INTRODUCTION
Sepsis is a life-threatening, multiple-organ dysfunction condition caused by an infection that induces immune dysfunction in the host.[1] It is an important medical and health problem that yearly affects thousands of patients worldwide. Sepsis-associated encephalopathy (SAE) is a common complication of sepsis. SAE refers to diffuse brain dysfunction. The incidence of SAE is 8%-70%, and it is also one of the most common brain disorders in the intensive care unit.[2,3] So far, there are no clear diagnostic criteria for SAE. SAE diagnosis excludes direct infection of the central nervous system, head trauma, fat embolism, adverse drug reactions, other factors that affect consciousness, and diffuse cerebral dysfunction caused by the systemic inflammatory response.[4,5] A multicenter study found that 307 (23.0%) of 1,333 patients with severe sepsis had severely altered mental states.[2] However, sensitive diagnostic tools, such as electrophysiological tests for brain function, revealed that almost all sepsis patients possessed mental abnormalities.[6-8] Brain dysfunction is often overlooked because sepsis patients are not diagnosed with SAE during hospitalization.
SAE is a disorder with complex and unclear pathogenesis.[9] Cerebral microcirculation is one important pathophysiological symptom of SAE.[10] In sepsis patients with impaired brain autoregulation, the cerebral vessel responses to carbon dioxide concentration and extracellular pH become slow.[11] When systemic blood pressure drops sharply, inadequate cerebral perfusion will likely occur, leading to neurological dysfunction. Dysfunction of brain autoregulation leads to an inability to respond to changes in mean arterial pressure.[6,10,12,13] Related studies have shown that neuronal damage after cerebral ischemia is region-selective, and the vulnerabilities of neurons in sensitive areas are also different.[14] The hippocampus and neocortex are prone to damage after cerebral ischemia. Neurons in the CA1 area of the hippocampus are especially sensitive to transient ischemia, whereas apoptosis in the CA3 area is known as selective vulnerability. Sepsis patients have a higher risk of non-Alzheimer’s dementia compared with the general population.[15,16] At present, most clinical diagnoses of SAE are based only on clinical manifestations without electrophysiological or biochemical tests. As a result, many sepsis patients with hidden neurological dysfunction do not undergo comprehensive neuropsychological tests because they do not have significant psychiatric disorders in hospitals. The nervous system function in such patients is not clear; thus, most sepsis patients don’t receive corresponding rehabilitation treatment.
This study aimed to investigate whether sepsis causes loss of brain volume and cognitive function. We used magnetic resonance imaging (MRI) scans to evaluate the nervous system integrity of sepsis patients and healthy controls. We focused on the hippocampus, thalamus, caudate, putamen, pallidum, amygdala, and ventral diencephalon because these areas are considered as the most appropriate regions for analysis throughout the brain. The CA1 area of the hippocampus was also analyzed because CA1 is particularly sensitive to ischemia and hypoxia.[14] Neuropsychological tests were used to assess the neurological function of patients. Particular emphasis was placed on the cognitive and executive functions, which are susceptible to be influenced by ischemia and hypoxia.[17]
METHODS
Study population
This study included 20 sepsis patients who were not diagnosed clinically with SAE but had abnormal electroencephalograms (EEGs). These patients were admitted to the emergency department of the Second Affiliated Hospital of Xi’an Jiaotong University from June 2015 to November 2018, and the clinical data were collected and analyzed.
The patients were diagnosed with sepsis, which was defined in accordance with the criteria.[1] All patients had no change of mental state during hospitalization, but their EEGs revealed abnormalities, including background abnormalities, changes in cycles and rhythms, and epileptiform activity. Background abnormality was characterized by slow background activity, including diffuse slow waves, persistent θ waves, and slow delta waves or burst suppression, with or without autonomous background variation. The periodic and rhythmic changes were manifested as three-phase waves, periodic epileptic rhythms, intermittent rhythmic δ activities in the frontal region, pseudoperiodic epileptic discharges on one side or epileptic discharges on both sides, and abnormal seizure periods. All sepsis patients completed Acute Physiology and Chronic Health Evaluation II (APACHE II)[18] scoring (score 0 to 71) on admission. After admission, patients received empirical anti-infection treatment. For patients with positive blood cultures in the later stage, the anti-infection regimen was adjusted according to the blood culture results. All patients with hemodynamic abnormalities received active fluid resuscitation, and crystalloid fluid was preferred. All patients underwent an MRI examination within one month after hospital discharge. The control group was composed of 20 healthy people (from the Physical Examination Center of the Second Affiliated Hospital of Xi’an Jiaotong University); their sex, age, education level, hypertension, coronary heart disease (CHD), diabetes mellitus (DM), and other basic information were matched with those of the sepsis group. All participants were required to have no previous history of neurological diseases so as not to affect the results of this study. All participants underwent neuropsychological tests within one month after enrolling in the study. Table 1 summarizes the basic demographic information and clinical characteristics of the two groups.
Table 1 Demographic and clinical characteristics of patients with sepsis and healthy controls
| Parameters | Sepsis patients (n=20) | Healthy people (n=20) | P-value |
|---|---|---|---|
| Sex (F:M) | 8:12 | 9:11 | 0.749 |
| Age (years) | 57.60±3.46 | 55.80±4.41 | 0.159 |
| Education (years) | 13.50±5.12 | 12.70±4.87 | 0.616 |
| LVEF | 0.52±0.27 | 0.58±0.32 | 0.525 |
| Hypertersion (Y:N) | 9:11 | 10:10 | 0.752 |
| DM (Y:N) | 12:8 | 10:10 | 0.525 |
| CHD (Y:N) | 4:16 | 5:15 | 0.705 |
| Smoking (Y:N) | 12:8 | 16:4 | 0.168 |
| NSAID use (Y:N) | 3:17 | 1:19 | 0.292 |
| APACHE II score | 11.85 | 0 | - |
LVEF: left ventricular ejection fraction; DM: diabetes mellitus; CHD: coronary heart disease; NSAID: nonsteroidal anti-inflammatory drug; APACHE II: Acute Physiology and Chronic Health Evaluation II; Y:N=Yes:No.
Neuropsychological assessments
Neuropsychological assessments were performed in all sepsis patients and healthy controls. All sepsis patients completed the test within one month after discharge, and participants in the control group completed the test within one month after joining the study. The assessments included the following cognitive functions: (1) general intelligence test using the Wechsler Adult Intelligence Scale-III (Chinese translation version);[19] (2) visual evaluation using the Hooper Visual Organization Test;[20] (3) memory function using the California Verbal Learning Test-II (CVLT-II);[21] (4) attention using the Stroop Test (ST);[22] (5) executive function using the Wisconsin Card Sorting Test;[23] (6) working memory using the Paced Auditory Serial Addition Test (PASAT 2 and 3);[24] and (7) changes in the familiarity and recognition functions in memory using the process dissociation procedure (PDP) test.[25]
Image acquisition
The MRI data were gathered from all 40 people. All images were acquired using a GE Signa HDxt 3.0T TX dual-gradient dual-RF source MRI scanner and a head orthogonal eight-channel phased-array coil. High-resolution axial 3D T1-weighted images of the entire brain were obtained using a 3D fast spoiled gradient-recalled sequence. The scanning parameters were as follows: time of repetition 8.0 ms; time of echo 3.1 ms; inversion time 400 ms; thickness 1 mm; flip angle 12°; matrix 240×240; number of excitation 1; and field of view 24 cm×18 cm. Moreover, 158 layers were scanned without interval.
Image analyses
FreeSurfer v6.0 (http://surfer.nmr.mgh.harvard.edu/) was used for image analysis. FreeSurfer is a powerful suite of tools that performs highly reliable and automated analysis of the human brain.[26] The analysis included volumetric segmentation of the brain structure and the segmentation of the hippocampus. FreeSurfer can accurately identify and segment cerebral cortex and subcortical structures in MRI imaging data and measure the changes of subpixel accuracy of cerebral cortex thickness with high sensitivity. FreeSurfer was used to segment the hippocampus and to obtain the volumes of different brain regions. The results of all scans and all automatic segmentation were visually examined to ensure proper skull dissection and correct segmentation.
Ethics statement
The Research Ethics Board of the Medical Center and Psychology Department of the Xi’an Jiaotong University approved this study.
RESULTS
Demographic information
There were no significant differences between the sepsis group and the healthy control group in general demographic data that included sex ratio, age, education level, hypertension, CHD, DM, tobacco use, and nonsteroidal anti-inflammatory drug (NSAID) use (Table 1).
Neuropsychological assessment
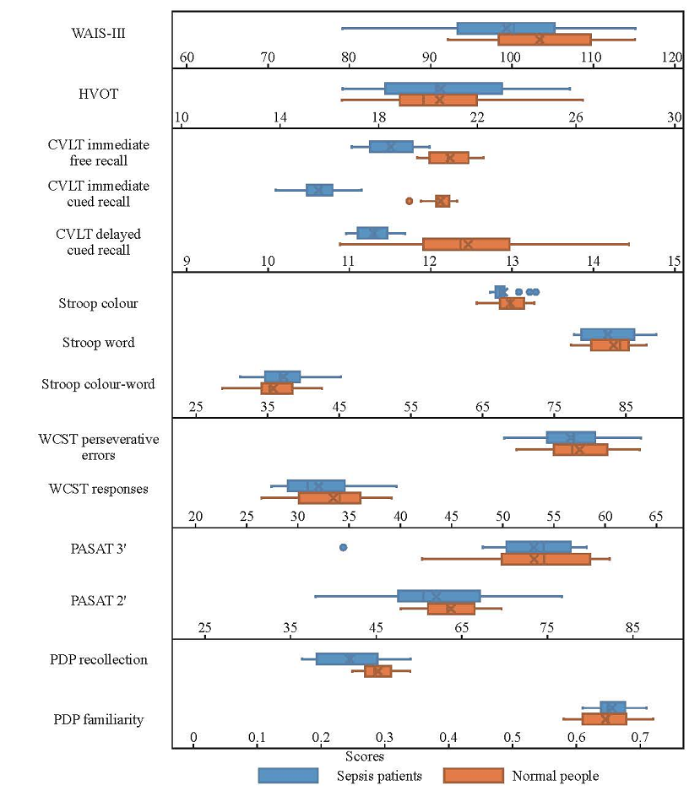
Figure 1 shows the results of clinical neuropsychological tests of different cognitive region functions. The results were tested by a normal distribution (Kolmogorov-Smirnov test). Data of the two groups were fitted to a normal distribution so that they could be compared using the t-test between two pairs of samples. According to the Wechsler Adult Intelligence Scale-III, no difference in the overall intelligence quotient (IQ) was found between the two groups (P>0.05), a condition that could be used as a background to explain other areas of performance. In addition, we didn’t find any significant differences in visual assessment, executive function, or attention tests between the two groups (P>0.05). Although the sepsis group showed a cognitive decline clinically, no significant difference was found compared with the healthy control group (P>0.05). The levels of immediate free recall, immediate cued recall, and delayed cued recall in the CVLT-II were significantly lower in sepsis patients (P<0.05). No significant difference in PASAT 2 or 3 was found between the two groups (P>0.05). The explicit memory (recollection process) of the PDP test was lower in the sepsis group compared with the control group, but no significant difference was found in the implicit memory familiarity.
Figure 1.
Figure 1.
Results of clinical neuropsychological tests of different cognitive region functions between the two groups. WAIS-III: Wechsler Adult Intelligence Scale-III; HVOT: Hooper Visual Organization Test; CVLT: California Verbal Learning Test; WCST: Wisconsin Card Sorting Test; PASAT: Paced Auditory Serial Addition Test; PDP: process dissociation procedure.
Structural neuroimaging
We used FreeSurfer v6.0 to automatically analyze and measure the volumes of different brain regions and hippocampal formation in the sepsis and control groups. The results indicated that the volumes of the left and right hippocampi in sepsis patients were significantly lower than those in the control group (P<0.05). Compared with the control group, the volume of the presubiculum in the hippocampus of sepsis patients decreased, and the difference was statistically significant (P<0.05). The volumes of CA1, CA3, CA4, molecular layer, granular dentate gyrus cell layer, and the hippo-amyg transitional area between the hippocampus and the amygdala were smaller in the sepsis group than in the healthy control group, but the differences were not statistically significant (P>0.05). There was no significant difference in subcortical volume between the two groups, including the thalamus, caudate, putamen, pallidum, amygdala, and ventral diencephalon (P>0.05), but we found that the subcortical volume in the sepsis group was smaller than that in the control group (Table 2).
