World Journal of Emergency Medicine ›› 2023, Vol. 14 ›› Issue (2): 112-121.doi: 10.5847/wjem.j.1920-8642.2023.026
• Original Articles • Previous Articles Next Articles
Bao-tao Huang, Yi-heng Cheng, Bo-sen Yang, Yi-ke Zhang, Fang-yang Huang, Yong Peng, Xiao-bo Pu, Mao Chen( )
)
Received:2022-05-09
Online:2023-03-03
Published:2023-03-01
Contact:
Mao Chen
E-mail:hmaochen@vip.sina.com
Bao-tao Huang, Yi-heng Cheng, Bo-sen Yang, Yi-ke Zhang, Fang-yang Huang, Yong Peng, Xiao-bo Pu, Mao Chen. The influence of pressure injury risk on the association between left ventricular ejection fraction and all-cause mortality in patients with acute myocardial infarction 80 years or older[J]. World Journal of Emergency Medicine, 2023, 14(2): 112-121.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2023.026
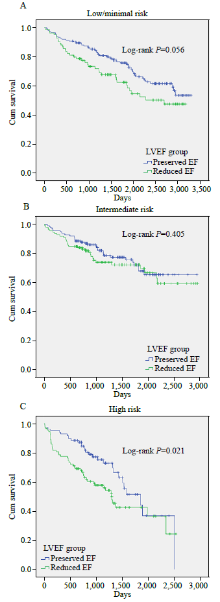
Figure 1.
Kaplan-Meier survival curves of patients with different pressure injury risks stratified by reduced or preserved EF. A: low/minimal pressure injury risk; B: intemediate pressure injury risk; C: high pressure injury risk. LVEF: left ventricular ejection fraction; EF: ejection fraction.
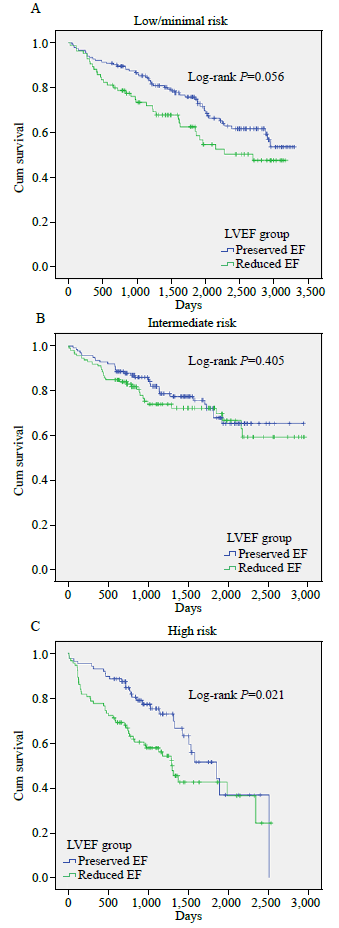
Table 1.
Demographics and baseline characteristics of patients survived hospitalization for AMI with 80 years or older
| Variables | Total (n=677) | Low/minimal risk of pressure injury (n=239) | Intermediate risk of pressure injury (n=256) | High risk of pressure injury (n=182) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preserved EF (n=154) | Reduced EF (n=85) | P-value | Preserved EF (n=142) | Reduced EF (n=114) | P-value | Preserved EF (n=88) | Reduced EF (n=94) | P-value | ||||
| Age, years | 83.0 (81.0-85.0) | 83.0 (81.0-84.0) | 82.0 (81.0-84.0) | 0.397 | 83.0 (81.0-86.0) | 83.0 (81.0-86.0) | 0.672 | 84.0 (81.8-86.0) | 84.0 (81.0-86.0) | 0.900 | ||
| Male | 412 (60.9%) | 93 (60.4%) | 63 (74.1%) | 0.046 | 82 (57.7%) | 64 (56.1%) | 0.896 | 51 (58.0%) | 59 (62.8%) | 0.609 | ||
| BMI, kg/m2 | 22.2 (20.0-24.7) | 23.5 (20.9-27.1) | 22.9 (21.1-24.7) | 0.356 | 22.2 (20.1-24.2) | 22.8 (20.5-24.4) | 0.539 | 20.6 (19.0-24.0) | 21.5 (19.2-24.0) | 0.663 | ||
| Current smoker | 139 (20.5%) | 34 (22.1%) | 19 (22.4%) | 0.036 | 31 (21.8%) | 14 (12.3%) | 0.134 | 20 (22.7%) | 21 (22.3%) | 0.791 | ||
| Current drinker | 111 (16.4%) | 27 (17.5%) | 15 (17.6%) | 0.270 | 24 (16.9%) | 16 (14.0%) | 0.820 | 14 (15.9%) | 15 (16.0%) | 0.414 | ||
| Hypertension | 412 (60.9%) | 92 (59.7%) | 54 (63.5%) | 0.662 | 82 (57.7%) | 69 (60.5%) | 0.748 | 57 (64.8%) | 58 (61.7%) | 0.783 | ||
| Diabetes mellitus | 162 (23.9%) | 42 (27.3%) | 14 (16.5%) | 0.084 | 27 (19.0%) | 32 (28.1%) | 0.119 | 23 (26.1%) | 24 (25.5%) | 1 | ||
