INTRODUCTION
Pyogenic liver abscess (PLA) is characterized by bacterial invasion of the liver through various pathways, resulting in localized inflammation and pus formation. Its incidence is increasing, with an estimated rate of approximately 5.7 per 100,000 people.[1] PLA is more likely to occur in elderly individuals, those with underlying medical conditions, and individuals with compromised immune function. The disease progresses rapidly and when bacteria enter the bloodstream, it can lead to sepsis and even death.[2] Sepsis is one of the most fatal and epidemic syndromes in intensive care units and emergency clinics.[3] Clinical studies conducted at multiple centers in China have shown that Xuebijing (XBJ) injection can reduce the 28-day mortality associated with sepsis.[4] XBJ can also alleviate the inflammatory response, improve organ function, and shorten the intensive care unit (ICU) stay in patients with PLA complicated with sepsis.[5] However, the specific molecular mechanisms underlying the effects of XBJ in alleviating PLA complicated by sepsis have not been elucidated. Network pharmacology is a new scientific approach that involves the joint analysis of drugs, components, target genes, disease genes, signaling pathways, and biological processes.[6,7] This approach is often employed to reveal the relationships between drugs, diseases, and target genes. The present study aimed to explore the mechanisms of XBJ in treating PLA complicated with sepsis using a network pharmacology approach, with the objective of providing a theoretical basis and scientific evidence for its clinical application.
METHODS
Identification of active ingredients and targets of XBJ
We used the ETCM database (http://www.tcmip.cn/ETCM/index.php/Home/) to retrieve active ingredients of XBJ (Paeonia lactiflora Pall [Chinese: Chishao], Carthamus tinctorius L. [Chinese: Honghua], Salvia miltiorrhiza Bge. [Chinese: Danshen], Angelica sinensis [Chinese: Danggui], and Ligusticum chuanxiong Hort. [Chinese: Chuanxiong]). With the screening criteria of oral bioavailability ≥30% and drug likeness ≥0.1,[6,7] we obtained the target proteins for each active ingredient from the ETCM data and used the UniProt database (http://www.uniprot.org/) to find the corresponding human target genes for each active target, which are considered the targets of XBJ.
Identification of potential targets related to PLA and sepsis
Using the keywords “pyogenic liver abscess” and “sepsis,” we conducted searches in the GeneCards database (https://www.genecards.org/), PharmGKB database (https://www.pharmgkb.org/), DisGeNET database (https://www.disgenet.org/), Online Mendelian Inheritance in Man (OMIM) database (https://www.omim.org/), Therapeutic Targets Database (TTD) (http://db.idrblab.net/ttd/), and DrugBank database (https://www.drugbank.ca/). The target data from these six databases were merged, and duplicates were removed to obtain the targets related to PLA and sepsis. Finally, the intersection of targets between the PLA and sepsis was identified.
Identification of potential treatment targets
The targets of PLA complicated with sepsis were mapped to the targets of XBJ to identify potential treatment targets. A Venn diagram was created to visualize the intersection. Using Cytoscape 3.8.0, we imported the drugs, active ingredients, and potential treatment targets to construct a network diagram of active ingredients of XBJ and potential treatment targets.
The potential treatment targets were analyzed using the STRING platform (https://cn.string-db.org) with the species set to “Homo sapiens”. A protein-protein interaction (PPI) network was generated with an interaction threshold set at >0.9. The PPI network was imported into Cytoscape 3.8.0 for visualization. The CytoNCA plug-in was used to filter for six parameters: betweenness centrality, closeness centrality, degree centrality, eigenvector centrality, network centrality, and local average connectivity. All of these parameters were needed to be greater than or equal to the median value of the target proteins.[7] A second round of screening was conducted on the filtered target nodes to identify core target proteins.
Identification of signaling pathways and functional enrichment
Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analyses were also conducted for potential treatment targets using the Metascape[8] database (http://metascape.org/gp/index.html) with a significance threshold of P<0.01 and species set to “Homo sapiens.” The results were visualized for further analysis.
Molecular docking of active ingredients with core targets
Two-dimensional (2D) structures of active ingredients corresponding to core targets were obtained from the PubChem database (https://pubchem.ncbi.nlm.nih.gov/). ChemBio3D software was used to convert these 2D structures into three-dimensional (3D) structures. The 3D structures of the core target proteins were downloaded from the PDB database (https://www.rcsb.org/), and PyMOL software was used for dehydration and hydrogenation. The AutoDock software was used to perform molecular docking between the active ingredients and core treatment targets. The binding energies were calculated, with lower energy values indicating greater affinity. Visualizations were generated using PyMOL software.
