INTRODUCTION
Septic cardiomyopathy (SCM) is reversible myocardial depression, which occurs in the early stages of sepsis and septic shock, however, definitions and diagnostic criteria have yet to be unified.[1,2] The echocardiographic parameters of left ventricular ejection fraction (LVEF) are routine measures and the clinical standard for assessing cardiac function. The threshold used to define “abnormal” is generally set according to an LVEF of between 40% and 50%.[2]Even though LVEF measures are non-invasive and readily available, results largely depend upon loading conditions.[1⇓-3] LVEF is the fraction of chamber volume ejected in systole (stroke volume) in relation to the volume of the blood in the ventricle at the end of diastole (end-diastolic volume). LVEF is widely considered a predictor of mortality, although it does not provide an accurate subclinical assessment of contractility. This means that LVEF is less useful for those with sepsis or septic shock patients because “normal” LVEF readings can be observed even in those with impaired contractility.
Speckle-tracking imaging technologies enable us to track “speckle” displacement using two-dimensional (2D) echocardiographic images.[4] This can be used to assess movement in the cardiac cycle or strain, which refers to the percentage of change in myocardial length/thickness compared to the initial length/thickness of the myocardium during contractions. These change percentages are measured longitudinally, radially, and across circumferential directions, providing further insights. This relatively new approach has an agreement with the current gold standard like cardiovascular magnetic resonance (CMR),[5,6] which is feasible, repeatable, and accurate. It would appear that speckle-tracking echocardiography (STE) provides a more sensitive measure of contractility and can be used to overcome many shortcomings of LVEF readings.
Global longitudinal strain (GLS) has reduced interobserver and intraobserver variability, and is more sensitive and specific in identifying subclinical LV systolic dysfunction.[7] GLS improves STE in terms of reproducibility and is considered easier for trainees to grasp. Over the past decade, studies have applied GLS technology to SCM and have found that strain measurements are not only more sensitive than conventional echocardiography, but also more accurate for patients with preserved LVEF,[8⇓-10] and could be used for diagnostics, prognostics, and longer-term follow-ups.[11,12] Few studies have explored the characteristics of myocardial function in the early stage of sepsis or septic shock or whether it is affected by infection severity such as shock state, which may be significant for sepsis or septic shock management. Therefore, it is necessary to understand whether early septic shock causes more strain changes than sepsis alone. It is also necessary to investigate the characteristics of strain parameters in sepsis and septic shock populations.
METHODS
Study setting
This is a cross-sectional study conducted in the Emergency Department (ED) of Peking Union Medical College Hospital. This facility is also the State Key Laboratory of Complex Severe and Rare Diseases. The study was conducted between 1st June and 31st December, 2021. The research protocol was approved by the Institutional Review Board (IRB) of Peking Union Medical College Hospital. Written informed consent was obtained from all patients (or their legal guardians) before being allowed to participate. The study was performed in accordance with the ethical standards established in the updated Declaration of Helsinki.
Participants
All patients who were admitted to the ED with acute infection were screened and diagnosed according to the standard definition, Sepsis 3.0[13] (supplementary Table 1), for complete inclusion and exclusion criteria. Resuscitation and management strategies were implemented according to the Surviving Sepsis Campaign (SSC) guidelines.[14]
Table 1. Two-dimensional echocardiographic parameters and laboratory tests of the investigated groups
