Despite efforts to develop treatment technology for cardiac arrest (CA), CA incidence and mortality rates are still high.[1,2] A recent study of CA patients in emergency departments revealed that the incidence of CA is increasing annually, and the in-hospital survival rate of CA patients is only approximately 28.7%.[3] Echocardiography has been widely used as an important monitoring tool in critical care and helps to identify the cause of shock, monitor hemodynamics, and guide fluid therapy utilization.[4] One study reported that approximately one-third of patients underwent formal echocardiography during hospitalization in the intensive care unit (ICU).[5]
However, the clinical value of echocardiography in the management of CA patients has not been confirmed, especially in critically ill patients. Therefore, this study aimed to investigate the association between the use of echocardiography and the prognosis of hospitalized CA patients in the ICU.
This was a retrospective study based on data from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database, which was developed and maintained by the Laboratory for Computational Physiology at the Massachusetts Institute of Technology with ethical approval.[6]
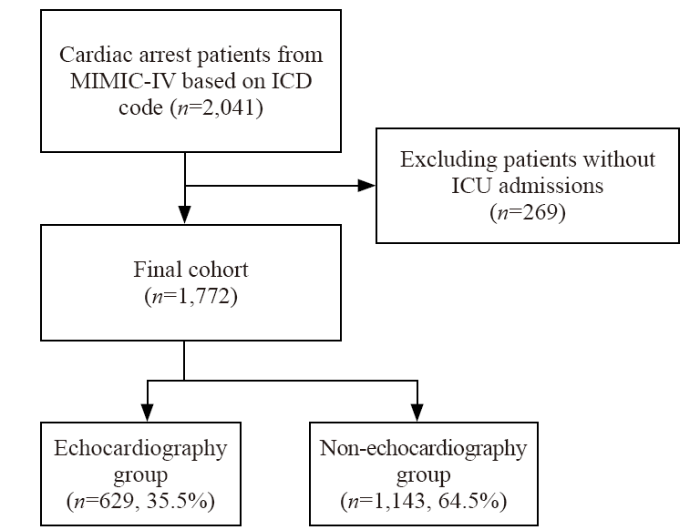
Patients meeting the following criteria were included in our study: (1) records of admission to the ICU; (2) aged over 18 years at the time of first admission; (3) diagnosed with CA according to the International Classification of Diseases, 9th and 10th Revision (427.5 [cardiac arrest] for the 9th Revision, and I46 [cardiac arrest], I46.2 [cardiac arrest due to underlying cardiac condition], I46.8 [cardiac arrest due to other underlying condition], and I46.9 [cardiac arrest, cause unspecified] for the 10th Revision). A total of 2,041 adult patients in the MIMIC-IV were diagnosed with CA. A total of 1,772 patients were admitted to the ICU and were eligible for inclusion in the subsequent analysis. In the final sample, a total of 629 patients (35.5% of the included patients) underwent echocardiography examination and composed the echocardiography group, whereas the remaining 1,143 patients who did not undergo echocardiography composed the non-echocardiography group. The generation process of the final research cohort is shown in Figure 1.
Figure 1.
Figure 1.
Research cohort. MIMIC-IV: Medical Information Mart for Intensive Care IV; ICD: International Classification of Diseases; ICU: intensive care unit.
We first performed a descriptive statistical analysis on the basic characteristics of patients in the two groups to investigate potential factors influencing patient prognosis. The factors included patient sex, weight, height, the highest and lowest values of vital signs, and arterial lactate during the first 24 h after admission to the ICU. In addition, indexes including the Glasgow Coma Scale (GCS) and Sequential Organ Failure Assessment (SOFA) scores during the first 24 h after admission to the ICU, and the age-adjusted Charlson Comorbidity Index (CCI) calculated based on the patient’s age and ICD-9 or ICD-10 codes, were included. We also considered whether the patients experienced sepsis during hospitalization. Additionally, mechanical ventilation and the use of vasoactive drugs (dopamine, norepinephrine and vasopressin) were also considered predictive factors.
The primary outcome was in-hospital death of CA patients admitted to the ICU. The secondary outcome was the patient's survival period within 28 d after entering the ICU.