RESULTS
Active ingredients and targets of XBJ
We identified 29 active ingredients of XBJ in Paeonia lactiflora Pall (Chinese: Chishao), 22 in Carthamus tinctorius L. (Chinese: Honghua), 65 in Salvia miltiorrhiza Bge. (Chinese: Danshen), two in Angelica sinensis (Chinese: Danggui), and seven in Ligusticum chuanxiong Hort. (Chinese: Chuanxiong) based on the pharmacokinetic criteria from the ETCM database. After the identification of the corresponding target proteins for each active ingredient from the ETCM database and the removal of duplicates, 224 targets were obtained.
Potential targets for treating PLA complicated with sepsis
With respect to the GeneCards database, 604 targets related to the PLA were obtained (score ≥1). We obtained 0, 24, 0, 0, and 12 targets from the PharmGKB, DisGeNET, OMIM, TTD, and DrugBank databases, respectively. After removing duplicate targets and merging data from these six databases, a total of 623 targets were obtained. Similarly, sepsis-related targets were obtained from GeneCards (2,121 targets), PharmGKB (0 targets), DisGeNET (1,453 targets), OMIM (1 target), TTD (28 targets), and DrugBank (14 targets). After merging and removing duplicates, a total of 2,965 targets were obtained. The intersection of targets between PLA and sepsis resulted in 357 targets.
Potential treatment targets
The intersection of the active ingredient targets of XBJ with the targets of PLA complicated with sepsis yielded 54 potential treatment targets. A network diagram constructed using Cytoscape 3.8.0 and containing 72 active ingredients that act on potential treatment targets indicated that quercetin, luteolin, and kaempferol acted on 42, 22, and 14 potential treatment targets, respectively, suggesting their potential as the main active ingredients in the treatment of PLA complicated by sepsis.
The STRING platform was used to analyze the 54 potential treatment targets, and the PPI analysis results were imported into Cytoscape 3.8.0 software for visualization. Using the CytoNCA plug-in, the first round of screening identified the following targets: signal transducer and activator of transcription 3, tumor protein 53, intercellular adhesion molecule 1, epidermal growth factor receptor, chemokine ligand 2, vascular cell adhesion molecule 1, interleukin-4 (IL-4), interferon-gamma, IL-10, IL-1β, tumor necrosis factor (TNF), IL-6, IL-8, and prostaglandin-endoperoxide synthase 2. In the second round of screening, the IL-1β, IL-6, and TNF targets were obtained.
Potential treatment target pathways and functional enrichment results
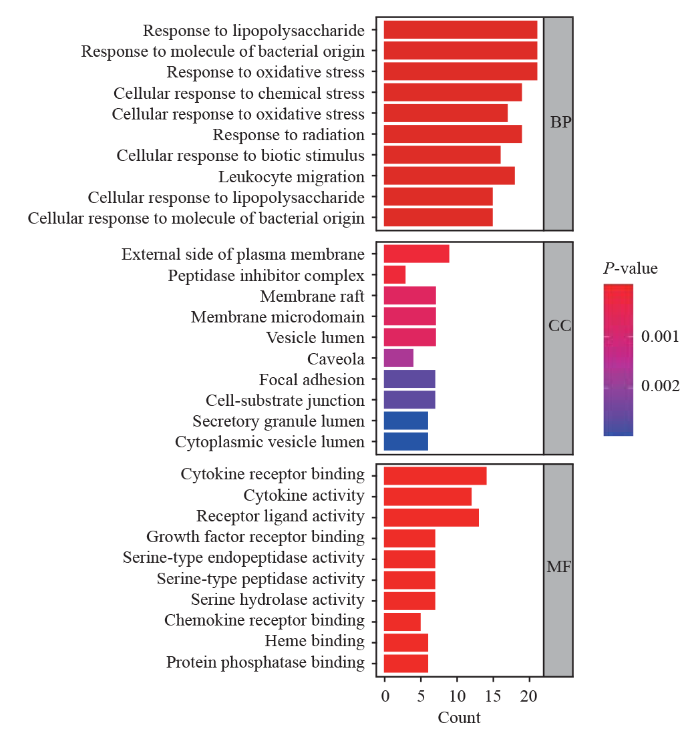
The potential treatment targets (n=54) were imported into the Metascape platform for GO functional enrichment analysis (P<0.01), resulting in 1,329 entries. The top 10 entries for biological processes (BP), cellular components, and molecular functions are shown in Figure 1.
Figure 1.
Figure 1.