| Prior MI | 82 (12.1%) | 14 (9.1%) | 3 (3.5%) | 0.181 | 20 (14.1%) | 14 (12.3%) | 0.812 | 12 (13.6%) | 19 (20.2%) | 0.326 | ||
| Prior PCI | 17 (2.5%) | 3 (1.9%) | 2 (2.4%) | 1 | 3 (2.1%) | 3 (2.6%) | 1 | 1 (1.1%) | 5 (5.3%) | 0.244 | ||
| Prior CABG | 6 (0.9%) | 0 (0.0%) | 1 (1.2%) | 0.763 | 1 (0.7%) | 0 (0.0%) | 1 | 1 (1.1%) | 3 (3.2%) | 0.661 | ||
| Cerebrovascular disease | 64 (9.5%) | 14 (9.1%) | 9 (10.6%) | 0.883 | 13 (9.2%) | 10 (8.8%) | 1 | 14 (15.9%) | 4 (4.3%) | 0.017 | ||
| Peripheral artery disease | 2 (0.3%) | 1 (0.6%) | 0 (0.0%) | 1 | 1 (0.7%) | 0 (0.0%) | 1 | 0 | 0 | NA | ||
| Chronic kidney disease | 43 (6.4%) | 4 (2.6%) | 7 (8.2%) | 0.095 | 5 (3.5%) | 9 (7.9%) | 0.210 | 8 (9.1%) | 10 (10.6%) | 0.920 | ||
| Systolic blood pressure, mmHg | 126.0 (109.8-144.0) | 129.0 (112.0-144.8) | 124.0 (111.0-144.0) | 0.791 | 125.0 (106.0-145.0) | 128.5 (112.0-145.0) | 0.368 | 125.5 (102.0-144.8) | 123.0 (108.0-139.0) | 0.627 | ||
| Diastolic blood pressure, mmHg | 70.0 (62.0-80.0) | 70.0 (63.0-78.0) | 71.0 (66.0-81.0) | 0.112 | 68.0 (58.0-75.0) | 73.0 (64.0-82.8) | <0.001 | 69.5 (57.5-78.2) | 73.0 (64.0-86.0) | 0.026 | ||
| Heart rate, beats/min | 80.0 (70.0-91.0) | 78.0 (68.0-85.0) | 82.0 (73.0-98.0) | 0.002 | 74.0 (64.2-84.0) | 84.0 (73.0-96.0) | <0.001 | 80.0 (70.0-93.2) | 88.0 (77.5-103.0) | 0.001 | ||
| Killip classification | 0.025 | 0.171 | 0.003 | |||||||||
| Class I | 297 (43.9%) | 81 (52.6%) | 29 (34.1%) | 79 (55.6%) | 52 (45.6%) | 36 (40.9%) | 20 (21.3%) | |||||
| Class II | 213 (31.5%) | 50 (32.5%) | 36 (42.4%) | 41 (28.9%) | 32 (28.1%) | 28 (31.8%) | 26 (27.7%) | |||||
| Class III | 152 (22.5%) | 22 (14.3%) | 17 (20.0%) | 20 (14.1%) | 28 (24.6%) | 20 (22.7%) | 45 (47.9%) | |||||
| Class IV | 15 (2.2%) | 1 (0.6%) | 3 (3.5%) | 2 (1.4%) | 2 (1.8%) | 4 (4.5%) | 3 (3.2%) | |||||
| Total cholesterol, mmol/L | 4.0 (3.5-4.8) | 4.1 (3.6-4.9) | 4.0 (3.6-4.8) | 0.681 | 4.1 (3.5-4.8) | 4.1 (3.4-4.8) | 0.942 | 4.1 (3.4-4.9) | 3.9 (3.3-4.3) | 0.111 | ||
| LDL cholesterol, mmol/L | 2.3 (1.8-2.9) | 2.4 (1.9-3.0) | 2.4 (2.0-2.9) | 0.791 | 2.3 (1.8-2.9) | 2.3 (1.7-3.0) | 0.792 | 2.3 (1.8-2.9) | 2.1 (1.7-2.6) | 0.074 | ||
| Serum glucose, mmol/L | 7.5 (6.0-9.8) | 7.0 (5.7-9.8) | 7.6 (6.3-8.9) | 0.378 | 7.2 (6.0-8.9) | 7.7 (6.1-10.3) | 0.122 | 7.4 (6.2-10.2) | 7.9 (6.3-10.3) | 0.834 | ||
| Hemoglobin, g/L | 122.0 (109.0-133.0) | 122.0 (111.0-132.8) | 121.0 (109.0-138.0) | 0.801 | 123.0 (110.2-131.8) | 121.0 (109.0-133.0) | 0.856 | 118.5 (107.8-133.0) | 118.0 (102.2-131.8) | 0.379 | ||
