Elevated serum lactate levels, which have been observed even during hemodynamic stability, have been considered an important marker of impaired tissue perfusion among sepsis patients. Some studies have established lactate levels as diagnostic, therapeutic, and prognostic indicators of tissue perfusion in sepsis.[4,5] Previous studies have also shown that elevated blood lactate levels were associated with an increased risk of death. [4,5]
Increased blood lactate levels have been used to identify critically ill patients at high risk of death even before the development of hemodynamic instability.[6⇓⇓-9] Scott et al[7] observed a 3-fold increase in 30-d mortality in children with a venous lactate level >36 mg/dL. Early venous lactate levels assist in the assessment of sepsis severity. Venous lactate levels are able to predict outcomes among patients with sepsis. Venous lactate levels are more manageable and less painful to determine compared to arterial samples.[10] The peripheral venous lactate levels may serve as an alternative to arterial blood lactate measurements to predict in-hospital mortality.[8,9]
Blood lactate levels can be measured by various devices (central laboratory, point-of-care blood gas analyzer). Most devices used at the bedside have acceptable limits of agreement compared to central laboratory devices.[10]
This study aimed to compare the predictability of venous lactate to other measures, such as arterial lactate, Sequential Organ Failure Assessment (SOFA), quick SOFA (qSOFA), and systemic inflammatory response syndrome (SIRS) criteria, to predict 28-d hospital mortality and morbidity in patients with sepsis admitted to the ED.
METHODS
Study design and setting
This study was a retrospective cohort. A prognostic prediction research study was conducted in the ED, Faculty of Medicine Ramathibodi Hospital, a university-affiliated super tertiary care hospital in Bangkok, Thailand. The Ethics Committee of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, approved this study in terms of Human Rights Related to Research Involving Human Subjects (Ethics code: MURA2017/247, date of IRB approval 22 May 2017).
Inclusion and exclusion criteria
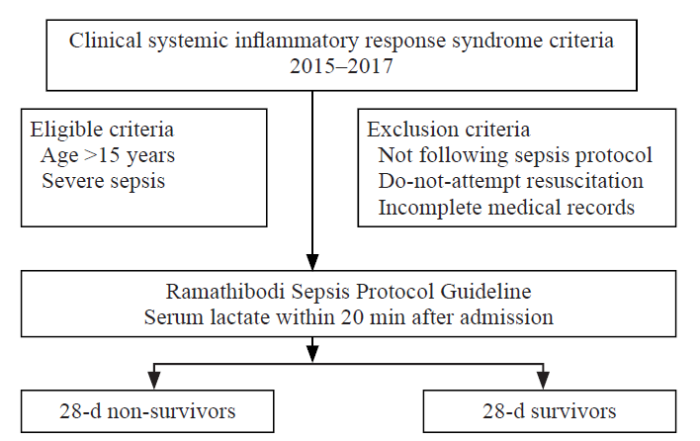
Patients who visited the ED with clinical SIRS determined from the electronic medical record from August 2015 to March 2017 were recruited (Figure 1).
Figure 1.
Figure 1.
Patient inclusion flow diagram.
The eligible criteria were patients older than 15 years who visited the ED for severe sepsis. According to the Surviving Sepsis Campaign 2012 guideline,[2] severe sepsis was defined as sepsis-induced tissue hypoperfusion or organ dysfunction (any of the following thought to be due to the infection): (1) sepsis-induced hypotension; (2) blood lactate level above the upper limits of the normal laboratory; (3) urine output <0.5 mL/(kg·h) for more than 2 h despite adequate fluid resuscitation; (4) acute lung injury with PaO2/FiO2 <250 mmHg (1 mmHg=0.133 kPa) in the absence of pneumonia as the infection source; (5) acute lung injury with PaO2/FiO2 <200 mmHg in the presence of pneumonia as the infection source; (6) creatinine >2.0 mg/dL; (7) total bilirubin >2 mg/dL; (8) platelet count <100,000/cumm; and (9) coagulopathy (international normalized ratio >1.5).
The exclusion criteria were as follows: (1) not following the sepsis protocol; (2) do-not-attempt resuscitation; or (3) incomplete medical records.
