World Journal of Emergency Medicine ›› 2024, Vol. 15 ›› Issue (4): 289-296.doi: 10.5847/wjem.j.1920-8642.2024.059
• Original Articles • Previous Articles Next Articles
Hao Li1, Chang Liu1, Ying Cui1, Panpan Chang2,3,4( ), Wei Chong1(
), Wei Chong1( )
)
Received:2023-07-29
Accepted:2023-12-25
Online:2024-07-15
Published:2024-07-01
Contact:
Wei Chong, Email: wchong@cmu.edu.cn; Panpan Chang, Email: changpanpan@bjmu.edu.cn
Hao Li, Chang Liu, Ying Cui, Panpan Chang, Wei Chong. Effect of tubastatin A on NLRP3 inflammasome activation in macrophages under hypoxia/reoxygenation conditions[J]. World Journal of Emergency Medicine, 2024, 15(4): 289-296.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2024.059

Figure 2.
Effect of TubA on the expression of HDAC6, Hsp90, and iNOS in macrophages under H/R. A: western blotting results of the protein expression of HDAC6, Hsp90, and iNOS in RAW264.7 cells; B: the relative protein expression levels. Compared with the control group, **P<0.01; compared with the H/R group, ##P<0.01, #P<0.05 (n=3). The concentration of TubA was 2.5 μmol/L. H/R: hypoxia/reoxygenation; TubA: tubastatin A.
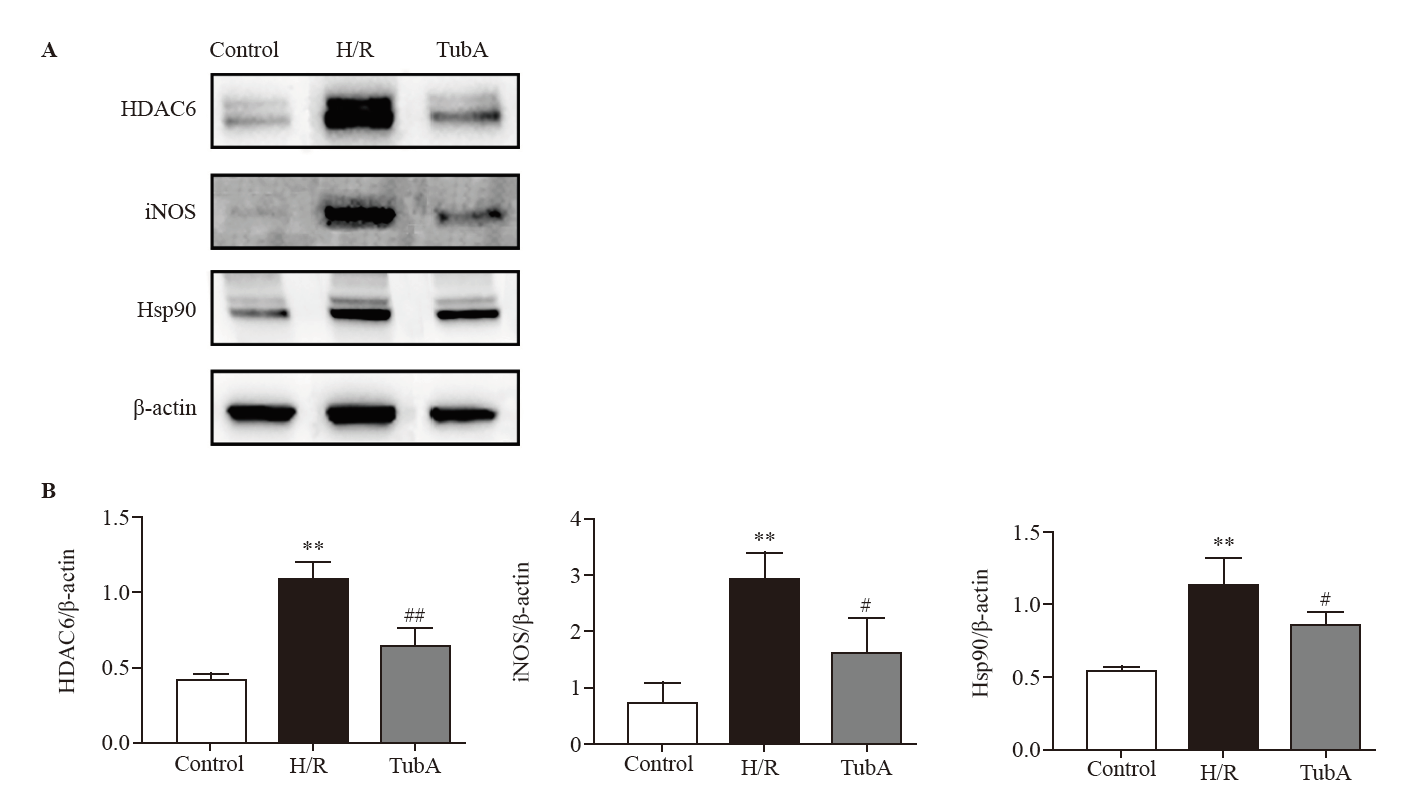

Figure 3.