| Variables | Sepsis 3.0 | cTnI (99th URL) 0.056 μg/L | LVEF_SB | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Septic shock (n=21) | Sepsis (n=39) | P | ≥99th URL (n=23) | <99th URL (n=37) | P | <50% (n=14) | ≥50% (n=46) | P | |
| Conventional echocardiography | |||||||||
| LVEF_Teich, % | 61.45±11.55 | 62.53±7.43 | 0.70 | 58.97±9.45 | 64.09±8.28 | 0.03* | 54.49±9.50 | 64.45±7.55 | 0.01* |
| LVEF_SB, % | 53.42±6.96 | 55.04±6.19 | 0.36 | 51.71±7.59 | 56.17±5.06 | 0.01* | 45.79±3.82 | 57.10±4.49 | 0.01* |
| CI, % | 29.88±16.59 | 28.81±12.76 | 0.77 | 28.39±14.46 | 29.68±14.09 | 0.73 | 0.27±0.16 | 0.30±0.13 | 0.49 |
| LVOT_VTI, mm | 16.52±3.94 | 17.22±3.59 | 0.50 | 15.74±3.80 | 17.74±3.46 | 0.04* | 14.63±3.72 | 17.69±3.41 | 0.01* |
| LVOT_SV, mL | 39.34±11.69 | 44.51±10.26 | 0.08 | 38.87±11.05 | 45.08±10.34 | 0.03* | 40.38±13.50 | 43.40±10.13 | 0.37 |
| LVOT_CO, L/min | 3.83±1.42 | 3.85±1.24 | 0.93 | 3.83±1.49 | 3.78±1.15 | 0.92 | 3.74±1.40 | 3.82±1.26 | 0.83 |
| E/A | 1.01±0.26 | 1.07±0.35 | 0.33 | 1 (0.90, 1.18) | 1 (0.94, 1.17) | 0.58 | 1 (1.00, 1.55) | 1 (0.91, 1.14) | 0.26 |
| e', cm/s | 12.48±3.84 | 12.12±3.04 | 0.69 | 12.23±3.51 | 12.23±3.20 | 0.95 | 12.55±4.20 | 12.13±3.01 | 0.68 |
| E/e' ratio (lateral) | 6.33±2.19 | 6.02±2.07 | 0.59 | 6.13±2.42 | 6.07±1.88 | 0.77 | 5.89±2.32 | 6.16±2.03 | 0.68 |
| Speckle-tracking echocardiography | |||||||||
| GLS, % | -15.48±3.43 | -16.59±3.82 | 0.27 | -14.74±4.21 | -17.11±3.06 | 0.02* | -12.29±2.61 | -17.39±3.12 | 0.01* |
| GCS, % | -17.19±4.77 | -16.38±4.17 | 0.50 | -15.17±4.31 | -17.59±4.19 | 0.04* | -14.14±4.00 | -17.43±4.22 | 0.01* |
| GRS, % | 22.81±5.68 | 19.87±5.56 | 0.06 | 19.35±5.89 | 21.86±5.49 | 0.09 | 18.79±5.40 | 21.54±5.73 | 0.12 |
| LVEF_STI, % | 49.00±10.81 | 50.78±9.59 | 0.52 | 46.61±11.37 | 52.36±8.43 | 0.03* | 38.31±8.25 | 53.76±7.34 | 0.01* |
| Laboratory test | |||||||||
| Platelet, ×109/L | 186.05±96.42 | 178.85±100.07 | 0.79 | 149.61±88.79 | 201.11±99.47 | 0.05 | 132.00±86.25 | 196.39±97.30 | 0.03* |
| CRP, mg/L | 127.48±89.94 | 152.93±81.46 | 0.64 | 150.67±82.50 | 160.19±80.60 | 0.66 | 171.75±87.04 | 151.91±79.18 | 0.43 |
| Procalcitonin, ng/L | 4.65 (0.58, 16.50) | 6.00 (1.00, 16.00) | 0.17 | 10.00 (2.90, 74.00) | 5.30 (1.40, 18.00) | 0.04* | 10.00 (5.25, 91.00) | 5.20 (1.30, 17.00) | 0.14 |
| cTnI, ng/mL | 0.03 (0, 0.68) | 0.02 (0, 0.02) | 0.23 | 0 (0, 3.00) | 0.02 (0, 0.02) | 0.01* | 0.02 (0, 3.25) | 0.02 (0, 0.02) | 0.16 |
| NT-proBNP, ng/mL | 2989 (1002, 9663) | 1031 (165, 5423) | 0.02* | 6436 (2763, 17254) | 881 (200, 1596) | 0.01* | 12026 (4929, 18810) | 1028 (246, 2832) | 0.01* |
| CK, U/L | 108 (68, 391) | 72 (34, 271) | 0.31 | 180 (74, 414) | 63 (32, 136) | 0.30 | 233 (61, 945) | 75 (35, 248) | 0.11 |
| CK-MB, U/L | 1.8 (0.8, 5.7) | 1.0 (0, 2.0) | 0.05 | 2.0 (1.0, 9.0) | 1.0 (0, 2.0) | 0.10 | 2.0 (1.0, 18.0) | 1.0 (0, 2.1) | 0.02* |
| Cr, μmol/L | 156 (106, 224) | 87 (59, 139) | 0.01* | 136 (94, 209) | 95 (58, 150) | 0.05 | 159 (82, 232) | 103 (63, 146) | 0.09 |
| Lac, mmol/L | 3.3 (2.2,5.4) | 2.0 (1.0, 2.0) | 0.01* | 2.0 (2.0, 4.0) | 2.0 (1.0, 3.0) | 0.29 | 2.5 (2.0, 5.3) | 2.0 (1.0, 3.0) | 0.09 |
Data are presented as means with standard deviations, medians (lower quartile to upper quartile) or number (n) of patients (%), as appropriate. *P<0.05. cTnI: cardiac troponin I; LVEF: left ventricular ejection fraction; Teich: Teichholz's formula; SB: Simpson's biplane; CI: collapsibility index (inferior vena cava); LVOT: left ventricular outflow tract; VTI: velocity-time integral; SV: stroke volume; CO: cardiac output; E/A: ratio of early to late mitral inflow peak velocity; e': early diastolic mitral annular velocity; E/e': ratio of early trans-mitral flow velocity to the early diastolic mitral annular velocity; GLS: global longitudinal strain; GCS: global circumferential strain; GRS: global radial strain; STI: speckle- tracking imaging; CRP: C-reactive protein; NT-proBNP: N-terminal pro-B-type natriuretic peptide; CK: creatine kinase; CK-MB: creatine kinase-myocardial band isoenzyme; Cr: creatinine; Lac: lactic acid.