Data collection
The researchers reviewed the medical records in the database software of RAMATHIBODI electronic medical record (EMR). Because this was a retrospective observational cohort study, the researchers did not influence clinical decision-making. The clinicians were blinded to the data collection process.
The potential confounding factors, such as age, sex, comorbidities, information at the ED triage area, initial venous lactate level, and arterial lactate level, were recorded. The qSOFA score and SIRS criteria were calculated from the patient data. Treatments, such as a mechanical ventilator, vasopressors, and time to antibiotic administration, were reviewed from the hospital database.
In the ED, lactate levels were used to screen suspected sepsis patients. Every suspected sepsis patient had serum lactate checked within 20 min of the initial ED physician evaluation. The patients with initial venous lactate levels >4 mmol/L were re-evaluated for arterial lactate levels and analyzed by point-of-care BloodGas GEM 3000 (codei1 sr02971).
Primary and secondary outcomes
The primary outcome of this study was to determine the initial venous lactate level as a predictor of 28-d hospital mortality. The secondary outcomes were defined as a predictor of the vasopressor and mechanical ventilator used within 24 h among patients with sepsis in the ED.
Statistical analyses
Categorical variables are expressed as absolute values and percentages and continuous variables as medians and interquartile ranges (IQRs). Categorical variables were compared using the Chi-square test or Fisher’s exact test when appropriate, while continuous variables were compared using the Mann-Whitney U-test.
We used the area under the receiver operating characteristic (AUROC) curve and odds ratio (OR) from logistic regression to assess the initial venous lactate’s ability to determine the primary and secondary outcomes. The model calibration was also evaluated using the Hosmer-Lemeshow test with a P-value <0.05 suggesting imperfective calibration and the observed-to-expected (O/E) ratio with a ratio of 1 indicating perfect calibration. Correlations between venous and arterial lactate levels were also presented using the equation. We used Stata version 14.0 (StataCorp LP., USA) for statistical analyses.
RESULTS
Demographic and descriptive data
The demographic and descriptive data of the 460 included patients are listed in Table 1. Non-survivors had higher initial venous lactate levels (median, 5.9 mmol/L vs. 4.0 mmol/L; P=0.001).
Table 1. Demographic and descriptive data of the included patients
| Demographic data | All (n=460) | Non-survivors (n=130) | Survivors (n=330) | P-value |
|---|---|---|---|---|
| Age, years | 70 (59-81) | 69 (59-82) | 72 (59-80) | 0.970 |
| Male | 233 (50.7) | 68 (52.3) | 165 (50.0) | 0.660 |
| Comorbidities | ||||
| Systemic hypertension | 223 (48.5) | 53 (40.7) | 170 (51.5) | 0.030 |
| Diabetes mellitus | 136 (29.6) | 34 (26.2) | 102 (30.9) | 0.310 |
| Congestive heart failure | 25 (5.4) | 9 (6.9) | 16 (4.8) | 0.380 |
| End-stage renal disease | 13 (2.8) | 5 (3.8) | 8 (2.4) | 0.410 |
| Oncologic | 118 (25.6) | 46 (35.4) | 72 (21.8) | 0.003 |
| Transplant | 12 (2.6) | 3 (2.3) | 9 (2.7) | 0.802 |
| Liver cirrhosis | 29 (6.3) | 12 (9.2) | 17 (5.2) | 0.110 |
| Ischemic heart disease | 48 (10.4) | 14 (10.8) | 34 (10.3) | 0.880 |
| Neuromuscular disease | 131 (28.5) | 30 (23.1) | 101 (30.6) | 0.110 |
| Source of infection | ||||