| Serum creatinine, μmoI/L | 95.0 (76.0-125.0) | 87.0 (70.0-107.6) | 103.0 (82.0-125.0) | 0.003 | 88.0 (74.0-114.8) | 94.0 (75.0-123.0) | 0.210 | 103.5 (82.8-135.0) | 108.0 (87.2-175.0) | 0.199 | ||
| Peak troponin T, ng/L | 2,785.0 (929.6-5,857.0) | 2,255.5 (608.6-5,431.8) | 3,985.0 (915.0-7,299.0) | 0.028 | 3,012.0 (945.0-5,516.5) | 2,901.0 (1,162.5-6,170.0) | 0.472 | 2,709.0 (1,237.5-5,853.0) | 2,330.0 (1,020.8-5,384.2) | 0.568 | ||
| Peak NT-proBNP, ng/L | 5,208.0 (2,205.0-12,537.0) | 2,529.0 (1,286.0-6,464.2) | 7,555.5 (3,691.0-12,846.8) | <0.001 | 3,260.0 (1,449.0-5,970.0) | 8,229.5 (3,899.5-15,822.8) | <0.001 | 5,730.0 (2,285.5-12,215.5) | 13,268.0 (7,556.0-25,993.0) | <0.001 | ||
| Left ventricular ejection fraction, % | 52.0 (43.0-61.0) | 60.0 (55.0-64.0) | 44.0 (40.0-47.0) | <0.001 | 60.5 (56.0-65.0) | 42.5 (37.0-45.8) | <0.001 | 60.5 (55.0-65.2) | 39.0 (33.2-44.8) | <0.001 | ||
| Types of AMI | 0.973 | 0.223 | 0.621 | |||||||||
| STEMI | 400 (59.1%) | 87 (56.5%) | 49 (57.6%) | 88 (62.0%) | 78 (68.4%) | 48 (54.5%) | 50 (53.2%) | |||||
| NSTEMI | 262 (38.7%) | 62 (40.3%) | 33 (38.8%) | 52 (36.6%) | 32 (28.1%) | 40 (45.5%) | 43 (45.7%) | |||||
| Uncertain* | 15 (2.2%) | 5 (3.2%) | 3 (3.5%) | 2 (1.4%) | 4 (3.5%) | 0 (0.0%) | 1 (1.1%) | |||||
| Left main and/or three- vessel disease | 232 (34.3%) | 51 (33.1%) | 25 (29.4%) | 0.657 | 50 (35.2%) | 38 (33.3%) | 0.856 | 28 (31.8%) | 40 (42.6%) | 0.179 | ||
| PCI procedure | 494 (73.0%) | 118 (76.6%) | 62 (72.9%) | 0.635 | 115 (81.0%) | 86 (75.4%) | 0.357 | 56 (63.6%) | 57 (60.6%) | 0.792 | ||
| Number of stent implanted | 1.0 (1.0-2.0) | 1.0 (1.0-2.0) | 1.5 (1.0-2.0) | 0.550 | 1.0 (1.0-2.0) | 1.0 (1.0-2.0) | 0.983 | 1.0 (1.0-2.0) | 1.0 (1.0-2.0) | 0.899 | ||
| Aspirin | 588 (86.9%) | 145 (94.2%) | 73 (85.9%) | 0.013 | 130 (91.5%) | 98 (86.0%) | 0.363 | 68 (77.3%) | 74 (78.7%) | 0.892 | ||
| Clopidogrel | 593 (87.6%) | 142 (92.2%) | 76 (89.4%) | 0.362 | 131 (92.3%) | 93 (81.6%) | 0.033 | 72 (81.8%) | 79 (84.0%) | 0.804 | ||
| Ticagrelor | 17 (2.5%) | 2 (1.3%) | 0 (0.0%) | 0.433 | 3 (2.1%) | 8 (7.0%) | 0.119 | 2 (2.3%) | 2 (2.1%) | 0.955 | ||
| Statins | 595 (87.9%) | 141 (91.6%) | 76 (89.4%) | 0.464 | 126 (88.7%) | 98 (86.0%) | 0.731 | 73 (83.0%) | 81 (86.2%) | 0.674 | ||
| ACEIs or ARBs or ARNI | 271 (40.0%) | 65 (42.2%) | 32 (37.6%) | 0.562 | 61 (43.0%) | 48 (42.1%) | 0.793 | 30 (34.1%) | 35 (37.2%) | 0.848 | ||
| β-blocker | 334 (49.3%) | 89 (57.8%) | 54 (63.5%) | 0.578 | 65 (45.8%) | 53 (46.5%) | 0.774 | 31 (35.2%) | 42 (44.7%) | 0.376 | ||
| Spironolactone | 265 (39.1%) | 42 (27.3%) | 45 (52.9%) | <0.001 | 38 (26.8%) | 59 (51.8%) | <0.001 | 30 (34.1%) | 51 (54.3%) | 0.017 | ||
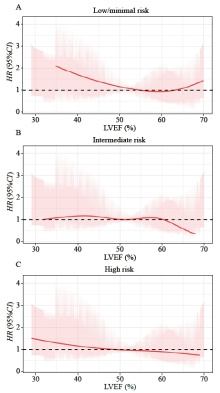
Figure 2.