A column chart of the results of the GO functional enrichment analysis is shown, depicting the top 10 results. GO: Gene Ontology; BP: biological processes; CC: cellular components; MF: molecular function.
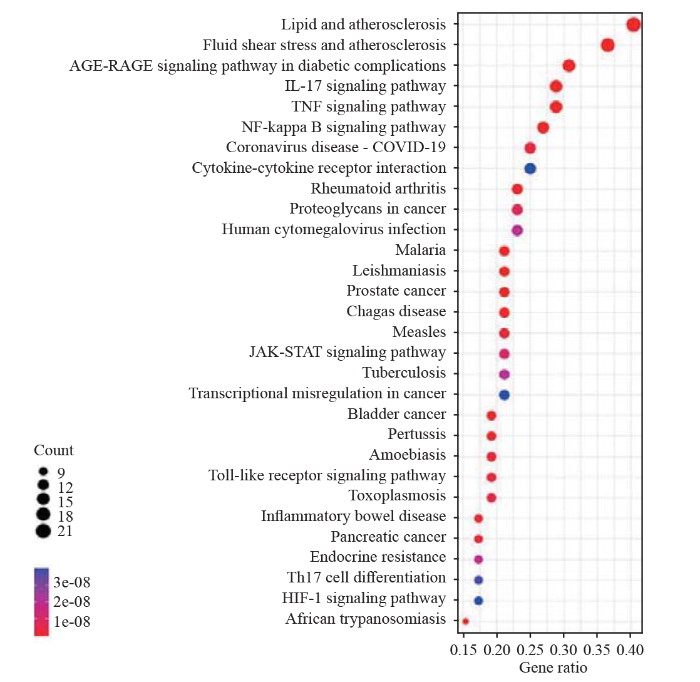
KEGG pathway enrichment analysis of the 54 potential treatment targets was performed using the Metascape platform and yielded 125 pathways (P<0.01). The top 30 signaling pathways are shown in Figure 2. After removing broad and disease-related pathways, the four signaling pathways most relevant to treating PLA complicated by sepsis with XBJ were found to be the IL-17, TNF, nuclear factor-kappa B (NF-κB), and Toll-like receptor (TLR) signaling pathways. The IL-17, TNF, NF-κB, and TLR signaling pathways were enriched for 15, 15, 14, and 10 potential treatment targets, respectively.
Figure 2.
Figure 2.
Bubble chart of the KEGG pathway enrichment analysis, depicting the top 30 results. KEGG: Kyoto Encyclopedia of Genes and Genomes.
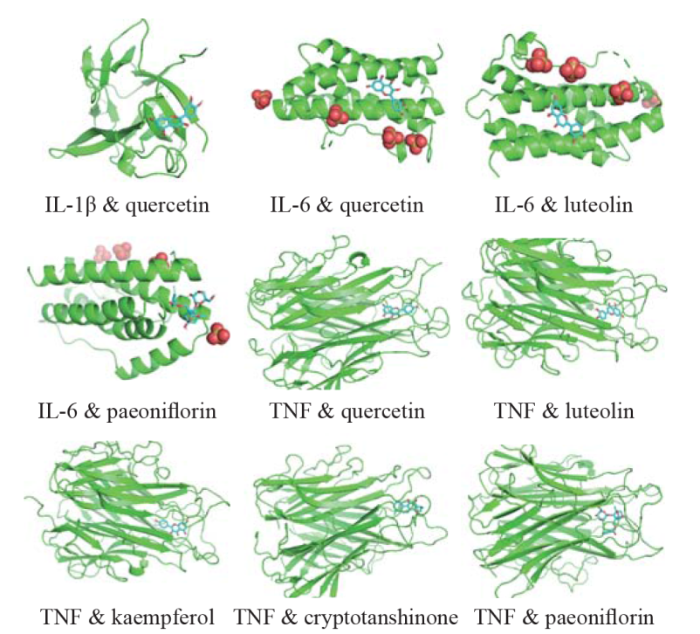
Molecular docking results
Using AutoDock software, molecular docking was performed between the active ingredients of XBJ and the potential treatment core targets (IL-1β, IL-6, and TNF). A binding energy of ≤ -5 kcal/mol suggested a strong binding affinity between the receptor and ligand.[7] The binding energies between IL-1β, IL-6, TNF, and the active ingredients are shown in Table 1. The results of molecular docking experiments of IL-1β, IL-6, and TNF with the active ingredients are illustrated in Figure 3.
