
| 1-3 million | 55 | 25.2% |
| 300,000-1 million | 84 | 38.5% |
| 100,000-300,000 | 49 | 22.5% |
| 20-100,000 | 13 | 6.0% |
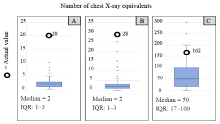
Figure 1.
Box plots of physician estimates of effective radiation dose from pelvic imaging compared with actual values from the literature. The black circles represent the actual values. Median and interquartile range (IQR) values for each imaging study are reported below the respective graph. A: pelvic X-ray (AP); B: hip X-ray (cross-table lateral); C: pelvic CT scan.
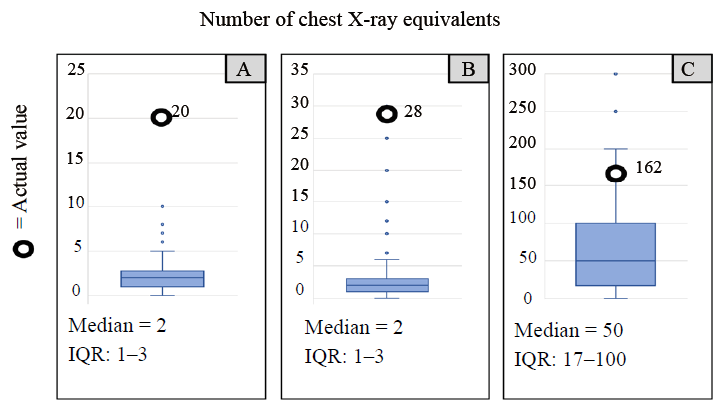
Figure 2.
Box plots of physician estimates of effective radiation dose from lumbar spine imaging compared with actual values from the literature. The black circles represent the actual values. Median and interquartile range (IQR) values for each imaging study are reported below the respective graph. A: lumbar X-rays (two views); B: lumbar CT scan.
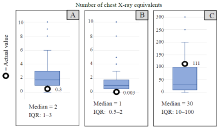
Figure 3.
Box plots of physician estimates of effective radiation dose from lower extremity imaging compared with actual values from the literature. The black circles represent the actual values. Median and interquartile range (IQR) values for each imaging study are reported below the respective graph. A: femur X-ray (AP); B: ankle X-ray (AP); C: lower extremity CT scan.
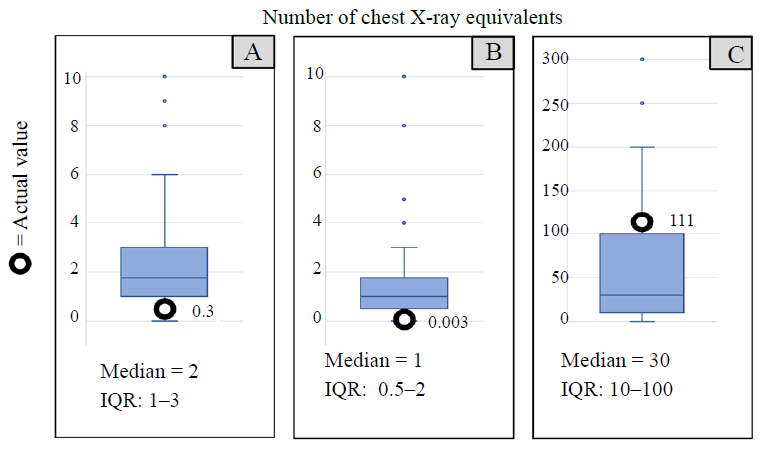
Table 2.