Effect of TubA on the ROS in macrophages under H/R. A: ROS levels in RAW264.7 cells measured under fluorescence microscopy; B: semi-quantitative analysis of ROS levels in each group. Compared with the control group, **P<0.01; compared with the H/R group, #P<0.05 (n=3). The concentration of TubA was 2.5 μmol/L. H/R: hypoxia/reoxygenation; TubA: tubastatin A.


Figure 4.
Effect of TubA on NLRP3 inflammasome activation in macrophages under H/R. A: western blotting analysis of the protein expressions of NLRP3, GSDMD, caspase-1, GSDMD-N, and caspase-1 p20 in RAW264.7 cells. B: the relative expression levels of the NLRP3, GSDMD, caspase-1, GSDMD-N, and caspase-1 p20 proteins. Compared with the control group, **P<0.01, *P<0.05; compared with the H/R group, #P<0.05 (n=3). The concentration of TubA was 2.5 μmol/L. H/R: hypoxia/reoxygenation; TubA: tubastatin A.
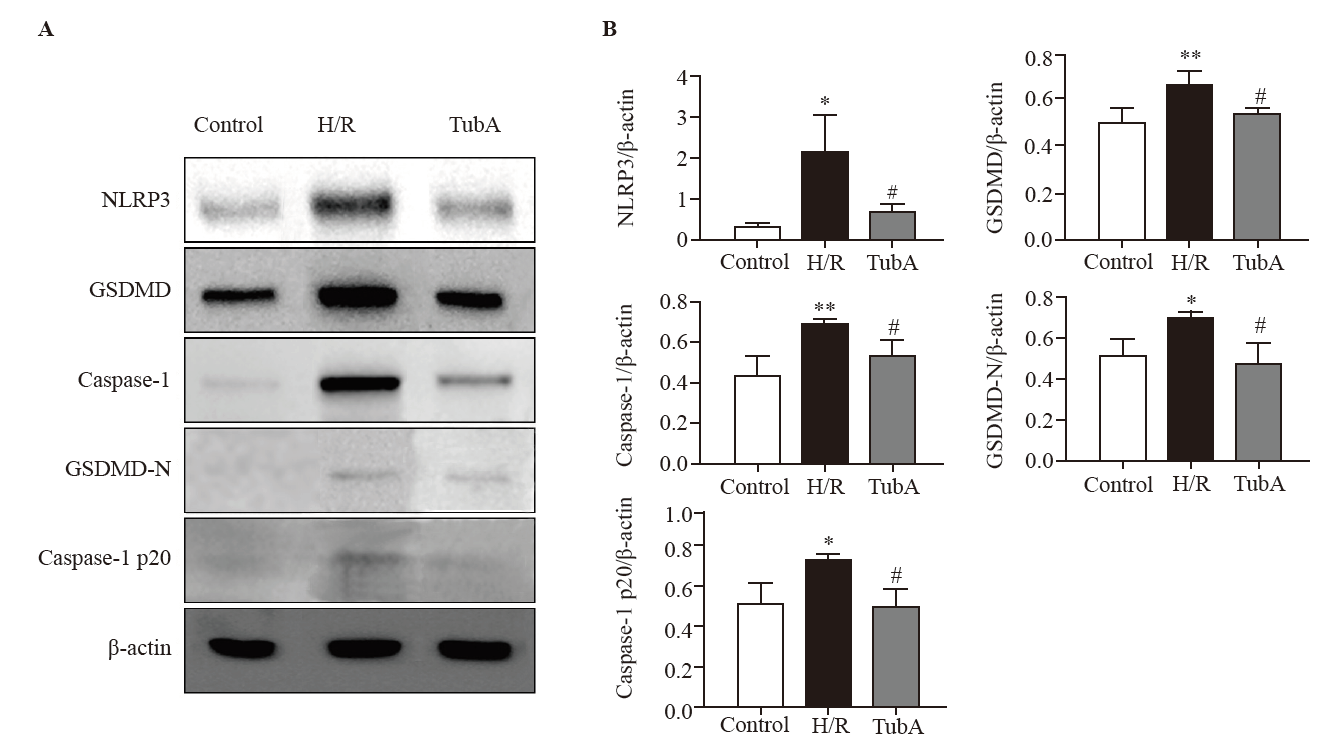

Figure 5.