| Respiratory system | 247 (53.7) | 86 (66.2) | 161 (48.8) | 0.001 |
| Gastrointestinal system | 92 (20.0) | 19 (14.6) | 73 (22.1) | 0.070 |
| Urinary system | 63 (13.7) | 10 (7.7) | 53 (16.1) | 0.020 |
| Skin infection | 18 (3.9) | 4 (3.1) | 14 (4.2) | 0.560 |
| Blood stream | 17 (3.7) | 5 (3.8) | 12 (3.6) | 0.910 |
| Systolic blood pressure, mmHg | 115 (90-139) | 107 (83-135) | 120 (95-142) | 0.004 |
| Mean arterial pressure, mmHg | 81 (66-97) | 76 (62-92) | 82 (68-99) | 0.010 |
| Diagnosis at ED | ||||
| Septic shock | 141 (30.6) | 57 (43.8) | 84 (25.5) | 0.001 |
| Time to antibiotic administration, min | 50 (35-65) | 45 (35-60) | 50 (35-68) | 0.270 |
| Positive hemoculture | 108 (23.5) | 33 (25.4) | 75 (22.7) | 0.560 |
| Initial venous lactate, mmol/L | 4.2 (2.9-6.4) | 5.9 (3.1-9.4) | 4.0 (2.7-5.5) | 0.001 |
| Initial arterial lactate, mmol/L | 4.0 (2.3-6.0) | 5.4 (3.0-8.8) | 3.5 (2.0-5.2) | 0.001 |
| SIRS criteria | 3 (2-3) | 3 (3-4) | 2 (2-3) | 0.001 |
| qSOFA score | 1 (1-2) | 2 (1-3) | 1 (1-2) | 0.001 |
| SOFA score | 6 (4-10) | 10 (8-12) | 5 (3-7) | 0.001 |
| Vasopressor use on day one | 201 (43.7) | 96 (73.8) | 105 (31.8) | 0.001 |
| Mechanical ventilation on day one | 275 (59.8) | 123 (94.6) | 152 (46.1) | 0.001 |
Data are expressed as n (%) and medians and interquartile ranges; SIRS: systemic inflammatory response syndrome; qSOFA: quick sequential organ failure assessment.
Univariate and multivariate analyses
Univariate analysis revealed odds ratios of 1.19 (95% confidence interval [CI] 1.12-1.27) for initial venous lactate level, 2.31 (95% CI 1.74-3.06) for qSOFA score, 0.65 (95% CI 0.42-0.97) for hypertension, 1.12 (95% CI 0.85-1.22) for active malignancy, and 1.57 (95% CI 1.22-1.7) for respiratory tract infection (supplementary Table 1).
Multivariate analysis identified initial venous lactate (adjusted OR 1.17, 95% CI 1.09-1.24) and qSOFA score (adjusted OR 2.12, 95% CI 1.58-2.83) as independent factors for 28-d hospital mortality (supplementary Table 1).
Performance of initial venous or arterial lactate
The performance of initial venous lactate and initial arterial lactate for predicting outcomes is presented in Table 2.
Table 2. Performance of initial venous lactate and initial arterial lactate for predicting outcomes
| Outcomes | Calibration | Discrimination | |||
|---|---|---|---|---|---|
| HL chi2 | P-value | O/E ratio (95% CI) | AUROC curve (95% CI) | P-value | |
| 7-d hospital mortality | 3.38 | 0.493 | 0.96 (0.73-1.19) | 0.67 (0.60-0.74) | 0.001 |
| Initial venous lactate (n=460) | |||||
| Initial arterial lactate (n=433) | 2.42 | 0.654 | 0.97 (0.74-1.20) | 0.69 (0.62-0.76) | 0.001 |
| 28-d hospital mortality | 5.69 | 0.227 | 1.00 (0.84-1.16) | 0.65 (0.60-0.71) | 0.001 |
| Initial venous lactate (n=460) | |||||
| Initial arterial lactate (n=433) | 2.89 | 0.583 | 1.00 (0.84-1.17) | 0.66 (0.60-0.72) | 0.001 |
| Vasopressor use on day one | 5.46 | 0.492 | 1.00 (0.89-1.11) | 0.62 (0.57-0.68) | 0.001 |
| Initial venous lactate (n=460) | |||||
| Initial arterial lactate (n=433) | 6.46 | 0.376 | 1.00 (0.89-1.12) | 0.60 (0.55-0.66) | 0.001 |
| Ventilator use on day one | 11.32 | 0.021 | 1.00 (0.92-1.08) | 0.54 (0.48-0.60) | 0.150 |
| Initial venous lactate (n=460) | |||||
| Initial arterial lactate (n=433) | 8.00 | 0.165 | 1.00 (0.92-1.07) | 0.58 (0.53-0.64) | 0.010 |
HL: Hosmer-Lemeshow; O/E ratio: observed-to-expected ratio; CI: confidence interval; AUROC curve: area under the receiver operating characteristic curve.