Restricted cubic spline curves of the associations between LVEF and risk of all-cause death. A: low/minimal pressure injury risk; B: intermediate pressure injury risk; C: high pressure injury risk. LVEF: left ventricular ejection fraction; HR: hazard ratio; CI: confidence interval.

Table 2.
Crude and risk-adjusted hazard ratios of long-term all-cause death
| Pressure injury risk group | All-cause death, n (%) | Crude HR (95% CI), P-value | P for interaction | Adjusted HR* (95% CI), P-value | Adjusted P for interaction | |
|---|---|---|---|---|---|---|
| Preserved EF | Reduced EF | |||||
| < 0.001 | 0.003 | |||||
| Low/minimal risk (n=239) | 50/154 (32.5) | 36/85 (42.4) | 1.52 (0.99-2.33), P=0.058 | 1.29 (0.80-2.11), P=0.299 | ||
| Intermediate risk (n=256) | 33/142 (23.2) | 31/114 (27.2) | 1.23 (0.75-2.01), P=0.406 | 1.14 (0.65-2.02), P=0.651 | ||
| High risk (n=182) | 29/88 (33.0) | 47/94 (50) | 1.72 (1.08-2.73), P=0.022 | 1.81 (1.03-3.20), P=0.040 | ||
| [1] |
Hajhosseini B, Longaker MT, Gurtner GC. Pressure injury. Ann Surg. 2020; 271:671-9.
doi: 10.1097/SLA.0000000000003567 pmid: 31460882 |
| [2] |
Redelings MD, Lee NE, Sorvillo F. Pressure ulcers: more lethal than we thought? Adv Skin Wound Care. 2005; 18(7): 367-72.
doi: 10.1097/00129334-200509000-00010 pmid: 16160463 |
| [3] |
Cowan L, Broderick V, Alderden JG. Pressure injury prevention considerations for older adults. Crit Care Nurs Clin North Am. 2020; 32(4): 601-9.
doi: 10.1016/j.cnc.2020.08.009 |
| [4] |
Jaul E. Assessment and management of pressure ulcers in the elderly. Drugs Aging. 2010; 27(4): 311-25.
doi: 10.2165/11318340-000000000-00000 |
| [5] | Wassel CL, Delhougne G, Gayle JA, Dreyfus J, Larson B. Risk of readmissions, mortality, and hospital-acquired conditions across hospital-acquired pressure injury (HAPI) stages in a US National Hospital Discharge database. Int Wound J. 2020; 17(6): 1924-34. |
| [6] |
Song YP, Shen HW, Cai JY, Zha ML, Chen HL. The relationship between pressure injury complication and mortality risk of older patients in follow-up: a systematic review and meta-analysis. Int Wound J. 2019; 16(6): 1533-44.
doi: 10.1111/iwj.13243 |
| [7] |
Komici K, Vitale DF, Leosco D, Mancini A, Corbi G, Bencivenga L, et al. Pressure injuries in elderly with acute myocardial infarction. Clin Interv Aging. 2017; 12: 1495-501.
doi: 10.2147/CIA.S135676 pmid: 29033559 |
| [8] |
Silber H, Shiyovich A, Gilutz H, Ziedenberg H, Abu Tailakh M, Plakht Y. Decreased Norton’s functional score is an independent long-term prognostic marker in hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction II (SAMI-II) project. Int J Cardiol. 2017; 228: 694-9.
doi: S0167-5273(16)33570-7 pmid: 27886612 |
| [9] |
Bhatt AS, Ambrosy AP, Velazquez EJ. Adverse remodeling and reverse remodeling after myocardial infarction. Curr Cardiol Rep. 2017; 19(8): 71.
doi: 10.1007/s11886-017-0876-4 pmid: 28660552 |
| [10] |
Chew DS, Heikki H, Schmidt G, Kavanagh KM, Dommasch M, Bloch Thomsen PE, et al. Change in left ventricular ejection fraction following first myocardial infarction and outcome. JACC Clin Electrophysiol. 2018; 4(5): 672-82.
doi: 10.1016/j.jacep.2017.12.015 |
| [11] |
Chew DS, Wilton SB, Kavanagh K, Southern DA, Tan-Mesiatowsky LE, Exner DV, et al. Left ventricular ejection fraction reassessment post-myocardial infarction: current clinical practice and determinants of adverse remodeling. Am Heart J. 2018; 198: 91-6.
doi: S0002-8703(17)30381-2 pmid: 29653653 |
| [12] |
Romero J, Kahan J, Kelesidis I, Makani H, Wever-Pinzon O, Medina H, et al. CMR imaging for the evaluation of myocardial stunning after acute myocardial infarction: a meta-analysis of prospective trials. Eur Heart J Cardiovasc Imaging. 2013; 14(11): 1080-91.
