INTRODUCTION
Cardiac arrest remains a leading cause of death in emergency departments around the world and has a high incidence and associated economic costs.[1,2] Some patients with cardiac arrest who achieve a return of spontaneous circulation (ROSC) after cardiopulmonary resuscitation (CPR) cannot maintain their spontaneous circulation and thus develop a second cardiac arrest (i.e., recurrent cardiac arrest or rearrest) within a short time. Rearrest is a critical barrier to survival after cardiac arrest.[3] Up to 50% of patients who achieve ROSC will develop rearrest.[4⇓-6] Moreover, rearrest is associated with high mortality and poor neurological outcomes.[7⇓-9] Because high-quality CPR can only provide less than one-third of normal cardiac output (CO), prolonged CPR in patients with rearrest reduces the possibility of ROSC.[3] If patients at higher risk of rearrest can be identified earlier and receive more aggressive treatment, such as extracorporeal CPR (ECPR), their prognosis may be improved.
Only a few studies have retrospectively analyzed the characteristics of patients who have rearrest, and the findings from these studies have raised some concerns about the risk factors for rearrest. Extreme tachycardia at the time of ROSC is associated with a high probability of sustained ROSC.[10] However, assessment based on heart rate and heart rhythm may be unreliable because these findings are easily affected by many factors, such as the administration of adrenaline. A previous study has proven that end-tidal carbon dioxide (ETCO2) has a clear relationship with the cardiac index and coronary perfusion pressure.[11] ETCO2 can be used to monitor the quality of CPR, detect ROSC, and predict survival after cardiac arrest.[12⇓⇓-15] Our research group has shown that pulse oximetry photoplethysmogram (POP) and its waveform components are also important physiological parameters during resuscitation and are also closely related to ROSC during CPR in patients with cardiac arrest.[13,16,17] We hypothesized that the combination of ETCO2 and POP might be discriminative for the early recognition of patients at risk of unsustained ROSC before rearrest. Therefore, we conducted this multicenter, prospective, observational study to investigate whether ETCO2 and POP either separately or in combination can predict unsustained ROSC.
METHODS
Population and study setting
This multicenter, prospective, observational study was conducted from December 1, 2013 to November 30, 2014 in the emergency departments of fourteen hospitals in six provinces located throughout China. The exclusion criteria were unobtainable POP, ETCO2, or electrocardiogram (ECG) measurements, data loss, or data with incorrect timings.
Data collection
Data collection was performed using Utstein templates. General data included the patient identifier, age, sex, incident date, known precipitating event, preexisting illnesses, cause of cardiac arrest (if known), location of cardiac arrest, details of advanced cardiac life support (ACLS) procedures (including endotracheal intubation, any vasopressors used, defibrillation attempts and settings), and survival data (24-hour and 28-day survival).
All patients received CPR by trained physicians according to current ACLS guidelines established by the American Heart Association.[18] ECG and POP were monitored at the initiation of CPR. ETCO2 was continuously monitored starting immediately after endotracheal intubation. We acquired the area under the curve (AUCp) and amplitude (Amp) of the POP waveform from the near-infrared signals of POP.[17] All patient data were collected for at least 20 min after ROSC to determine whether the patient rearrested. The mean Amp, AUCp, and ETCO2 during the last 2 min of CPR and the first 10 min after ROSC were calculated as described in a previous study.[17]
ROSC was defined as the restoration of a palpable pulse and autonomous cardiac rhythm after the completion or cessation of CPR. Unsustained ROSC was defined as rearrest within 20 min after a previous ROSC.[19⇓-21] Patients with ROSC who did not meet the criteria for unsustained ROSC were considered to have sustained ROSC.
Ethical statement
The study protocol was approved by the ethics committee of the Peking Union Medical College Hospital (approval number: 20131S-512). This study was registered on the ClinicalTrials.gov.
