World Journal of Emergency Medicine ›› 2022, Vol. 13 ›› Issue (2): 106-113.doi: 10.5847/wjem.j.1920-8642.2022.021
• Original Articles • Previous Articles Next Articles
Qian-lin Gu1, Peng Jiang1, Hui-fen Ruan2, Hao Tang1, Yang-bing Liang1, Zhong-fu Ma1, Hong Zhan1( )
)
Received:2020-06-09
Accepted:2020-12-20
Online:2021-11-19
Published:2022-03-01
Contact:
Hong Zhan
E-mail:zhanhong81@126.com
Qian-lin Gu, Peng Jiang, Hui-fen Ruan, Hao Tang, Yang-bing Liang, Zhong-fu Ma, Hong Zhan. The expression of oxidative stress genes related to myocardial ischemia reperfusion injury in patients with ST-elevation myocardial infarction[J]. World Journal of Emergency Medicine, 2022, 13(2): 106-113.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2022.021
Table 1
Comparison of clinical data between the control and AMI (STEMI type) groups
| Variables | Control group (n=10) | AMI group (n=11) |
|---|---|---|
| Age (years) | 53.00±6.55 | 61.44±13.70 |
| Sex (male/female) | 7/3 | 7/4 |
| WBC (×109/L) | 6.41±0.72 | 11.67±4.85# |
| N (×109/L) | 3.89±0.81 | 9.27±4.75# |
| L (×109/L) | 1.86±0.44 | 1.56±0.52 |
| M (×109/L) | 0.74±0.37 | 0.30±0.07# |
| CK-MB (U/L) | 10.62±6.01 | 96.20±116.22 |
| T-AOC (U/mL) | 12.80±1.79 | 20.48±2.55 |
Table 2
Genes significantly differentially expressed in the AMI group compared with the control group
| Gene symbol | Description | Up/Down | Fold change | P-value |
|---|---|---|---|---|
| TNFSF6 | Tumor necrosis factor (ligand) superfamily, member 6 | Up | 2.100 | 0.003 |
| TRADD | TNFRSF1A-associated via death | Up | 2.090 | 0.008 |
| DNAJB1 | DNAJ (Hsp40) homolog, subfamily B, member 1 | Up | 3.390 | 0.008 |
| DNAJB2 | DNAJ (Hsp40) homolog, subfamily B, member 2 | Up | 3.230 | 0.008 |
| GADD45A | Growth arrest and DNA-damage-inducible, alpha | Up | 2.030 | 0.004 |
| HSPD1 | Heat shock 60 kDa protein 1 (chaperonin) | Up | 2.040 | 0.005 |
| PRDX2 | Peroxiredoxin 2 | Up | 2.000 | 0.008 |
| RAD50 | RAD50 homolog (S. cerevisiae) | Up | 2.140 | 0.008 |
| CYP1A1 | Cytochrome P450, family 1, subfamily A, polypeptide 1 | Down | 0.421 | 0.009 |
| CCNG1 | Cyclin G1 | Down | 0.281 | 0.009 |
| CAT | Catalase | Down | 0.408 | 0.011 |
| ATM | Ataxia telangiectasia mutated (includes complementation groups A, C, and D) | Down | 0.156 | 0.013 |

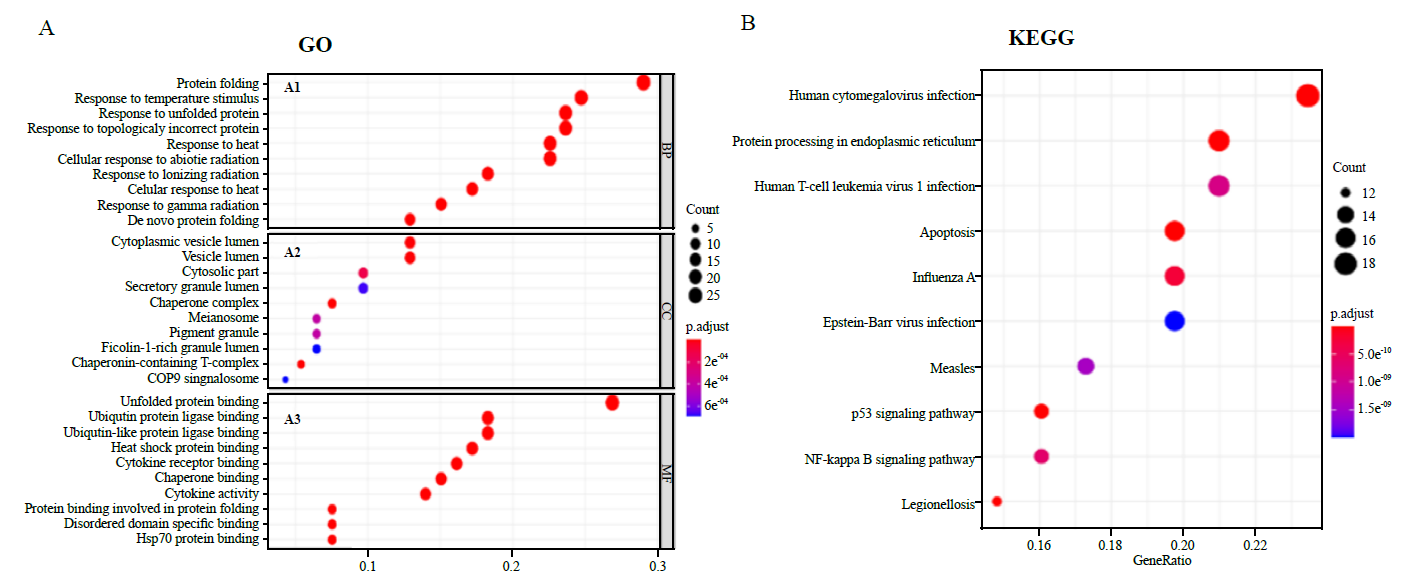
Figure 2.