Table 1. Binding energies of IL-1β, IL-6, and TNF with the active ingredient of Xuebijing
| Target protein | Active ingredient | Binding energy (kcal/mol) |
|---|---|---|
| IL-1β | Quercetin | -7.3 |
| IL-6 | Quercetin | -6.9 |
| IL-6 | Luteolin | -7.2 |
| IL-6 | Paeoniflorin | -6.6 |
| TNF | Quercetin | -9.2 |
| TNF | Luteolin | -9.2 |
| TNF | Kaempferol | -9.5 |
| TNF | Cryptotanshinone | -8.6 |
| TNF | Paeoniflorin | -10.5 |
IL: interleukin; TNF: tumor necrosis factor.
Figure 3.
Figure 3.
Molecular docking of IL-1β, IL-6, and TNF. IL-1β: interleukin-1β; IL-6: interleukin-6; TNF: tumor necrosis factor.
DISCUSSION
PLA is a common critical condition encountered in emergency medicine and is characterized by rapid disease progression. Approximately 73.1% of patients with PLA develop sepsis, and 9.1% of them progress to septic shock.[2] XBJ is a compound formulation composed of various herbs known for its blood-activating and stasis-removing properties, including Paeonia lactiflora Pall (Chinese: Chishao), Carthamus tinctorius L. (Chinese: Honghua), Salvia miltiorrhiza Bge. (Chinese: Danshen), Angelica sinensis (Chinese: Danggui), and Ligusticum chuanxiong Hort. (Chinese: Chuanxiong). In addition, XBJ has anti-inflammatory, microcirculatory, and immunomodulatory effects. XBJ can alleviate the inflammatory response caused by inflammatory factors and endotoxins in sepsis, regulate the anti-inflammatory and pro-inflammatory systems to achieve a relative balance, improve microcirculation and organ function, and reduce the mortality rate of patients with sepsis.[9] However, the specific molecular mechanisms of action of XBJ in the treatment of PLA combined with sepsis are not well understood.
The network diagram of drug-active ingredient targets constructed in this study revealed that XBJ contains 72 active ingredients that act on 54 potential treatment targets in patients with PLA combined with sepsis. Among these, quercetin, luteolin, and kaempferol were the most targeted compounds. Quercetin is a flavonoid compound that has a range of biological activities, including the regulation of oxidative stress, anti-inflammatory effects, and anti-infectious properties. Quercetin can reduce the oxidative stress and inflammatory responses induced by lipopolysaccharides in the liver, ameliorate tissue injury, and protect the liver.[10] It can also decrease the release of IL-1β, IL-6, and TNF-α, thus ameliorating the inflammatory response.[11] Quercetin can alleviate oxidative stress, inflammation, and TLR mRNA expression; regulate immune responses; and mitigate organ dysfunction related to sepsis, making it beneficial for sepsis[12] Luteolin is a tetrahydroxy flavonoid with various biological activities, including antibacterial, anti-inflammatory, and anti-oxidative stress responses. Luteolin reduces inflammation and liver cell injury induced by lipopolysaccharides by inhibiting the production and release of high mobility group box 1 (HMGB1) and activation of cyclooxygenase-2 (COX-2).[13] It has a beneficial effect on sepsis through multiple pathways, such as alleviating oxidative stress, influencing the initiation of inflammatory pathways, reducing the expression of inflammatory factors, and modulating the immune response.[14] Kaempferol is a natural polyphenol small molecule that can inhibit oxidative stress injury and inflammation in the livers of septic rats.[15] Kaempferol can combat sepsis by alleviating the inflammatory response induced by lipopolysaccharides through the regulation of the sphingosine kinase type 1/sphingosine 1-phosphate (SphK1/S1P) signaling pathway, thus stabilizing the endothelial barrier.[16] Therefore, the active ingredients in XBJ for treating PLA combined with sepsis are quercetin, luteolin, and kaempferol. These three compounds may be potential drugs for treating PLA combined with sepsis.
This study constructed a PPI network of the 54 potential treatment targets in patients with PLA combined with sepsis and identified core targets through two rounds of screening. These core targets were IL-1β, TNF, and IL-6. Monocytes and macrophages primarily produce IL-1β in response to endotoxins, and this cytokine serves as another crucial inflammatory factor in systemic inflammatory response syndrome and plays an irreplaceable role in sepsis.[17] During sepsis, IL-1β produced by macrophages disrupts vascular stability through IL-1R1, serving as a key mediator in promoting inflammation and tissue injury.[18] IL-1β levels may be a potential diagnostic and predictive biomarker for sepsis and an independent risk factor for predicting mortality within 28 d after sepsis.[19] TNF is a pro-inflammatory cytokine and serum biomarker for inflammation and immune-mediated diseases. An imbalance in the serum TNF receptor ligand level in critically ill patients with sepsis can predict mortality.[20] TNF can also induce hepatocyte apoptosis and necrotic apoptosis in hepatic inflammation.[2] IL-6 is an important inflammatory cytokine produced by various cells. The release of large amounts of IL-6 and other inflammatory factors during sepsis causes liver cell injury, leading to acute liver dysfunction. Early suppression of its release is highly important for preventing and treating organ dysfunction in sepsis patients.[22] IL-6 plays a crucial role in regulating immune and inflammatory responses, and high levels of IL-6 are associated with an increased risk of severe sepsis and mortality.[232] The above findings indicate that IL-1β, TNF, and IL-6 are potential therapeutic molecular targets for PLA combined with sepsis.