Transthoracic echocardiography
Echocardiographic parameters were collected within 24 h of sepsis or septic shock diagnosis, and after the standard three-hour bundle determining in the SSC guidelines. Point-of-care transthoracic echocardiograms (TTE) were performed on patients with a supine position and from a left lateral position using a Mindray M9 (Mindray Bio-Medical Electronics Co., Ltd., China). We adhered to image standards as recommended by the American Society of Echocardiography.[15] All examinations were performed by certified emergency specialists under the supervision of a certified cardiologist.
LVEF was measured using both the Teichholz's method (LVEF_Teich) which used M-mode, and Simpson's biplane method (LVEF_SB) from the left four- to two-chamber apical views. The following measures were made to assess diastolic functions: early (E) and late (A) mitral inflow peak velocities, as well as early diastolic mitral annular velocity (e') which were acquired at the lateral mitral annuli with tissue Doppler imaging (TDI). Ratios for early trans-mitral flow velocity to the early diastolic mitral annular velocity (E/e') were calculated. Velocity-time integral (VTI) for the left ventricular outflow tract (LVOT) was measured using Doppler echocardiography to calculate stroke volume (SV) and cardiac output (CO). Cardiac preload was indirectly estimated by measuring the diameter of inferior vena cava (IVC) and inspiratory collapsibility index (CI).
2D-speckle-tracking and post-processing analysis
Imaging standards were set according to the consensus of the European Association of Cardiovascular Imaging and the American Society of Echocardiograph.[4] GLS was calculated from the three standard apical perspectives, i.e., two-, three-, and four-chamber views. Global circumferential strain (GCS) and global radical strain (GRS) were measured from parasternal short-axis views, from the left ventricular mitral valve, papillary muscles, to the apex. Images were obtained at a frame rate of 50-90 frames/s. By recording at least three consecutive cardiac cycles, the best single cardiac cycle was selected according to image quality and tracking quality. Images were rejected if they were of poor quality or if we could not track two or more adjacent segments.
Mindray TT-QA software (Mindray Bio-Medical Electronics Co., Ltd., China) was provided with the apparatus and can automatically trace a region of interest (ROI) using a point-and-click approach. Adjustments can also be made in accordance with the width of the ROI to achieve the best alignment. Thereafter, three apical images and two parasternal short-axis images were divided into six standard segments using the Mindray M9 apparatus. Meanwhile, the apical levels for parasternal short axes were divided into four segments. The corresponding number of time-strain curves were generated in each section, which jointly outlined the entire left ventricular wall. GLS, GRS, and GCS were the average systolic peaks of the segments, which were expressed as change percentages. Negative GLS and GCS values, as well as positive GRS values, were taken to represent myocardial contractility. All echocardiographic interpreters were blinded to all clinical data at the time of image analysis.
Clinical data
Glasgow Coma Scale (GCS) scores, Sequential Organ Failure Assessment (SOFA) scores, and Acute Physiology and Chronic Health Evaluation II (APACHE II) scores at the time of admission were collected. Data taken around the time of TTE were collected, including demographics, vital signs, hemodynamic, respiratory, laboratory results, and comorbidities. Sources of infection were identified using body fluid cultures, including blood, alveolar lavage fluid, urine, serous effusion, cerebrospinal fluid, and wound swab.
Subgrouping
Subgroups were based on the criteria provided in Sepsis 3.0[13] and through consensus for proposed values of analyzed SCM variables (cTnI and LVEF_SB).[1,2]All participants were further subdivided according to the following three grouping standards: (1) septic shock, sepsis (without shock); (2) cTnI ≥99th percentile upper reference limit (URL) 0.056 μg/L, cTnI <99th URL 0.056 μg/L; (3) LVEF_SB ≥50%, LVEF_SB <50%.
Statistical analysis
Data were presented as means with standard deviations or as simple count data (or proportions), as indicated. The Student's t-test was performed to compare characteristics, laboratory tests, and echocardiographic parameters between groups when distribution was considered normal. Alternately, the Mann-Whitney U-test was implemented when normal distribution was not evident.
Categorical data were compared using standard Chi-square tests. Bivariate correlations were summarized using a correlation matrix to assess relations between cardiac systolic and diastolic, hemodynamic indexes and myocardial injury markers. The R-value for indexes with obvious correlations in the heat map was calculated using Pearson's or Spearman's coefficients.