Enrichment analysis of oxidative stress genes related to MIRI. A1-3 and B: the enrichment analysis results of genes, namely biological processes, cellular components, molecular functions, and KEGG respectively. The main 10 results of each term are shown, and the color indicates the significant degree of enrichment and the size indicates the number of genes enriched for each result. GO: gene ontology; KEGG: kyoto encyclopedia of genes and genomes.
| 1 | Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020; 141(9):e139-596. |
| 2 |
Arslan F, Bongartz L, Ten Berg JM, Jukema JW, Appelman Y, Liem AH, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: comments from the Dutch ACS working group. Neth Heart J. 2018; 26(9):417-21.
doi: 10.1007/s12471-018-1134-0 pmid: 29974355 |
| 3 |
Kalogeris T, Bao Y, Korthuis RJ. Mitochondrial reactive oxygen species: a double edged sword in ischemia/reperfusion vs preconditioning. Redox Biol. 2014; 2:702-14.
doi: 10.1016/j.redox.2014.05.006 pmid: 24944913 |
| 4 |
Buja LM. Myocardial ischemia and reperfusion injury. Cardiovasc Pathol. 2005; 14(4):170-5.
doi: 10.1016/j.carpath.2005.03.006 |
| 5 |
Freude B, Masters TN, Robicsek F, Fokin A, Kostin S, Zimmermann R, et al. Apoptosis is initiated by myocardial ischemia and executed during reperfusion. J Mol Cell Cardiol. 2000; 32(2):197-208.
pmid: 10722797 |
| 6 |
Chouchani ET, Pell VR, Gaude E, Aksentijević D, Sundier SY, Robb EL, et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature. 2014; 515(7527):431-5.
doi: 10.1038/nature13909 |
| 7 |
Kurian GA, Rajagopal R, Vedantham S, Rajesh M. The role of oxidative stress in myocardial ischemia and reperfusion injury and remodeling: revisited. Oxid Med Cell Longev. 2016; 2016:1656450.
doi: 10.1155/2016/1656450 pmid: 27313825 |
| 8 |
Marczin N, El-Habashi N, Hoare GS, Bundy RE, Yacoub M. Antioxidants in myocardial ischemia-reperfusion injury: therapeutic potential and basic mechanisms. Arch Biochem Biophys. 2003; 420(2):222-36.
pmid: 14654061 |
| 9 |
Dhalla NS, Elmoselhi AB, Hata T, Makino N. Status of myocardial antioxidants in ischemia-reperfusion injury. Cardiovasc Res. 2000; 47(3):446-56.
pmid: 10963718 |
| 10 |
Weiss JN, Korge P, Honda HM, Ping PP. Role of the mitochondrial permeability transition in myocardial disease. Circ Res. 2003; 93(4):292-301.