Statistical analysis
The statistical analysis was performed using SPSS 24.0 for Windows (IBM Corp., USA). Continuous data are presented as the means±standard deviations or medians with interquartile ranges depending on the normality of the distribution, and categorical data are presented as numbers with percentages. Continuous variables were compared by applying Student’s t-test or the Mann-Whitney U-test, as appropriate, and categorical variables were compared using the χ2 test or Fisher’s exact test. A P-value less than 0.05 was considered statistically significant. A logistic regression analysis model was used to analyze predictive factors. The receiver operating characteristic (ROC) curve analysis was performed to evaluate the accuracy of the predicted unsustained ROSC. The optimal cutoff point was determined by estimating Youden’s index.
RESULTS
Baseline characteristics
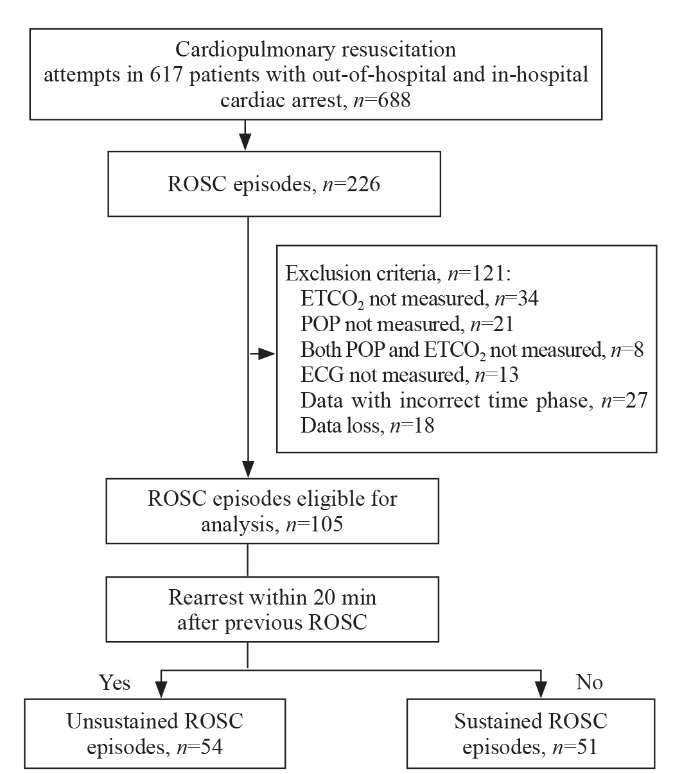
From December 1, 2013 to November 30, 2014, a total of 617 patients with cardiac arrest received 688 CPR attempts. Forty-six patients received CPR more than once. Among the 688 CPR attempts, 226 (32.8%) resulted in ROSC, and 121 were excluded because of data loss or incomplete data; thus, the remaining 105 CPR attempts were included in our study. These 105 CPR attempts were performed in 80 patients (16 patients underwent CPR more than once). Among them, 54 ROSC episodes resulted in subsequential rearrest within 20 min after previous ROSC, and these patients were assigned to the unsustained ROSC group; the remaining 51 were assigned to the sustained ROSC group (Figure 1). Patients in whom the last ROSC episode was unsustained were regarded as unsustained ROSC patients, and patients in whom the last ROSC episode was sustained were regarded as sustained ROSC patients. The baseline information and clinical features of the patients in the two groups (32 unsustained ROSC patients and 48 sustained ROSC patients) are shown in Table 1.
Figure 1.
Figure 1.
Flowchart of the study population. ROSC: return of spontaneous circulation; ETCO2: end-tidal carbon dioxide; POP: pulse oximetry photoplethysmogram; ECG: electrocardiogram.