Table 2 The volume of different brain regions (mm3)
| Parameters | Sepsis patients (n=20) | Healthy people (n=20) | P-value |
|---|---|---|---|
| Left hippocampal subfields | |||
| Whole hippocampus | 3,259.72±330.42 | 3,476.74±292.90 | 0.034 |
| Subiculum | 432.18±108.56 | 428.61±119.28 | 0.921 |
| CA1 | 605.17±98.76 | 629.19±91.67 | 0.430 |
| Presubiculum | 254.18±61.79 | 308.78±79.61 | 0.020 |
| Parasubiculum | 72.89±14.72 | 76.54±19.61 | 0.510 |
| CA3 | 241.65±58.67 | 274.63±62.31 | 0.093 |
| CA4 | 286.19±72.06 | 291.03±68.47 | 0.829 |
| Hippo-amyg transitional area | 65.23±31.76 | 67.21±24.89 | 0.827 |
| Molecular layer | 576.87±101.27 | 591.72±98.16 | 0.640 |
| Granule dentate gyrus cell layer | 309.72±65.43 | 321.58±71.86 | 0.588 |
| Right hippocampal subfields | |||
| Whole hippocampus | 3,090.40±347.39 | 3,367.58±301.87 | 0.010 |
| Subiculum | 418.76±108.53 | 461.72±107.65 | 0.216 |
| CA1 | 654.92±103.68 | 701.75±115.48 | 0.185 |
| Presubiculum | 308.72±95.46 | 392.87±86.78 | 0.005 |
| Parasubiculum | 61.65±31.76 | 67.82±29.74 | 0.530 |
| CA3 | 239.74±81.65 | 261.76±76.49 | 0.384 |
| CA4 | 254.82±107.83 | 286.65±132.74 | 0.410 |
| Hippo-amyg transitional area | 74.73±42.69 | 78.64±34.73 | 0.752 |
| Molecular layer | 599.78±98.67 | 621.76±107.64 | 0.505 |
| Granule dentate gyrus cell layer | 317.95±98.65 | 348.69±87.69 | 0.304 |
| Left subcortical segmentation | |||
| Thalamus | 7,243.76±498.57 | 6,935.64±512.87 | 0.061 |
| Caudate | 3,395.46±329.58 | 3,492.76±312.75 | 0.344 |
| Putamen | 5,349.82±806.63 | 5,437.65±798.67 | 0.731 |
| Pallidum | 1,498.47±419.54 | 1,529.03±452.93 | 0.826 |
| Amygdala | 1,743.67±489.73 | 1,728.44±521.64 | 0.925 |
| Ventral diencephalon | 3,598.43±112.54 | 3,655.64±101.65 | 0.100 |
| Right subcortical segmentation | |||
| Thalamus | 6,291.64±776.84 | 5,921.56±881.42 | 0.167 |
| Caudate | 3,154.87±89.76 | 3,345.26±92.65 | 0.089 |
| Putamen | 5,083.46±119.47 | 5,143.65±121.65 | 0.123 |
| Pallidum | 1,327.65±64.53 | 1,293.64±72.47 | 0.125 |
| Amygdala | 1,873.45±175.94 | 1,908.82±216.72 | 0.574 |
| Ventral diencephalon | 3,728.59±433.29 | 3,892.39±397.28 | 0.220 |
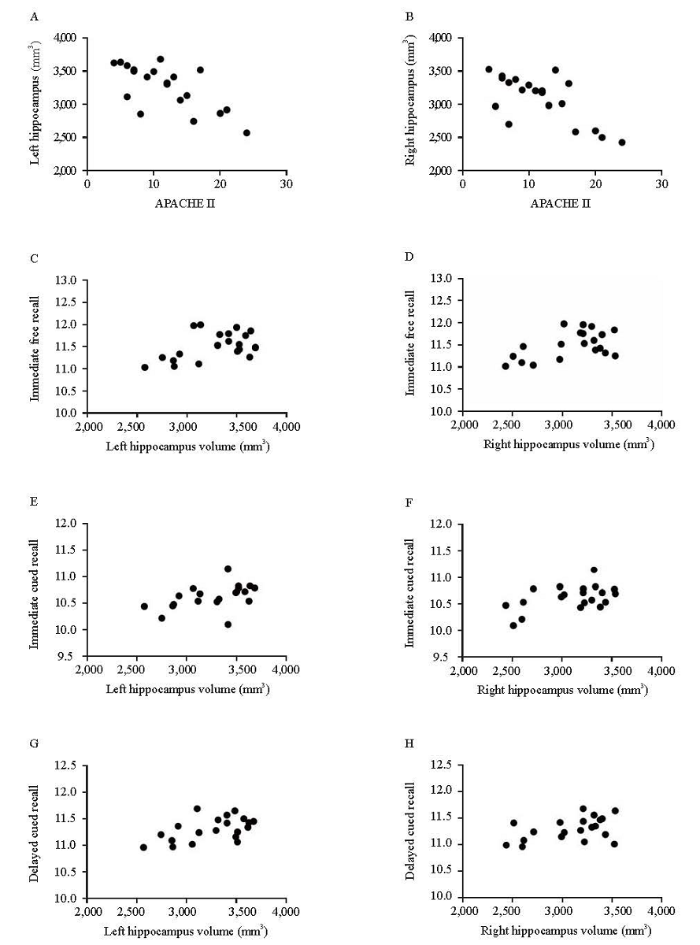
Correlations between hippocampal volumes and neuropsychological tests
The APACHE II score of the sepsis group was negatively correlated with the volumes of left and right hippocampi (Figure 2A, r= -0.690, P<0.05; Figure 2B, r= -0.694, P<0.05), and the volumes of left and right hippocampi were positively correlated with immediate free recall (Figure 2C, r=0.496, P<0.05; Figure 2D, r=0.526, P<0.05), immediate cued recall (Figure 2E, r=0.484, P<0.05; Figure 2F, r=0.497, P<0.05), and delayed cued recall (Figure 2G, r=0.571, P<0.05; Figure 2H, r=0.448, P<0.05) of the CVLT-II (Figure 2). In the sepsis group, the hippocampal volume was significantly positively correlated with recollection but wasn’t correlated with familiarity (P<0.05). No correlation was found between the hippocampal volume and CVLT-II in the healthy control group (P>0.05), and between other cognitive tests and hippocampal volume in the two groups (P>0.05).
Figure 2.
Figure 2.
Correlations between APACHE II scores and hippocampal volume (A and B) and between estimates of neuropsychological test results and hippocampal volumes (C-H).
DISCUSSION
Severe infection often causes neurological impairment. In a prospective cohort study, Yaffe et al[27] first reported a threefold increase in the risk of moderate-to-severe cognitive impairment after recovery from severe sepsis. A considerable number of patients develop abnormal neuropsychiatric function during hospitalization. After excluding direct infection of the central nervous system, head trauma, fat embolism, and adverse drug reactions that affect the state of consciousness, the diffuse brain dysfunction caused by the systemic inflammatory response can be diagnosed as SAE.[4,5] Many sepsis patients don’t receive comprehensive neuropsychological tests after discharge because they do not have obvious mental disorders during their hospital stay. Clinicians do not obtain a clear understanding of the nervous system function in sepsis patients; thus, many patients do not receive the corresponding rehabilitation treatment. In the present study, the volume of the hippocampus in sepsis patients without neurological and psychiatric abnormalities was found to be reduced compared with that in the control group.
Azabou et al[28] found that an abnormal EEG and mental disorders could occur in the early stage of sepsis. The investigators further analyzed the data of sepsis patients in the recovery stage or discharged from the hospital about one month after treatment. Thus, in our study, we performed neuropsychological tests in participants within one month after enrollment.
Several neuropsychological tests on cognitive functions were performed, including visual, attention, memory, executive, and working memory. Although no differences in IQ, visual assessment, executive function, or attention test were found between sepsis patients and controls, sepsis patients exhibited a lower relative performance in immediate free recall, immediate cued recall, and delayed cued recall. Sepsis increases the risk of dementia[29,30,31] that severely affects the integrity of cognition and function[32] and reduces the quality of life.[30] In this study, no significant decline in the executive and attention functions was found in the early stage after sepsis patients were discharged from the hospital. This finding indicated that the impairment of executive and attention functions might not be an acute process, and rehabilitation training might delay the decline in executive and attention functions, thereby improving the life quality of sepsis patients.
The memory function of sepsis patients, immediate free recall, immediate cued recall, or delayed cued recall declined significantly. The CA1 area and presubiculum of the hippocampus were related to the learning and memory functions.[31] The integrity of hippocampal neuronal structure and function is the premise of maintaining learning and memory; the decline in memory function in sepsis patients may be related to the decrease in the hippocampal volume.
In this study, the APACHE II scores on admission were negatively correlated with the hippocampal volume in the sepsis group. The results were similar to those of previous studies, indicating that the APACHE II score had a particular significance in the prognosis of patients with severe nervous system disorders.[33] The APACHE II scores of sepsis patients can be used as an index to evaluate the integrity of the nervous system.
The hippocampal volume was significantly correlated with recollection, but not with familiarity. The memory function of the hippocampus was controversial.[34,35] Some differences existed between familiarity and recollection as two different components of memory. The findings of this study supported the idea that the hippocampus had a function in recollection. The volume of the presubiculum in the hippocampus decreased in sepsis patients, indicating that recollection was related to this area.
Because of the effects of various inflammatory factors, sepsis patients often develop hypotension leading to insufficient cerebral perfusion and changes in brain microcirculation.[4,5] The neuronal damage after cerebral ischemia is region-selective, and the vulnerability of neurons in sensitive areas is also different during cerebral ischemia and hypoxia.[14] In this study, the volume of the presubiculum decreased in the sepsis patients, and this was consistent with the results of previous studies. The main subjects of previous studies were patients with whole brain chronic hypoxia or acute hypoxia. The findings of our study indicated that the whole brain hypoxic condition may exist in sepsis instead of a localized injury caused by local exposure to inflammatory factors alone.
These three results indicate that the factors that cause intracranial injury in sepsis patients may be more complicated than simple ischemia and hypoxia.
The volume of the presubiculum, which was not a vulnerable area of patients, also decreased in the areas considered to be vulnerable to ischemia. These results indicated that the factors, which caused intracranial injury in sepsis patients, might be more complicated. Of course, we cannot rule out inaccuracies due to the small sample size, the clarity of imaging, and the FreesSufer software division of the hippocampal formation.
The present study mainly focused on sepsis patients who didn’t have an obvious nervous system dysfunction during hospitalization but had abnormal EEGs. Because SAE is often diagnosed by clinical manifestations, some sepsis patients with abnormal EEGs are not timely recognized with SAE. Although most patients have early memory impairment, they are often discharged without evaluated with neuropsychological measures, and they are not considered in need of rehabilitation training. The impairment gradually affects the executive and attention functions, which can lead to challenges in life after discharge. Therefore, more advanced tests are needed to identify neurological abnormalities in sepsis patients during hospitalization, and early rehabilitation of sepsis patients who are not diagnosed with SAE should not be neglected. This approach may contribute to an improvement in the life quality of patients. We also found that executive and attention dysfunctions did not exist in sepsis patients at an early stage, and thus, by taking some steps early, we may be able to prevent or slow the decline in executive and attention functions.
There were some limitations in our study. The control group in our study was composed of healthy people. Although they were matched with the sepsis group for basic features such as sex, age, educational level, hypertension, CHD, diabetes, smoking, and NSAID use, sepsis patients may also have some unknown high risk of infection. Meanwhile, the study was a single-center, limited-sample study, which might affect the reliability of the results.
CONCLUSIONS
In general, sepsis can lead to a decrease in the size of the hippocampus, accompanied by early memory deficits. More advanced tests are needed to identify neurological abnormalities in sepsis patients during hospitalization. Even if they do not develop neurological dysfunction during hospitalization, sepsis patients should be assessed neurologically and, if necessary, treated with appropriate rehabilitation after hospital discharge. This strategy may improve long-term nervous system prognosis and quality of life, and reduce the incidence of non-Alzheimer’s dementia.
Funding: This work was supported by the Shanxi Province Key Scientific and Technological Project (2016YFJH2-05), and the Youth Project of the Second Affiliated Hospital of Xi’an Jiaotong University (YJ[QN]201523).
Ethical approval: The Research Ethics Board of the Medical Center and Psychology Department of the Xi’an Jiaotong University approved this study.
Conflicts of interest: The authors have no competing interests relevant to the present study.
Contributors: All authors read and approved the final version of the manuscript.
Reference
Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016
DOI:10.1007/s00134-016-4523-0 URL [Cited within: 2]
Impact of encephalopathy on mortality in the sepsis syndrome. The Veterans Administration Systemic Sepsis Cooperative Study Group
DOI:10.1097/00003246-199008000-00001
URL
PMID:2379391
[Cited within: 2]