doi: 10.1161/01.RES.0000087542.26971.D4 |
| 11 |
Morciano G, Giorgi C, Bonora M, Punzetti S, Pavasini R, Wieckowski MR, et al. Molecular identity of the mitochondrial permeability transition pore and its role in ischemia-reperfusion injury. J Mol Cell Cardiol. 2015; 78:142-53.
doi: 10.1016/j.yjmcc.2014.08.015 |
| 12 |
Letavernier E, Zafrani L, Perez J, Letavernier B, Haymann JP, Baud L. The role of calpains in myocardial remodelling and heart failure. Cardiovasc Res. 2012; 96(1):38-45.
doi: 10.1093/cvr/cvs099 pmid: 22425901 |
| 13 |
Inserte J, Hernando V, Garcia-Dorado D. Contribution of calpains to myocardial ischaemia/reperfusion injury. Cardiovasc Res. 2012; 96(1):23-31.
doi: 10.1093/cvr/cvs232 pmid: 22787134 |
| 14 |
McCafferty K, Forbes S, Thiemermann C, Yaqoob MM. The challenge of translating ischemic conditioning from animal models to humans: the role of comorbidities. Dis Model Mech. 2014; 7(12):1321-33.
doi: 10.1242/dmm.016741 pmid: 25481012 |
| 15 |
Benzie IF, Strain JJ. The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: the FRAP assay. Anal Biochem. 1996; 239(1):70-6.
pmid: 8660627 |
| 16 | Hoffman JW Jr, Gilbert TB, Poston RS, Silldorff EP. Myocardial reperfusion injury: etiology, mechanisms, and therapies. J Extra Corpor Technol. 2004; 36(4):391-411. |
| 17 |
Romson JL, Hook BG, Kunkel SL, Abrams GD, Schork MA, Lucchesi BR. Reduction of the extent of ischemic myocardial injury by neutrophil depletion in the dog. Circulation. 1983; 67(5):1016-23.
pmid: 6831665 |
| 18 |
Granfeldt A, Jiang R, Wang NP, Mykytenko J, Eldaif S, Deneve J, et al. Neutrophil inhibition contributes to cardioprotection by postconditioning. Acta Anaesthesiol Scand. 2012; 56(1):48-56.
doi: 10.1111/j.1399-6576.2011.02577.x pmid: 22103673 |
| 19 |
Shimizu T, Suzuki S, Sato A, Nakamura Y, Ikeda K, Saitoh S, et al. Cardio-protective effects of pentraxin 3 produced from bone marrow-derived cells against ischemia/reperfusion injury. J Mol Cell Cardiol. 2015; 89(Pt B):306-13.
doi: 10.1016/j.yjmcc.2015.10.013 |
| 20 | Santos-Junior VA, Lollo PCB, Cantero MA, Moura CS, Amaya-Farfan J, Morato PN. Heat shock proteins: protection and potential biomarkers for ischemic injury of cardiomyocytes after surgery. Braz J Cardiovasc Surg. 2018; 33(3):291-302. |
| 21 |
Chess PR, O’Reilly MA, Sachs F, Finkelstein JN. Reactive oxidant and p42/44 MAP kinase signaling is necessary for mechanical strain-induced proliferation in pulmonary epithelial cells. J Appl Physiol (1985). 2005; 99(3):1226-32.
doi: 10.1152/japplphysiol.01105.2004 |
| 22 |
Stegall MD, Park WD, Kim DY, Covarrubias M, Khair A, Kremers WK. Changes in intragraft gene expression secondary to ischemia reperfusion after cardiac transplantation. Transplantation. 2002; 74(7):924-30.
pmid: 12394832 |
| 23 |
Jeremias I, Kupatt C, Martin-Villalba A, Habazettl H, Schenkel J, Boekstegers P, et al. Involvement of CD95/Apo1/Fas in cell death after myocardial ischemia. Circulation. 2000; 102(8):915-20.
pmid: 10952962 |
| 24 |
Zhang L, Zhang L, Li YH, Zhang HY, Chen ML, Gao MM, et al. High-dose glucose-insulin-potassium treatment reduces myocardial apoptosis in patients with acute myocardial infarction. Eur J Clin Invest. 2005; 35(3):164-70.
pmid: 15733070 |
| 25 |
Hou J, Fu J, Li D, Han X, Li L, Song W, et al. Transcriptomic analysis of myocardial ischemia using the blood of rat. PLoS One. 2015; 10(11):e0141915.