KEGG enrichment analysis suggested that XBJ may exert therapeutic effects on PLA complicated with sepsis by modulating signaling pathways, primarily the IL-17, TNF, NF-κB, and TLR signaling pathways. Regulating the IL-17, TNF, NF-κB, and TLR signaling pathways can reduce the release of inflammatory factors such as IL-1β, TNF, and IL-6; alleviate oxidative stress injury; and suppress inflammation, thereby preventing or mitigating organ dysfunction caused by sepsis. The TLR signaling pathway plays an important role in the immune system by recognizing pathogens such as lipopolysaccharides, inducing inflammation, and participating in the inflammatory process of sepsis. The transduction of endogenous negative regulatory factors of TLR signaling can be used as a gene therapy for treating cytokine storms in sepsis.[243] XBJ can inhibit the expression of TLR4 on the cell surface induced by lipopolysaccharides, thereby inhibiting the release of endogenous inflammatory mediators,[25] which is consistent with the results of the present study. GO enrichment analysis of the BP indicates that the treatment targets mainly involved responses to lipopolysaccharides, bacterial molecules, oxidative stress, and white blood cell migration. XBJ may regulate the above-mentioned BPs to alleviate PLA complicated with sepsis.
A lower binding energy between the receptor and the ligand indicates has better binding activity and greater stability of the complex. A binding energy of ≤ -5 kcal/mol suggested a strong binding affinity between the receptor and ligand.[7] The molecular docking binding energies for IL-1β, TNF, and IL-6 were all ≤ -5 kcal/mol, confirming the strong binding activity and stable conformations of these proteins, as predicted in this study.
CONCLUSION
This study demonstrated that quercetin, luteolin, and kaempferol are the core XBJ components that can help in treating PLA complicated with sepsis. The targets IL-1β, IL-6, and TNF, as well as the IL-17, TNF, NF-κB, and TLR signaling pathways, are crucial targets and pathways for XBJ in the treatment of PLA complicated with sepsis, providing a theoretical foundation and scientific basis for its clinical application. Since the identification of the active ingredients, targets, and pathways of XBJ in this study was based on network bioinformatics and data calculations, this study has certain limitations, and further experimental validation of the mechanisms of XBJ in the treatment of PLA complicated with sepsis is necessary.
Funding: The study was supported by Hunan Province Key Research and Development Program (2020SKC2004).
Ethical approval: The study was approved by ethical committee of Hunan Provincial People’s Hospital.
Conflicts of interest: All authors declare that they do not have any potential conflict of interest in relation to this manuscript.
Contributors: WZ: conceptualization, design, data collection, visualization, writing original draft; MYF: conceptualization; XL and FY: literature search; EZ: methodology; XTH: conceptualization, funding acquisition, supervision, writing - review, editing.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
A comparison of pyogenic liver abscess in patients with or without diabetes: a retrospective study of 246 cases
DOI:10.1186/s12876-018-0875-y
PMID:30285638
[Cited within: 1]

Background: Pyogenic liver abscess(PLA) has become common in patients with diabetes mellitus (DM), but it is unclear whether differences exist between patients with and without DM. A retrospective study was performed to identify these differences, summarize the clinical experience, and improve the diagnosis and treatment of PLA.Methods: The patients were enrolled in a teaching hospital from January 2012 to December 2016. The patients were separated into two groups based on comorbidity with diabetes mellitus (DM). The DM group was further separated into two subgroups according to the HbA1C concentration to investigate whether glycaemic control affected the clinical characteristics of PLA patients with DM. Chi-square, Fisher's exact test, and t-tests were used to analyse and evaluate differences between the two groups.Results: Two hundred and forty-six PLA patients were identified and 90 (36.6%) had comorbid DM. Patients with DM were older, had higher levels of alkaline phosphatase and gamma-glutamyl transferase, hypertension, a loss of body weight, a single abscess, and combined antibiotic therapy with the use of carbapenems and Klebsiella pneumoniae in their blood cultures but a less frequent history of abdominal surgery and Escherichia coli in their pus cultures. When DM patients were compared to non-DM patients, each of these differences was significant (P < 0.05). Diabetic PLA patients with poor glycaemic control had a significantly higher proportion of fever and both lobes abscess(P < 0.05).Conclusion: PLA patients with diabetes are older, have more serious complications, a higher prevalence of cardiovascular disease, an increased use of combined antibiotic therapy with carbapenem, and K. pneumoniae as the predominant pathogen, but these patients had fewer abdominal surgeries and fewer E. coli infections. In addition, poorly controlled glycaemia in diabetic PLA patients is associated with high incidence of fever and both lobes abscess.