Accuracy of radiation dose estimates by physician characteristics (n=218)
| Variables | Error index* (Mean/Median) | P-valuea |
|---|---|---|
| Specialty | 0.133 | |
| Orthopedic surgery | 997.3/1,007.6 | |
| Non-orthopedic surgeryb | 1,118.4/932.9 | |
| Years in practice | 0.429 | |
| ≤10 | 1,035.1/954.9 | |
| >10 | 1,093.3/995.6 | |
| Fellowship trained | 0.109 | |
| No | 1,028.8/950.4 | |
| Yes | 1,151.9/1,009.4 | |
| Practice setting | 0.526 | |
| Academic | 1,027.6/952.6 | |
| Community | 1,016.0/994.4 | |
| Mixed | 1,093.0/1,000.8 | |
| Region | 0.945 | |
| East Coast | 1,009.2/952.5 | |
| Midwest | 1,116.3/995.9 | |
| West Coast | 960.4/952.9 | |
| Population | 0.076 | |
| >300,000 | 1,030.5/952.6 | |
| ≤300,000 | 1,086.1/1,011.4 | |
| Radiation consideration | 0.928 | |
| ≤50% | 991.1/1,009.4 | |
| >50% | 1,136.4/1,003.9 | |
| Thyroid shield use | 0.179 | |
| ≤50% | 996.0/1,028.1 | |
| >50% | 1,119.7/1,003.2 | |
| Leaded eye wear use | 0.576 | |
| ≤50% | 1,116.8/1,005.1 | |
| >50% | 1,057.7/1,013.9 | |
| Discussion of radiation with imaging | 0.098 | |
| ≤50% | 1,060.8/977.5 | |
| >50% | 911.6/903.9 | |
| Discussion of radiation with procedures | 0.007 | |
| ≤50% | 1,076.3/992.4 | |
| >50% | 896.0/852.4 | |
| Patient declinec | 0.982 | |
| No | 1,098.9/927.4 | |
| Yes | 1,022.4/968.9 |
Table 3.
Physician radiation consideration and disclosure (n=218)
| Questions | Number | Percent* |
|---|---|---|
| How frequently do you consider radiation exposure when using fluoroscopy? | ||
| Always | 63 | 51.6% |
| Most of the time | 35 | 28.7% |
| About half of the time | 7 | 5.7% |
| Sometimes | 16 | 13.1% |
| Never | 1 | 0.8% |
| N/A | 96 | |
| How frequently do you wear a thyroid shield when using fluoroscopy? | ||
| Always | 70 | 56.0% |
| Most of the time | 41 | 32.8% |
| About half of the time | 4 | 3.2% |
| Sometimes | 5 | 4.0% |
| Never | 5 | 4.0% |
| N/A | 93 | |
| How frequently do you wear leaded eye wear when using fluoroscopy? | ||
| Always | 9 | 7.4% |
| Most of the time | 8 | 6.6% |
| About half of the time | 6 | 4.9% |
| Sometimes | 14 | 11.5% |
| Never | 85 | 69.7% |
| N/A | 96 | |
| How frequently is your ability to wear lead affected limited availability in the hospital? | ||
| Always | 8 | 5.7% |
| Most of the time | 15 | 10.6% |
| About half of the time | 9 | 6.4% |
| Sometimes | 56 | 39.7% |
| Never | 53 | 37.6% |
| N/A | 77 | |
| When recommending a patient undergo imaging, how often do you discuss radiation with the patient? | ||
| Always | 2 | 0.9% |
| Most of the time | 19 | 8.7% |
| About half of the time | 31 | 14.2% |
| Sometimes | 125 | 57.3% |
| Never | 41 | 18.8% |
| N/A | 0 | |
| When discussing risk/benefits of a procedure, how often do you discuss radiation risk with the patient? | ||
| Always | 3 | 1.4% |
| Most of the time | 33 | 15.1% |
| About half of the time | 20 | 9.2% |
| Sometimes | 96 | 44.0% |
| Never | 66 | 30.3% |
| N/A | 0 | |
| Has a patient ever declined to undergo imaging because they did not want the radiation? | ||
| No | 68 | 31.2% |
| Yes | 150 | 68.8% |
| 1 |
Vallier HA, Ahmadinia K, Forde FA, Ekstein C, Nash CL Jr, Tornetta P 3rd. Trends in musculoskeletal imaging in trauma patients: how has our practice changed over time? J Orthop Trauma. 2014; 28(10): e236-41.
doi: 10.1097/BOT.0000000000000076 |
| 2 |
Smith-Bindman R, Miglioretti DL, Johnson E, Lee C, Feigelson HS, Flynn M, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012; 307(22): 2400-9.
doi: 10.1001/jama.2012.5960 pmid: 22692172 |
| 3 | Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood). 2008; 27(6): 1491-502. |
| 4 |
Broder JS, Hollingsworth CL, Miller CM, Meyer JL, Paulson EK. Prospective double-blinded study of abdominal-pelvic computed tomography guided by the region of tenderness: estimation of detection of acute pathology and radiation exposure reduction. Ann Emerg Med. 2010; 56(2): 126-34.