For descriptive statistical analysis, categorical variables are presented as frequencies and percentages, and were compared between the echocardiography group and the non-echocardiography group via the Pearson Chi-square test or Fisher’s exact test. For continuous variables, the Shapiro-Wilk test was used to test whether the variables conformed to a normal distribution. The descriptive statistics are presented as the mean with standard deviation (SD) if the variables conformed to a normal distribution. Otherwise, the data are presented as the median and interquartile range (IQR). Comparisons between the echocardiography and non-echocardiography groups were performed with Student’s t test for variables conforming to a normal distribution and the Mann-Whitney U test for variables conforming to a nonnormal distribution.
For missing data in the database for the aforementioned statistical analyses, we adopted a multiple imputation method called predictive mean matching (PMM) to form the missing values and improve the overall quality of the dataset.
The supplementary Table 1 presents the descriptive statistical results of the patients included in the analysis of the original cohort. There were significant differences in several predictive factors between the echocardiography and non-echocardiography groups, implying that there could be concerns due to differences in the personal characteristics of the patients in the two groups, which can interfere with the use of echocardiography. To perform the propensity score matching (PSM) model, the Logistic regression was firstly used to calculate the probability of each patient’s receiving echocardiography as the propensity score for them to receive the treatment of echocardiography. Subsequently, the study used the closest matching method, setting the maximum propensity score difference as the 0.2 standard deviation of propensity scores, and matched the patients between the subsamples of those receiving echocardiography and those not receiving echocardiography at a ratio of 1:1. After the matching process, a total of 604 pairs of patients (1,208 patients) were successfully retained. Table 1 shows the descriptive statistics for the matched study cohort composed of the 1,208 patients. There was no significant difference in the distribution of covariates between the echocardiography group and the non-echocardiography group after matching, as measured by both P and standard mean difference (SMD) values, indicating good balance. Similar results can also be observed for the distributions of the SMDs of the variables shown in supplementary Figure 1.
Table 1. Characteristics of patients in the matched cohorts (weighted)
| Covariates | Echocardiography group (n=604) | Non-echocardiography group (n=604) | P-value | SMD-weighted |
|---|---|---|---|---|
| Basic characteristics | ||||
| Age, years | 63.89±16.73 | 62.70±16.34 | 0.839 | 0.001 |
| Female sex | 231 (38.2) | 224 (37.1) | 0.678 | 0.005 |
| BMI, kg/m2 | 29.08±7.48 | 28.98±7.48 | 0.82 | 0.007 |
| Admission location | 309 (51.2) | 313 (51.8) | 0.818 | 0.001 |
| Diagnosis (ICD-10 code=I462) | 49 (8.1) | 59 (9.8) | 0.313 | 0.005 |
| Vital signs | ||||
| HR, min, beats/min | 67.40±18.79 | 67.01±18.38 | 0.716 | 0.004 |
| HR, max, beats/min | 108.47±25.40 | 108.35±24.78 | 0.934 | 0.011 |
| SBP, min, mmHg | 80.86±19.24 | 80.15±21.40 | 0.544 | 0.007 |
