INTRODUCTION
Acute coronary syndrome (ACS) is a critical manifestation of coronary artery disease (CAD) with high mortality and disability. Although CAD is common in older individuals, the incidence is increasing in middle-aged and young populations (early-onset CAD). Early-onset CAD has serious consequences, such as early death and long-term disability.[1,2]
Metabolic syndrome is associated with ACS in patients <45 years of age and is more valuable than established cardiovascular risk factors,[3] and obesity is the most prevalent risk factor for ACS in young adults.[4] However, with improvements in living standards and an increase in the incidence of metabolic syndrome, the impact of metabolic syndrome on ACS onset age is unclear in China. Furthermore, the long-term prognosis of patients with early-onset ACS is controversial. During a 10.3-year follow-up of patients with premature acute myocardial infarction (AMI), 23% of patients experienced major adverse cardiovascular events. Of these patients, 6% died, 17% experienced re-AMI, and 5% suffered ischemic stroke.[5] Another study showed a favorable prognosis with short- and medium-term follow-ups of young patients with AMI.[6] Here, we aim to investigate effects of metabolic syndrome on onset age and long-term outcomes in patients with ACS.
METHODS
Study population
A total of 6,431 patients with ACS who underwent percutaneous coronary intervention (PCI) at Fuwai Hospital, National Center for Cardiovascular Diseases (Beijing, China), from January to December 2013, were enrolled. Early-onset CAD was defined in males ≤50 years of age and females ≤60 years of age.[7] After excluding patients with previous myocardial infarction (MI), previous PCI, and previous coronary artery bypass graft, 1,558 patients conformed to the definition of early-onset ACS (including unstable angina pectoris, non-ST-segment elevation MI, and ST-segment elevation MI), and 3,044 patients were allocated to the late-onset ACS group. The study protocol was approved by our institutional review board, and written informed consent was obtained from patients before intervention. The study was approved by the ethics committee of the hospital (ethical application number: IRB2012-BG-006; approval number: 2013-449).
Procedures, medications, and patient follow-up
The PCI strategy and stent type were at the treating physician’s discretion. Patients scheduled for PCI received standardized drug treatment before and after the procedure. All patients were followed up in the hospital and evaluated by clinic visits or by phone after one month, six months, one year, two years, and five years. Patients were advised to return for coronary angiography if clinically indicated by symptoms or signs of myocardial ischemia.
Definitions
Major adverse cardiovascular and cerebrovascular events (MACCEs), including all-cause death, cardiac death, recurrent MI, stent thrombosis, target vessel revascularization (TVR), recurrent stroke, and bleeding events, were assessed during a five-year follow-up. MI was defined in accordance with the third universal definition of MI.[8] Unplanned TVR was defined as event-driven repeat PCI or surgical bypass of any segment of the target vessel for ischemic symptoms.[9] Stent thrombosis was defined in accordance with the Academic Research Consortium’s definition and was classified as definite, probable, or possible.[9] Bleeding was quantified in accordance with Bleeding Academic Research Consortium criteria, and types 2-5 were included in the analysis.[10]
Metabolic syndrome included obesity, hypertension, diabetes mellitus, hypertriglyceridemia, and low high-density lipoprotein cholesterol (HDL-C). Obesity was defined as body mass index (BMI) ≥28 kg/m2. Hypertension was defined as a history of hypertension and in-hospital blood pressure >130/85 mmHg (1 mmHg=0.133 kPa). Hypertriglyceridemia was definite as triglyceride (TG) concentration ≥1.7 mmol/L, and low HDL-C was defined as HDL-C concentration <1.04 mmol/L. If patients demonstrated 3-5 of these criteria, they were diagnosed with metabolic syndrome.
Statistical analysis
Continuous variables were compared using the Student’s t-test, and categorical variables were compared using Pearson’s χ2 test. Continuous variables were presented as mean±standard deviation and categorical variables as the number with frequency. Survival curves were calculated using Kaplan-Meier estimates and compared using the log-rank test for endpoints. The results of logistic regression were expressed as odds ratios (ORs) and 95% confidence intervals (CIs). Clinical and statistical covariates entered into the model and adjusted in the multivariate analysis. All statistical analyses were performed using SPSS version 19.0 (IBM Corp., Armonk, New York, USA). Significance was set at a two-sided P-value <0.05.
RESULTS
Baseline characteristics
The response rate of the five-year follow-up was 91.5%. The proportions of patients with early-onset ACS (n=1,558) and late-onset ACS (n=3,044) with no previous CAD history (n=4,602) were 33.9% and 66.1%, respectively. Patients’ basic characteristics are shown in Table 1.