doi: 10.1016/j.annemergmed.2009.11.023 pmid: 20074835 |
| 5 |
Bohl DD, Hijji FY, Massel DH, Mayo BC, Long WW, Modi KD, et al. Patient knowledge regarding radiation exposure from spinal imaging. Spine J. 2017; 17(3): 305-12.
doi: S1529-9430(16)30967-6 pmid: 27664337 |
| 6 |
Narain AS, Hijji FY, Yom KH, Kudaravalli KT, Haws BE, Singh K. Radiation exposure and reduction in the operating room: perspectives and future directions in spine surgery. World J Orthop. 2017; 8(7): 524-30.
doi: 10.5312/wjo.v8.i7.524 pmid: 28808622 |
| 7 |
Goodman BS, Carnel CT, Mallempati S, Agarwal P. Reduction in average fluoroscopic exposure times for interventional spinal procedures through the use of pulsed and low-dose image settings. Am J Phys Med Rehabil. 2011; 90(11): 908-12.
doi: 10.1097/PHM.0b013e318228c9dd |
| 8 |
Dewey P, Incoll I. Evaluation of thyroid shields for reduction of radiation exposure to orthopaedic surgeons. Aust N Z J Surg. 1998; 68(9): 635-6.
doi: 10.1111/ans.1998.68.issue-9 |
| 9 |
Bedetti G, Pizzi C, Gavaruzzi G, Lugaresi F, Cicognani A, Picano E. Suboptimal awareness of radiologic dose among patients undergoing cardiac stress scintigraphy. J Am Coll Radiol. 2008; 5(2): 126-31.
doi: 10.1016/j.jacr.2007.07.020 pmid: 18242529 |
| 10 |
Baumann BM, Chen EH, Mills AM, Glaspey L, Thompson NM, Jones MK, et al. Patient perceptions of computed tomographic imaging and their understanding of radiation risk and exposure. Ann Emerg Med. 2011; 58(1): 1-7.e2.
doi: 10.1016/j.annemergmed.2010.10.018 pmid: 21146900 |
| 11 | Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004; 231(2): 393-8. |
| 12 |
Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007; 357(22): 2277-84.
doi: 10.1056/NEJMra072149 |
| 13 |
Prasarn ML, Martin E, Schreck M, Wright J, Westesson PL, Morgan T, et al. Analysis of radiation exposure to the orthopaedic trauma patient during their inpatient hospitalisation. Injury. 2012; 43(6): 757-61.
doi: 10.1016/j.injury.2011.08.026 pmid: 21907988 |
| 14 |
Baskerville JR, Chang JH, Viator M, Rutledge W, Miryala R, Duval KE, et al. Dose versus diagnosis: iatrogenic radiation exposure by multidetector computerised tomography in an academic emergency department with measurement of clinically actionable results and emergently treatable findings. Emerg Med J. 2009; 26(1): 15-9.
doi: 10.1136/emj.2008.059543 pmid: 19104088 |
| 15 |
Edwin A. Don’t lie but don’t tell the whole truth: the therapeutic privilege - is it ever justified? Ghana Med J. 2008; 42(4): 156-61.
pmid: 19452024 |
| 16 |
McCollough CH, Schueler BA. Calculation of effective dose. Med Phys. 2000; 27(5): 828-37.
doi: 10.1118/1.598948 pmid: 10841384 |
| 17 |
Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009; 91(8): 1882-9.
doi: 10.2106/JBJS.H.01199 pmid: 19651945 |
| 18 | Giordano BD, Grauer JN, Miller CP, Morgan TL, Rechtine GR 2nd. Radiation exposure issues in orthopaedics. J Bone Joint Surg Am. 2011; 93(12): e69(1-10). |
| 19 |
Young M, Dempsey M, Rocha Ade L, Podeszwa DA. The cross-table lateral radiograph results in a significantly increased effective radiation dose compared with the Dunn and single frog lateral radiographs. J Pediatr Orthop. 2015; 35(2): 157-61.
doi: 10.1097/BPO.0000000000000231 pmid: 24919137 |
| 20 |
Simpson AK, Whang PG, Jonisch A, Haims A, Grauer JN. The radiation exposure associated with cervical and lumbar spine radiographs. J Spinal Disord Tech. 2008; 21(6): 409-12.