Sepsis, an important cause of hospital mortality, continues to be a diagnostic and therapeutic challenge. To define more clearly the impact of encephalopathy on the course of sepsis, the various clinical signs of sepsis, blood culture results, and mortality rates were examined in relation to mental status in septic patients. Patients were classified as having an acutely altered mental status due to sepsis (AAMS), preexisting altered mental status (PAMS), or normal mental status (NMS). Twenty-three (307/1333) percent of the study patients had an acutely altered sensorium secondary to sepsis. Patients with AAMS had a higher mortality (49%) than patients with PAMS (41%) or patients with NMS (26%) (p less than .000001). Multivariate analysis disclosed that altered mental status, hypothermia, hypotension, thrombocytopenia, and the absence of shaking chills were independent predictors of increased mortality in the sepsis syndrome. Patients with Gram-negative bacteremia (28%) were as likely to have AAMS as patients with Gram-positive bacteremia (25%) or patients with negative blood cultures (23%). In summary, alterations in mental status are common in septic patients, and are associated with significantly higher mortality.
The encephalopathy associated with septic illness
URL
PMID:2078909
[Cited within: 1]

Physicians and surgeons have long recognized that septic illness may be accompanied by abnormal brain functions; however, no systematic, comprehensive study has been done to define the clinical and laboratory features of the syndrome of sepsis-associated encephalopathy. We undertook such a prospective study in a tertiary care hospital and found that of 69 patients with fever and microbial cultures, 32 had marked brain dysfunction, 17 showed mild encephalopathy, and 20 were clinically nonencephalopathic. Severe cases showed obtundation and paratonic rigidity while milder cases showed confusion, inappropriate behavior, inattention, disorientation, and writing errors. There were no focal neurological deficits. The following factors correlated with the severity of brain dysfunction: adult respiratory distress syndrome; fatal outcome; certain types of EEG abnormality; axonal peripheral neuropathy; elevated peripheral white blood cell count; elevated serum levels of alkaline phosphatase, bilirubin, creatinine, phosphate, potassium, and urea; reduced blood pressure and reduced serum albumin level. Our data suggest that brain functions fail with dysfunction of other organs in septic illness. Pathogenetic mechanisms are discussed. The brain dysfunction should be regarded as potentially reversible, even in severely encephalopathic cases. Prompt control of the infection is the most important measure in controlling the encephalopathy and in preventing the increased mortality found with severely encephalopathic patients.
Sepsis associated encephalopathy
Pathophysiology of septic encephalopathy: a review
DOI:10.1097/00003246-200008000-00057
URL
PMID:10966289
[Cited within: 3]