Risk factors and early diagnosis of sepsis caused by liver abscess
Endothelial cell metabolism in sepsis
DOI:10.5847/wjem.j.1920-8642.2023.019 URL [Cited within: 1]
Effect of an herbal-based injection on 28-day mortality in patients with sepsis: the EXIT-SEP randomized clinical trial
DOI:10.1001/jamainternmed.2023.0780
PMID:37126332
[Cited within: 1]

Previous research has suggested that Xuebijing injection (XBJ), an herbal-based intravenous preparation, may reduce mortality among patients with sepsis.To determine the effect of XBJ vs placebo on 28-day mortality among patients with sepsis.The Efficacy of Xuebijing Injection in Patients With Sepsis (EXIT-SEP) trial was a multicenter, randomized double-blind, placebo-controlled trial conducted in intensive care units at 45 sites and included 1817 randomized patients with sepsis (sepsis 3.0) present for less than 48 hours. Patients aged 18 to 75 years with a Sequential Organ Failure Assessment score of 2 to 13 were enrolled. The study was conducted from October 2017 to June 2019. The final date of follow-up was July 26, 2019. Data analysis was performed from January 2020 to August 2022.The patients were randomized to receive either intravenous infusion of XBJ (100 mL, n = 911) or volume-matched saline placebo (n = 906) every 12 hours for 5 days.The primary outcome was 28-day mortality.Among the 1817 patients who were randomized (mean [SD] age, 56.5 [13.5] years; 1199 [66.0%] men), 1760 (96.9%) completed the trial. In these patients, the 28-day mortality rate was significantly different between the placebo group and the XBJ group (230 of 882 patients [26.1%] vs 165 of 878 patients [18.8%], respectively; P < .001). The absolute risk difference was 7.3 (95% CI, 3.4-11.2) percentage points. The incidence of adverse events was 222 of 878 patients (25.3%) in the placebo group and 200 of 872 patients (22.9%) in the XBJ group.In this randomized clinical trial among patients with sepsis, the administration of XBJ reduced 28-day mortality compared with placebo.ClinicalTrials.gov Identifier: NCT03238742.
The clinical effect of Xuebijing on the patients with bacterial liver abscess and sepsis
Network pharmacology prediction and molecular docking-based strategy to explore the potential mechanism of Huanglian Jiedu Decoction against sepsis
DOI:10.1016/j.compbiomed.2022.105389 URL [Cited within: 2]
Network pharmacology prediction and molecular docking-based strategy to discover the potential pharmacological mechanism of Huai Hua San against ulcerative colitis
DOI:10.2147/DDDT.S319786
PMID:34349502
[Cited within: 5]

Huai Hua San (HHS), a famous Traditional Chinese Medicine (TCM) formula, has been widely applied in treating ulcerative colitis (UC). However, the interaction of bioactives from HHS with the targets involved in UC has not been elucidated yet.A network pharmacology-based approach combined with molecular docking and in vitro validation was performed to determine the bioactives, key targets, and potential pharmacological mechanism of HHS against UC.Bioactives and potential targets of HHS, as well as UC-related targets, were retrieved from public databases. Crucial bioactive ingredients, potential targets, and signaling pathways were acquired through bioinformatics analysis, including protein-protein interaction (PPI), as well as the Gene Ontology (GO) and the Kyoto Encyclopedia of Genes and Genomes (KEGG) analysis. Subsequently, molecular docking was carried out to predict the combination of active compounds with core targets. Lastly, in vitro experiments were conducted to further verify the findings.A total of 28 bioactive ingredients of HHS and 421 HHS-UC-related targets were screened. Bioinformatics analysis revealed that quercetin, luteolin, and nobiletin may be potential candidate agents. JUN, TP53, and ESR1 could become potential therapeutic targets. PI3K-AKT signaling pathway might play an important role in HHS against UC. Moreover, molecular docking suggested that quercetin, luteolin, and nobiletin combined well with JUN, TP53, and ESR1, respectively. Cell experiments showed that the most important ingredient of HHS, quercetin, could inhibit the levels of inflammatory factors and phosphorylated c-Jun, as well as PI3K-Akt signaling pathway in LPS-induced RAW264.7 cells, which further confirmed the prediction by network pharmacology strategy and molecular docking.Our results comprehensively illustrated the bioactives, potential targets, and molecular mechanism of HHS against UC. It also provided a promising strategy to uncover the scientific basis and therapeutic mechanism of TCM formulae in treating diseases.© 2021 Liu et al.