doi: 10.1097/BSD.0b013e3181568656 pmid: 18679095 |
| 21 | Wall B, Haylock R, Jansen J, Hillier MC, Hart D, Shrimpton PC. Radiation risks from medical X-ray examinations as a function of the age and sex of the patient. 2011. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/340147/HPA-CRCE-028_for_website.pdf |
| 22 |
Gower-Thomas K, Lewis MH, Shiralkar S, Snow M, Galland RB, Rennie A. Doctors’ knowledge of radiation exposures is deficient. BMJ. 2002; 324(7342): 919.
doi: 10.1136/bmj.324.7342.919 |
| 23 |
Singh P, Aggarwal S, Singh Kapoor AM, Kaur R, Kaur A. A prospective study assessing clinicians attitude and knowledge on radiation exposure to patients during radiological investigations. J Nat Sci Biol Med. 2015; 6(2): 398-401.
doi: 10.4103/0976-9668.160019 |
| 24 |
Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors’ knowledge of radiation exposure: questionnaire study. BMJ. 2003; 327(7411): 371-2.
doi: 10.1136/bmj.327.7411.371 |
| 25 |
Arslanoğlu A, Bilgin S, Kubal Z, Ceyhan MN, Ilhan MN, Maral I. Doctors’ and intern doctors’ knowledge about patients’ ionizing radiation exposure doses during common radiological examinations. Diagn Interv Radiol. 2007; 13(2): 53-5.
pmid: 17562506 |
| 26 |
Ahmed TAN, Taha S. Radiation exposure, the forgotten enemy: toward implementation of national safety program. Egypt Heart J. 2017; 69(1): 55-62.
doi: 10.1016/j.ehj.2016.10.001 pmid: 29622955 |
| 27 |
Krille L, Hammer GP, Merzenich H, Zeeb H. Systematic review on physician’s knowledge about radiation doses and radiation risks of computed tomography. Eur J Radiol. 2010; 76(1): 36-41.
doi: 10.1016/j.ejrad.2010.08.025 |
| 28 |
Fetterly KA, Mathew V, Lennon R, Bell MR, Holmes DR Jr, Rihal CS. Radiation dose reduction in the invasive cardiovascular laboratory: implementing a culture and philosophy of radiation safety. JACC Cardiovasc Interv. 2012; 5(8): 866-73.
doi: 10.1016/j.jcin.2012.05.003 |
| 29 |
Kuon E, Weitmann K, Hoffmann W, Dörr M, Reffelmann T, Hummel A, et al. Efficacy of a minicourse in radiation-reducing techniques in invasive cardiology: a multicenter field study. JACC Cardiovasc Interv. 2014; 7(4): 382-90.
doi: 10.1016/j.jcin.2013.11.016 |
| 30 | Lukoff J, Olmos J. Minimizing medical radiation exposure by incorporating a new radiation “vital sign” into the electronic medical record: quality of care and patient safety. Perm J. 2017; 21: 17-007. |
| 31 |
Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy: “how far away is far enough?”. J Orthop Trauma. 1997; 11(6): 392-8.
doi: 10.1097/00005131-199708000-00002 pmid: 9314144 |
| 32 |
Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005; 13(1): 69-76.
doi: 10.5435/00124635-200501000-00009 pmid: 15712984 |
| 33 |
Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, Saia B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond). 2005; 55(6): 498-500.