OBJECTIVES: Encephalopathy is a common complication of sepsis. This review describes the different pathologic mechanisms that may be involved in its etiology. DATA SOURCES: The studies described here were derived from the database PubMed (http: inverted question mark inverted question markwww.nlm.nih.gov) and from references identified in the bibliographies of pertinent articles and books. The citations are largely confined to English language articles between 1966 and 1998. Older publications were used if they were of historical significance. STUDY SELECTION: All investigations in which any aspect of septic encephalopathy was reported were included. This selection encompasses clinical, animal, and in vitro cell culture work. DATA EXTRACTION: The literature cited was published in peer-reviewed clinical or basic science journals or in books. DATA SYNTHESIS: Contradictions between the results of published studies are discussed. CONCLUSIONS: The most immediate and serious complication of septic encephalopathy is impaired consciousness, for which the patient may require ventilation. The etiology of septic encephalopathy involves reduced cerebral blood flow and oxygen extraction by the brain, cerebral edema, and disruption of the blood-brain barrier that may arise from the action of inflammatory mediators on the cerebrovascular endothelium, abnormal neurotransmitter composition of the reticular activating system, impaired astrocyte function, and neuronal degeneration. Currently, there is no treatment.
Impaired cerebrovascular autoregulation in patients with severe sepsis and sepsis-associated delirium
Pattern of brain injury in the acute setting of human septic shock
Clinical and imaging correlates of EEG patterns in hospitalized patients with encephalopathy
DOI:10.1007/s00415-012-6766-1
URL
[Cited within: 1]

To identify the relationship between pathologic electroencephalographic (EEG) patterns, clinical and neuroradiological abnormalities, and outcome in hospitalized patients with acute encephalopathy. This 5-year cohort study was performed at an academic tertiary care center. EEGs in 154 patients with altered mental status were classified according to five predefined patterns: Isolated continuous slowing of background activity (theta, theta/delta, and delta activity) and patterns with slowing background activity with episodic transients [i.e., triphasic waves (TWs) or frontal intermittent delta activity (FIRDA)]. Clinical characteristics, blood tests and neuroimaging were compared among groups. Associations between EEG patterns and structural and non-structural abnormalities were calculated. Glasgow Outcome Score >3 at discharge was defined as favorable and 1–3 as unfavorable outcome. In multivariable analyses, theta was associated with brain atrophy (OR 2.6, p = 0.020), theta/delta with intracerebral hemorrhages (OR 6.8, p = 0.005), FIRDA with past cerebrovascular accidents (OR 2.7, p = 0.004), TWs with liver or multi-organ failure (OR 6, p = 0.004; OR 4, p = 0.039), and delta activity with alcohol/drug abuse with or without intoxication, and HIV infection (OR 3.8, p = 0.003; OR 9, p = 0.004). TWs were associated with death (OR 4.5, p = 0.005); theta/delta with unfavorable outcomes (OR 2.5, p = 0.033), while patients with FIRDA had favorable outcomes (OR 4.8, p = 0.004). In encephalopathic patients, well-defined EEG patterns are associated with specific pathological conditions and outcomes, suggesting that mechanistic hypotheses underlie these abnormal EEG patterns. To clarify the respective contributions of non-structural and structural abnormalities to encephalopathy reflected in specific EEG patterns, prospective studies using continuous EEG monitoring during the acute onset of encephalopathy are needed.
Effect of dexmedetomidine versus lorazepam on outcome in sepsis patients: an a priori-designed analysis of the MENDS randomized controlled trial
DOI:10.1186/cc8916
URL
PMID:20233428
[Cited within: 1]

INTRODUCTION: Benzodiazepines and alpha2 adrenoceptor agonists exert opposing effects on innate immunity and mortality in animal models of infection. We hypothesized that sedation with dexmedetomidine (an alpha2 adrenoceptor agonist), as compared with lorazepam (a benzodiazepine), would provide greater improvements in clinical outcomes among septic patients than among non-septic patients. METHODS: In this a priori-determined subgroup analysis of septic vs non-septic patients from the MENDS double-blind randomized controlled trial, adult medical/surgical mechanically ventilated patients were randomized to receive dexmedetomidine-based or lorazepam-based sedation for up to 5 days. Delirium and other clinical outcomes were analyzed comparing sedation groups, adjusting for clinically relevant covariates as well as assessing interactions between sedation group and sepsis. RESULTS: Of the 103 patients randomized, 63 (31 dexmedetomidine; 32 lorazepam) were admitted with sepsis and 40 (21 dexmedetomidine; 19 lorazepam) without sepsis. Baseline characteristics were similar between treatment groups for both septic and non-septic patients. Compared with septic patients who received lorazepam, the dexmedetomidine septic patients had 3.2 more delirium/coma-free days (DCFD) on average (95% CI for difference, 1.1 to 4.9), 1.5 (-0.1, 2.8) more delirium-free days (DFD) and 6 (0.3, 11.1) more ventilator-free days (VFD). The beneficial effects of dexmedetomidine were more pronounced in septic patients than in non-septic patients for both DCFDs and VFDs (P-value for interaction = 0.09 and 0.02 respectively). Additionally, sedation with dexmedetomidine, compared with lorazepam, reduced the daily risk of delirium [OR, CI 0.3 (0.1, 0.7)] in both septic and non-septic patients (P-value for interaction = 0.94). Risk of dying at 28 days was reduced by 70% [hazard ratio 0.3 (0.1, 0.9)] in dexmedetomidine patients with sepsis as compared to the lorazepam patients; this reduction in death was not seen in non-septic patients (P-value for interaction = 0.11). CONCLUSIONS: In this subgroup analysis, septic patients receiving dexmedetomidine had more days free of brain dysfunction and mechanical ventilation and were less likely to die than those that received a lorazepam-based sedation regimen. These results were more pronounced in septic patients than in non-septic patients. Prospective clinical studies and further preclinical mechanistic studies are needed to confirm these results. TRIAL REGISTRATION: NCT00095251.
Microcirculatory alterations in patients with severe sepsis: impact of time of assessment and relationship with outcome
DOI:10.1097/CCM.0b013e3182742e8b
URL
PMID:23318492
[Cited within: 2]