doi: 10.1093/ehjci/jet040 pmid: 23575990 |
| [13] | Heusch G, Gersh BJ. The pathophysiology of acute myocardial infarction and strategies of protection beyond reperfusion: a continual challenge. Eur Heart J. 2016; 38(11): 774-84. |
| [14] |
Tripolt NJ, Kolesnik E, Pferschy PN, Verheyen N, Ablasser K, Sailer S, et al. Impact of EMpagliflozin on cardiac function and biomarkers of heart failure in patients with acute MYocardial infarction—the EMMY trial. Am Heart J. 2020; 221: 39-47.
doi: 10.1016/j.ahj.2019.12.004 |
| [15] |
De Luca L. Established and emerging pharmacological therapies for post-myocardial infarction patients with heart failure: a review of the evidence. Cardiovasc Drugs Ther. 2020; 34(5): 723-35.
doi: 10.1007/s10557-020-07027-4 pmid: 32564304 |
| [16] |
Wu WY, Biery DW, Singh A, Divakaran S, Berman AN, Ayuba G, et al. Recovery of left ventricular systolic function and clinical outcomes in young adults with myocardial infarction. J Am Coll Cardiol. 2020; 75(22): 2804-15.
doi: S0735-1097(20)34929-9 pmid: 32498808 |
| [17] | Brooks GC, Lee BK, Rao R, Lin F, Morin DP, Zweibel SL, et al. Predicting persistent left ventricular dysfunction following myocardial infarction. J Am Coll Cardiol. 2016; 67(10): 1186-96. |
| [18] |
Malebranche D, Hasan S, Fung M, Har B, Champagne P, Schnell G, et al. Patterns of left-ventricular function assessment in patients with acute coronary syndromes. CJC Open. 2021; 3(6): 733-40.
doi: 10.1016/j.cjco.2020.12.028 pmid: 34169252 |
| [19] |
Hall M, Dondo TB, Yan AT, Mamas MA, Timmis AD, Deanfield JE, et al. Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: latent class analysis of a nationwide population-based cohort. PLoS Med. 2018; 15(3): e1002501.
doi: 10.1371/journal.pmed.1002501 |
| [20] | He W, Goodkind D, Kowal P. An aging world: 2015 (International Population Reports, P95/16-1). Washington DC: U.S. Census Bureau, U.S. Government Publishing Office. 2016. |
| [21] |
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2018; 40(3): 237-69.
doi: 10.1093/eurheartj/ehy462 |
| [22] | Lupón J, Gavidia-Bovadilla G, Ferrer E, de Antonio M, Perera-Lluna A, López-Ayerbe J, et al. Heart failure with preserved ejection fraction infrequently evolves toward a reduced phenotype in long-term survivors. Circ Heart Fail. 2019; 12(3): e005652. |
| [23] |
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2015; 28(1): 1-39.e14.
doi: 10.1016/j.echo.2014.10.003 |
| [24] |
Ayello EA, Braden B. How and why to do pressure ulcer risk assessment. Adv Skin Wound Care. 2002; 15(3): 125-31;quiz132-33.
doi: 10.1097/00129334-200205000-00008 pmid: 12055446 |
| [25] |
Bandle B, Ward K, Min SJ, Drake C, McIlvennan CK, Kao D, et al. Can Braden score predict outcomes for hospitalized heart failure patients? J Am Geriatr Soc. 2017; 65(6): 1328-32.
doi: 10.1111/jgs.14801 pmid: 28221672 |
| [26] | Braden scale - for predicting pressure sore risk. Available at: https://www.in.gov/health/files/Braden_Scale.pdf |
| [27] | Braden BJ, Maklebust J. Preventing pressure ulcers with the Braden scale: an update on this easy-to-use tool that assesses a patient’s risk. Am J Nurs. 2005; 105(6): 70-2. |
| [28] |
Reinius P, Mellbin L, Holzmann MJ, Siddiqui AJ. Percutaneous coronary intervention versus conservative treatment for non ST-segment elevation myocardial infarction in patients above 80 years of age. Int J Cardiol. 2018; 267: 57-61.
doi: S0167-5273(17)37615-5 pmid: 29859705 |
| [29] |
de Belder A, Myat A, Blaxill J, Haworth P, O’Kane PD, Hatrick R, et al. Revascularisation or medical therapy in elderly patients with acute anginal syndromes: the RINCAL randomised trial. EuroIntervention. 2021; 17(1): 67-74.
doi: 10.4244/EIJ-D-20-00975 pmid: 33226000 |
| [30] |
Makam RP, Erskine N, Yarzebski J, Lessard D, Lau J, Allison J, et al. Decade long trends (2001-2011) in duration of pre-hospital delay among elderly patients hospitalized for an acute myocardial infarction. J Am Heart Assoc. 2016; 5(4): e002664.