Table 1 Patients’ baseline characteristics between two groups
| Parameters | Early-onset ACS (n=1,558) | Late-onset ACS (n=3,044) | P-value | ||
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years) | 47.27±6.30 | 63.17±7.60 | <0.001* | ||
| Female, n (%) | 404 (25.9) | 737 (24.2) | 0.201 | ||
| BMI (kg/m2) | 26.49±3.31 | 25.51±3.13 | <0.001* | ||
| Risk factors and medical history, n (%) | |||||
| Hypertension history | 946 (60.7) | 1,959 (64.4) | 0.016* | ||
| Diabetes mellitus | 391 (25.1) | 866 (28.4) | 0.016* | ||
| Hyperlipidemia | 1,103 (65.0) | 1,915 (62.9) | 0.159 | ||
| Family history of CAD | 431 (27.7) | 690 (22.7) | <0.001* | ||
| Smoking history | 895 (57.4) | 1,696 (55.7) | 0.510 | ||
| Previous stroke | 79 (5.1) | 392 (12.9) | <0.001* | ||
| Peripheral vascular disease | 16 (1.0) | 69 (2.3) | 0.003* | ||
| Examination | |||||
| White blood cell count before PCI (×109/L) | 7.12±1.91 | 6.90±1.85 | <0.001* | ||
| HGB before PCI (g/L) | 143.46±15.43 | 139.26±16.27 | <0.001* | ||
| PLT before PCI (×109/L) | 223.58±57.09 | 206.97±56.22 | <0.001* | ||
| HbAlc (%) | 6.53±1.33 | 6.56±1.18 | 0.483 | ||
| B-brain natriuretic peptide (pg/mL) | 680.73±386.46 | 804.05±719.57 | <0.001* | ||
| Big endothelin (pmol/L) | 0.26±0.22 | 0.29±0.27 | <0.001* | ||
| Erythrocyte sedimentation rate (mm/h) | 11.35±11.46 | 12.51±12.66 | 0.003* | ||
| TC (mmol/L) | 4.35±1.13 | 4.21±0.99 | <0.001* | ||
| LDL-C (mmol/L) | 2.62±0.96 | 2.52±0.85 | <0.001* | ||
| HDL-C (mmol/L) | 0.98±0.27 | 1.05±0.29 | <0.001* | ||
| Triglyceride (mmol/L) | 2.04±1.27 | 1.70±0.97 | <0.001* | ||
| Uric acid (µmol/L) | 348.50±87.75 | 334.56±83.25 | <0.001* | ||
| eGFR (mL/[minute·1.73 m2]) | 100.82±11.81 | 87.36±14.11 | <0.001* | ||
| LVEF (%) | 63.52±6.54 | 63.27±6.78 | 0.229 | ||
| Angiographic and procedural characteristics | |||||
| LM or 3-vessel disease, n (%) | 60 (3.9) | 124 (4.1) | 0.715 | ||
| Complex lesion (lesion of type B2 or C), n (%) | 1,158 (74.3) | 2,291 (75.3) | 0.488 | ||
| Bifurcation disease, n (%) | 308 (19.8) | 582 (19.1) | 0.598 | ||
| Occlusion disease, n (%) | 323 (20.7) | 524 (17.2) | 0.004* | ||
| Syntax score | 11.11±7.42 | 11.97±7.89 | <0.001* | ||
| Number of target lesion | 1.41±0.68 | 1.41±0.65 | 0.632 | ||
| Number of stents per patient | 1.78±1.11 | 1.83±1.05 | 0.127 | ||
| Antiplatelet therapy duration | |||||
| Aspirin duration >1 year, n (%) | 1,533 (98.4) | 2,965 (97.1) | 0.008* | ||
| Clopidogrel duration >1 year, n (%) | 1,502 (96.4) | 2,921 (96.0) | 0.459 | ||
| Dual antiplatelet therapy >1 year, n (%) | 1,067 (68.5) | 2,016 (66.2) | 0.123 | ||
| ACS type, n (%) | |||||
| STEMI | 436 (28.0) | 637 (20.9) | <0.001* | ||
| NSTEMI | 128 (8.2) | 241 (7.9) | 0.502 | ||
| UA | 994 (63.8) | 2,166 (71.2) | <0.001* | ||
*P<0.05; BMI: body mass index; CAD: coronary artery disease; PCI: percutaneous coronary intervention; HGB: hemoglobin; PLT: platele; HbAlc: glycosylated hemoglobin; TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; eGFR: estimated glomerular filtration rate; LVEF: left ventricular ejection fraction; LM: left main artery; ACS: acute coronary syndrome; STEMI: ST-segment elevation myocardial infarction; NSTEMI: non-ST segment elevation myocardial infarction; UA: unstable angina.
Association between metabolic syndrome and early-onset ACS
Compared with the late-onset ACS group, the proportions of patients with obesity, hypertriglyceridemia, and low HDL-C were significantly higher, while the proportions of patients with hypertension (66.2% vs. 71.2%, P<0.001) and diabetes mellitus (25.1% vs. 28.4%, P=0.016) were lower in the early-onset ACS group. The percentage of patients who met more than three metabolic syndrome criteria was significantly higher in the early-onset ACS group compared with the late-onset ACS group (46.1% vs. 35.7%, P<0.001). Multivariate logistic regression revealed obesity, hypertriglyceridemia, and low HDL-C as independent risk factors for early-onset ACS (Table 2).