OBJECTIVES: Sepsis induces microvascular alterations that may play an important role in the development of organ dysfunction. However, the relationship of these alterations to systemic variables and outcome is still not well defined. We investigated which factors may influence microcirculatory alterations in patients with severe sepsis and whether these are independently associated with mortality. DESIGN: Analysis of prospectively collected data from previously published studies by our group. SETTING: A 36-bed, medicosurgical university hospital Department of Intensive Care. PATIENTS: A total of 252 patients with severe sepsis in whom the sublingual microcirculation was visualized using orthogonal polarization spectral or sidestream darkfield imaging techniques. MEASUREMENTS AND MAIN RESULTS: Microcirculatory measurements were obtained either early, within 24h of the onset of severe sepsis (n = 204), or later, after 48h (n = 48). When multiple measurements were obtained, only the first was considered. Although global hemodynamic variables were relatively preserved (mean arterial pressure 70 [65-77] mm Hg, cardiac index 3.3 [2.7-4.0] L/min.m, and SvO2 68.3 [62.8-74.7]%), microvascular variables were markedly altered (proportion of perfused small vessels 65 [50-74]%, microvascular flow index 2.15 [1.80-2.60], and heterogeneity of proportion of perfused small vessels 35 [20-50]%). Among microcirculatory variables, proportion of perfused small vessels was the strongest predictor of outcome (receiver operating characteristic curve area 0.818 [0.766-0.871], p < 0.001). Survival rates decreased markedly with severity of alterations in the proportion of perfused small vessels (70% and 75% in the two upper proportion of perfused small vessel quartiles compared with 3% and 44% in the two lower quartiles, p < 0.0001). Multivariable analysis identified proportion of perfused small vessels and sequential organ failure assessment score as independent predictors of outcome. Microcirculatory alterations were less severe in the later than in the earlier (proportion of perfused small vessels, 74 [57-82]% vs. 63 [48-71]%, p = 0.004) phase of sepsis. In multivariable analysis focused on the early period of sepsis, proportion of perfused small vessels and lactate were independent predictors of outcome. CONCLUSIONS: Microcirculatory alterations are stronger predictors of outcome than global hemodynamic variables.
Cerebral autoregulation is influenced by carbon dioxide levels in patients with septic shock
DOI:10.1007/s12028-009-9289-6
URL
[Cited within: 1]

Background
Altered brain perfusion may play an important role in the development of sepsis-associated encephalopathy. However, whether or not cerebral autoregulation (CA) is preserved in such condition has been debated. CA is dependent on cerebral vascular tone, the main determinant of which is the concentration of carbon dioxide (CO2). The purpose of this study was to evaluate the influence of PaCO2 on the cerebral autoregulatory capacity in patients with septic shock.Dysfunction of vasomotor reactivity in severe sepsis and septic shock
DOI:10.1007/s001340101005
URL
PMID:11534574
[Cited within: 1]

OBJECTIVE: Perfusion abnormalities are an overall phenomenon in severe sepsis and septic shock, leading to organ dysfunction. We investigated whether carbon dioxide (CO2)-induced vasomotor reactivity (VMR) is impaired in septic patients, compared with values obtained outside sepsis. DESIGN: Prospective, clinical study. SETTING: Six-bed neurologic critical care unit of a university hospital. PATIENTS AND PARTICIPANTS: Eight consecutive patients with severe sepsis and septic shock. MEASUREMENTS AND RESULTS: CO2-reactivity was measured during and outside a period of severe sepsis or septic shock according to ACCP/SCCM criteria by means of transcranial Doppler sonography and near-infrared spectroscopy (NIRS). VMR was calculated as the percentage change of cerebral blood flow velocity (normalized CO2-reactivity, NCR) and absolute changes in concentration of oxygenated hemoglobin, deoxygenated hemoglobin, total hemoglobin (HbO2, Hb, HbT) and Hbdiff (difference between HbO2 and Hb) in micromol/l per 1% increase in end-tidal CO2 (CR-HbO2, CR-Hb, CR-HbT, CR-Hbdiff). NCR and NIRS-reactivities were significantly reduced during severe sepsis and septic shock compared with values outside sepsis (mean, SD, Wilcoxon): NCR 11.0 (7.1) versus 30.7 (13.0), p < 0.02; CR-HbO2 0.70 (0.61) versus 2.33 (1.11), p < 0.02; CR-Hb -0.17 (0.74) versus -1.42 (1.28), p < 0.04; CR-HbT 0.53 (0.48) versus 1.05 (0.40), p < 0.03; CR-Hbdiff 0.91 (1.33) versus 3.75 (2.33), p < 0.02. This indicates a severely disturbed VMR. CONCLUSIONS: In the advent of a disturbed cerebral autoregulation, critical drops in blood pressure during sepsis are transferred directly into the vascular bed, leading to cerebral hypoperfusion. This mechanism might contribute to the pathogenesis of septic encephalopathy.
Cerebral perfusion in sepsis-associated delirium
DOI:10.1186/cc6891
URL
PMID:18457586
[Cited within: 1]

INTRODUCTION: The pathophysiology of sepsis-associated delirium is not completely understood and the data on cerebral perfusion in sepsis are conflicting. We tested the hypothesis that cerebral perfusion and selected serum markers of inflammation and delirium differ in septic patients with and without sepsis-associated delirium. METHODS: We investigated 23 adult patients with sepsis, severe sepsis, or septic shock with an extracranial focus of infection and no history of intracranial pathology. Patients were investigated after stabilisation within 48 hours after admission to the intensive care unit. Sepsis-associated delirium was diagnosed using the confusion assessment method for the intensive care unit. Mean arterial pressure (MAP), blood flow velocity (FV) in the middle cerebral artery using transcranial Doppler, and cerebral tissue oxygenation using near-infrared spectroscopy were monitored for 1 hour. An index of cerebrovascular autoregulation was calculated from MAP and FV data. C-reactive protein (CRP), interleukin-6 (IL-6), S-100beta, and cortisol were measured during each data acquisition. RESULTS: Data from 16 patients, of whom 12 had sepsis-associated delirium, were analysed. There were no significant correlations or associations between MAP, cerebral blood FV, or tissue oxygenation and sepsis-associated delirium. However, we found a significant association between sepsis-associated delirium and disturbed autoregulation (P = 0.015). IL-6 did not differ between patients with and without sepsis-associated delirium, but we found a significant association between elevated CRP (P = 0.008), S-100beta (P = 0.029), and cortisol (P = 0.011) and sepsis-associated delirium. Elevated CRP was significantly correlated with disturbed autoregulation (Spearman rho = 0.62, P = 0.010). CONCLUSION: In this small group of patients, cerebral perfusion assessed with transcranial Doppler and near-infrared spectroscopy did not differ between patients with and without sepsis-associated delirium. However, the state of autoregulation differed between the two groups. This may be due to inflammation impeding cerebrovascular endothelial function. Further investigations defining the role of S-100beta and cortisol in the diagnosis of sepsis-associated delirium are warranted. TRIAL REGISTRATION: ClinicalTrials.gov NCT00410111.
Selective vulnerability of the hippocampus in brain ischemia
DOI:10.1016/j.neuroscience.2015.08.034 URL [Cited within: 3]
Delirium as a predictor of long-term cognitive impairment in survivors of critical illness
DOI:10.1097/CCM.0b013e3181e47be1
URL
PMID:20473145
[Cited within: 1]

OBJECTIVE: To test the hypothesis that duration of delirium in the intensive care unit is an independent predictor of long-term cognitive impairment after critical illness requiring mechanical ventilation. DESIGN: Prospective cohort study. SETTING: Medical intensive care unit in a large community hospital in the United States. PATIENTS: Mechanically ventilated medical intensive care unit patients who were assessed daily for delirium while in the intensive care unit and who underwent comprehensive cognitive assessments 3 and 12 mos after discharge. MEASUREMENTS AND MAIN RESULTS: Of 126 eligible patients, 99 survived>or=3 months after critical illness; long-term cognitive outcomes were obtained for 77 (78%) patients. Median age was 61 yrs, 51% were admitted with sepsis/acute respiratory distress syndrome, and median duration of delirium was 2 days. At 3-mo and 12-mo follow-up, 79% and 71% of survivors had cognitive impairment, respectively (with 62% and 36% being severely impaired). After adjusting for age, education, preexisting cognitive function, severity of illness, severe sepsis, and exposure to sedative medications in the intensive care unit, increasing duration of delirium was an independent predictor of worse cognitive performance-determined by averaging age-adjusted and education-adjusted T-scores from nine tests measuring seven domains of cognition-at 3-mo (p=.02) and 12-mo follow-up (p=.03). Duration of mechanical ventilation, alternatively, was not associated with long-term cognitive impairment (p=.20 and .58). CONCLUSIONS: In this study of mechanically ventilated medical intensive care unit patients, duration of delirium (which is potentially modifiable) was independently associated with long-term cognitive impairment, a common public health problem among intensive care unit survivors.
Septicemia is associated with increased risk for dementia: a population-based longitudinal study
DOI:10.18632/oncotarget.20899
URL
PMID:29137424
[Cited within: 1]