The initial venous lactate level had a modest ability to predict vasopressor administration within 24 h of ED arrival; however, it had a poor ability to predict mechanical ventilator use within 24 h after ED arrival (Table 2).
The Hosmer-Lemeshow test for initial venous lactate and arterial lactate levels was not significant. The O/E ratio was near 1, indicating good calibration and the ability to predict 7-d and 28-d hospital mortality and vasopressor administration within 24 h.
The ability of the initial venous lactate level to discriminate between survivors and non-survivors after 28 d was not inferior to that of the qSOFA score and SIRS criteria (supplementary Figure 1). There was no significant difference in the ability to predict mortality between the initial venous lactate level and the qSOFA score (P=0.89) or SIRS criteria (P=0.4).
DISCUSSION
In a recent study conducted in Thailand, Musikatavorn et al[9] reported that a single measurement of initial venous lactate was not associated with 30-d mortality. However, the study included non-elderly patients with sepsis who had hemodynamic stability. In another study in Thailand, Permpikul et al[11] reported that patients with severe sepsis and septic shock who had an initial lactate level >2 mmol/L suffered higher mortality (43.6%). The study did not indicate whether the initial lactate measurements were arterial or venous. Our study showed that the initial venous lactate level could predict 7-d and 28-d hospital mortality among patients with severe sepsis with or without shock. Moreover, no significant difference was observed between the initial venous lactate level and arterial lactate level in their ability to predict 7-d and 28-d hospital mortality and vasopressor administration within 24 h. However, our results showed that the initial venous lactate level was not associated with mechanical ventilator use within 24 h. Our study found that only respiratory tract infections, such as pneumonia, bronchitis, and tracheobronchitis, were independent factors associated with mechanical ventilator use during the first day (adjusted OR 4.76, 95% CI 2.97-7.63, adjusted by qSOFA, initial venous lactate, COPD, time to antibiotic and systolic blood pressure).
Many prognostic scores have been developed and used to predict the risk of death and early resuscitation for patients with sepsis to reduce mortality rates. The qSOFA score and SIRS criteria have been easy to use in the ED. Previous studies have shown that the qSOFA score has an excellent ability to predict mortality among patients with sepsis both inside and outside the intensive care unit.[12⇓-14] Another study, however, showed that the qSOFA score failed to detect severe sepsis and had a more inferior ability to predict mortality compared to SIRS criteria.[15]
The present study showed that initial venous lactate’s ability to discriminate between survivors and non-survivors within 28 d was not inferior to that of the qSOFA score and SIRS criteria. Multivariate analysis showed that the initial venous lactate level and qSOFA score were independent predictors of 28-d mortality.
This study has some limitations. This study was a retrospective study conducted in a single center. ED overcrowding and the availability of hospital admission to definite treatment may have affected patient outcomes. The information bias of the reviewer may be our limitation.
CONCLUSIONS
Initial venous lactate levels may have a modest ability to predict 7-d and 28-d hospital mortality and vasopressor administration within 24 h during severe sepsis. Moreover, no significant differences in the ability to predict 7-d and 28-d hospital mortality were observed between the initial venous lactate level and the qSOFA score or SIRS criteria.
Funding: None.
Ethical approval: The Ethics Committee of Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, approved this study in terms of Human Rights Related to Research Involving Human Subjects (Ethics code: MURA2017/247, date of IRB approval 22 May 2017).