Effect of TubA on IL-1β and IL-18 secretion in macrophages under H/R. A: IL-1β secretion by RAW264.7 cells; B: IL-18 secretion by RAW264.7 cells. Compared with the control group, **P<0.01; compared with the H/R group, ##P<0.01 (n=3). The concentration of TubA was 2.5 μmol/L. H/R: hypoxia/reoxygenation; TubA: tubastatin A; IL-1β: interleukin-1β.
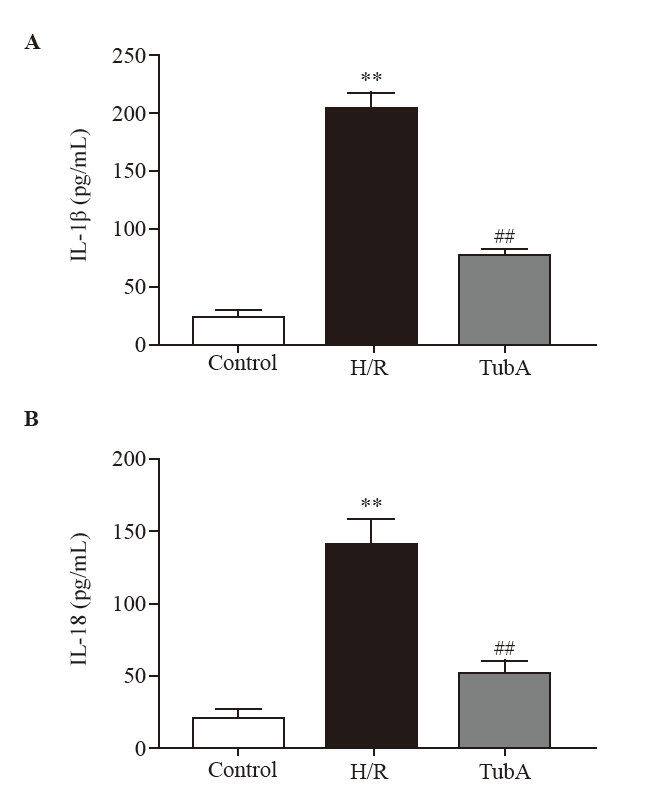

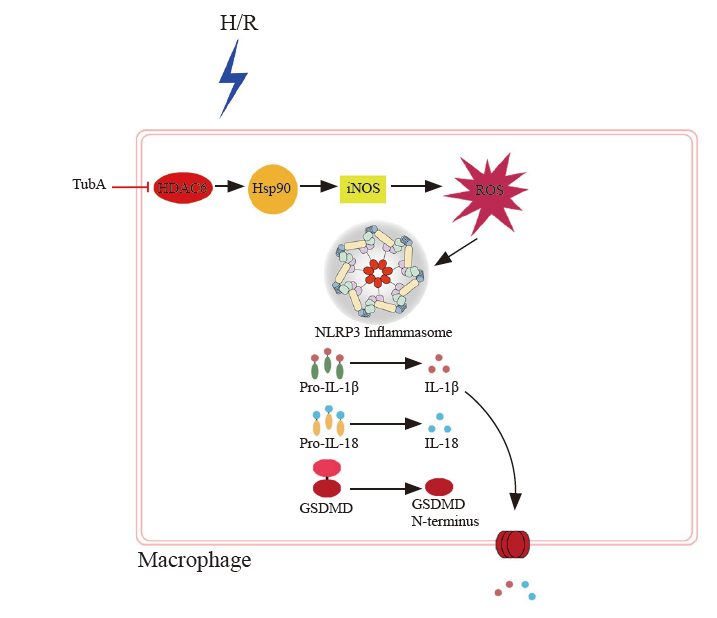
Figure 6.