Table 1. Baseline information of patients in the sustained ROSC group and unsustained ROSC group
| Parameters | Unsustained ROSC patients (n=32) | Sustained ROSC patients (n=48) | P-value |
|---|---|---|---|
| Sex, female, n (%) | 7 (21.9) | 17 (35.4) | 0.195 |
| Age, years, median (IQR) | 63.0 (45.5, 77.0) | 63.5 (50.3, 73.5) | 0.848 |
| Location of cardiac arrest, n (%) | |||
| Out of hospital | 6 (18.8) | 11 (22.9) | 0.655 |
| In hospital | 26 (81.2) | 37 (77.1) | |
| Cause of cardiac arrest, n (%) | |||
| Cardiogenic | 12 (37.5) | 17 (35.4) | 0.849 |
| Hypoxemic | 9 (28.1) | 18 (37.5) | 0.385 |
| Shock | 6 (18.8) | 6 (12.5) | 0.655 |
| Stroke | 2 (6.3) | 3 (6.3) | 1.000 |
| Trauma | 3 (9.4) | 4 (8.3) | 1.000 |
| Survival rate, n (%) | |||
| 24-hour survival | 3 (9.4) | 14 (29.2) | 0.034* |
| 28-day survival | 0 (0) | 4 (8.3) | 0.249 |
ROSC: return of spontaneous circulation; IQR: interquartile range. *P<0.05.
The patients’ median age was 63.5 (49.3, 74.0) years, and 56 (70.0%) of the 80 patients were male. Seventeen (21.3%) patients had out-of-hospital cardiac arrest. There was no significant difference in sex, age, or location of cardiac arrest between the sustained and unsustained ROSC groups. The 24-hour survival rate was significantly higher in the sustained ROSC group than in the unsustained ROSC group (29.2% vs. 9.4%, P<0.05). No patient in the unsustained ROSC group survived to 28 d post-resuscitation.
ETCO2 and POP parameters
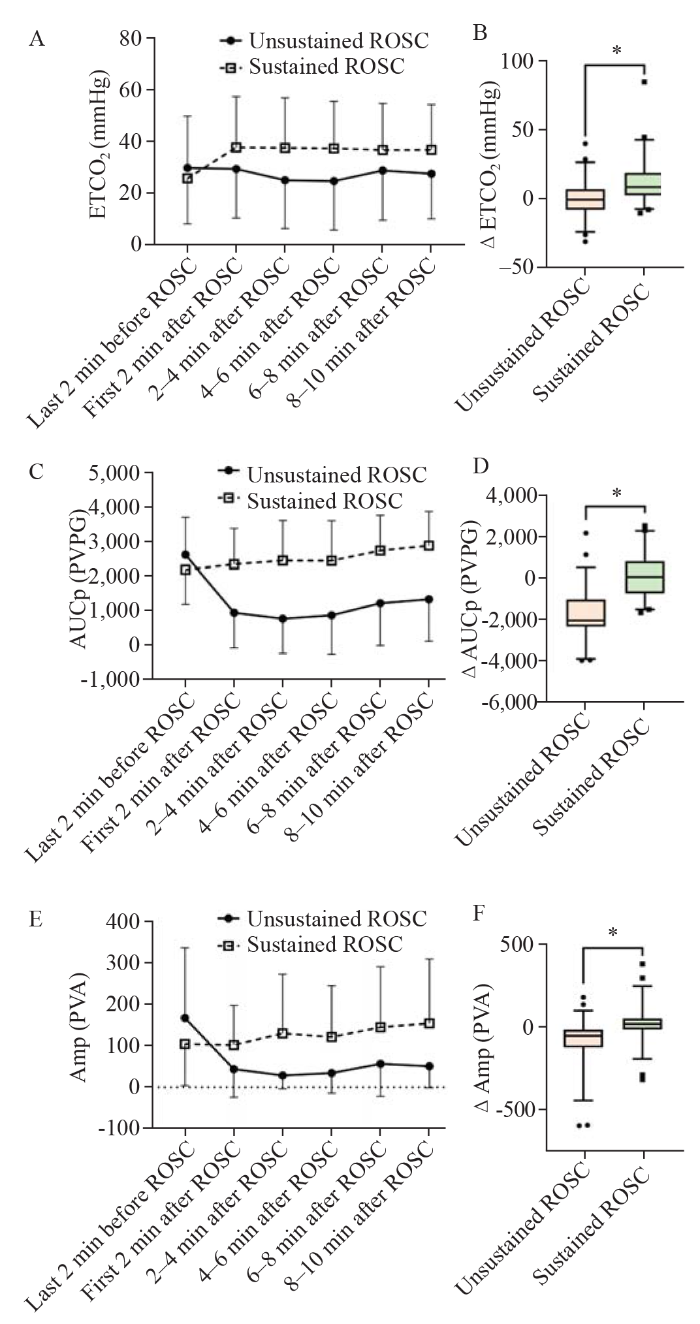
The mean ETCO2, AUCp, and Amp in both groups were recorded every two minutes from 2 min before ROSC to 10 min after ROSC, as shown in Figure 2. For all 105 ROSC episodes, the mean ETCO2 in the first 2 min after ROSC was significantly higher than that before ROSC (P<0.05). In the sustained ROSC group, the ETCO2 after ROSC was significantly higher than that in the last 2 min before ROSC (P<0.05), whereas in the unsustained ROSC group, there was no significant change. In the unsustained ROSC group, the AUCp and Amp after ROSC were significantly lower than those