Statistical analysis was performed using R (version 4.1.2). Graphs were created using GraphPad Prism software (version 8.0.2) and MedCalc statistical software (version 20.023). The corrplot package in R was used to calculate correlation coefficients and consider the significance of each correlation in the heat-mapping algorithm. The two-tailed P-value of 0.05 was set as the threshold for statistical significance.
RESULTS
Recruitment
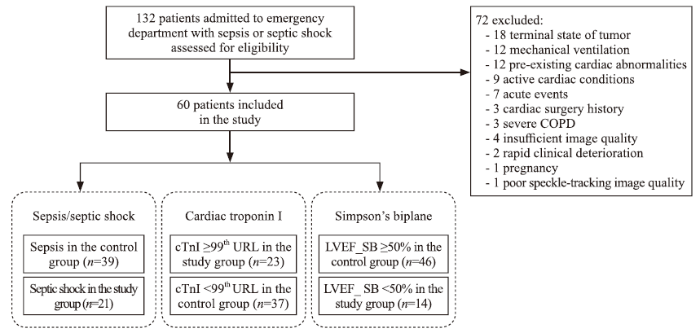
A total of 132 consecutive adult patients who had been admitted to the ED for sepsis or septic shock were recruited. After exclusion, 60 patients were considered eligible for further analysis. Details of exclusion processes and subgroups are provided in Figure 1.
Figure 1.
Figure 1.
Flowchart for participant assignment. cTnI: cardiac troponin I; LVEF: left ventricular ejection fraction; SB: Simpson's biplane; COPD: chronic obstructive pulmonary disease; 99th URL: 99 percentile upper reference limit.
Patient characteristics
Demographics and clinical parameters are provided in supplementary Table 2. Age and gender distributions did not differ significantly between the three subgroups. The subgroups were well-balanced with regards GCS, co-morbidities and in terms of the infection sources.
The patients with septic shock had a higher heart rate (HR) (P=0.04) and norepinephrine (NE) doses (P=0.01), as well as a lower systolic blood pressure (SBP) (P=0.01) and diastolic blood pressure (DBP) (P=0.01) compared to the patients with sepsis.
SOFA and APACHE II scores were significantly higher in the septic shock subgroup and in the LVEF_SB <50% subgroup (P=0.01). Levels of partial pressure of arterial oxygen to fraction of inspired oxygen (P/F) were significantly lower in the septic shock subgroup (P=0.03) and in the LVEF_SB <50% subgroup (P=0.02).
Conventional echocardiographic data
Conventional echocardiographic parameters across subgroups have been provided in Table 1. Differences in LVEF_Teich, LVEF_SB, LVOT_VTI, LVOT_SV, LVOT_ CO, E/A, e', E/e', and CI were not statistically significant between the septic shock and sepsis subgroups. However, LVEF_Teich and LVEF_SB decreased significantly in patients with cTnI ≥99th URL compared to patients with cTnI <99th URL (P=0.03, P=0.01, respectively). Additionally, LVEF_Teich, LVEF_SB, and LVOT_VTI significantly decreased in patients with LVEF_SB <50% compared to patients with LVEF_SB ≥50% (all P=0.01).
Speckle-tracking echocardiographic data
STE parameters across subgroups have also been provided in Table 1. There were no significant differences in GLS, GCS GRS, or LVEF_STI between the subgroups of patients with septic shock and sepsis (all with P>0.05). The analysis of GLS and GCS revealed that strain was significantly less negative in the subgroup of patients with cTnI ≥99th URL compared to the patients with cTnI < 99th URL (P=0.02, P=0.04, respectively). Additionally, GLS and GCS were significantly also less negative in the subgroup of patients with LVEF_SB <50% compared to the subgroup of patients with LVEF_SB ≥50% (both P=0.01).
The values of left ventricular systolic function assessed by GLS were significantly higher (which indicates poorer contractility) in the subgroup of patients with abnormal cTnI and LVEF_SB levels (-14.74%±4.21% in cTnI≥99th vs. -17.11%±3.06% in cTnI<99th URL, P=0.02; -12.29%±2.61% in LVEF_SB<50% vs. -17.39%±3.12% in LVEF_SB≥50%, P=0.01) compared to their counterparts. No significant differences were identified between septic shock and sepsis subgroups in this regard (-15.48%±3.43% vs. -16.59%±3.82%, P=0.27) (supplementary Figure 1).
Laboratory tests
Laboratory test results are provided in Table 1. N-terminal pro-B-type natriuretic peptide (NT-proBNP) (P=0.02), Cr (P=0.01), and lactate (P=0.01) levels were significantly higher in patients with septic shock compared to patients with sepsis.
In the subgroup of patients with cTnI ≥99th URL, the level of procalcitonin (PCT) (P=0.04) and NT-proBNP (P=0.01) were significantly higher compared to patients with cTnI <99th URL.