doi: 10.1093/occmed/kqi048 |
| [1] | Xinlei Wang, Yao Sun, Xiaoyu Ni, Shu Zhang. Development and validation of an emergency bloodstream infection score for predicting in-hospital mortality in patients with community-acquired bloodstream infections [J]. World Journal of Emergency Medicine, 2023, 14(4): 280-286. |
| [2] | Ahmed Faidh Ramzee, Ayman El-Menyar, Mohammad Asim, Ahad Kanbar, Khalid Ahmed, Bahaa Daoud, Saji Mathradikkal, Ahmad Kloub, Hassan Al-Thani, Sandro Rizoli. The impact of emergency department length of stay on the outcomes of trauma patients requiring hospitalization: a retrospective observational study [J]. World Journal of Emergency Medicine, 2023, 14(2): 96-105. |
| [3] | Jee Yen Kuck, Abdul Muhaimin Noor Azhar, Neena Wee, Rishya Manikam. Diagnostic accuracy of the tongue blade test combined with clinical signs to detect maxillary and mandibular fractures in the emergency department [J]. World Journal of Emergency Medicine, 2023, 14(2): 122-127. |
| [4] | Guang-mei Wang, Yong Li, Shuo Wu, Wen Zheng, Jing-jing Ma, Feng Xu, Jia-qi Zheng, He Zhang, Jia-li Wang, Yu-guo Chen. The combination of creatine kinase-myocardial band isoenzyme and point-of-care cardiac troponin/ contemporary cardiac troponin for the early diagnosis of acute myocardial infarction [J]. World Journal of Emergency Medicine, 2022, 13(3): 163-168. |
| [5] | Ittai Shichman, Or Shaked, Shai Factor, Ahuva Weiss-Meilik, Amal Khoury. Emergency department electric scooter injuries after the introduction of shared e-scooter services: A retrospective review of 3,331 cases [J]. World Journal of Emergency Medicine, 2022, 13(1): 5-10. |
| [6] | Ralphe Bou Chebl, Nader El Souki, Mirabelle Geha, Imad Majzoub, Rima Kaddoura, Hady Zgheib. Two-point compression ultrasonography: Enough to rule out lower extremity deep venous thrombosis? [J]. World Journal of Emergency Medicine, 2021, 12(4): 268-273. |
| [7] | Lori Stolz, Elaine Situ-LaCasse, Josie Acuña, Matthew Thompson, Nicolaus Hawbaker, Josephine Valenzuela, Uwe Stolz, Srikar Adhikari. What is the ideal approach for emergent pericardiocentesis using point-of-care ultrasound guidance? [J]. World Journal of Emergency Medicine, 2021, 12(3): 169-173. |
| [8] | Kasım Turgut, Erdal Yavuz, Mine Kayacı Yıldız, Mehmet Kaan Poyraz. Violence toward emergency physicians: A prospective-descriptive study [J]. World Journal of Emergency Medicine, 2021, 12(2): 111-116. |
| [9] | Marin Pavlov, Lucija Klobučar, Iva Klobučar, Kristina Žgela, Vesna Degoricija. Does shifting to professional emergency department staffing affect the decision for chest radiography? [J]. World Journal of Emergency Medicine, 2021, 12(2): 87-92. |
| [10] | Hady Zgheib, Aline El Zakhem, Cynthia Wakil, Mohamad Ali Cheaito, Rola Cheaito, Antoine Finianos, Ralphe Bou Chebl, Rima Kaddoura, Nader Al Souky, Imad El Majzoub. Role of urine studies in asymptomatic febrile neutropenic patients presenting to the emergency department [J]. World Journal of Emergency Medicine, 2021, 12(2): 99-104. |
| [11] | William Gilliam, Jackson F. Barr, Brandon Bruns, Brandon Cave, Jordan Mitchell, Tina Nguyen, Jamie Palmer, Mark Rose, Safura Tanveer, Chris Yum, Quincy K. Tran. Factors associated with refractory pain in emergency patients admitted to emergency general surgery [J]. World Journal of Emergency Medicine, 2021, 12(1): 12-17. |
| [12] | Rebekah Shaw, Erica Popovsky, Alyssa Abo, Marni Jacobs, Nicole Herrera, James Chamberlain, Andrea Hahn. Improving antibiotic prescribing in the emergency department for uncomplicated community-acquired pneumonia [J]. World Journal of Emergency Medicine, 2020, 11(4): 199-205. |
| [13] | Hai-jiang Zhou, Tian-fei Lan, Shu-bin Guo. Outcome prediction value of National Early Warning Score in septic patients with community-acquired pneumonia in emergency department: A single-center retrospective cohort study [J]. World Journal of Emergency Medicine, 2020, 11(4): 206-215. |
| [14] | Chuan-qi Ding, Yu-ping Zhang, Yu-wei Wang, Min-fei Yang, Sa Wang, Nian-qi Cui, Jing-fen Jin. Death and do-not-resuscitate order in the emergency department: A single-center three-year retrospective study in the Chinese mainland [J]. World Journal of Emergency Medicine, 2020, 11(4): 231-237. |
| [15] | Maybritt I. Kuypers, Adinda Klijn, Nieke E. Mullaart-Jansen, Frans B. Plötz. Availability and quality of procedural sedation and analgesia in emergency departments without emergency physicians: A national survey in the Netherlands [J]. World Journal of Emergency Medicine, 2020, 11(2): 69-73. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