Table 2 Logistic regression analysis of metabolic syndrome components for early-onset ACS
| Parameters | OR | 95% CI | P-value |
|---|---|---|---|
| Female | 1.470 | 1.219-1.774 | <0.001* |
| Obesity (body mass index ≥28 kg/m2) | 1.590 | 1.345-1.881 | <0.001* |
| Hypertension | 0.697 | 0.596-0.817 | <0.001* |
| Diabetes mellitus | 0.808 | 0.683-0.955 | 0.012* |
| Hypertriglyceridemia (triglyceride ≥1.7 mmol/L) | 1.403 | 1.185-1.660 | <0.001* |
| Low HDL-C (HDL-C <1.04 mmol/L) | 1.464 | 1.231-1.742 | <0.001* |
| Family history of coronary artery disease | 1.247 | 1.078-1.443 | 0.003* |
| Smoking | 1.097 | 0.940-1.282 | 0.240 |
| Total cholesterol | 1.089 | 0.907-1.308 | 0.361 |
| LDL-C | 1.004 | 0.820-1.229 | 0.971 |
| Uric acid | 1.002 | 1.000-1.002 | 0.002* |
| Three to five metabolic syndrome components | 1.902 | 0.863-1.381 | 0.465 |
*P<0.05; OR: odds ratio; CI: confidence interval; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol.
Long-term outcomes of early-onset ACS and effects of metabolic syndrome
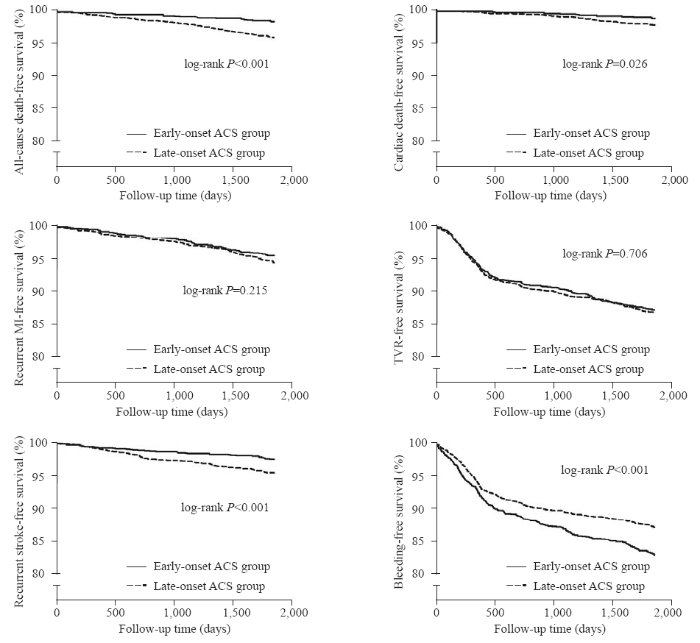
The clinical outcomes showed that the incidence of MACCEs was not significantly different between the two groups during the in-hospital follow-up. After the five-year follow-up, the incidences of all-cause death, cardiac death, and recurrent stroke were lower in the early-onset ACS group, while the incidence of bleeding events was higher in the early-onset ACS group (Table 3), compared with the late-onset ACS group. Kaplan-Meier estimates showed the same trend (Figure 1).
Table 3 Clinical outcomes in patients with early-onset ACS and late-onset ACS during five-year follow-up, n (%)
| Parameters | Hospitalization events | Five-year follow-up events | ||||
|---|---|---|---|---|---|---|
| Early-onset ACS (n=1,558) | Late-onset ACS (n=3,044) | P-value | Early-onset ACS (n=1,558) | Late-onset ACS (n=3,044) | P-value | |
| MACCEs | 18 (1.2) | 51 (1.7) | 0.169 | 262 (16.8) | 662 (21.7) | <0.001* |
| All-cause death | 2 (0.1) | 6 (0.2) | 0.596 | 24 (1.5) | 117 (3.8) | <0.001* |
| Cardiac death | 2 (0.1) | 5 (0.2) | 0.768 | 17 (1.1) | 61 (2.0) | 0.023* |
| Recurrent myocardial infarction | 17 (1.1) | 45 (1.5) | 0.281 | 81 (5.2) | 191 (6.3) | 0.143 |
| Stent thrombosis | 3 (0.2) | 8 (0.3) | 0.644 | - | - | - |
| Target vessel revascularization | - | - | - | 195 (12.5) | 392 (12.9) | 0.728 |
| Recurrent stroke | 0 (0) | 0 (0) | 1.000 | 34 (2.2) | 127 (4.2) | 0.001* |
| Bleeding (BARC 2 to 5) | 1 (0.1) | 3 (0.1) | 0.708 | 255 (16.4) | 377 (12.4) | <0.001* |
*P<0.05; ACS: acute coronary syndrome; MACCEs: major adverse cardiovascular and cerebrovascular events; BARC: Bleeding Academic Research Consortium grade.
Figure 1.
Figure 1.
Kaplan-Meier survival analysis. MI: myocardial infarction; TVR: target vessel revascularization.
In a subgroup analysis of early-onset ACS, the incidences of MACCEs (20.1% vs. 14.0%, respectively, P=0.002), recurrent MI (6.5% vs. 4.0%, P=0.027), and TVR (14.9% vs. 10.8%, P=0.008) in patients with metabolic syndrome were higher compared with patients without metabolic syndrome. Other ischemic and bleeding events were not significantly different between the two subgroups.