Conflicts of interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors: TP wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Effect of neutrophil CD64 for diagnosing sepsis in emergency department
DOI:10.5847/wjem.j.1920-8642.2020.02.003 URL [Cited within: 1]
Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012
DOI:10.1007/s00134-012-2769-8
PMID:23361625
[Cited within: 3]

To provide an update to the "Surviving Sepsis Campaign Guidelines for Management of Severe Sepsis and Septic Shock," last published in 2008.A consensus committee of 68 international experts representing 30 international organizations was convened. Nominal groups were assembled at key international meetings (for those committee members attending the conference). A formal conflict of interest policy was developed at the onset of the process and enforced throughout. The entire guidelines process was conducted independent of any industry funding. A stand-alone meeting was held for all subgroup heads, co- and vice-chairs, and selected individuals. Teleconferences and electronic-based discussion among subgroups and among the entire committee served as an integral part of the development.The authors were advised to follow the principles of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system to guide assessment of quality of evidence from high (A) to very low (D) and to determine the strength of recommendations as strong (1) or weak (2). The potential drawbacks of making strong recommendations in the presence of low-quality evidence were emphasized. Recommendations were classified into three groups: (1) those directly targeting severe sepsis; (2) those targeting general care of the critically ill patient and considered high priority in severe sepsis; and (3) pediatric considerations.Key recommendations and suggestions, listed by category, include: early quantitative resuscitation of the septic patient during the first 6 h after recognition (1C); blood cultures before antibiotic therapy (1C); imaging studies performed promptly to confirm a potential source of infection (UG); administration of broad-spectrum antimicrobials therapy within 1 h of the recognition of septic shock (1B) and severe sepsis without septic shock (1C) as the goal of therapy; reassessment of antimicrobial therapy daily for de-escalation, when appropriate (1B); infection source control with attention to the balance of risks and benefits of the chosen method within 12 h of diagnosis (1C); initial fluid resuscitation with crystalloid (1B) and consideration of the addition of albumin in patients who continue to require substantial amounts of crystalloid to maintain adequate mean arterial pressure (2C) and the avoidance of hetastarch formulations (1B); initial fluid challenge in patients with sepsis-induced tissue hypoperfusion and suspicion of hypovolemia to achieve a minimum of 30 mL/kg of crystalloids (more rapid administration and greater amounts of fluid may be needed in some patients (1C); fluid challenge technique continued as long as hemodynamic improvement is based on either dynamic or static variables (UG); norepinephrine as the first-choice vasopressor to maintain mean arterial pressure ≥65 mmHg (1B); epinephrine when an additional agent is needed to maintain adequate blood pressure (2B); vasopressin (0.03 U/min) can be added to norepinephrine to either raise mean arterial pressure to target or to decrease norepinephrine dose but should not be used as the initial vasopressor (UG); dopamine is not recommended except in highly selected circumstances (2C); dobutamine infusion administered or added to vasopressor in the presence of (a) myocardial dysfunction as suggested by elevated cardiac filling pressures and low cardiac output, or (b) ongoing signs of hypoperfusion despite achieving adequate intravascular volume and adequate mean arterial pressure (1C); avoiding use of intravenous hydrocortisone in adult septic shock patients if adequate fluid resuscitation and vasopressor therapy are able to restore hemodynamic stability (2C); hemoglobin target of 7-9 g/dL in the absence of tissue hypoperfusion, ischemic coronary artery disease, or acute hemorrhage (1B); low tidal volume (1A) and limitation of inspiratory plateau pressure (1B) for acute respiratory distress syndrome (ARDS); application of at least a minimal amount of positive end-expiratory pressure (PEEP) in ARDS (1B); higher rather than lower level of PEEP for patients with sepsis-induced moderate or severe ARDS (2C); recruitment maneuvers in sepsis patients with severe refractory hypoxemia due to ARDS (2C); prone positioning in sepsis-induced ARDS patients with a PaO (2)/FiO (2) ratio of ≤100 mm Hg in facilities that have experience with such practices (2C); head-of-bed elevation in mechanically ventilated patients unless contraindicated (1B); a conservative fluid strategy for patients with established ARDS who do not have evidence of tissue hypoperfusion (1C); protocols for weaning and sedation (1A); minimizing use of either intermittent bolus sedation or continuous infusion sedation targeting specific titration endpoints (1B); avoidance of neuromuscular blockers if possible in the septic patient without ARDS (1C); a short course of neuromuscular blocker (no longer than 48 h) for patients with early ARDS and a PaO (2)/FI O (2) <150 mm Hg (2C); a