NT-proBNP and creatine kinase-myocardial band isoenzyme (CK-MB) levels were significantly higher in the patients with LVEF_SB <50% compared to patients with LVEF_SB ≥50% (P=0.01, P=0.02, respectively), while the platelet (PLT) count was significantly lower in the subgroup of same patients (P=0.03).
Correlation between echocardiographic variables and laboratory tests
In the supplementary Figure 2 which provides a correlation matrix, contractility indices including LVEF_SB and LVEF_STI correlated with non-invasive hemodynamic parameter of LVOT_VTI to some degree and negatively correlated with strain indices, including GLS and GCS.
Cardiac injury indices including cTnI and NT-proBNP positively correlated with GLS. There was also a negative correlation between GLS and LVEF_SB, LVEF_STI and LVOT_VTI.
Diastolic function indices including E/A, e', E/e' were not significantly associated with other echocardiographic variables or laboratory tests. Indices reflecting disease severity, such as SOFA and APACHE II scores, also did not appear significant in relation to echocardiographic variables.
The main correlations between investigated laboratory tests and echocardiographic parameters observed in the correlation matrix have been summarized. We found a significant negative correlation between GLS and LVEF_SB (r= -0.69, P<0.001) and a moderate correlation between GCS and LVEF_SB (r= -0.39, P=0.002), although there was no significant correlation between GRS and LVEF_SB (P=0.199). In addition, there was a moderate correlation between GLS and GCS (r= 0.47, P<0.001).
For echocardiographic variables and serum biomarkers, GLS positively correlated with cardiac injury indices including both cTnI (r=0.40, P=0.002) and NT-proBNP (r=0.44, P=0.001). Both cTnI and NT-proBNP were found to negatively correlate with LVEF_SB (r= -0.36, P=0.005; r= -0.38, P=0.003, respectively). Please see supplementary Figure 3 for further details.
DISCUSSION
This study attempted to gain insight into whether early septic shock causes more strain changes than sepsis alone. We also planned to investigate the characteristics of strain parameters in sepsis and septic shock populations. We found there was no significant difference in early strain parameters between patients with sepsis and septic shock (P>0.05). However, we also found that strain parameters for GLS and GCS were significantly less negative (both P<0.05) in subgroups of patients with abnormal troponin levels (cTnI ≥99th URL) and LVEF values (LVEF_SB <50%). Additionally, we identified significant but moderate correlations between GLS and cTnI, NT-proBNP levels (both P<0.05).
Previous studies carried out by Shahul et al,[16]Lanspa et al,[17] and Innocenti et al[18] analyzed echocardiographic findings for patients within 24 h of admission to intensive care unit (ICU), and found no association between septic shock and GLS or LVEF. Other studies found significantly lower GLS values in ICU patients with septic shock (P<0.001).[9,10] One might postulate that different time windows for measurements might cause different results. In addition to participant characteristics, it is necessary to factor in context. The study conducted by Shahul et al[16] found a significant decrease of GLS in patients with septic shock (P<0.001) only after 24 h in ICU, which may provide an explanation. Our study was conducted in an ED (rather than in an ICU) and therefore, conventional echocardiography and STE were performed after the initial three hours of resuscitation and once patients had been diagnosed with sepsis or septic shock. This may be the reason why we did not observe an association between shock and subclinical myocardial dysfunction. Further artificial intelligence studies will likely provide more insight, although interconnected, national (and international) datasets are needed.
The underlying mechanisms involved in strain changes in sepsis and septic shock are not fully understood. While there is a possibility that microvascular contraction in the highly vulnerable subendocardial muscle layer may lead to ischemic injury, longitudinal fibers are also highly prone to ischemia.[2,19] Compared with other echocardiographic parameters, GLS provides insight into the systolic shortening of LV from the base to apex, and provides information on LV emptying and dilation, which appears to hold superior diagnostic strength.[20] GLS has been proven more sensitive to early myocardial systolic abnormalities compared to conventional echocardiographic methods,[21,22] and therefore could reflect the severity of the infection.[23]However, this evidence comes from animal modelling which does not always apply to humans. Evidence has emerged that GLS has high clinical applicability and an overall GLS of greater than -18% is usually accepted as abnormal,[24]but this cut-off has yet to be validated because there is no official consensus for the cut-off for SCM. Many studies have reported that a cut-off of -15%[10,25⇓⇓-28] would be appropriate, although this may vary substantially within samples. Therefore, it would seem prudent to incorporate GLS into clinical practice as a supplementary parameter for LVEF, as this would help us to understand SCM.