DISCUSSION
Metabolic syndrome is becoming increasingly common with changes in lifestyle. Metabolic syndrome can be easily identified in the clinic; however, the effect of metabolic syndrome on onset age and long-term prognosis of patients with ACS has not been investigated. The major findings of this study are as follows: (1) approximately one-third of patients with ACS had early-onset ACS and were more likely to demonstrate ST-segment elevation MI, and the overall prognosis of patients with early-onset ACS was better than that of patients with late-onset ACS; (2) obesity, hypertriglyceridemia, and low HDL-C were independent risk factors for early-onset ACS; and (3) metabolic syndrome was related to an increase in MACCEs in patients with early-onset ACS, especially recurrent MI and TVR.
Overall condition of patients with early-onset ACS
The atherosclerotic plaques of younger patients are rich in foam cells, which reduce plaque stability and induce early-onset ACS.[11] However, as there is no standardized age to delineate early-onset ACS at present, the incidence of early-onset ACS differs between epidemiological surveys.[12,13,14] In the present study, 33.9% of patients with ACS without previous CAD after PCI met the age diagnostic criteria for early-onset ACS; thus, more than one-third of young and middle-aged patients who experienced acute coronary events were treated with PCI. In this study, patients with early-onset ACS more frequently presented with ST-segment elevation MI, while patients with late-onset ACS more frequently presented with unstable angina. This suggests that plaque stability in patients with early-onset ACS may be worse, and coronary artery reserve or ischemic pre-adaptation may be lower, when compared with patients with late-onset ACS, which may induce transmutable MI.
With the widespread use of PCI for the treatment of ACS, patients with early-onset ACS demonstrate excellent immediate and long-term survival outcomes.[15] A small-sample study examining the prognosis of patients with early-onset ACS showed that the mortality of early-onset ACS was similar to ACS in older patients, but another study showed better outcomes in younger patients.[6] Thus, there is still controversy about the clinical prognosis of patients with early-onset ACS. In the current study, the incidence of inhospitable MACCEs was not significantly different between the early- and late-onset ACS groups, but long-term outcomes, including all-cause death, cardiac death, and recurrent stroke, were less frequently observed in the early-onset ACS group. During the five-year follow-up, the mortality rate of patients with early-onset ACS was 1.5% (3.8% in patients with late-onset ACS), which indicated that the long-term follow-up of ischemic events in patients with early-onset ACS did not increase. However, the incidence of bleeding events in patients with early-onset ACS was higher compared with patients with late-onset ACS, which may be related to the longer duration of antiplatelet therapy.
Relationship between metabolic syndrome and ACS onset age
Traditional risk factors, such as hypertension, diabetes mellitus, dyslipidemia, smoking, and family history of CAD, are associated with early-onset ACS.[16] In the current study, we found that patients with early-onset ACS had a higher BMI, higher TG, and total cholesterol concentrations. Logistic regression revealed metabolic syndrome components, including obesity, hypertriglyceridemia, and low HDL-C, as independent risk factors for early-onset ACS. These findings indicate that the metabolic abnormality caused by metabolic syndrome is related to the occurrence and development of early-onset ACS, which could be controlled by primary and secondary CAD preventions and would reduce the incidence of early-onset ACS.
Effects of metabolic syndrome on a long-term prognosis in patients with early-onset ACS
Patients with early-onset ACS with metabolic syndrome had a higher incidence of MACCEs compared with patients with late-onset ACS after five years of follow-up. Metabolic syndrome was associated with an increased risk of adverse cardiovascular events in patients with early-onset ACS.[17,18] This result emphasized that patients with early-onset ACS and metabolic syndrome should be encouraged to achieve more strict weight control and should receive standard drug treatments to rectify abnormalities in blood lipids, blood glucose, and blood pressure to reduce the long-term incidence of adverse cardiovascular events.
Other factors associated with early-onset ACS
A family history of CAD and hyperuricemia were positively correlated with early-onset ACS in this study. Previous studies showed that a family history of CAD and hyperuricemia are related to CAD,[16] and hyperuricemia could independently confer a higher risk of mortality in patients with AMI. This may be due to coronary artery injury caused by uric acid and the local inflammatory response. Hyperuricemia can also accelerate atherosclerosis by promoting LDL oxidation and inducing vascular endothelial dysfunction, which may lead to early-onset ACS.
Potential clinical implications
The current study showed a definite correlation between metabolic syndrome and early-onset ACS, and identified the effect of metabolic syndrome on adverse prognosis. Although the overall prognosis of patients with early-onset ACS is better compared with patients with late-onset ACS, we should pay more attention to metabolic syndrome in young patients and offer appropriate intervention in clinical practice. This could delay ACS occurrence and improve prognosis, especially in developing countries.
Limitations
Several limitations should be considered. First, our data were obtained from a single clinical center. Second, the criteria of age for the diagnosis of premature CAD should be verified; however, at the time of the study, a reference standard was lacking. Third, this was an observational study with a non-randomized design, and unmeasured confounders may have precluded definitive conclusions.
CONCLUSIONS
Metabolic syndrome components, including obesity, hypertriglyceridemia, and low HDL-C, are independent risk factors for early-onset ACS and relate to an increase in recurrent MI and revascularization. An effective control of metabolic syndrome may reduce the incidence of early-onset ACS and improve the long-term prognosis.
Funding: The study was supported by the National Key Research and Development Program of China (2016YFC130130 [Subtopic: 2016YFC1301301]).