before ROSC (P<0.001). In the sustained ROSC group, however, the Amp remained stable, and the AUCp showed an increasing trend after ROSC (r=0.164, P<0.05). The changes in ETCO2, AUCp, and Amp from 2 min after ROSC to 2 min before ROSC (ΔETCO2, ΔAUCp, and ΔAmp, respectively) were significantly different between the two groups (P<0.05) (Figure 2).
Figure 2.
Figure 2.
Mean parameter values every two minutes from 2 min before ROSC to 10 min after ROSC, and differences of changes in parameter values between 2 min after ROSC and 2 min before ROSC in unsustained and sustained ROSC groups. A: ETCO2; B: ΔETCO2; C: AUCp; D: ΔAUCp; E: Amp; F: ΔAmp. *P<0.05. ROSC: return of spontaneous circulation; ETCO2: end-tidal carbon dioxide; AUCp: area under the curve of pulse oximetry photoplethysmogram; Amp: wave amplitude of pulse oximetry photoplethysmogram; ΔETCO2, ΔAUCp, ΔAmp: change in ETCO2, AUCp and Amp from 2 min after ROSC and 2 min before ROSC. PVPG: pulse oximeter voltage plehtysmography; PVA: pulse oximeter votage amplitude.
Factors relevant to unsustained ROSC
Logistic regression analysis showed that among the eight clinically relevant factors, including patient demographics, in-hospital cardiac arrest (IHCA), cardiac arrest, first CPR (i.e., CPR episode after the first cardiac arrest) and physiological parameters, ΔETCO2 and ΔAUCp were independently associated with sustained ROSC (odds ratio [OR]=0.931, P=0.011 and OR=0.998, P<0.001), while the first CPR was independently associated with unsustained ROSC (OR=4.817, P=0.047) (supplementary Table 1).
Prediction value for unsustained ROSC
The ROC curves were plotted according to the sustainability of ROSC of cardiac arrest patients after initial ROSC, with ΔETCO2 and ΔAUCp as test variables. The results showed that the area under the curves of ΔETCO2, ΔAUCp, and the combination of both to predict unsustained ROSC were 0.752 (95% confidence interval [95% CI] 0.660-0.844), 0.883 (95% CI 0.818-0.948), and 0.902 (95% CI 0.842-0.962), respectively (supplementary Figure 1 and supplementary Table 2).