Metascape provides a biologist-oriented resource for the analysis of systems-level datasets
DOI:10.1038/s41467-019-09234-6
PMID:30944313
[Cited within: 1]

A critical component in the interpretation of systems-level studies is the inference of enriched biological pathways and protein complexes contained within OMICs datasets. Successful analysis requires the integration of a broad set of current biological databases and the application of a robust analytical pipeline to produce readily interpretable results. Metascape is a web-based portal designed to provide a comprehensive gene list annotation and analysis resource for experimental biologists. In terms of design features, Metascape combines functional enrichment, interactome analysis, gene annotation, and membership search to leverage over 40 independent knowledgebases within one integrated portal. Additionally, it facilitates comparative analyses of datasets across multiple independent and orthogonal experiments. Metascape provides a significantly simplified user experience through a one-click Express Analysis interface to generate interpretable outputs. Taken together, Metascape is an effective and efficient tool for experimental biologists to comprehensively analyze and interpret OMICs-based studies in the big data era.
Effect of Xuebijing on inflammatory response and clinical efficacy in patients with sepsis
Involvement of P450s and nuclear receptors in the hepatoprotective effect of quercetin on liver injury by bacterial lipopolysaccharide
DOI:10.1080/08923973.2020.1742154 URL [Cited within: 1]
Quercetin and quercitrin attenuates the inflammatory response and oxidative stress in LPS-induced RAW264.7 cells: in vitro assessment and a theoretical model
A comprehensive systematic review of the therapeutic effects and mechanisms of action of quercetin in sepsis
DOI:10.1016/j.phymed.2021.153567 URL [Cited within: 1]
Luteolin attenuates hepatic injury in septic mice by regulating P2X7R-based HMGB1 release
DOI:10.1039/D1FO01746B
URL
[Cited within: 1]

Luteolin reverses septic hepatic injury, especially inflammation, likely by regulating the release of HMGB1 through the P2X7R–RAGE–TLR4 axis.
Effects of luteolin on sepsis: a comprehensive systematic review
DOI:10.1016/j.phymed.2023.154734 URL [Cited within: 1]
The effect of kaempferol on liver function injury in septic rats and its relationship with HIF-1α/HK2 signaling pathway
Kaempferol alleviates the inflammatory response and stabilizes the pulmonary vascular endothelial barrier in LPS-induced sepsis through regulating the SphK1/S1P signaling pathway
DOI:10.1016/j.cbi.2022.110221 URL [Cited within: 1]
Interleukin-1β protection against experimental sepsis in mice
DOI:10.1007/s10753-020-01341-7 [Cited within: 1]
IL-1β suppression of VE-cadherin transcription underlies sepsis-induced inflammatory lung injury
DOI:10.1172/JCI136908
PMID:32298238
[Cited within: 1]

Unchecked inflammation is a hallmark of inflammatory tissue injury in diseases such as acute respiratory distress syndrome (ARDS). Yet the mechanisms of inflammatory lung injury remain largely unknown. Here we showed that bacterial endotoxin lipopolysaccharide (LPS) and cecal ligation and puncture-induced (CLP-induced) polymicrobial sepsis decreased the expression of transcription factor cAMP response element binding (CREB) in lung endothelial cells. We demonstrated that endothelial CREB was crucial for VE-cadherin transcription and the formation of the normal restrictive endothelial adherens junctions. The inflammatory cytokine IL-1β reduced cAMP generation and CREB-mediated transcription of VE-cadherin. Furthermore, endothelial cell-specific deletion of CREB induced lung vascular injury whereas ectopic expression of CREB in the endothelium prevented the injury. We also observed that rolipram, which inhibits type 4 cyclic nucleotide phosphodiesterase-mediated (PDE4-mediated) hydrolysis of cAMP, prevented endotoxemia-induced lung vascular injury since it preserved CREB-mediated VE-cadherin expression. These data demonstrate the fundamental role of the endothelial cAMP-CREB axis in promoting lung vascular integrity and suppressing inflammatory injury. Therefore, strategies aimed at enhancing endothelial CREB-mediated VE-cadherin transcription are potentially useful in preventing sepsis-induced lung vascular injury in ARDS.