doi: 10.1161/JAHA.115.002664 |
| [31] |
Ouellet GM, Geda M, Murphy TE, Tsang S, Tinetti ME, Chaudhry SI. Prehospital delay in older adults with acute myocardial infarction: the ComprehenSIVe evaluation of risk factors in older patients with acute myocardial infarction study. J Am Geriatr Soc. 2017; 65(11): 2391-6.
doi: 10.1111/jgs.15102 pmid: 29044463 |
| [32] |
Gupta A, Tsang S, Hajduk A, Krumholz HM, Nanna MG, Green P, et al. Presentation, treatment, and outcomes of the oldest-old patients with acute myocardial infarction: the SILVER-AMI study. Am J Med. 2021; 134(1): 95-103.
doi: 10.1016/j.amjmed.2020.07.020 pmid: 32805225 |
| [33] |
Richter D, Guasti L, Walker D, Lambrinou E, Lionis C, Abreu A, et al. Frailty in cardiology: definition, assessment and clinical implications for general cardiology. A consensus document of the Council for Cardiology Practice (CCP), Association for Acute Cardio Vascular Care (ACVC), Association of Cardiovascular Nursing and Allied Professions (ACNAP), European Association of Preventive Cardiology (EAPC), European Heart Rhythm Association (EHRA), Council on Valvular Heart Diseases (VHD), Council on Hypertension (CHT), Council of Cardio-Oncology (CCO), Working Group (WG) Aorta and Peripheral Vascular Diseases, WG e-Cardiology, WG Thrombosis, of the European Society of Cardiology, European Primary Care Cardiology Society (EPCCS). Eur J Prev Cardiol. 2022; 29:216-227.
doi: 10.1093/eurjpc/zwaa167 |
| [34] | Kochar A, Chen AY, Sharma PP, Pagidipati NJ, Fonarow GC, Cowper PA, et al. Long-term mortality of older patients with acute myocardial infarction treated in US clinical practice. J Am Heart Assoc. 2018; 7(13): e007230. |
| [35] |
Sawant AC, Josey K, Plomondon ME, Maddox TM, Bhardwaj A, Singh V, et al. Temporal trends, complications, and predictors of outcomes among nonagenarians undergoing percutaneous coronary intervention. JACC Cardiovasc Interv. 2017; 10(13): 1295-303.
doi: 10.1016/j.jcin.2017.03.051 |
| [36] |
Bromage DI, Jones DA, Rathod KS, Grout C, Iqbal MB, Lim P, et al. Outcome of 1051 octogenarian patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: observational cohort from the London heart attack group. J Am Heart Assoc. 2016; 5(6): e003027.
doi: 10.1161/JAHA.115.003027 |
| [37] |
Phan DQ, Rostomian AH, Schweis F, Chung J, Lin B, Zadegan R, et al. Revascularization versus medical therapy in patients aged 80 years and older with acute myocardial infarction. J Am Geriatr Soc. 2020; 68(11): 2525-33.
doi: 10.1111/jgs.16747 |
| [38] |
Kumar S, McDaniel M, Samady H, Forouzandeh F. Contemporary revascularization dilemmas in older adults. J Am Heart Assoc. 2020; 9(3): e014477.
doi: 10.1161/JAHA.119.014477 |
| [39] |
Damluji AA, Huang J, Bandeen-Roche K, Forman DE, Gerstenblith G, Moscucci M, et al. Frailty among older adults with acute myocardial infarction and outcomes from percutaneous coronary interventions. J Am Heart Assoc. 2019; 8(17): e013686.
doi: 10.1161/JAHA.119.013686 |
| [40] | Sanchis J, Ariza-Solé A, Abu-Assi E, Alegre O, Alfonso F, Barrabés JA, et al. Invasive versus conservative strategy in frail patients with NSTEMI: the MOSCA-FRAIL clinical trial study design. Rev Esp Cardiol (Engl Ed). 2019;72(2): 154-9. |
| [41] |
Mele D, Nardozza M, Ferrari R. Left ventricular ejection fraction and heart failure: an indissoluble marriage? Eur J Heart Fail. 2018; 20(3): 427-30.
doi: 10.1002/ejhf.1071 pmid: 29314500 |
| [42] |
Hall TS, von Lueder TG, Zannad F, Rossignol P, Duarte K, Chouihed T, et al. Relationship between left ventricular ejection fraction and mortality after myocardial infarction complicated by heart failure or left ventricular dysfunction. Int J Cardiol. 2018; 272: 260-6.
doi: S0167-5273(18)30005-6 pmid: 30144995 |
| [43] |
Hall TS, von Lueder TG, Zannad F, Rossignol P, Duarte K, Chouihed T, et al. Left ventricular ejection fraction and adjudicated, cause-specific hospitalizations after myocardial infarction complicated by heart failure or left ventricular dysfunction. Am Heart J. 2019; 215: 83-90.
doi: S0002-8703(19)30149-8 pmid: 31291604 |
| [44] |
Siontis GC, Branca M, Serruys P, Silber S, Räber L, Pilgrim T, et al. Impact of left ventricular function on clinical outcomes among patients with coronary artery disease. Eur J Prev Cardiol. 2019; 26:1273-84.