| SBP, max, mmHg | 151.92±29.15 | 152.19±28.37 | 0.871 | 0.001 |
| DBP, min, mmHg | 42.48±13.13 | 42.28±13.55 | 0.787 | 0.005 |
| DBP, max, mmHg | 90.11±20.84 | 90.57±20.30 | 0.713 | 0.012 |
| RR, min, breaths/min | 12.98±4.52 | 13.03±4.77 | 0.85 | 0.001 |
| RR, max, breaths/min | 29.60±7.78 | 29.43±7.43 | 0.696 | 0.009 |
| T, min, ℃ | 35.73±1.42 | 35.72±1.46 | 0.937 | 0.008 |
| T, max, ℃ | 37.08±1.23 | 37.06±1.47 | 0.737 | 0.009 |
| SpO2, min, % | 2.46±2.02 | 2.53±2.01 | 0.762 | 0.003 |
| SpO2, max, % | 99.64±1.40 | 99.65±1.60 | 0.878 | 0.02 |
| Laboratory tests | ||||
| Lac, min, mmol/L | 2.46±2.02 | 2.53±2.01 | 0.554 | <0.001 |
| Lac, max, mmol/L | 5.02±3.85 | 5.17±4.21 | 0.528 | 0.013 |
| Scoring system | ||||
| GCS | 10.06±4.75 | 10.06±4.93 | 0.991 | 0.001 |
| SOFA score | 9.49±4.38 | 9.48±4.31 | 0.947 | 0.005 |
| Age-adjusted CCI | 6.12±3.05 | 6.05±3.04 | 0.664 | 0.011 |
| Sepsis | 485 (80.3) | 483 (80.0) | 0.885 | 0.002 |
| ICU_CA | 102 (16.9) | 83 (13.7) | 0.129 | 0.007 |
| Interventions, n (%) | ||||
| MV | 477 (79.0) | 481 (79.6) | 0.776 | 0.004 |
| NE | 404 (66.9) | 399 (66.1) | 0.761 | 0.005 |
| DP | 107 (17.7) | 105 (17.4) | 0.88 | 0.004 |
| Va | 185 (30.6) | 183 (30.3) | 0.901 | 0.007 |
Diagnosis: ICD-10 code=I462 (cardiac arrest due to underlying cardiac condition); BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; min: minimum; max: maximum; HR: heart rate; RR: respiratory rate; T: temperature; SpO2: pulse oxygen saturation; Lac: lactate; GCS: Glasgow Coma Scale; SOFA: Sequential Organ Failure Assessment; CCI: Charlson Comorbidity Index; ICU: intensive care unit; ICU_CA: cardiac arrest happened in ICU; MV: mechanical ventilation; NE: norepinephrine; DP: dopamine; Va: vasopressin.
With the balanced sample, we investigated the primary outcome, the in-hospital death of CA patients admitted to the ICU. With the matched cohort of 604 pairs of patients, we used univariate regression, multivariate regression, dual robustness, and PSM models to evaluate the impact of echocardiography utilization on the in-hospital death outcome of patients with CA in the ICU. As shown in supplementary Table 2, the evaluation results with odds ratios (ORs) significantly lower than 1 according to the various estimation models revealed that there was a negative association between echocardiography utilization and in-hospital death. The results suggested that the in-hospital mortality of patients who underwent echocardiography was lower, which was robust.
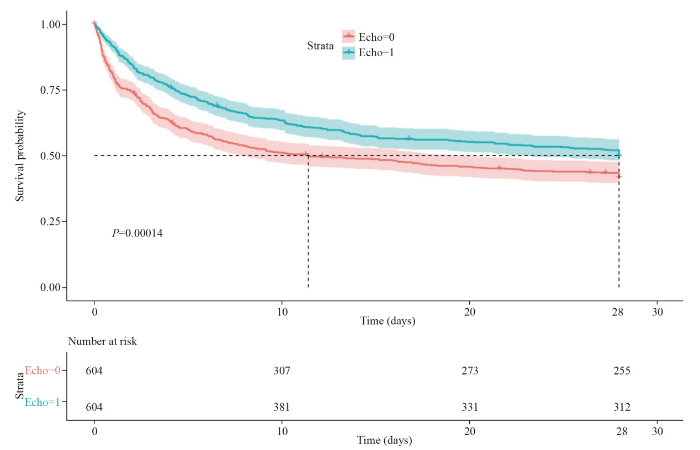
In addition, the matched data were used to analyze the secondary outcome of patient survival within 28 d. In the analysis, the log-rank method was used to construct Kaplan-Meier survival curves to evaluate the impact of echocardiography utilization on 28-day survival after patient admission to the ICU. The results reported in Figure 2 indicated that the 28-day mortality rate of patients with CA in the echocardiograph group was significantly lower, and there were more survivors within 28 d after hospitalization in the ICU for the echocardiography group (P<0.001).
Figure 2.
Figure 2.
The 28-day survival after admission to the ICU for the matched cohorts. The red line (echo=0) represents the survival probability for patients without echocardiography data. The blue line (echo=1) represents the survival probability for patients who underwent echocardiography. ICU: intensive care unit.