Background: Systemic infection has been linked to cognitive impairment. We hypothesized that patients with septicemia are predisposed to increased risks for developing dementia in a long-term setting. Methods: This observational, retrospective, longitudinal, nation-wide population-based study was conducted using the data deduced from Longitudinal Health Insurance Database (LHID) in Taiwan. All patients with septicemia hospitalized for the first time from 2001 to 2011 without prior dementia were included. The development of Alzheimer's disease (AD) or non-Alzheimer dementias (NAD) in relation to the development of septicemia for each patient was recorded. An age- and sex-matched cohort without septicemia and without prior dementia served as the control. Septicemia, dementia, and other confounding factors were defined according to International Classification of Diseases Clinical Modification Codes. Cox proportional-hazards regressions were utilized to analyze adjusted hazard ratios. Results: Patients with septicemia had a higher risk for developing dementia based on hazard ratios (HRs) (p<0.001). Patients with septicemia in the younger age groups had a greater dementia risk (p<0.01). Septicemia was associated with subsequent NAD (p<0.001), whereas the increased risk of AD was statistically insignificant (p>0.05). Furthermore, higher severity of septicemia was associated with increased risk of developing dementia. Conclusions: Our findings suggest that septicemia is associated with an increased risk in developing NAD but not AD. A likely causal role of septicemia in increasing the risk of NAD is suggested, according to the findings that patients with higher severity of septicemia carried greater risk of sustaining dementia.
Long-term cognitive impairment and functional disability among survivors of severe sepsis
DOI:10.1001/jama.2010.1553
URL
PMID:20978258
[Cited within: 1]

CONTEXT: Cognitive impairment and functional disability are major determinants of caregiving needs and societal health care costs. Although the incidence of severe sepsis is high and increasing, the magnitude of patients' long-term cognitive and functional limitations after sepsis is unknown. OBJECTIVE: To determine the change in cognitive impairment and physical functioning among patients who survive severe sepsis, controlling for their presepsis functioning. DESIGN, SETTING, AND PATIENTS: A prospective cohort involving 1194 patients with 1520 hospitalizations for severe sepsis drawn from the Health and Retirement Study, a nationally representative survey of US residents (1998-2006). A total of 9223 respondents had a baseline cognitive and functional assessment and had linked Medicare claims; 516 survived severe sepsis and 4517 survived a nonsepsis hospitalization to at least 1 follow-up survey and are included in the analysis. MAIN OUTCOME MEASURES: Personal interviews were conducted with respondents or proxies using validated surveys to assess the presence of cognitive impairment and to determine the number of activities of daily living (ADLs) and instrumental ADLs (IADLs) for which patients needed assistance. RESULTS: Survivors' mean age at hospitalization was 76.9 years. The prevalence of moderate to severe cognitive impairment increased 10.6 percentage points among patients who survived severe sepsis, an odds ratio (OR) of 3.34 (95% confidence interval [CI], 1.53-7.25) in multivariable regression. Likewise, a high rate of new functional limitations was seen following sepsis: in those with no limits before sepsis, a mean 1.57 new limitations (95% CI, 0.99-2.15); and for those with mild to moderate limitations before sepsis, a mean of 1.50 new limitations (95% CI, 0.87-2.12). In contrast, nonsepsis general hospitalizations were associated with no change in moderate to severe cognitive impairment (OR, 1.15; 95% CI, 0.80-1.67; P for difference vs sepsis = .01) and with the development of fewer new limitations (mean among those with no limits before hospitalization, 0.48; 95% CI, 0.39-0.57; P for difference vs sepsis <.001 and mean among those with mild to moderate limits, 0.43; 95% CI, 0.23-0.63; P for difference = .001). The declines in cognitive and physical function persisted for at least 8 years. CONCLUSIONS: Severe sepsis in this older population was independently associated with substantial and persistent new cognitive impairment and functional disability among survivors. The magnitude of these new deficits was large, likely resulting in a pivotal downturn in patients' ability to live independently.
APACHE II: a severity of disease classification system
URL
PMID:3928249
[Cited within: 1]

This paper presents the form and validation results of APACHE II, a severity of disease classification system. APACHE II uses a point score based upon initial values of 12 routine physiologic measurements, age, and previous health status to provide a general measure of severity of disease. An increasing score (range 0 to 71) was closely correlated with the subsequent risk of hospital death for 5815 intensive care admissions from 13 hospitals. This relationship was also found for many common diseases. When APACHE II scores are combined with an accurate description of disease, they can prognostically stratify acutely ill patients and assist investigators comparing the success of new or differing forms of therapy. This scoring index can be used to evaluate the use of hospital resources and compare the efficacy of intensive care in different hospitals or over time.
WAIS-III and WMS-III performance in chronic Lyme disease
DOI:10.1017/S1355617706060231
URL
PMID:16433951
[Cited within: 1]

There is controversy regarding the nature and degree of intellectual and memory deficits in chronic Lyme disease. In this study, 81 participants with rigorously diagnosed chronic Lyme disease were administered the newest revisions of the Wechsler Adult Intelligence Scale (WAIS-III) and Wechsler Memory Scale (WMS-III), and compared to 39 nonpatients. On the WAIS-III, Lyme disease participants had poorer Full Scale and Performance IQ's. At the subtest level, differences were restricted to Information and the Processing Speed subtests. On the WMS-III, Lyme disease participants performed more poorly on Auditory Immediate, Immediate, Auditory Delayed, Auditory Recognition Delayed, and General Memory indices. Among WMS-III subtests, however, differences were restricted to Logical Memory (immediate and delayed) and Family Pictures (delayed only), a Visual Memory subtest. Discriminant analyses suggest deficits in chronic Lyme are best characterized as a combination of memory difficulty and diminished processing speed. Deficits were modest, between one-third and two-thirds of a standard deviation, consistent with earlier studies. Depression severity had a weak relationship to processing speed, but little other association to test performance. Deficits in chronic Lyme disease are consistent with a subtle neuropathological process affecting multiple performance tasks, although further work is needed to definitively rule out nonspecific illness effects.
Development of the Chinese version of the Hooper Visual Organization Test: normative data
DOI:10.1097/MRR.0b013e3283588b95
URL
[Cited within: 1]

The present study consisted of two phases: development and psychometric validation of a Chinese version of the Hooper Visual Organization Test (HVOT) using Rasch analysis and the provision of normative data on the basis of a representative sample of the Chinese-speaking population. The HVOT was administered to 1008 healthy adults aged 15-79 years, 60 patients with stroke, and 60 patients with schizophrenia. The results indicated that with 12 items removed, the resulting 18-item scale was found to be unidimensional, with satisfactory internal consistency and no evidence of differential item functioning or bias for age, sex and educational level. There were significant differences between each of the two patient groups and normal controls on the scores of the Rasch-developed measure. All test-retest coefficients exceeded 90 in patient samples. As performance on the Chinese version decreases with age and lower years of education, regression-based normative data that took age and education into account were established. A cut-off score of 21.5, out of an x-y range, the higher the better, resulted in a sensitivity of 0.86 and a specificity of 0.68. The normative data presented here will enable clinicians to determine different levels of visuosynthetic impairments more precisely.
The California Verbal Learning Test-second edition: test-retest reliability, practice effects, and reliable change indices for the standard and alternate forms
DOI:10.1016/j.acn.2006.06.002
URL
PMID:16843636
[Cited within: 1]

The California Verbal Learning Test - second edition (CVLT-II) is one of the most widely used neuropsychological tests in North America. The present study evaluated the 1-month test-retest reliability and practice effects associated with the standard and alternate forms of the CVLT-II in a sample of 195 healthy adults. Eighty participants underwent repeat assessment using the standard form of the CVLT-II on both occasions, whereas the remaining 115 individuals received the standard form at baseline and the alternate form at follow-up. Consistent with prior research, results revealed generally large test-retest correlation coefficients for the primary CVLT-II measures in both the standard/standard (range=0.80-0.84) and standard/alternate (range=0.61-0.73) cohorts. Despite exhibiting slightly lower test-retest reliability coefficients, participants in the alternate form group displayed notably smaller practice effects (Cohen's d range=-0.01 to 0.18) on the primary indices relative to individuals who received the standard form on both occasions (Cohen's d range=0.27-0.61). Reliable change indices were also generated and applied to primary CVLT-II variables to determine the base rates of significant improvements (range=2-10%), declines (range=0-7%), and stability (range=85-97%) in performance over time. Overall, findings from this study support the test-retest reliability of the standard and alternate forms of the CVLT-II in healthy adults and may enhance the usefulness of this test in longitudinal neuropsychological evaluations.
Studies of interference in serial verbal reactions
DOI:10.1037/h0054651 URL [Cited within: 1]
Sensitivity of the Wisconsin Card Sorting Test (64-Card Version) versus the Tower of London (Drexel Version) for detecting executive dysfunction in children with epilepsy
DOI:10.1080/09297049.2016.1265101
URL
PMID:28049367
[Cited within: 1]