DISCUSSION
CPR is regarded as the standard procedure for all cardiac arrest patients. However, the state of circulation varies greatly in different patients. We advocate that CPR should not just be a one-size-fits-all process. Physicians should make timely clinical decisions, such as whether to start ECPR based on physiological parameters. Predictors of an increased chance of sustained ROSC include the initial cardiac rhythm, the performance of bystander basic life support, a short interval from scene to hospital, and early defibrillation.[22,23] However, few studies have been performed to investigate the physiological parameters with which to predict the sustainability of ROSC in patients with cardiac arrest in real time. The present multicenter observational study was performed to investigate the ability of physiological parameters (ETCO2 and POP [including Amp and AUCp]) to predict the sustainability of ROSC.
In this study, the rate of ROSC was 32.8%, which falls close to the reported rate of ROSC in the literature of 24% to 44%.[4,24] The incidence of rearrest after previous ROSC in the present study was 51.4%, which is also consistent with the range of 35% to 50% reported in previous studies.[4,7⇓-9,24] Rearrest is a strong predictor of poor outcomes.[25] The 24-hour survival rate was significantly lower in patients in our study with unsustained ROSC than in those with sustained ROSC, and no patients with unsustained ROSC survived to 28 d. Sufficient carbon monoxide (CO) and blood pressure are needed to maintain sustained ROSC. However, high-quality CPR only provides 15% to 25% of normal CO.[3] Prolonged CPR in patients with unsustained ROSC reduces the possibility of ROSC. In patients with unsustained ROSC, early recognition and intervention, such as ECPR, might improve the prognosis by avoiding hypoperfusion due to rearrest and repeated resuscitation. Rearrest is generally diagnosed retrospectively, providing limited opportunities for clinicians to improve outcomes. The novelty of our study is that we attempted to identify patients at high risk of rearrest at an earlier stage by monitoring physiological parameters that are easily accessible and noninvasive.
ETCO2 has been investigated in many previous studies and is regarded as an indicator of ROSC in patients with cardiac arrest.[16,17] Its level reflects tissue metabolism, lung perfusion, and alveolar ventilation, and it is closely related to the quality of CPR and a patient’s prognosis. In this study, the ETCO2 of both groups exceeded 25 mmHg (1 mmHg=0.133 kPa) during CPR, indicating a generally high quality of resuscitation and a good possibility of ROSC. Pokorná et al[26] proposed that ETCO2 after ROSC was significantly higher than before ROSC, and a sudden increase in ETCO2 of >10 mmHg can be used as an indicator for ROSC. In our study, we did observe this “elevated ETCO2 after ROSC” phenomenon. However, when we divided our patients into a sustained ROSC group and an unsustained ROSC group, we found that in the sustained ROSC group, ETCO2 after ROSC was significantly higher than that before ROSC, whereas in the unsustained ROSC group, ETCO2 did not change significantly. The significant increase in ETCO2 in the sustained ROSC group may have occurred for the following reasons: the cardiac index after ROSC may have been higher in the sustained group compared with the unsustained group, which could have caused a sharp rise in ETCO2; in addition, the rapid increase in ETCO2 after ROSC may have been related to CO2 washout from tissues that had been poorly perfused during cardiac arrest.[27] This suggests that patients with sustained ROSC have both better macrocirculation and better microcirculation, which may contribute to the sustainability of ROSC. However, ETCO2 can be affected by various factors, such as cardiac arrest, vasopressor administration, and bicarbonate fluid administration. Thus, an accurate ETCO2 cutoff value for ROSC has not been fully established. Our study showed that the ΔETCO2 had high clinical significance for the identification of unsustained ROSC.