Value of IL-1β and IL-23 in predicting 28-day mortality due to sepsis: a retrospective study
Serum levels of TNF receptor ligands are dysregulated in sepsis and predict mortality in critically ill patients
DOI:10.1371/journal.pone.0153765 URL [Cited within: 1]
TNF in the liver: targeting a central player in inflammation
DOI:10.1007/s00281-022-00910-2
PMID:35122118

Tumour necrosis factor-α (TNF) is a multifunctional cytokine. First recognized as an endogenous soluble factor that induces necrosis of solid tumours, TNF became increasingly important as pro-inflammatory cytokine being involved in the immunopathogenesis of several autoimmune diseases. In the liver, TNF induces numerous biological responses such as hepatocyte apoptosis and necroptosis, liver inflammation and regeneration, and autoimmunity, but also progression to hepatocellular carcinoma. Considering these multiple functions of TNF in the liver, we propose anti-TNF therapies that specifically target TNF signalling at the level of its specific receptors.© 2022. The Author(s).
Effects of inhibition of IL-6/STAT3 signaling pathway on liver injury in septic rats
Association between IL-6 polymorphisms and sepsis
DOI:10.1177/1753425919872818
URL

The aim of the present study was to determine whether IL-6 polymorphisms correlate with sepsis. According to the inclusion criteria, the association of IL-6 polymorphisms with sepsis was searched in databases and analysed using comprehensive meta-analysis software. A total of 16 studies were included in this meta-analysis. There was no significant association between the IL-6-174G/C polymorphism and sepsis risk in the total population (C vs. G: OR = 1.04, 95% CI = 0.79–1.38; CC vs. GG: OR = 0.86, 95% CI = 0.53–1.41; CG vs. GG: OR = 0.99, 95% CI = 0.79–1.24; dominant model: OR = 0.97, 95% CI = 0.74–1.29; recessive model: OR = 0.92, 95% CI = 0.61–1.39). When patients were stratified according to ethnicity, a statistically significant association was observed in Asians and Africans. As for the -572G/C polymorphism, the results showed that the IL-6-572C/G polymorphism was not associated with sepsis susceptibility (G vs. C: OR = 0.98, 95% CI = 0.79–1.22; GG vs. CC: OR = 1.46, 95% CI = 0.53–4.03; GC vs. CC: OR = 0.82, 95% CI = 0.54–1.27; dominant model: OR = 0.88, 95% CI = 0.55–1.41; recessive model: OR = 1.55, 95% CI = 0.82–2.92). The data indicated that the IL-6-174G/C polymorphism may contribute to sepsis risk, especially in Africans and Asians. No significant association was observed between the IL-6-572G/C polymorphism and sepsis risk.
Toll-like receptors in sepsis-associated cytokine storm and their endogenous negative regulators as future immunomodulatory targets
DOI:10.1016/j.intimp.2020.107087 URL
HMGB1-TLR4-IL23-IL17A axis promotes paraquat-induced acute lung injury by mediating neutrophil infiltration in mice
DOI:10.1038/s41598-017-00721-8
PMID:28377603
[Cited within: 1]

Paraquat is a poisoning herbicide that primarily targets lung, leading to severe acute lung injury characterized by extensive neutrophil infiltration. However, the mechanisms underlying the neutrophil infiltration is not clear. In this study, we demonstrated the significance of the signaling cascade from high-mobility group box 1 (HMGB1), to Toll-like receptor 4 (TLR4), interleukin-23 (IL-23), and lastly to IL-17A during the paraquat-induced neutrophil infiltration and the subsequent lung injury in mice. Paraquat challenge significantly elevated serum levels of IL-17A and IL-23, the percentage of IL-17A-producing γδT cells in the lung, and the level of HMGB1 in bronchoalveolar lavage fluid. Reducing IL-17A production using an anti-γδT antibody, targeting IL-23 with the neutralizing antibody against IL-23p19, and blocking HMGB1 signaling by using glycyrrhizin or TLR4 mice all dramatically inhibited the infiltration of neutrophils and attenuated lung injury. These novel findings not only reveal the critical role of HMGB1-TLR4-IL-23-IL-17A axis in the pathogenesis of paraquat-induced acute lung injury, but also provide promising therapeutic targets for treating paraquat poisoning.