Ethical approval: The study was approved by the Ethics Committee of Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China (ethical application number: IRB2012-BG-006; approval number: 2013-449).
Conflicts of interest: All authors declared no conflicts of interest.
Contributors: BX and YZ contributed equally to this work. All authors revised and approved the final version of the manuscript.
Reference
Premature coronary heart disease and traditional risk factors — can we do better?
URL
PMID:24757620
[Cited within: 1]

BACKGROUND: Traditional cardiovascular risk factors are strong predictors of an increased likelihood for premature CHD. Considering the benefits of risk factors management, it is imperative to find and treat them before looking for more unknown and weak risk factors. OBJECTIVES: Limited information is available about the demographic and historical characteristics of the patients with premature Coronary Heart Disease (CHD) in IR Iran. The main objective of this study was to determine the prevalence of the traditional risk factors in these patients. Also, the researchers hypothesized that there are insufficient risk assessment and preventive intervention methods for the asymptomatic adult population. METHODS: This study was conducted on 125 patients with premature CHD (age<50 years) who were admitted in two academic hospitals with acute coronary syndromes. The patients were accepted since they had a definite CHD on the basis of acute myocardial infarction (elevated cardiac enzymes) or documented CAD in coronary angiography. RESULTS: The mean age of the study population was 42.50+/-5.65 (26 to 49 years). Among the patients,92 (73.6%) were male, 113 (90.4%) were married, 58 (46.4%) were smokers,19 (15.2%) were opium users, 97 (77.6%) had dyslipidemia, 44 (35.2%) had hypertension, and 33 (26.4%) had diabetes mellitus. In addition, family history was presented in 54 patients (43.2%). Among the study population, 120 patients (96%) had at least one of the traditional risk factors, including dyslipidemia, hypertension, diabetes mellitus, cigarette smoking, and family history of CHD. However, none of the dyslipidemic patients had controlled total cholesterol, LDL, HDL, and triglyceride. Also, none of the diabetic patients had hemoglobin A1C<7%. Among the 44 hypertensive patients, blood pressure of 15 ones (34%) was within the normal range. Besides, only 3 patients (2.4%) had regular physical activity (at least 30 minutes, three times a week). CONCLUSIONS: Premature Coronary Heart Disease is a public health problem. However, there is lack of effective and intensive treatments of well-defined traditional risk factors and prevention methods for the majority of the patients experiencing premature CHD. In sum, there is still plenty of room for improvement of risk management in IR Iran.
A programme of lifestyle intervention in families for cardiovascular risk reduction (PROLIFIC study): design and rationale of a family based randomized controlled trial in individuals with family history of premature coronary heart disease
DOI:10.1186/s12889-016-3928-6
URL
PMID:28056897
[Cited within: 1]

BACKGROUND: Recognizing patterns of coronary heart disease (CHD) risk in families helps to identify and target individuals who may have the most to gain from preventive interventions. The overall goal of the study is to test the effectiveness and sustainability of an integrated care model for managing cardiovascular risk in high risk families. The proposed care model targets the structural and environmental conditions that predispose high risk families to development of CHD through the following interventions: 1) screening for cardiovascular risk factors, 2) providing lifestyle interventions 3) providing a framework for linkage to appropriate primary health care facility, and 4) active follow-up of intervention adherence. METHODS: Initially, a formative qualitative research component will gather information on understanding of diseases, barriers to care, specific components of the intervention package and feedback on the intervention. Then a cluster randomized controlled trial involving 740 families comprising 1480 participants will be conducted to determine whether the package of interventions (integrated care model) is effective in reducing or preventing the progression of CHD risk factors and risk factor clustering in families. The sustainability and scalability of this intervention will be assessed through economic (cost-effectiveness analyses) and qualitative evaluation (process outcomes) to estimate value and acceptability. Scalability is informed by cost-effectiveness and acceptability of the integrated cardiovascular risk reduction approach. DISCUSSION: Knowledge generated from this trial has the potential to significantly affect new programmatic policy and clinical guidelines that will lead to improvements in cardiovascular health in India. TRIAL REGISTRATION NUMBER: NCT02771873, registered in May 2016 ( https://clinicaltrials.gov/ct2/show/results/NCT02771873 ).
The relative value of metabolic syndrome and cardiovascular risk score estimates in premature acute coronary syndromes
DOI:10.1016/j.ahj.2007.10.038
URL
PMID:18294493
[Cited within: 1]

BACKGROUND: To compare the relative value of metabolic syndrome (MetS) and cardiovascular risk score estimates in patients with acute coronary syndromes (ACS) aged <45 years. PATIENTS AND METHODS: Two hundred consecutive patients (183 men, mean age 40.8 +/- 3.5 years) presented with a first-ever ACS, and 200 age-and sex-matched controls were evaluated. Metabolic syndrome diagnostic criteria, European Risk SCORE estimation function, and the Framingham Risk Score (FRS) were assessed in all participants. RESULTS: The prevalence of the MetS was significantly higher in the patients' group compared with the control group (51.5% vs 26.0%, P < .001). No subjects with a SCORE >1.0% were identified. The mean 10-year FRS for patients and controls was 13.03% +/- 7.96% and 10.02 +/- 8.10%, respectively (P < .001), whereas only 22.5% of ACS patients had a 10-year risk >20.0% compared with 14.5% of controls (P = .04). After controlling for potential confounders, MetS was associated with 1.93 (95% CI 1.13-3.28, P = .01) higher odds of having an ACS. Moreover, the odds had a positive association with the increasing cumulative number of MetS components. Crude and adjusted ORs for the FRS were 1.05 (95% CI 1.029-1.08, P = .001) and 0.98 (95% CI 0.92-1.05, P = NS), respectively. CONCLUSION: Metabolic syndrome is highly associated with ACS in subjects <45 years of age and seems to be more valuable than established cardiovascular risk calculators.