In this study, both the AUCp and Amp of pulse oximetry in patients with unsustained ROSC significantly decreased after initial ROSC, whereas the AUCp and Amp in patients with sustained ROSC remained stable or showed an increasing trend after ROSC. In our previous study, we found that POP parameters, such as AUCp and Amp, could be used to identify ROSC in patients with cardiac arrest.[17] The present study further suggests that AUCp and Amp can be used to identify the sustainability of ROSC. POP parameters have been shown to be associated with peripheral perfusion in critically ill patients in many previous studies.[28⇓-30] Cardiac arrest induces an extreme state of shock, and the macrocirculation needs to be maintained first; the peripheral circulation may need to be sacrificed. When ROSC is achieved, the peripheral circulation improves secondary to the improvement in macrocirculation. Some ROSC patients may be in a state called “central-peripheral separation”. These patients with a low Amp or AUCp despite higher ETCO2, i.e., those with good macrocirculation but poor peripheral circulation, are more likely to have unsustained ROSC. Therefore, POP parameters represent the status of the peripheral circulation and can be used to observe the sustainability of ROSC. In this study, AUCp was a better indicator to predict unsustained ROSC than Amp. The possible reason was that Amp is more susceptible to interference, such as finger movement, making it less reliable than AUCp.
We found that cardiac arrest patients who had both low ETCO2 and low AUCp might not develop ROSC, whereas those with both high ETCO2 and high AUCp were more likely to achieve sustained ROSC. Cardiac arrest patients who have high ETCO2 but low AUCp likely have sufficient macrocirculation but poor peripheral circulation and are at high risk of developing rearrest within a short time. Only patients with improved macro- and micro-circulation can achieve sustained ROSC. Thus, the combination of ΔETCO2 and ΔAUCp may be a good predictor for sustained ROSC.
Our study had some limitations. This was a relatively small sample size observational study. Additionally, our study mainly focused on patients with in-hospital cardiac arrest because the data from these patients were more complete. However, these patients may have had other underlying diseases, and the causes of cardiac arrest may have been different from those of out-of-hospital cardiac arrest, resulting in selection bias. A total of 121 patients were excluded because of incomplete data. A large number of them (34.7%) lacked ETCO2 data, which may reflect the challenge of measuring ETCO2 in the clinical setting.
CONCLUSIONS
In this multicenter observational study of 105 ROSC episodes, more than half of the ROSC episodes resulted in rearrest. Patients with unsustained ROSC had a poorer prognosis than those with sustained ROSC. High ΔETCO2 but low ΔAUCp was associated with unsustained ROSC in cardiac arrest patients after an initial ROSC episode. The combination of ΔETCO2 and ΔAUCp showed a significant predictive value for the sustainability of ROSC.
Funding: This study supported by National Natural Science Foundation of China General Program (82172179), Mathematics Tianyuan Fund (12126604), and Central High-level Hospital Clinical Research Project (2022-PUMCH-B-110).
Ethical approval: The research was carried out in compliance with the Declaration of Helsinki. The study protocol was approved by the ethics committee of the Peking Union Medical College Hospital (approval number: 20131S-512).
Conflicts of interests: The authors have no relevant financial or non-financial interests to disclose.
Contributors: All authors contributed significantly to the writing and revision of this manuscript and approved the final version. JX, YGC and XZY made equal contribution to this study.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Survival from pediatric out-of-hospital cardiac arrest during nights and weekends: an updated Japanese registry-based study
DOI:10.1016/j.jacasi.2022.01.005 URL [Cited within: 1]
Global research trends in cardiac arrest research: a visual analysis of the literature based on CiteSpace
DOI:10.5847/wjem.j.1920-8642.2022.071 URL [Cited within: 1]
Refractory cardiac arrest: where extracorporeal cardiopulmonary resuscitation fits
DOI:10.1097/MCC.0000000000000769
PMID:33027149
[Cited within: 3]

Extracorporeal cardiopulmonary resuscitation (ECPR) is a powerful technique increasingly used to care for patients with refractory cardiac arrest. This review will detail where ECPR fits in the current care of cardiac arrest patients, including the key aspects of ECPR deployment and patient selection shown to maximize its benefit.ECPR has been shown to improve neurologically favourable survival in patients with refractory cardiac arrest in numerous nonrandomized cohort studies. The haemodynamic, oxygenation and ventilation support provided by ECPR eliminates the need for return of spontaneous circulation (ROSC) and prevents ongoing injury from shock or rearrest. However, ECPR is one component of an entire system of resuscitation care necessary for positive outcomes. The intense resources needed require that patient eligibility criteria are well delineated to direct ECPR to patients likely to benefit. The other components of the system, including emergency medical services, cannulation teams and postarrest care teams, also require substantial training and dedication.ECPR is a system of resuscitation care that must be optimized at every level to successfully treat patients with refractory cardiac arrest.