Our study uncovered a suggestive effect of early troponin elevation rather than septic shock on myocardial dysfunction. Despite implementing more rigorous inclusion and exclusion criteria, we did not observe a significant difference in troponin levels between the sepsis and septic shock subgroups. However, under troponin-based subgroup analysis, we found that an abnormal troponin level can manifest with less negative GLS, GCS and lower LVEF. Previous research[29] has found a strong correlation between cardiac troponin, infection severity, and sepsis prognosis. However, due to their lack of evaluation of cardiac function and morphology, there is no direct evidence around elevated troponin levels in relation to potential abnormal cardiac stress and injury. A previous study has included echocardiography and found that abnormal levels of troponin are related to sepsis-induced myocardial dysfunction, which has an independent prognostic value.[26]In addition, we also observed a moderate correlation of troponin level with GLS and LVEF (r=0.40, P=0.002 and r= -0.36, P=0.005). This may enable us to identify global muscle dysfunction, simultaneously allowing us to better understand the pathophysiology of SCM. Therefore, the timing of echocardiography is important and should be considered with the rationalization of medical resources. We believe that it is necessary to carry out routine echocardiography early in the infection to understand abnormal troponin levels and STE to identify subclinical myocardial systolic dysfunction.
We included cardiac morphology analysis in this study, and found that NT-proBNP was related to cardiac performance. Circulating NT-proBNP was significantly higher in patients with septic shock, and in those with abnormal cTnI and LVEF_SB. There also appeared to be a modest correlation in NT-proBNP with both GLS (r=0.44) and LVEF_SB (r= -0.38). This means that circulating NT-proBNP was likely related to septic shock occurrences.[29]However, NT-proBNP is affected by fluid loading conditions, especially after resuscitation of sepsis or septic shock, and therefore we cannot recommend this biomarker for SCM analysis.
Strength and limitations
Compared with most clinical studies conducted in ICUs, this rather novel study is one of the few to include strain measurement in an ED setting. That is, we tried to advance the inspection time window to the end of initial resuscitation, after diagnosing sepsis or septic shock. This helps us respond to the conditions under which we conduct bedside echocardiographic assessment for patients at risk of SCM. Additionally, drawing on the evidence from previous relevant studies, we embedded very strict eligibility criteria to control for potential confounding factors and formulated criteria by excluding the effects of pre-existing cardiopulmonary disease, acute medical conditions other than infections, iatrogenic mechanical support, etc.
There were a number of limitations. Patients in the ED are usually assigned to final inpatient destinations within 48 hours, so we were unable to obtain dynamic changes in indicators during the course of the disease. Additionally, we could not rule out the possible evolution of left and right ventricular dysfunction. We also could not explore individual demographic or clinical factors, nor could we apply multivariate analysis to this sample because we had so few participants.
CONCLUSIONS
Evidence from this single ED study shows that myocardial dysfunction, such as lower LVEF or less negative GLS values in patients with sepsis or septic shock, is more affected by myocardial injury. The GLS may be incorporated into the mainstream clinical practice as a supplementary parameter for LVEF in patients with elevated troponin levels. Early screening and intervention for these patients may improve the prognosis, although we need to work together to develop larger datasets for modelling and to develop artificial intelligence algorithms. Further research is needed to define cut-off values and to understand tachycardia and the hemodynamic effects in SCM patients.
Funding: None.
Ethics approval: The research protocol was approved by the Institutional Review Board of Peking Union Medical College Hospital. Written informed consent was obtained from all patients (or their legal representatives) before being allowed to participate.
Conflicts of interests: All the authors declare that they have no conflicts of interest.
Contributors: XF and JX: conceived and designed the study; XZY: study design assessment; XF: data acquisition; XF and LNZ: statistical analysis; FX: manuscript preparation; SS: manuscript editing; XL an HDZ: provided critical appraisal of the study; JX and ZXY: manuscript review. All authors read and approved the final manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Pathophysiology of sepsis-induced cardiomyopathy
DOI:10.1038/s41569-020-00492-2
PMID:33473203
[Cited within: 3]

Sepsis is the life-threatening organ dysfunction caused by a dysregulated host response to infection and is the leading cause of death in intensive care units. Cardiac dysfunction caused by sepsis, usually termed sepsis-induced cardiomyopathy, is common and has long been a subject of interest. In this Review, we explore the definition, epidemiology, diagnosis and pathophysiology of septic cardiomyopathy, with an emphasis on how best to interpret this condition in the clinical context. Advances in diagnostic techniques have increased the sensitivity of detection of myocardial abnormalities but have posed challenges in linking those abnormalities to therapeutic strategies and relevant clinical outcomes. Sophisticated methodologies have elucidated various pathophysiological mechanisms but the extent to which these are adaptive responses is yet to be definitively answered. Although the indications for monitoring and treating septic cardiomyopathy are clinical and directed towards restoring tissue perfusion, a better understanding of the course and implications of septic cardiomyopathy can help to optimize interventions and improve clinical outcomes.