Potential mechanisms of tubastatin A (TubA) on NLRP3 inflammasome activation in macrophages under hypoxia/reoxygenation (H/R). The expression of HDAC6, Hsp90, and iNOS is increased in macrophages under H/R, resulting in elevated levels of ROS and NLRP3 inflammasome activation. Cleavage of GSDMD leads to the formation of GSDMD-N, which is then inserted into the cell membrane. This leads to an increase in the secretion of IL-1β and IL-18. TubA inhibits the expression of HDAC6, Hsp90, and iNOS in macrophages under H/R, thereby reducing ROS levels and inhibiting NLRP3 inflammasome activation. Additionally, TubA decreases the expression of GSDMD and GSDMD-N, along with the secretion of IL-1β and IL-18.
| [1] | Waltz PK, Kautza B, Luciano J, Dyer M, Stolz DB, Loughran P, et al. Heme oxygenase-2 localizes to mitochondria and regulates hypoxic responses in hepatocytes. Oxid Med Cell Longev. 2018;2018: 2021645. |
| [2] |
Liu Y, Lu TF, Zhang C, Xue ZZ, Xu J, Busuttil RW, et al. Pituitary adenylate cyclase-activating polypeptides prevent hepatocyte damage by promoting yes-associated protein in liver ischemia-reperfusion injury. Transplantation. 2019; 103(8): 1639-48.
doi: 10.1097/TP.0000000000002742 pmid: 31348437 |
| [3] | Pang QY, Zhao Y, Chen X, Zhao KY, Zhai QX, Tu FX. Apigenin protects the brain against ischemia/reperfusion injury via caveolin-1/VEGF in vitro and in vivo. Oxid Med Cell Longev. 2018;2018: 7017204. |
| [4] | Schett G, Neurath MF. Resolution of chronic inflammatory disease: universal and tissue-specific concepts. Nat Commun. 2018; 9(1): 3261. |
| [5] | Guo SM, Dong L, Li JH, Chen YT, Yao Y, Zeng R, et al. C-X3-C motif chemokine ligand 1/receptor 1 regulates the M1 polarization and chemotaxis of macrophages after hypoxia/reoxygenation injury. Chronic Dis Transl Med. 2021; 7(4): 254-65. |
| [6] | Jiang YN, Chen XY, Fan MY, Li H, Zhu WN, Chen X, et al. TRAIL facilitates cytokine expression and macrophage migration during hypoxia/reoxygenation via ER stress-dependent NF-κB pathway. Mol Immunol. 2017;82: 123-36. |
| [7] | Zhong Y, Gu LJ, Ye YZ, Zhu H, Pu B, Wang JC, et al. JAK2/STAT3 axis intermediates microglia/macrophage polarization during cerebral ischemia/reperfusion injury. Neuroscience. 2022;496: 119-28. |
| [8] |
Rathinam VAK, Chan FK. Inflammasome, inflammation, and tissue homeostasis. Trends Mol Med. 2018; 24(3): 304-18.
doi: S1471-4914(18)30004-2 pmid: 29433944 |
| [9] |
Takahashi M. Cell-specific roles of NLRP3 inflammasome in myocardial infarction. J Cardiovasc Pharmacol. 2019; 74(3): 188-93.