protocolized approach to blood glucose management commencing insulin dosing when two consecutive blood glucose levels are >180 mg/dL, targeting an upper blood glucose ≤180 mg/dL (1A); equivalency of continuous veno-venous hemofiltration or intermittent hemodialysis (2B); prophylaxis for deep vein thrombosis (1B); use of stress ulcer prophylaxis to prevent upper gastrointestinal bleeding in patients with bleeding risk factors (1B); oral or enteral (if necessary) feedings, as tolerated, rather than either complete fasting or provision of only intravenous glucose within the first 48 h after a diagnosis of severe sepsis/septic shock (2C); and addressing goals of care, including treatment plans and end-of-life planning (as appropriate) (1B), as early as feasible, but within 72 h of intensive care unit admission (2C). Recommendations specific to pediatric severe sepsis include: therapy with face mask oxygen, high flow nasal cannula oxygen, or nasopharyngeal continuous PEEP in the presence of respiratory distress and hypoxemia (2C), use of physical examination therapeutic endpoints such as capillary refill (2C); for septic shock associated with hypovolemia, the use of crystalloids or albumin to deliver a bolus of 20 mL/kg of crystalloids (or albumin equivalent) over 5-10 min (2C); more common use of inotropes and vasodilators for low cardiac output septic shock associated with elevated systemic vascular resistance (2C); and use of hydrocortisone only in children with suspected or proven "absolute"' adrenal insufficiency (2C).Strong agreement existed among a large cohort of international experts regarding many level 1 recommendations for the best care of patients with severe sepsis. Although a significant number of aspects of care have relatively weak support, evidence-based recommendations regarding the acute management of sepsis and septic shock are the foundation of improved outcomes for this important group of critically ill patients.
The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
DOI:10.1001/jama.2016.0287 URL [Cited within: 1]
Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock
DOI:10.1097/CCM.0b013e31819fcf68
PMID:19325467
[Cited within: 2]

Serum lactate is a potentially useful biomarker to risk-stratify patients with severe sepsis; however, it is plausible that elevated serum lactate is simply a manifestation of clinically apparent organ dysfunction and/or shock (i.e., refractory hypotension).To test whether the association between initial serum lactate level and mortality in patients presenting to the emergency department (ED) with severe sepsis is independent of organ dysfunction and shock.Single-center cohort study. The primary outcome was 28-day mortality and the risk factor variable was initial venous lactate (mmol/L), categorized as low (< 2), intermediate (2-3.9), or high (> or = 4). Potential covariates included age, sex, race, acute and chronic organ dysfunction, severity of illness, and initiation of early goal-directed therapy. Multivariable logistic regression analyses were stratified on the presence or absence of shock.The ED of an academic tertiary care center from 2005 to 2007.Eight hundred thirty adults admitted with severe sepsis in the ED.None.Mortality at 28 days was 22.9% and median serum lactate was 2.9 mmol/L. Intermediate (odds ratio [OR] = 2.05, p = 0.024) and high serum lactate levels (OR = 4.87, p < 0.001) were associated with mortality in the nonshock subgroup. In the shock subgroup, intermediate (OR = 3.27, p = 0.022) and high serum lactate levels (OR = 4.87, p = 0.001) were also associated with mortality. After adjusting for potential confounders, intermediate and high serum lactate levels remained significantly associated with mortality within shock and nonshock strata.Initial serum lactate was associated with mortality independent of clinically apparent organ dysfunction and shock in patients admitted to the ED with severe sepsis. Both intermediate and high serum lactate levels were independently associated with mortality.
Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study
Peripheral venous and arterial lactate agreement in septic patients in the emergency department: a pilot study
DOI:10.1097/MEJ.0b013e328361321c
PMID:23591521
[Cited within: 1]

Lactate measurements are routinely used in sepsis for prognostication and for guiding treatment. Although venous lactate measurements have widely been used, most studies have used arterial lactate (A-LACT). The interchangeability between the measurements is debatable. This pilot study aimed to investigate whether an agreement exists between peripheral venous lactate (PV-LACT) and A-LACT with respect to sepsis in the Emergency Department (ED). PV-LACT lactate and A-LACT measurements were taken from a convenience sample of 37 patients presenting to a tertiary hospital ED between November 2010 and August 2011. The agreement between the paired measurements was assessed using Bland-Altman analysis. The mean difference between the measurements (venous-arterial) was 0.54 mmol/l, with 95% limits of agreement of -0.11 to 1.18 mmol/l. This pilot study demonstrates the potential use of PV-LACT as a substitute for A-LACT measurement in septic ED patients. However, further definitive investigation is needed to support widespread clinical adoption of peripheral venous lactate.