Septic cardiomyopathy
DOI:10.1097/CCM.0000000000002851
PMID:29227368
[Cited within: 4]

To describe, with an emphasis on clinical applications, what is known about the pathophysiology, management, and implications of septic cardiomyopathy in the adult ICU.A PubMed literature review was performed for relevant articles. Only articles in English that studied human adults with sepsis were included.Multiple competing definitions for septic cardiomyopathy hinder understanding of this entity. Although many patients with sepsis develop cardiac dysfunction, the impact of septic cardiomyopathy on prognosis and therapy remains to be demonstrated. Treatment of septic cardiomyopathy is aimed at treating the underlying sepsis and providing specific supportive care for cardiogenic shock when present.Septic cardiomyopathy is an important contributor to organ dysfunction in sepsis. Guided treatment of septic cardiomyopathy may affect patients' prognosis, especially when their cardiac index is substantially decreased. The implication of septic cardiomyopathy for both short- and long-term outcomes is an important area for future investigation.
Current status of septic cardiomyopathy: basic science and clinical progress
DOI:10.3389/fphar.2020.00210 URL [Cited within: 1]
Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry task force to standardize deformation imaging
DOI:10.1093/ehjci/jeu184 URL [Cited within: 2]
Test-retest reliability of left and right ventricular systolic function by new and conventional echocardiographic and cardiac magnetic resonance parameters
DOI:10.1093/ehjci/jeaa206 URL [Cited within: 1]
Global longitudinal strain and global circumferential strain by speckle-tracking echocardiography and feature-tracking cardiac magnetic resonance imaging: comparison with left ventricular ejection fraction
The use of machine learning for the care of hypertension and heart failure
DOI:10.1016/j.jacasi.2021.07.005 URL [Cited within: 1]
Outcome prediction in sepsis: speckle tracking echocardiography based assessment of myocardial function
DOI:10.1186/cc13987 URL [Cited within: 1]
Speckle tracking echocardiography in patients with septic shock: a case control study (SPECKSS)
DOI:10.1186/s13054-016-1327-0 URL [Cited within: 2]
Prognostic role of left ventricular systolic function measured by speckle tracking echocardiography in septic shock
Left ventricular systolic function evaluated by strain echocardiography and relationship with mortality in patients with severe sepsis or septic shock: a systematic review and meta-analysis
DOI:10.1186/s13054-018-2113-y URL [Cited within: 1]
Global longitudinal strain using speckle-tracking echocardiography as a mortality predictor in sepsis: a systematic review
DOI:10.1177/0885066618761750
PMID:29552957
[Cited within: 1]

The data on speckle-tracking echocardiography (STE) in patients with sepsis are limited. This systematic review from 1975 to 2016 included studies in adults and children evaluating cardiovascular dysfunction in sepsis, severe sepsis, and septic shock utilizing STE for systolic global longitudinal strain (GLS). The primary outcome was short- or long-term mortality. Given the significant methodological and statistical differences between published studies, combining the data using meta-analysis methods was not appropriate. A total of 120 studies were identified, with 5 studies (561 patients) included in the final analysis. All studies were prospective observational studies using the 2001 criteria for defining sepsis. Three studies demonstrated worse systolic GLS to be associated with higher mortality, whereas 2 did not show a statistically significant association. Various cutoffs between -10% and -17% were used to define abnormal GLS across studies. This systematic review revealed that STE may predict mortality in patients with sepsis; however, the strength of evidence is low due to heterogeneity in study populations, GLS technologies, cutoffs, and timing of STE. Further dedicated studies are needed to understand the optimal application of STE in patients with sepsis.
The third international consensus definitions for sepsis and septic shock (Sepsis 3.0)
DOI:10.1001/jama.2016.0287 URL [Cited within: 2]
Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock 2021
DOI:10.1097/CCM.0000000000005337 URL [Cited within: 1]
Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging
DOI:10.1016/j.echo.2014.10.003 URL [Cited within: 1]
Detection of myocardial dysfunction in septic shock: a speckle-tracking echocardiography study
DOI:10.1213/ANE.0000000000000943
PMID:26397444
[Cited within: 2]

Patients with septic shock are at increased risk of myocardial dysfunction. However, the left ventricular ejection fraction (EF) typically remains preserved in septic shock. Strain measurement using speckle-tracking echocardiography may quantify abnormalities in myocardial function not detected by conventional echocardiography. To investigate whether septic shock results in greater strain changes than sepsis alone, we evaluated strain in patients with sepsis and septic shock.We prospectively identified 35 patients with septic shock and 15 with sepsis. These patients underwent serial transthoracic echocardiograms at enrollment and 24 hours later. Measurements included longitudinal, radial, and circumferential strain in addition to standard echocardiographic assessments of left ventricular function.Longitudinal strain worsened significantly over 24 hours in patients with septic shock (P < 0.0001) but did not change in patients with sepsis alone (P = 0.43). No significant changes in radial or circumferential strain or EF were observed in either group over the 24-hour measurement period. In patients with septic shock, the significant worsening in longitudinal strain persisted after adjustment for left ventricular end-diastolic volume and vasopressor use (P < 0.0001). In patients with sepsis, adjustment for left ventricular end-diastolic volume and vasopressor use did not alter the finding of no significant differences in longitudinal strain (P = 0.48) or EF (P = 0.96).In patients with septic shock, but not sepsis, myocardial strain imaging using speckle-tracking echocardiography identified myocardial dysfunction in the absence of changes in EF. These data suggest that strain imaging may play a role in cardiovascular assessment during septic shock.