doi: 10.1097/FJC.0000000000000709 pmid: 31356542 |
| [10] | Kelley N, Jeltema D, Duan YH, He Y. The NLRP3 inflammasome: an overview of mechanisms of activation and regulation. Int J Mol Sci. 2019; 20(13): 3328. |
| [11] | Bian F, Yang XY, Xu G, Zheng T, Jin S. CRP-induced NLRP3 inflammasome activation increases LDL transcytosis across endothelial cells. Front Pharmacol. 2019;10: 40. |
| [12] | Boucher D, Monteleone M, Coll RC, Chen KW, Ross CM, Teo JL, et al. Caspase-1 self-cleavage is an intrinsic mechanism to terminate inflammasome activity. J Exp Med. 2018; 215(3): 827-40. |
| [13] | Wang L, Hauenstein AV. The NLRP3 inflammasome: mechanism of action, role in disease and therapies. Mol Aspects Med. 2020;76: 100889. |
| [14] | Song JQ, Jiang LY, Fu CP, Wu X, Liu ZL, Xie L, et al. Heterozygous SOD2 deletion deteriorated chronic intermittent hypoxia-induced lung inflammation and vascular remodeling through mtROS-NLRP3 signaling pathway. Acta Pharmacol Sin. 2020; 41(9): 1197-207. |
| [15] | Pu JL, Huang ZT, Luo YH, Mou T, Li TT, Li ZT, et al. Fisetin mitigates hepatic ischemia-reperfusion injury by regulating GSK3β/AMPK/NLRP 3 inflammasome pathway. Hepatobiliary Pancreat Dis Int. 2021; 20(4): 352-60. |
| [16] | Shi B, Lyu CJ, Le ZK, Ji HS, Xiao Y, Zhang YY, et al. NLRP3 activation in macrophages promotes acute intestinal injury in neonatal necrotizing enterocolitis. World J Pediatr. 2024; 20(2):153-64. |
| [17] | Sheu JR, Hsieh CY, Jayakumar T, Lin GY, Lee HN, Huang SW, et al. HDAC6 dysfunction contributes to impaired maturation of adult neurogenesis in vivo: vital role on functional recovery after ischemic stroke. J Biomed Sci. 2019; 26(1): 27. |
| [18] |
Moreno-Gonzalo O, Mayor F Jr, Sánchez-Madrid F. HDAC6 at crossroads of infection and innate immunity. Trends Immunol. 2018; 39(8): 591-5.
doi: S1471-4906(18)30107-8 pmid: 29937401 |
| [19] | Chang PP, Li H, Hu H, Li YQ, Wang TB. The role of HDAC6 in autophagy and NLRP3 inflammasome. Front Immunol. 2021;12: 763831. |
| [20] |
Williams AM, Dennahy IS, Bhatti UF, Biesterveld BE, Graham NJ, Li YQ, et al. Histone deacetylase inhibitors: a novel strategy in trauma and sepsis. Shock. 2019; 52(3): 300-6.
doi: 10.1097/SHK.0000000000001308 pmid: 30601405 |
| [21] |
Chang ZG, Li YQ, He W, Liu BL, Halaweish I, Bambakidis T, et al. Selective inhibition of histone deacetylase 6 promotes survival in a rat model of hemorrhagic shock. J Trauma Acute Care Surg. 2015; 79(6): 905-10.
doi: 10.1097/TA.0000000000000784 pmid: 26680133 |
| 22 | Magupalli VG, Negro R, Tian YZ, Hauenstein AV, di Caprio G, Skillern W, et al. HDAC6 mediates an aggresome-like mechanism for NLRP3 and pyrin inflammasome activation. Science. 2020;369(6510): eaas8995. |
| [23] | Li T, Zhang C, Hassan S, Liu XY, Song FJ, Chen KX, et al. Histone deacetylase 6 in cancer. J Hematol Oncol. 2018; 11(1): 111. |
| [24] | Birbo B, Madu EE, Madu CO, Jain A, Lu Y. Role of HSP90 in cancer. Int J Mol Sci. 2021; 22(19): 10317. |
| [25] |
Seidel C, Schnekenburger M, Dicato M, Diederich M. Histone deacetylase 6 in health and disease. Epigenomics. 2015; 7(1): 103-18.