doi: 10.1177/2047487319841939 pmid: 30966820 |
| [45] | Jenča D, Melenovský V, Stehlik J, Staněk V, Kettner J, Kautzner J, et al. Heart failure after myocardial infarction: incidence and predictors. ESC Heart Fail. 2021;8:222-37. |
| [46] |
Yan YL, Liu B, Du J, Wang J, Jing XD, Liu YJ, et al. SGLT2i versus ARNI in heart failure with reduced ejection fraction: a systematic review and meta-analysis. ESC Heart Fail. 2021; 8(3): 2210-9.
doi: 10.1002/ehf2.13313 pmid: 33749159 |
| [47] |
Dunlay SM, Chamberlain AM. Multimorbidity in older patients with cardiovascular disease. Curr Cardiovasc Risk Rep. 2016; 10: 3.
doi: 10.1007/s12170-016-0491-8 |
| [48] |
Vilela EM, Ladeiras Lopes R, Torres S, João A, Ribeiro J, Primo J, et al. Differential impact of a cardiac rehabilitation program on functional parameters in elderly versus non-elderly myocardial infarction survivors. Cardiology. 2020; 145(2): 98-105.
doi: 10.1159/000504875 pmid: 31838463 |
| [49] |
Yoshioka N, Takagi K, Morishima I, Morita Y, Uemura Y, Inoue Y, et al. Influence of preadmission frailty on short- and mid-term prognoses in octogenarians with ST-elevation myocardial infarction. Circ J. 2019; 84(1): 109-18.
doi: 10.1253/circj.CJ-19-0467 pmid: 31787661 |
| [50] |
Sundaram V, Rothnie K, Bloom C, Zakeri R, Sahadevan J, Singh A, et al. Impact of comorbidities on peak troponin levels and mortality in acute myocardial infarction. Heart 2020; 106(9): 677-85.
doi: 10.1136/heartjnl-2019-315844 pmid: 32102896 |
| [51] |
Jaul E, Barron J, Rosenzweig JP, Menczel J. An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr. 2018; 18(1): 305.
doi: 10.1186/s12877-018-0997-7 pmid: 30537947 |
| [52] |
Perneger TV, Héliot C, Raë AC, Borst F, Gaspoz JM. Hospital-acquired pressure ulcers: risk factors and use of preventive devices. Arch Intern Med. 1998; 158 (17): 1940-5
doi: 10.1001/archinte.158.17.1940 pmid: 9759692 |
| [53] |
Wehner GJ, Jing LY, Haggerty CM, Suever JD, Leader JB, Hartzel DN, et al. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie? Eur Heart J. 2019; 41(12): 1249-57.
doi: 10.1093/eurheartj/ehz550 |
| [54] |
Adamo M, Gardner RS, McDonagh TA, Metra M. The ‘Ten Commandments’ of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 43(6): 440-1.
doi: 10.1093/eurheartj/ehab853 |
| [55] |
Gevaert AB, Tibebu S, Mamas MA, Ravindra NG, Lee SF, Ahmad T, et al. Clinical phenogroups are more effective than left ventricular ejection fraction categories in stratifying heart failure outcomes. ESC Heart Fail. 2021; 8(4): 2741-54.
doi: 10.1002/ehf2.13344 pmid: 33934542 |
| [56] |
Kaura A, Sterne JAC, Trickey A, Abbott S, Mulla A, Glampson B, et al. Invasive versus non-invasive management of older patients with non-ST elevation myocardial infarction (SENIOR-NSTEMI): a cohort study based on routine clinical data. Lancet. 2020; 396(10251): 623-34.
doi: S0140-6736(20)30930-2 pmid: 32861307 |
| [57] |
Nishihira K, Watanabe N, Kuriyama N, Shibata Y. Clinical outcomes of nonagenarians with acute myocardial infarction who undergo percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care. 2020; 9(5): 488-95.
doi: 10.1177/2048872620921596 |
| [58] | Barry M, Nugent L. Pressure ulcer prevention in frail older people. Nurs Stand. 2015; 30(16): 50-8. |
| [59] |
Walker DM, Gale CP, Lip G, Martin-Sanchez FJ, McIntyre HF, Mueller C, et al. Editor’s Choice - Frailty and the management of patients with acute cardiovascular disease: a position paper from the Acute Cardiovascular Care Association. Eur Heart J Acute Cardiovasc Care. 2018; 7(2): 176-93.