Risk factors for acute coronary syndrome in patients below the age of 40 years
DOI:10.1016/j.ehj.2018.05.005
URL
PMID:30591735
[Cited within: 1]

Background: Acute coronary syndrome (ACS) refers to a spectrum of symptoms compatible with acute myocardial ischemia. Plasma markers of inflammation have been recently identified as diagnostic aid and risk predictors. The present study, conducted in Slemani Cardiac Hospital (SCH), Sulaimaniyah, Iraq aimed to recognize some risk factors for ACS in Iraqi adults younger than 40. Methodology: This is a prospective case-control study of 100 patients with ACS vs. a control group of 100 healthy volunteers. The study began at 1st January 2014 and ended at 31st December 2016. All patients were subjected to full history taking, clinical examination including measurement of waist circumference and body mass index (BMI). Investigations included electrocardiography (ECG), echocardiography, full blood count, measurement of lipid profile and C-reactive protein (CRP). The patients were managed by percutaneous coronary intervention (PCI). Results: The mean age of the patients was 36years (range 28-40). Eighty-five% of patients were male. The mean BMI (29kg/m(2)) and waist circumference (98cm) of the patients were higher than the controls (24kg/m(2) and 72cm respectively). The leukocytes, lymphocytes and neutrophil counts as well as CRP in both groups were within the normal range. The most prevalent risk factor was obesity (n=86). Other risk factors were smoking (n=62), hypertension (n=26), diabetes mellitus (n=22) and positive family history of ACS (n=24). Most patients (n=83) had multi-vessel coronary artery disease (2-3 vessels). Conclusion: ACS in young adults is an increasing health problem. Obesity was found to be the most prevalent risk factor.
Long-term outcome and risk assessment in premature acute myocardial infarction: a 10-year follow-up study
DOI:10.1016/j.ijcard.2017.03.146
URL
PMID:28395980
[Cited within: 1]

BACKGROUND: Premature acute myocardial infarction (AMI) is a rare disease carrying significant morbidity and mortality. Existing data on outcome in these patients is based on retrospective analysis of angiographic reports or refer to time periods with incomparable treatment regimes, making them unusable for risk assessment in times of widespread use of reperfusion therapy. Aim of this study was to assess the outcome of premature AMI in a prospectively recruited study population enrolled in the times of modern reperfusion therapy. METHODS: We included 102 consecutive AMI survivors (
Acute myocardial infarction in young adults: prognostic role of angiotensin — converting enzyme, angiotensin II type I receptor, apolipoprotein E, endothelial constitutive nitric oxide synthase, and glycoprotein IIIa genetic polymorphisms at medium-term follow-up
DOI:10.1067/mhj.2000.106165
URL
PMID:10827377
[Cited within: 2]

BACKGROUND: A number of reports have investigated the association between various gene polymorphisms and the phenotypic expression of myocardial infarction. No investigations have evaluated the prognostic role of genetic factors in young people with premature coronary disease. The aim of this study was to investigate the influence of genetic factors compared with that of conventional risk factors on follow-up events in a population of Italian young adults with myocardial infarction. METHODS AND RESULTS: The study population consisted of 106 young patients (mean age 40 +/- 4 years, range 23 to 45 years) with diagnosis of acute myocardial infarction. Clinical and genetic data from the group of patients with events during follow-up were compared with those from patients without events. The following genetic polymorphisms were tested: angiotensin I converting enzyme, angiotensin II type I receptor, apolipoprotein E (ApoE), endothelial constitutive nitric oxide synthase, and platelet glycoprotein IIIa. Coronary angiography was performed in 94 patients. Coronary angiography showed coronary artery disease in 93% of patients. During follow-up (46 +/- 12 months, range 25 to 72) the overall combined end points (cardiac death, myocardial infarction, and revascularization procedures) accounted for 21 events. Family history of coronary artery disease, smoking, stenosis of the left anterior descending artery at coronary angiography, and ApoE polymorphism (presence of epsilon4 allele) were significantly more prevalent (univariate analysis) in the group of patients with events. Logistic multivariate analysis showed that ApoE polymorphism (P =. 004, odds ratio [OR] 6.8, 95% confidence interval [CI] 2 to 22), family history (P =.005, OR 8.3, 95% CI 2 to 35), smoking after acute myocardial infarction (P =.008, OR 10.9, 95% CI 2 to 62), and left anterior descending coronary artery disease (P =.02. OR 6.6, 95% CI 1.3 to 33) were independent predictors of adverse events. CONCLUSIONS: Myocardial infarction at a young age is commonly characterized by evidence of multiple cardiovascular risk factors and by a favorable prognosis in short- and medium-term follow-up. Evidence of significant disease at coronary angiography suggests the presence of a premature atherosclerotic process. ApoE polymorphism (presence of epsilon4 allele) appears to be a strong independent predictor of adverse events, suggesting a remarkable influence in the accelerated coronary disease.
Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction
DOI:10.1038/nature13917
URL
PMID:25487149
[Cited within: 1]

Myocardial infarction (MI), a leading cause of death around the world, displays a complex pattern of inheritance. When MI occurs early in life, genetic inheritance is a major component to risk. Previously, rare mutations in low-density lipoprotein (LDL) genes have been shown to contribute to MI risk in individual families, whereas common variants at more than 45 loci have been associated with MI risk in the population. Here we evaluate how rare mutations contribute to early-onset MI risk in the population. We sequenced the protein-coding regions of 9,793 genomes from patients with MI at an early age ( 190 mg dl(-1). At apolipoprotein A-V (APOA5), carriers of rare non-synonymous mutations were at 2.2-fold increased risk for MI. When compared with non-carriers, LDLR mutation carriers had higher plasma LDL cholesterol, whereas APOA5 mutation carriers had higher plasma triglycerides. Recent evidence has connected MI risk with coding-sequence mutations at two genes functionally related to APOA5, namely lipoprotein lipase and apolipoprotein C-III (refs 18, 19). Combined, these observations suggest that, as well as LDL cholesterol, disordered metabolism of triglyceride-rich lipoproteins contributes to MI risk.
Third universal definition of myocardial infarction
URL PMID:25689940 [Cited within: 1]
Clinical end points in coronary stent trials: a case for standardized definitions
DOI:10.1161/CIRCULATIONAHA.106.685313
URL
PMID:17470709
[Cited within: 2]

BACKGROUND: Although most clinical trials of coronary stents have measured nominally identical safety and effectiveness end points, differences in definitions and timing of assessment have created confusion in interpretation. METHODS AND RESULTS: The Academic Research Consortium is an informal collaboration between academic research organizations in the United States and Europe. Two meetings, in Washington, DC, in January 2006 and in Dublin, Ireland, in June 2006, sponsored by the Academic Research Consortium and including representatives of the US Food and Drug Administration and all device manufacturers who were working with the Food and Drug Administration on drug-eluting stent clinical trial programs, were focused on consensus end point definitions for drug-eluting stent evaluations. The effort was pursued with the objective to establish consistency among end point definitions and provide consensus recommendations. On the basis of considerations from historical legacy to key pathophysiological mechanisms and relevance to clinical interpretability, criteria for assessment of death, myocardial infarction, repeat revascularization, and stent thrombosis were developed. The broadly based consensus end point definitions in this document may be usefully applied or recognized for regulatory and clinical trial purposes. CONCLUSION: Although consensus criteria will inevitably include certain arbitrary features, consensus criteria for clinical end points provide consistency across studies that can facilitate the evaluation of safety and effectiveness of these devices.
Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding academic research consortium
URL PMID:21670242 [Cited within: 1]
NMR-based lipidomic analysis of blood lipoproteins differentiates the progression of coronary heart disease
DOI:10.1021/pr500061n
URL
PMID:24689886
[Cited within: 1]

Abnormal lipid composition and metabolism of plasma lipoproteins play a crucial role in the pathogenesis of coronary heart disease (CHD). A (1)H NMR-based lipidomic approach was used to investigate the correlation of coronary artery stenosis with the atherogenic (non-HDL) and atheroprotective (HDL) lipid profiles in 99 patients with CHD of various stages of disease and compared with 60 patients with normal coronary arteries (NCA), all documented in coronary angiography. The pattern recognition models created from lipid profiles predicted the presence of CHD with a sensitivity of 87% and a specificity of 88% in the HDL model and with 90% and 89% in the non-HDL model, respectively. Patients with mild, moderate, and severe coronary artery stenosis were progressively differentiated from those with NCA in the non-HDL model with a statistically significant separation of severe stage from both mild and moderate. In the HDL model, the progressive differentiation of the disease stages was statistically significant only between patients with mild and severe coronary artery stenosis. The lipid constituents of lipoproteins that mainly characterized the initial stages and then the progression of the disease were the high levels of saturated fatty acids in lipids in both HDL and non-HDL particles, the low levels of HDL-phosphatidylcholine, HDL-sphingomyelin, and omega-3 fatty acids and linoleic acid in lipids in non-HDL particles. The conventional lipid marker, total cholesterol, found in low levels in HDL and in high levels in non-HDL, also contributed to the onset of the disease but with a much lower coefficient of significance. (1)H NMR-based lipidomic analysis of atherogenic and atheroprotective lipoproteins could contribute to the early evaluation of the onset of coronary artery disease and possibly to the establishment of an appropriate therapeutic option.