Our results revealed that patients with CA in the ICU who underwent echocardiography had a better prognosis. Our findings suggest the possibility of using echocardiography to provide valuable information for emergency clinicians, which could contribute to the proper management of CA patients.
Despite decades of improvements in modern medical care, the survival rate of CA remains extremely low.[7] On the basis of the present findings, echocardiography is a safe, widely used, and relatively low-cost clinical diagnostic tool for evaluating and monitoring hemodynamic disorders in critically ill patients[8] and may help change treatment plans, thereby improving patient prognosis. Early echocardiography can help assess post-resuscitation shock subtypes to prevent mortality after CA.[9] In addition, the post-CA care guidelines also suggest that patients should undergo echocardiographic evaluation within 24 h after cardiopulmonary resuscitation to help guide treatment decisions.[10]
However, existing literature lacks prospective cohort studies evaluating the effectiveness of echocardiography. Researches on the application of echocardiography before CA and after cardiopulmonary resuscitation in critically ill patients is especially limited. It is still unclear how the application of echocardiography at different stages affects patient prognosis. Due to the environmental complexity and heterogeneity of individual patients, randomized controlled trial data may not be available in practice, limiting the refinement of the estimation. Therefore, it is of great research value to evaluate the effect of echocardiography on CA patient prognosis, using real-world data with the help of matching models to form a quasi-experimental design.
There were some limitations to this research. First, this study is a retrospective and observational study that faces multiple potential biases, and the results may interfere with other confounding factors that could not be adjusted. Second, owing to limitations in the research data source, the study was unable to determine the location, time, and initial treatment of CA in the patients, but these factors can be important for their prognosis. Third, whether echocardiography was utilized before the patient entered the ICU could not be confirmed. Consequently, we cannot determine the differences of various echocardiography modes and echocardiography at different stages. Finally, owing to the limited information available from retrospective studies, we cannot explore the working mechanisms of how the utilization of echocardiography can improve patient prognosis.
In conclusion, patients with CA in the ICU who underwent echocardiography may have a better prognosis, with lower 28-day mortality. In the future, researchers can organize strictly controlled studies on the utilization of echocardiography in practical environments, offering more valuable clinical evidence.
Funding: This study is supported by China National High Level Hospital Clinical Research Funding (2022-PUMCH-B-110).
Ethical approval: Not applicable. This was a retrospective study based on the MIMIC-IV database (https://physionet.org/content/mimiciv/1.0/), which has received ethical approval from the Institutional Review Boards at BIDMC and Massachusetts Institute of Technology (MIT). Individual patient consent was not needed because the database does not contain protected health information. The authors obtained permission to use the data.
Conflicts of interest: The authors do not have a financial interest or relationship to disclose regarding this research.
Contributors: NZ performed the research design, data collection and data analysis as well as the writing of the manuscript. QL performed the software work and data processing. HDZ contributed to the overall design and organization of the program. All the authors have read and approved the final manuscript.
All supplementary files in this paper are available at http://wjem.com.cn.
Reference
The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis
Improving mortality in pediatric out-of-hospital cardiac arrest events requires a multifactorial approach
DOI:10.1016/j.jacasi.2022.11.011 PMID:36873764 [Cited within: 1]
Cardiac arrest and related mortality in emergency departments in the United States: analysis of the nationwide emergency department sample
DOI:10.1016/j.resuscitation.2020.10.005
PMID:33086085
[Cited within: 1]

The aim of this study is to analyse the causes of cardiac arrests (CA) in the emergency departments (ED) in the United States and their clinical outcomes according to whether they had a primary or a secondary diagnosis of CA.Data from the Nationwide Emergency Department Sample was assessed for episodes of CA in the emergency department (ED) for adults from 2006 to 2014. Primary and secondary diagnoses of CA and mortality outcomes were evaluated in ED, inpatient and the combined in-hospital setting.There were 2,852,347 ED episodes with a diagnosis of CA (50.5% primary diagnosis, 49.5% secondary diagnosis). Among patients with a secondary diagnosis of CA, ∼33% patients had a primary cardiac diagnosis, followed by infectious and respiratory diagnoses. The survival to ED discharge was 53.2%; lower for primary versus secondary CA diagnosis (20.4% vs 86.7%). The in-hospital survival rate for all CA was 28.7%, and was lower for primary versus secondary CA diagnosis (15.7% vs 41.9%). Survival to hospital discharge was highest in the age group of 41-60 years (33.0%) and was least among >80 years (20.9%). Survival was also noted to be lower among female patients (27.9% vs 29.2%) and in the winter months.Survival with CA in ED is <30% of patients and is greater among patients with a secondary diagnosis of CA. CAs are associated with significant mortality in ED and hospital settings and measures should be taken to better manage cardiac, infection and respiratory causes particularly in the winter months.Copyright © 2020. Published by Elsevier B.V.