doi: 10.1177/2048872618758931 pmid: 29451402 |
| [1] | Guang-mei Wang, Yong Li, Shuo Wu, Wen Zheng, Jing-jing Ma, Feng Xu, Jia-qi Zheng, He Zhang, Jia-li Wang, Yu-guo Chen. The combination of creatine kinase-myocardial band isoenzyme and point-of-care cardiac troponin/ contemporary cardiac troponin for the early diagnosis of acute myocardial infarction [J]. World Journal of Emergency Medicine, 2022, 13(3): 163-168. |
| [2] | Wei-xian Xu, Yuan-yuan Fan, Yao Song, Xin Liu, Hui Liu, Li-jun Guo. Prognostic differences of catestatin among young and elderly patients with acute myocardial infarction [J]. World Journal of Emergency Medicine, 2022, 13(3): 169-174. |
| [3] | Qian-lin Gu, Peng Jiang, Hui-fen Ruan, Hao Tang, Yang-bing Liang, Zhong-fu Ma, Hong Zhan. The expression of oxidative stress genes related to myocardial ischemia reperfusion injury in patients with ST-elevation myocardial infarction [J]. World Journal of Emergency Medicine, 2022, 13(2): 106-113. |
| [4] | Li Li, Jun Yan, Lin-qin Ma, Wei Bi, Cai-jun Wu. Effects of Maxingloushi decoction on immune inflammation and programmed death markers in mice with chronic obstructive pulmonary disease [J]. World Journal of Emergency Medicine, 2022, 13(1): 40-45. |
| [5] | Tian Xu, Ya Li, Li-ding Zhao, Guo-sheng Fu, Wen-bin Zhang. Predictors of recurrent angina in patients with no need for secondary revascularization [J]. World Journal of Emergency Medicine, 2021, 12(1): 42-47. |
| [6] | Chuan-qi Ding, Yu-ping Zhang, Yu-wei Wang, Min-fei Yang, Sa Wang, Nian-qi Cui, Jing-fen Jin. Death and do-not-resuscitate order in the emergency department: A single-center three-year retrospective study in the Chinese mainland [J]. World Journal of Emergency Medicine, 2020, 11(4): 231-237. |
| [7] | Guo-xiong Chen, Hong-na Wang, Jin-lin Zou, Xiao-xu Yuan. Effects of intracoronary injection of nicorandil and tirofiban on myocardial perfusion and short-term prognosis in elderly patients with acute ST-segment elevation myocardial infarction after emergency PCI [J]. World Journal of Emergency Medicine, 2020, 11(3): 157-163. |
| [8] | Jun Jiang, Nai-liang Tian, Han-bin Cui, Chang-ling Li, Xian-bao Liu, Liang Dong, Yong Sun, Xiao-min Chen, Shao-liang Chen, Bo Xu, Jian-an Wang. Post-dilatation improves stent apposition in patients with ST-segment elevation myocardial infarction receiving primary percutaneous intervention: A multicenter, randomized controlled trial using optical coherence tomography [J]. World Journal of Emergency Medicine, 2020, 11(2): 87-92. |
| [9] | Hong-yi Wu, Ju-ying Qian, Qi-bing Wang, Jun-bo Ge. An unexpected electrocardiogram sign of subacute left ventricular free wall rupture: Its early awareness may be lifesaving [J]. World Journal of Emergency Medicine, 2020, 11(2): 117-119. |
| [10] | Changiz Gholipour, Bahram Samadi Rad, Samad Shams Vahdati, Amir Ghaffarzad, Armita Masoud. Evaluation of preventable trauma death in emergency department of Imam Reza hospital [J]. World Journal of Emergency Medicine, 2016, 7(2): 135-137. |
| [11] | Audrey L. Blewer, David G. Buckler, Jiaqi Li, Marion Leary, Lance B. Becker, Judy A. Shea, Peter W. Groeneveld, Mary E. Putt, Benjamin S. Abella. Impact of the 2010 resuscitation guidelines training on layperson chest compressions [J]. World Journal of Emergency Medicine, 2015, 6(4): 270-276. |
| [12] | Andrew Fu Wah Ho, Pin Pin Pek, Stephanie Fook-Chong, Ting Hway Wong, Yih Yng Ng, Aaron Sung Lung Wong, Marcus Eng Hock Ong. Prehospital system delay in patients with ST-segment elevation myocardial infarction in Singapore [J]. World Journal of Emergency Medicine, 2015, 6(4): 277-282. |
| [13] | Li-ming Li, Wen-bo Cai, Qin Ye, Jian-min Liu, Xin Li, Xiao-xing Liao. Comparison of plasma microRNA-1 and cardiac troponin T in early diagnosis of patients with acute myocardial infarction [J]. World Journal of Emergency Medicine, 2014, 5(3): 182-186. |
| [14] | Hua Zhou, Xiao-yan He, Shao-wei Zhuang, Juan Wang, Yan Lai, Wei-gang Qi, Yi-an Yao, Xue-bo Liu. Clinical and procedural predictors of no-reflow in patients with acute myocardial infarction after primary percutaneous coronary intervention [J]. World Journal of Emergency Medicine, 2014, 5(2): 96-102. |
| [15] | Ya Zhong, Ping Cao, Chuan-feng Tong, Xia Li. Effects of ramipril on ventricular arrhythmia after myocardial infarction in rabbits [J]. World Journal of Emergency Medicine, 2014, 5(2): 135-138. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