Prevalence of coronary heart disease — United States, 2006-2010
URL
PMID:21993341
[Cited within: 1]

Age-adjusted mortality rates for coronary heart disease (CHD) have declined steadily in the United States since the 1960s. Multiple factors likely have contributed to this decline in CHD deaths, including greater control of risk factors, resulting in declining incidence of CHD, and improved treatment. Greater control of risk factors and declining incidence can reduce CHD prevalence, whereas improved treatment that results in lower mortality rates and more persons living with CHD can increase prevalence. To estimate state-specific CHD prevalence and recent trends by age, sex, race/ethnicity, and education, CDC analyzed data from Behavioral Risk Factor Surveillance System (BRFSS) surveys for the period 2006-2010. This report summarizes the results of that analysis, which determined that, although self-reported CHD prevalence declined overall, substantial differences in prevalence existed by age, sex, race/ethnicity, education, and state of residence. These data can enable state and national health agencies to monitor CHD prevalence as a measure of progress toward meeting the Healthy People 2020 objective to reduce the U.S. rate of CHD deaths 20% from the 2007 baseline.
Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study
DOI:10.1016/S0140-6736(04)17018-9
URL
PMID:15364185
[Cited within: 1]

BACKGROUND: Although more than 80% of the global burden of cardiovascular disease occurs in low-income and middle-income countries, knowledge of the importance of risk factors is largely derived from developed countries. Therefore, the effect of such factors on risk of coronary heart disease in most regions of the world is unknown. METHODS: We established a standardised case-control study of acute myocardial infarction in 52 countries, representing every inhabited continent. 15152 cases and 14820 controls were enrolled. The relation of smoking, history of hypertension or diabetes, waist/hip ratio, dietary patterns, physical activity, consumption of alcohol, blood apolipoproteins (Apo), and psychosocial factors to myocardial infarction are reported here. Odds ratios and their 99% CIs for the association of risk factors to myocardial infarction and their population attributable risks (PAR) were calculated. FINDINGS: Smoking (odds ratio 2.87 for current vs never, PAR 35.7% for current and former vs never), raised ApoB/ApoA1 ratio (3.25 for top vs lowest quintile, PAR 49.2% for top four quintiles vs lowest quintile), history of hypertension (1.91, PAR 17.9%), diabetes (2.37, PAR 9.9%), abdominal obesity (1.12 for top vs lowest tertile and 1.62 for middle vs lowest tertile, PAR 20.1% for top two tertiles vs lowest tertile), psychosocial factors (2.67, PAR 32.5%), daily consumption of fruits and vegetables (0.70, PAR 13.7% for lack of daily consumption), regular alcohol consumption (0.91, PAR 6.7%), and regular physical activity (0.86, PAR 12.2%), were all significantly related to acute myocardial infarction (p<0.0001 for all risk factors and p=0.03 for alcohol). These associations were noted in men and women, old and young, and in all regions of the world. Collectively, these nine risk factors accounted for 90% of the PAR in men and 94% in women. INTERPRETATION: Abnormal lipids, smoking, hypertension, diabetes, abdominal obesity, psychosocial factors, consumption of fruits, vegetables, and alcohol, and regular physical activity account for most of the risk of myocardial infarction worldwide in both sexes and at all ages in all regions. This finding suggests that approaches to prevention can be based on similar principles worldwide and have the potential to prevent most premature cases of myocardial infarction.
Investigations for the assessment of adult patients presenting to the emergency department with supraventricular tachycardia
URL PMID:31893004 [Cited within: 1]
Clinical profile and impact of family history of premature coronary artery disease on clinical outcomes of patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction: analysis from the HORIZONS-AMI trial
DOI:10.1016/j.carrev.2014.09.002
URL
PMID:25288517
[Cited within: 1]

BACKGROUND/PURPOSE: Family history of coronary artery disease (CAD) is a well-established risk factor of future cardiovascular events. The authors sought to examine the relationship between family history of CAD and clinical profile and prognosis of patients with ST-elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PCI). MATERIALS/METHODS: Baseline features and clinical outcomes at 30 days and at 3 years from 3601 patients with STEMI enrolled in the HORIZONS-AMI trial were compared in patients with and without family history of premature CAD, which was present in 1059 patients (29.4%). RESULTS: These patients were younger (median 56.7 vs. 62.1years, P<0.0001) and more often current smokers (52.4% vs. 43.5%, P<0.0001), had more dyslipidemia (47.7% vs. 41.1%, P=0.0003), less diabetes mellitus (14.1% vs. 17.5%, P=0.01) and had shorter symptom onset to balloon times (median 213 vs. 225 min, P=0.02). Patients with a family history of premature CAD had higher rates of final TIMI 3 flow (93.8% vs. 90.6%, P=0.002), and myocardial blush grade 2 or 3 (83.2% vs. 78.0% P=0.0008), and fewer procedural complications. Although the unadjusted 30-day and 3-year mortality rates were lower in patients with a family history of premature CAD (1.8% vs. 3.0%, P=0.046 and 4.8% vs. 7.7%, P=0.002, respectively), by multivariable analysis the presence of a family history of premature CAD was not an independent predictor of death at 3 years (HR [95%CI]=1.00 [0.70, 1.44], P=0.98). CONCLUSIONS: A family history of premature CAD is not an independent predictor of higher mortality.
Newer perspectives of coronary artery disease in young
URL PMID:28070240 [Cited within: 2]
NCEP defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older
URL PMID:12716754 [Cited within: 1]
Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study
URL PMID:12860911 [Cited within: 1]