doi: 10.2217/epi.14.69 pmid: 25687470 |
| [26] | Yang XC, Cao XQ, Sheng LL, Yang ZW. Mechanism of histone deacetylase inhibitor tubastatin A promoting autophagy of Legionella pneumophila infected RAW264.7 cells. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2021; 37(8): 693-701. [Article in Chinese] |
| [27] |
Yan MP, Hou MK, Liu J, Zhang SL, Liu B, Wu XX, et al. Regulation of iNOS-derived ROS generation by HSP90 and cav-1 in porcine reproductive and respiratory syndrome virus-infected swine lung injury. Inflammation. 2017; 40(4): 1236-44.
doi: 10.1007/s10753-017-0566-9 pmid: 28493081 |
| [28] | Cheng K, Huang YQ, Wang CF. 1, 25(OH)2D3 inhibited ferroptosis in zebrafish liver cells (ZFL) by regulating Keap1-Nrf2-GPx4 and NF-κB-hepcidin axis. Int J Mol Sci. 2021; 22(21): 11334. |
| [29] |
Makley AT, Belizaire R, Campion EM, Goodman MD, Sonnier DI, Friend LA, et al. Simulated aeromedical evacuation does not affect systemic inflammation or organ injury in a murine model of hemorrhagic shock. Mil Med. 2012; 177(8): 911-6.
doi: 10.7205/milmed-d-11-00385 pmid: 22934369 |
| [30] | Li ZT, Liu H, Zhang WQ. NLRC3 alleviates hypoxia/reoxygenation induced inflammation in RAW264.7 cells by inhibiting K63-linked ubiquitination of TRAF6. Hepatobiliary Pancreat Dis Int. 2020; 19(5): 455-60. |
| [31] | Celen S, Rokka J, Gilbert TM, Koole M, Vermeulen I, Serdons K, et al. Translation of HDAC6 PET imaging using[18F]EKZ-001-cGMP production and measurement of HDAC6 target occupancy in nonhuman primates. ACS Chem Neurosci. 2020; 11(7): 1093-101. |
| [32] | Fan T, Huang ZX, Chen L, Wang W, Zhang BY, Xu Y, et al. Associations between autophagy, the ubiquitin-proteasome system and endoplasmic reticulum stress in hypoxia-deoxygenation or ischemia-reperfusion. Eur J Pharmacol. 2016;791: 157-67. |
| [33] | Henot F, Rioual E, Favier A, Macek P, Crublet E, Josso P, et al. Visualizing the transiently populated closed-state of human HSP 90 ATP binding domain. Nat Commun. 2022; 13(1): 7601. |
| [34] | Miyata Y. Hsp 90 inhibitor geldanamycin and its derivatives as novel cancer chemotherapeutic agents. Curr Pharm Des. 2005; 11(9): 1131-8. |
| [35] |
Yoshida M, Xia Y. Heat shock protein 90 as an endogenous protein enhancer of inducible nitric-oxide synthase. J Biol Chem. 2003; 278(38): 36953-8.
doi: 10.1074/jbc.M305214200 pmid: 12855682 |
| [36] | Zhao K, Huang Z, Lu HL, Zhou JF, Wei TT. Induction of inducible nitric oxide synthase increases the production of reactive oxygen species in RAW264.7 macrophages. Biosci Rep. 2010; 30(4): 233-41. |
| [37] | Dai JW, Chen QS, Huang WF, Shi K, Zhang YK, Li TT, et al. Liver kinase B1 attenuates liver ischemia/reperfusion injury via inhibiting the NLRP3 inflammasome. Acta Biochim Biophys Sin. 2021; 53(5): 601-11. |
| [38] |
Bruhn PJ, Nikolian VC, Halaweish I, Chang ZG, Sillesen M, Liu BL, et al. Tubastatin A prevents hemorrhage-induced endothelial barrier dysfunction. J Trauma Acute Care Surg. 2018; 84(2): 386-92.
doi: 10.1097/TA.0000000000001753 pmid: 29194316 |
| [39] |
Chang ZG, Li YQ, He W, Liu BL, Duan XZ, Halaweish I, et al. Inhibition of histone deacetylase 6 restores intestinal tight junction in hemorrhagic shock. J Trauma Acute Care Surg. 2016; 81(3): 512-9.