Executive function deficits are common in children and adolescents with epilepsy. Though the Wisconsin Card Sorting Task (WCST) is often considered the
The 50- and 100-item short forms of the Paced Auditory Serial Addition Task (PASAT): demographically corrected norms and comparisons with the full PASAT in normal and clinical samples
DOI:10.1076/jcen.25.4.571.13876
URL
PMID:12911108
[Cited within: 1]

While the standard 200-item version of the Paced Auditory Serial Addition Task (PASAT) is a sensitive neuropsychological instrument, it can be quite aversive to some patients due to its length and progressively increasing difficulty. We present demographically-corrected norms for 50 and 100-item short-form versions in a sample of 560 neurologically normal adults. Age, education, and ethnicity (but not gender) were found to be significant predictors of performance. In a clinical sample of 786 HIV-infected adults, diagnostic accuracy of the 50, 100, and 200-item versions was essentially equivalent (using clinical ratings of a comprehensive neuropsychological battery as the gold standard, overall classification rates of the three PASAT versions were 71%, 74%, and 73%, respectively), with better specificity (89-92%) than sensitivity (46-53%). The 50-item version showed moderate ceiling effects, but the 100-item test did not. In a mixed clinical sample of 40 subjects, the 50-item version was administered more than twice as fast as the 200-item version, and was tolerated better (discomfort rating of 4.0 vs. 5.9 on a 10-point scale, p < .05). We conclude that in many cases the PASAT-50 and PASAT-100 provide equivalent diagnostic accuracy with a significant reduction in administration time and patient discomfort.
A process dissociation framework: separating automatic from intentional uses of memory
DOI:10.1016/0749-596X(91)90025-F URL [Cited within: 1]
FreeSurfer
DOI:10.1016/j.neuroimage.2012.01.021
URL
[Cited within: 1]

FreeSurfer is a suite of tools for the analysis of neuroimaging data that provides an array of algorithms to quantify the functional, connectional and structural properties of the human brain. It has evolved from a package primarily aimed at generating surface representations of the cerebral cortex into one that automatically creates models of most macroscopically visible structures in the human brain given any reasonable T1-weighted input image. It is freely available, runs on a wide variety of hardware and software platforms, and is open source. (C) 2012 Elsevier Inc.
Patient and caregiver characteristics and nursing home placement in patients with dementia
DOI:10.1001/jama.287.16.2090
URL
PMID:11966383
[Cited within: 1]

CONTEXT: The decision to institutionalize a patient with dementia is complex and is based on patient and caregiver characteristics and the sociocultural context of patients and caregivers. Most studies have determined predictors of nursing home placement primarily according to patient or caregiver characteristics alone. OBJECTIVE: To develop and validate a prognostic model to determine the comprehensive predictors of placement among an ethnically diverse population of patients with dementia. DESIGN, SETTING, AND PARTICIPANTS: The Medicare Alzheimer's Disease Demonstration and Evaluation study, a prospective study at 8 sites in the United States, with enrollment between December 1989 and December 1994 of 5788 community-living persons with advanced dementia. MAIN OUTCOME MEASURES: Time to nursing home placement throughout a 36-month follow-up period, assessed by interview and review of Medicare records, and its association with patient and caregiver characteristics, obtained by interview at enrollment. RESULTS: Patients were divided into a development (n = 3859) and validation (n = 1929) cohort. In the development cohort, the Kaplan-Meier estimates of nursing home placement throughout 1, 2, and 3 years were 22%, 40%, and 52%, respectively. After multivariate adjustment, patient characteristics that were associated with nursing home placement were as follows: black ethnicity (hazard ratio, 0.60; 95% confidence interval [CI], 0.48-0.74), Hispanic ethnicity (HR, 0.40; 95% CI, 0.28-0.56) (both ethnicities were inversely associated with placement), living alone (HR, 1.74; 95% CI, 1.49-2.02), 1 or more dependencies in activities of daily living (HR, 1.38; 95% CI, 1.20-1.60), high cognitive impairment (for Mini-Mental Status Examination score < or =20: HR, 1.52; 95% CI, 1.33-1.73), and 1 or more difficult behaviors (HR, 1.30; 95% CI, 1.11-1.52). Caregiver characteristics associated with patient placement were age 65 to 74 years (HR, 1.17; 95% CI, 1.01-1.37), age 75 years or older (HR, 1.55; 95% CI, 1.31-1.84), and high Zarit Burden Scale score (for highest quartile: HR, 1.73; 95% CI, 1.49-2.00). Patients were assigned to quartiles of risk based on this model. In the development cohort, patients in the first, second, third, and fourth quartile had a 25%, 42%, 64%, and 91% rate of nursing home placement at 3 years, respectively. In the validation cohort, the respective rates were 21%, 50%, 64%, and 89%. The C statistic for 3-year nursing home placement was 0.66 in the development cohort and 0.63 in the validation cohort. CONCLUSIONS: Patient and caregiver characteristics are both important determinants of long-term care placement for patients with dementia. Interventions directed at delaying placement, such as reduction of caregiver burden or difficult patient behaviors, need to take into account the patient and caregiver as a unit.
Early standard electroencephalogram abnormalities predict mortality in septic intensive care unit patients
DOI:10.1371/journal.pone.0139969
URL
PMID:26447697
[Cited within: 1]

INTRODUCTION: Sepsis is associated with increased mortality, delirium and long-term cognitive impairment in intensive care unit (ICU) patients. Electroencephalogram (EEG) abnormalities occurring at the acute stage of sepsis may correlate with severity of brain dysfunction. Predictive value of early standard EEG abnormalities for mortality in ICU septic patients remains to be assessed. METHODS: In this prospective, single center, observational study, standard EEG was performed, analyzed and classified according to both Synek and Young EEG scales, in consecutive patients acutely admitted in ICU for sepsis. Delirium, coma and the level of sedation were assessed at the time of EEG recording; and duration of sedation, occurrence of in-ICU delirium or death were assessed during follow-up. Adjusted analyses were carried out using multiple logistic regression. RESULTS: One hundred ten patients were included, mean age 63.8 (+/-18.1) years, median SAPS-II score 38 (29-55). At the time of EEG recording, 46 patients (42%) were sedated and 22 (20%) suffered from delirium. Overall, 54 patients (49%) developed delirium, of which 32 (29%) in the days after EEG recording. 23 (21%) patients died in the ICU. Absence of EEG reactivity was observed in 27 patients (25%), periodic discharges (PDs) in 21 (19%) and electrographic seizures (ESZ) in 17 (15%). ICU mortality was independently associated with a delta-predominant background (OR: 3.36; 95% CI [1.08 to 10.4]), absence of EEG reactivity (OR: 4.44; 95% CI [1.37-14.3], PDs (OR: 3.24; 95% CI [1.03 to 10.2]), Synek grade >/= 3 (OR: 5.35; 95% CI [1.66-17.2]) and Young grade > 1 (OR: 3.44; 95% CI [1.09-10.8]) after adjustment to Simplified Acute Physiology Score (SAPS-II) at admission and level of sedation. Delirium at the time of EEG was associated with ESZ in non-sedated patients (32% vs 10%, p = 0.037); with Synek grade >/= 3 (36% vs 7%, p< 0.05) and Young grade > 1 (36% vs 17%, p< 0.001). Occurrence of delirium in the days after EEG was associated with a delta-predominant background (48% vs 15%, p = 0.001); absence of reactivity (39% vs 10%, p = 0.003), Synek grade >/= 3 (42% vs 17%, p = 0.001) and Young grade >1 (58% vs 17%, p = 0.0001). CONCLUSIONS: In this prospective cohort of 110 septic ICU patients, early standard EEG was significantly disturbed. Absence of EEG reactivity, a delta-predominant background, PDs, Synek grade >/= 3 and Young grade > 1 at day 1 to 3 following admission were independent predictors of ICU mortality and were associated with occurence of delirium. ESZ and PDs, found in about 20% of our patients. Their prevalence could have been higher, with a still higher predictive value, if they had been diagnosed more thoroughly using continuous EEG.
Association between dementia and infectious disease: evidence from a case-control study
DOI:10.1097/01.wad.0000165511.52746.1f
URL
PMID:15942327
[Cited within: 1]