Association between early lactate levels and 30-day mortality in clinically suspected sepsis in children
DOI:10.1001/jamapediatrics.2016.3681 URL [Cited within: 2]
Effectiveness of arterial, venous, and capillary blood lactate as a sepsis triage tool in ED patients
PMID:25432592
[Cited within: 2]

We evaluate the capacity of arterial (ABL), peripheral venous (VBL), and capillary (CBL) blood lactate concentration to early detect the presence of severe sepsis in patients admitted to the emergency department for a septic syndrome.Patients with signs of sepsis presenting to the emergency department were prospectively enrolled. Blood lactate was measured using a handheld point-of-care analyzer on microsamples of arterial, peripheral venous, and capillary blood. An arterial blood sample was dispatched to the central laboratory as a reference measurement.A total of 103 patients were enrolled in the study, with 63 patients presenting with a severe sepsis. There was a strong correlation between the point of care and the reference blood lactate measurement. The CBL, VBL, and ABL were all significantly different (3.01±0.29, 2.51±0.21, and 2.03±0.18 mmol/L, respectively; P<.001). The VBL value was the most efficient to detect early the presence of severe sepsis (areas under the receiver operating characteristic curves were 0.85±0.04, 0.76±0.05, and 0.75±0.05 for VBL, ABL, and CBL, respectively; P<.01). Mortality at 28 days was related to the severity of sepsis (28.6% vs 7.5%) and to the number or organ dysfunctions (P<.01). Arterial blood lactate, VBL, and CBL were all significantly associated with the 28th-day mortality.Initial VBL may be used efficiently to assess the severity of sepsis, and it could even be more effective than ABL and CBL to early detect the presence of severe sepsis.
Venous lactate in predicting the need for intensive care unit and mortality among nonelderly sepsis patients with stable hemodynamic
DOI:10.1016/j.ajem.2015.04.010
PMID:25936479
[Cited within: 3]

Our study aims to investigate the role of initial venous lactate in predicting the probability of clinical deterioration and 30-day mortality in nonelderly sepsis patients with acute infections, without hemodynamic shock.We enrolled emergency department patients aged 18 to 65 years with acute major infections, but without organ hypoperfusion, and obtained a single venous lactate measurement at initial presentation. As the primary end point, the eligible patients were tracked for the need for vasopressor or mechanical ventilation (MV) in the next 72 hours. The patients' venous lactate and related risk factors were analyzed. We also followed the cohort and the predictors to investigate their prognostic role for 30-day mortality.Of 392 patients, 74 required vasopressor/MV, and 388 patients were available for mortality analysis. An initial lactate greater than or equal to 2 mmol/L was the strongest independent predictor for the requirement of vasopressor/MV (adjusted odds ratio, 6.2; 95% confidence interval, 3.4-11.3). The other independent risk factors were immunosuppressive drug users and positive blood culture. However, the initial lactate was not associated with 30-day mortality. The factors that were associated with mortality were the use of vasopressor/MV, active malignancy, Rapid Emergency Medicine Score greater than or equal to 6, and hospitalization within 90 days.In nonelderly sepsis patients with stable hemodynamic, elevated venous lactate (≥2 mmol/L) was associated with an increased probability of the need for vasopressor/MV. However, unfavorable medical histories and the severity of physiologic changes may be associated with short-term mortality to a greater extent than the single value of initial lactate.Copyright © 2015 Elsevier Inc. All rights reserved.
Relationship between arterial and peripheral venous lactate levels
PMID:8816193 [Cited within: 2]
Relationship between arterial and peripheral venous lactate levels
PMID:8816193 [Cited within: 1]
Therapeutic goal achievements during severe sepsis and septic shock resuscitation and their association with patients’ outcomes
Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit
DOI:10.1186/s13054-017-1658-5 URL [Cited within: 1]
Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department
DOI:10.1001/jama.2016.20329 URL [Cited within: 1]
Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit
Poor performance of quick-SOFA (qSOFA) score in predicting severe Sepsis and mortality - a prospective study of patients admitted with infection to the emergency department