doi: 10.1097/TA.0000000000001137 pmid: 27257709 |
| [40] | Auzmendi-Iriarte J, Saenz-Antoñanzas A, Mikelez-Alonso I, Carrasco-Garcia E, Tellaetxe-Abete M, Lawrie CH, et al. Characterization of a new small-molecule inhibitor of HDAC 6 in glioblastoma. Cell Death Dis. 2020; 11(6): 417. |
| [41] |
Liang T, Fang H. Structure, functions and selective inhibitors of HDAC6. Curr Top Med Chem. 2018; 18(28): 2429-47.
doi: 10.2174/1568026619666181129141822 pmid: 30499393 |
| [42] | Mobley RJ, Raghu D, Duke LD, Abell-Hart K, Zawistowski JS, Lutz K, et al. MAP3K 4 controls the chromatin modifier HDAC6 during trophoblast stem cell epithelial-to-mesenchymal transition. Cell Rep. 2017; 18(10): 2387-400. |
| [43] | Liu P, Xiao J, Wang YL, Song XW, Huang LZ, Ren Z, et al. Posttranslational modification and beyond: interplay between histone deacetylase 6 and heat-shock protein 90. Mol Med. 2021; 27(1): 110. |
| [44] | Bai Y, Bai J, Lu P, Jing YM, Zheng WC, Wang LY, et al. Hirudin ameliorates myocardial ischemia-reperfusion injury in a rat model of hemorrhagic shock and resuscitation: roles of NLRP3-signaling pathway. Mol Cell Biochem. 2024; 479(1): 63-72. |
| [45] | Fu L, Zhang DX, Zhang LM, Song YC, Liu FH, Li Y, et al. Exogenous carbon monoxide protects against mitochondrial DNA-induced hippocampal pyroptosis in a model of hemorrhagic shock and resuscitation. Int J Mol Med. 2020; 45(4): 1176-86. |
| [1] | Rui Zhang, Meng-yang Xue, Bao-shan Liu, Wen-jun Wang, Xin-hui Fan, Bo-yuan Zheng, Qiu-huan Yuan, Feng Xu, Jia-li Wang, Yu-guo Chen. Aldehyde dehydrogenase 2 preserves mitochondrial morphology and attenuates hypoxia/reoxygenation-induced cardiomyocyte injury [J]. World Journal of Emergency Medicine, 2020, 11(4): 246-254. |
| [2] | Ruo Wu, Luo-gen Peng, Hui-min Zhao. Diverse coagulopathies in a rabbit model with different abdominal injuries [J]. World Journal of Emergency Medicine, 2017, 8(2): 141-147. |
| [3] | Bao-di Sun, Hong-mei Liu, Shi-nan Nie. S100B protein in serum is elevated after global cerebral ischemic injury [J]. World Journal of Emergency Medicine, 2013, 4(3): 165-168. |
| [4] | Cheng Zhang, Guang-rong Gao, Hui-yong Jiang, Chen-guang Lv, Bao-lei Zhang, Ming-shuang Xie, Zhi-li Zhang, Li Yu, Xue-feng Zhang. Effects of environmental hypothermia on hemodynamics and oxygen dynamics in a conscious swine model of hemorrhagic shock [J]. World Journal of Emergency Medicine, 2012, 3(2): 128-134. |
| [5] | Zhi-hong Liu, Xin-ri Zhang, Xiao-yun Hu, Meng-yu Cheng, Jian-ying Xu, Yong-cheng Du. Effect of glucocorticoid on MIP-1α and NF-кb expressing in the lung of rats undergoing mechanical ventilation with a high tidal volume [J]. World Journal of Emergency Medicine, 2011, 2(1): 66-69. |
| [6] | Fan Yang, Xiang-jun Bai, Duan Hu, Zhan-fei Li, Kai-jun Liu. Effect of triptolide on secretion of inflammatory cellular factors TNF-α and IL-8 in peritoneal macrophages of mice activated by lipopolysaccharide [J]. World Journal of Emergency Medicine, 2010, 1(1): 70-74. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