Associations among left ventricular systolic function, tachycardia, and cardiac preload in septic patients
DOI:10.1186/s13613-017-0240-2 URL [Cited within: 1]
Prognostic stratification in septic patients with overt and cryptic shock by speckle tracking echocardiography
DOI:10.1007/s11739-020-02545-3 URL [Cited within: 1]
10 years of speckle tracking echocardiography: still a novel technique or a definite tool for clinical practice
Assessment of left ventricular function by echocardiography: the case for routinely adding global longitudinal strain to ejection fraction
DOI:10.1016/j.jcmg.2017.11.017 URL [Cited within: 1]
2D speckle tracking imaging to assess sepsis induced early systolic myocardial dysfunction and its underlying mechanisms
Advantages of strain echocardiography in assessment of myocardial function in severe sepsis: an experimental study
DOI:10.1097/CCM.0000000000000310 URL [Cited within: 1]
Systolic dysfunction by two-dimensional speckle tracking echocardiography in dogs with parvoviral enteritis
DOI:10.1016/j.jvc.2021.01.006 URL [Cited within: 1]
Head-to-head comparison of global longitudinal strain measurements among nine different vendors: the EACVI/ASE inter-vendor comparison study
DOI:10.1016/j.echo.2015.06.011 URL [Cited within: 1]
SOFA score and left ventricular systolic function as predictors of short-term outcome in patients with sepsis
DOI:10.1007/s11739-016-1579-3 URL [Cited within: 1]
Comparison of Troponin I levels versus myocardial dysfunction on prognosis in sepsis
DOI:10.1007/s11739-021-02701-3 URL [Cited within: 2]
Strain echocardiography identifies impaired longitudinal systolic function in patients with septic shock and preserved ejection fraction
DOI:10.1186/s12947-015-0025-4 URL [Cited within: 1]
Characteristics of Sepsis-induced cardiac dysfunction using speckle-tracking echocardiography: a feasibility study
DOI:10.1177/0310057X1604400111 URL [Cited within: 1]
Sequential N-terminal pro-B-type natriuretic peptide and high-sensitivity cardiac troponin measurements during albumin replacement in patients with severe sepsis or septic shock
DOI:10.1097/CCM.0000000000001473
PMID:26571184
[Cited within: 2]

Myocardial dysfunction is a frequent complication in patients with severe sepsis and can worsen the prognosis. We investigated whether circulating biomarkers related to myocardial function and injury predicted outcome and were associated with albumin replacement.A multicenter, randomized clinical trial about albumin replacement in severe sepsis or septic shock (the Albumin Italian Outcome Sepsis trial).Forty ICUs in Italy.Nine hundred and ninety-five patients with severe sepsis or septic shock.Randomization to albumin and crystalloid solutions or crystalloid solutions alone.Plasma concentrations of N- terminal pro-B-type natriuretic peptide and high-sensitivity cardiac troponin T were measured 1, 2, and 7 days after enrollment. We tested the relationship of single marker measurements or changes over time with clinical events, organ dysfunctions, albumin replacement, and ICU or 90-day mortality in the overall population and after stratification by shock. N-terminal pro-B-type natriuretic peptide levels were abnormal in 97.4% of the patients and high-sensitivity cardiac troponin T in 84.5%, with higher concentrations in those with shock. After extensive adjustments, N-terminal pro-B-type natriuretic peptide concentrations predicted ICU or 90-day mortality, better than high-sensitivity cardiac troponin T. Early changes in N-terminal pro-B-type natriuretic peptide or high-sensitivity cardiac troponin T concentrations were independently associated with subsequent mortality in patients with shock. Patients given albumin had significantly higher N-terminal pro-B-type natriuretic peptide levels; in addition, early rise in N-terminal pro-B-type natriuretic peptide was associated with a better outcome in this subgroup.Circulating N-terminal pro-B-type natriuretic peptide and high-sensitivity cardiac troponin T are frequently elevated in severe sepsis or septic shock and have relevant prognostic value, which may be important in monitoring the clinical efficacy of supporting therapy.