What is new in critical care echocardiography?
The diagnostic yield of transthoracic echocardiography in the intensive care unit: a retrospective observational analysis
MIMIC-IV, a freely accessible electronic health record dataset
DOI:10.1038/s41597-022-01899-x
PMID:36596836
[Cited within: 1]

Digital data collection during routine clinical practice is now ubiquitous within hospitals. The data contains valuable information on the care of patients and their response to treatments, offering exciting opportunities for research. Typically, data are stored within archival systems that are not intended to support research. These systems are often inaccessible to researchers and structured for optimal storage, rather than interpretability and analysis. Here we present MIMIC-IV, a publicly available database sourced from the electronic health record of the Beth Israel Deaconess Medical Center. Information available includes patient measurements, orders, diagnoses, procedures, treatments, and deidentified free-text clinical notes. MIMIC-IV is intended to support a wide array of research studies and educational material, helping to reduce barriers to conducting clinical research.© 2023. The Author(s).
Approach to traumatic cardiac arrest in the emergency department: a narrative literature review for emergency providers
DOI:10.5847/wjem.j.1920-8642.2023.085
PMID:38188559
[Cited within: 1]

Traumatic cardiac arrest (TCA) is a major contributor to mortality and morbidity in all age groups and poses a significant burden on the healthcare system. Although there have been advances in treatment modalities, survival rates for TCA patients remain low. This narrative literature review critically examines the indications and effectiveness of current therapeutic approaches in treating TCA.We performed a literature search in the PubMed and Scopus databases for studies published before December 31, 2022. The search was refined by combining search terms, examining relevant study references, and restricting publications to the English language. Following the search, 943 articles were retrieved, and two independent reviewers conducted a screening process.A review of various studies on pre- and intra-arrest prognostic factors showed that survival rates were higher when patients had an initial shockable rhythm. There were conflicting results regarding other prognostic factors, such as witnessed arrest, bystander cardiopulmonary resuscitation (CPR), and the use of prehospital or in-hospital epinephrine. Emergency thoracotomy was found to result in more favorable outcomes in cases of penetrating trauma than in those with blunt trauma. Resuscitative endovascular balloon occlusion of the aorta (REBOA) provides an advantage to emergency thoracotomy in terms of occupational safety for the operator as an alternative in managing hemorrhagic shock. When implemented in the setting of aortic occlusion, emergency thoracotomy and REBOA resulted in comparable mortality rates. Veno-venous extracorporeal life support (V-V ECLS) and veno-arterial extracorporeal life support (V-A ECLS) are viable options for treating respiratory failure and cardiogenic shock, respectively. In the context of traumatic injuries, V-V ECLS has been associated with higher rates of survival to discharge than V-A ECLS.TCA remains a significant challenge for emergency medical services due to its high morbidity and mortality rates. Pre- and intra-arrest prognostic factors can help identify patients who are likely to benefit from aggressive and resource-intensive resuscitation measures. Further research is needed to enhance guidelines for the clinical use of established and emerging therapeutic approaches that can help optimize treatment efficacy and ameliorate survival outcomes.Copyright: © World Journal of Emergency Medicine.
Echocardiography for management of hypotension in the intensive care unit
Shock subtypes by left ventricular ejection fraction following out-of-hospital cardiac arrest
European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: postresuscitation care