Inflammation plays a part in the etiology of dementia. Whether this is the primary pathogenesis, or a secondary reaction is unclear. We postulate that since systemic infection can provoke the enhanced synthesis of inflammatory mediators in the brain, such diseases may promote the onset of dementia. We carried out a nested case-control study using the General Practice Research Database. Cases were patients with incident dementia, and controls without such a diagnosis. Infectious episodes in the four years preceding diagnosis were counted using diagnostic codes, or prescription codes for anti-infective drugs. We considered age, sex, smoking, diabetes mellitus, and frequency of consultation as potential confounders. There were 9954 valid cases, and 9374 valid controls. Cases were on average older, more likely to be female, to smoke and to have diabetes, than the controls. There was an increased risk of diagnosis of dementia in those patients older than 84 with infections (OR for 2 or more infections compared with 0 or 1 = 1.4, 95% CI 1.2 to 1.7). Smoking and diabetes mellitus were also shown to markedly increase the risk of diagnosis of dementia. We have shown a positive association between episodes of infection and increased likelihood of diagnosis of dementia in the very elderly. Smoking and diabetes mellitus are associated with onset of dementia in the elderly. The evidence from this study may represent cause and effect, since there is a credible biologic explanation.
Long-term mortality and quality of life in sepsis: a systematic review
DOI:10.1097/CCM.0b013e3181d8cc1d
URL
PMID:20308885
[Cited within: 2]

BACKGROUND: Long-term outcomes from sepsis are poorly understood, and sepsis in patients may have different long-term effects on mortality and quality of life. Long-term outcome studies of other critical illnesses such as acute lung injury have demonstrated incremental health effects that persist after hospital discharge. Whether patients with sepsis have similar long-term mortality and quality-of-life effects is unclear. OBJECTIVE: We performed a systematic review of studies reporting long-term mortality and quality-of-life data (>3 months) in patients with sepsis, severe sepsis, and septic shock using defined search criteria. DESIGN: Systematic review of the literature. INTERVENTIONS: None. MAIN RESULTS: Patients with sepsis showed ongoing mortality up to 2 yrs and beyond after the standard 28-day inhospital mortality end point. Patients with sepsis also had decrements in quality-of-life measures after hospital discharge. Results were consistent across varying severity of illness and different patient populations in different countries, including large and small studies. In addition, these results were consistent within observational and randomized, controlled trials. Study quality was limited by inadequate control groups and poor adjustment for confounding variables. CONCLUSIONS: Patients with sepsis have ongoing mortality beyond short-term end points, and survivors consistently demonstrate impaired quality of life. The use of 28-day mortality as an end point for clinical studies may lead to inaccurate inferences. Both observational and interventional future studies should include longer-term end points to better-understand the natural history of sepsis and the effect of interventions on patient morbidities.
Evidence for area CA1 as a match/mismatch detector: a high-resolution fMRI study of the human hippocampus
DOI:10.1002/hipo.20933
URL
[Cited within: 2]

The hippocampus is proposed to switch between memory encoding and retrieval by continually computing the overlap between what is expected and what is encountered. Central to this hypothesis is that area CA1 performs this calculation. However, empirical evidence for this is lacking. To test the theoretical role of area CA1 in match/mismatch detection, we had subjects study complex stimuli and then, during high-resolution fMRI scanning, make memory judgments about probes that either matched or mismatched expectations. More than any other hippocampal subfield, area CA1 displayed responses consistent with a match/mismatch detector. Specifically, the responses in area CA1 tracked the total number of changes present in the probe. Additionally, area CA1 was sensitive to both behaviorally relevant and irrelevant changes, a key feature of an automatic comparator. These results are consistent with, and provide the first evidence in humans for, the theoretically important role of area CA1 as a match/mismatch detector. (c) 2011 Wiley Periodicals, Inc.
Long-term outcomes from sepsis
DOI:10.1007/s11908-007-0059-3
URL
[Cited within: 1]

Long-term mortality following severe sepsis is high, and fewer than half of patients who experience severe sepsis are alive at 1 year. Mechanisms underlying increased long-term mortality remain poorly understood. Animal and human studies suggest that abnormalities of the innate immune system may contribute to increased long-term mortality. This review article examines the epidemiology and potential mechanisms underlying long-term outcomes from sepsis and challenges to conducting long-term outcome studies in the critically ill.
Role of APACHE II scoring system in the prediction of severity and outcome of acute intracerebral hemorrhage
DOI:10.3109/00207454.2015.1099099
URL
PMID:26393395
[Cited within: 1]

PURPOSE: Acute intracerebral hemorrhage (ICH) is prone to multiple organ dysfunction and has high disability and mortality. This study was to determine the role of acute physiology and chronic health evaluation II (APACHE II) scoring system in the prediction of severity and outcome of acute ICH. METHODS: A total of 546 ICH patients were prospectively recruited between 1 January 2013 and 31 December 2014. Patients were divided into three groups according to the APACHE II scores: low score group (5-16), moderate score group (17-28) and high score group (>/=29). The ICH volume and location, National Institutes of Health Stroke Scale (NIHSS) scores, Glasgow Coma Score and modified Rankin Scale (mRS) scores were used to assess the severity of acute ICH. Global outcome at three months was evaluated with the mRS. RESULTS: Of 479 patients, the average age was 56.4 +/- 3.4 years, 287 (59.9%) survived and 192 (40.1%) died. Results showed that the higher the APACHE II score, the higher the mortality was; the average hospital stay, ICH volume, NIHSS scores, mRS scores and survival rate were significantly different among three APACHE II groups (p < 0.05). APACHE II scores were able to predict the mortality and correlated positively with actual mortality (r = 0.84, p < 0.01). CONCLUSIONS: APACHE II scoring system can be used to predict the severity and outcome of acute ICH.
The role of the human hippocampus in familiarity-based and recollection-based recognition memory
DOI:10.1016/j.bbr.2010.04.020
URL
PMID:20412819
[Cited within: 1]

The ability to recognize a previously encountered stimulus is dependent on the structures of the medial temporal lobe and is thought to be supported by two processes, recollection and familiarity. A focus of research in recent years concerns the extent to which these two processes depend on the hippocampus and on the other structures of the medial temporal lobe. One view holds that the hippocampus is important for both processes, whereas a different view holds that the hippocampus supports only the recollection process and the perirhinal cortex supports the familiarity process. One approach has been to study patients with hippocampal lesions and to contrast old/new recognition (which can be supported by familiarity) to free recall (which is supported by recollection). Despite some early case studies suggesting otherwise, several group studies have now shown that hippocampal patients exhibit comparable impairments on old/new recognition and free recall. These findings suggest that the hippocampus is important for both recollection and familiarity. Neuroimaging studies and Receiver Operating Characteristic analyses also initially suggested that the hippocampus was specialized for recollection, but these studies involved a strength confound (strong memories have been compared to weak memories). When steps are taken to compare strong recollection-based memories with strong familiarity-based memories, or otherwise control for memory strength, evidence for a familiarity signal (as well as a recollection signal) is evident in the hippocampus. These findings suggest that the functional organization of the medial temporal lobe is probably best understood in terms unrelated to the distinction between recollection and familiarity.
Familiarity and recollection produce distinct eye movement, pupil and medial temporal lobe responses when memory strength is matched
DOI:10.1016/j.neuropsychologia.2012.08.001
URL
[Cited within: 1]

Two experiments explored eye measures (fixations and pupil response patterns) and brain responses (BOLD) accompanying the recognition of visual object stimuli based on familiarity and recollection. In both experiments, the use of a modified remember/know procedure led to high confidence and matched accuracy levels characterising strong familiarity (F3) and recollection (R) responses. In Experiment 1, visual scanning behaviour at retrieval distinguished familiarity-based from recollection-based recognition. Recollection, relative to strength-matched familiarity, involved significantly larger pupil dilations and more dispersed fixation patterns. In Experiment 2, the hippocampus was selectively activated for recollected stimuli, while no evidence of activation was observed in the hippocampus for strong familiarity of matched accuracy. Recollection also activated the parahippocampal cortex (PHC), while the adjacent perirhinal cortex (PRC) was actively engaged in response to strong familiarity (than to recollection). Activity in prefrontal and parietal areas differentiated familiarity and recollection in both the extent and the magnitude of activity they exhibited, while the dorsomedial thalamus showed selective familiarity-related activity, and the ventrolateral and anterior thalamus selective recollection-related activity. These findings are consistent with the view that the hippocampus and PRC play contrasting roles in supporting recollection and familiarity and that these differences are not a result of differences in memory strength. Overall, the combined pupil dilation, eye movement and fMRI data suggest the operation of recognition mechanisms drawing differentially on familiarity and recollection, whose 'neural bases are distinct within the MTL. (C) 2012 Elsevier Ltd.