doi: 10.1371/journal.pone.0141915 |
| 26 | Amodio G, Moltedo O, Faraonio R, Remondelli P. Targeting the endoplasmic Reticulum unfolded protein response to counteract the oxidative stress-induced endothelial dysfunction. Oxid Med Cell Longev. 2018; 2018:4946289. |
| 27 |
Csordás G, Renken C, Várnai P, Walter L, Weaver D, Buttle KF, et al. Structural and functional features and significance of the physical linkage between ER and mitochondria. J Cell Biol. 2006; 174(7):915-21.
pmid: 16982799 |
| 28 |
Verfaillie T, Rubio N, Garg AD, Bultynck G, Rizzuto R, Decuypere JP, et al. PERK is required at the ER-mitochondrial contact sites to convey apoptosis after ROS-based ER stress. Cell Death Differ. 2012; 19(11):1880-91.
doi: 10.1038/cdd.2012.74 pmid: 22705852 |
| [1] | Ji-yang Ling, Chun-sheng Li, Yun Zhang, Xiao-li Yuan, Bo Liu, Yong Liang, Qiang Zhang. Protective effect of extracorporeal membrane pulmonary oxygenation combined with cardiopulmonary resuscitation on post-resuscitation lung injury [J]. World Journal of Emergency Medicine, 2021, 12(4): 303-308. |
| [2] | Shuang-shuang Gu, Xiu-wen Kang, Jun Wang, Xiao-fang Guo, Hao Sun, Lei Jiang, Jin-song Zhang. Effects of extracellular vesicles from mesenchymal stem cells on oxygen-glucose deprivation/reperfusion-induced neuronal injury [J]. World Journal of Emergency Medicine, 2021, 12(1): 61-67. |
| [3] | Li-ming Li, Wen-bo Cai, Qin Ye, Jian-min Liu, Xin Li, Xiao-xing Liao. Comparison of plasma microRNA-1 and cardiac troponin T in early diagnosis of patients with acute myocardial infarction [J]. World Journal of Emergency Medicine, 2014, 5(3): 182-186. |
| [4] | Hua Zhou, Xiao-yan He, Shao-wei Zhuang, Juan Wang, Yan Lai, Wei-gang Qi, Yi-an Yao, Xue-bo Liu. Clinical and procedural predictors of no-reflow in patients with acute myocardial infarction after primary percutaneous coronary intervention [J]. World Journal of Emergency Medicine, 2014, 5(2): 96-102. |
| [5] | Li-li Ji, Xiao-feng Long, Hui Tian, Yu-fei Liu. Effect of transplantation of bone marrow stem cells on myocardial infarction size in a rabbit model [J]. World Journal of Emergency Medicine, 2013, 4(4): 304-310. |
| [6] | Xiao-xiao Meng, Rui-lan Wang, Shan Gao, Hui Xie, Jiu-ting Tan, Yong-bin Qian. Effect of ulinastatin on paraquat-induced-oxidative stress in human type II alveolar epithelial cells [J]. World Journal of Emergency Medicine, 2013, 4(2): 133-137. |
| [7] | Yan Chen, Wei Yang, Gan-nan Wang, Jun Li, Xiao-rong Li, Jian Zhang, Wei Yuan, Dao-wu Wang, Jin-song Zhang, Ke-jiang Cao. Circulating microRNAs, novel biomarkers of acute myocardial infarction: a systemic review [J]. World Journal of Emergency Medicine, 2012, 3(4): 257-260. |
| [8] | Hui-li Zhang, Yuan-fei Liu, Xu-rui Luo, Wei-hua Tan, Liang Huang. Saturated hydrogen saline protects rats from acute lung injury induced by paraquat [J]. World Journal of Emergency Medicine, 2011, 2(2): 149-153. |
| [9] | Xiao-dong Liu, Chun-lei Sun, Su-ping Mu, Xiao-mei Qiu, Hai-ying Yu. Acute myocardial infarction in a child with myocardial bridge [J]. World Journal of Emergency Medicine, 2011, 2(1): 70-72. |
| [10] | Yu Chen, Zhi-jian Chen, Yu-hua Liao, Zhe Cao, Jia-ding Xia, Hua Yang, Yi-mei Du. Effect of tumor necrosis factor-α on ventricular arrhythmias in rats with acute myocardial infarction in vivo [J]. World Journal of Emergency Medicine, 2010, 1(1): 53-58. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