Incidence of rearrest after return of spontaneous circulation in out-of-hospital cardiac arrest
DOI:10.3109/10903127.2010.497902
PMID:20809686
[Cited within: 3]

Return of spontaneous circulation (ROSC) occurs in 35.0 to 61.0% of emergency medical services (EMS)-treated out-of-hospital cardiac arrests (OHCAs); however, not all patients achieving ROSC survive to hospital arrival or discharge. Previous studies have estimated the incidence of some types of rearrest(RA) at 61.0 to 79.0%, and the electrocardiogram (ECG) waveform characteristics of prehospital RA rhythms have not been previously described.We sought to determine the incidence of RA in OHCA, to classify RA events by type, and to measure the time from ROSC to RA. We also conducted a preliminary analysis of the relationship between first EMS-detected rhythms and RA, as well as the effect of RA on survival.The Pittsburgh Regional Clinical Center of the National Heart, Lung, and Blood Institute (NHLBI) -sponsored Resuscitation Outcomes Consortium (ROC) provided cases from a population-based cardiac arrest surveillance program, ROC Epistry. Only OHCA cases of nontraumatic etiology with available and adequate ECG files were included. We analyzed defibrillator-monitor ECG tracings (Philips MRX), patient care reports (PCRs), and defibrillator audio recordings from EMS-treated cases of OHCA spanning the period from October 2006 to December 2008. We identified ROSC and RA through interpretation of ECG tracings and audio recordings. Rearrest events were categorized as ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), asystole, and pulseless electrical activity (PEA) based on ECG waveform characteristics. Proportions of RA rhythms were stratified by first EMS rhythm and compared using Pearson's chi-square test. Logistic regression was used to test the predictive relationship between RA and survival to hospital discharge.Return of spontaneous circulation occurred in 329 of 1,199 patients (27.4% [95.0% confidence interval (CI): 25.0-30.0%]) treated for cardiac arrest. Of these, 113 had ECG tracings that were available and adequate for analysis. Rearrest occurred in 41 patients (36.0% [95.0% CI: 26.0-46.0%]), with a total of 69 RA events. Survival to hospital discharge in RA cases was 23.1% (95.0% CI: 11.1-39.3%), compared with 27.8% (95.0% CI: 17.9-39.6%) in cases without RA. Counts of RA events by type were as follows: 17 VF (24.6% [95% CI: 15.2-36.5%]), 20 pulseless VT (29.0% [95.0% CI: 18.7-41.2%]), 26 PEA (37.0% [95.0% CI: 26.3-50.2%]), and six asystole (8.8% [95.0% CI: 3.3-18.0%]). Rearrest was not predictive of survival to hospital discharge; however, initial EMS rhythm was predictive of RA shockability. The overall median (interquartile range) time from ROSC to RA among all events was 3.1 (1.6-6.3) minutes.In this sample, the incidence of RA was 38.0%. The most common type of RA was PEA. Shockability of first EMS rhythm was found to predict subsequent RA rhythm shockability.
Survival and rearrest in out-of-hospital cardiac arrest patients with prehospital return of spontaneous circulation: a prospective multi-regional observational study
DOI:10.1080/10903127.2020.1733716 URL [Cited within: 1]
Prediction of return of spontaneous circulation in out-of-hospital cardiac arrest with non-shockable initial rhythm using point-of-care testing: a retrospective observational study
DOI:10.5847/wjem.j.1920-8642.2023.031
PMID:36911060
[Cited within: 1]

Out-of-hospital cardiac arrest (OHCA) is a public health concern, and many studies have been conducted on return of spontaneous circulation (ROSC) and its prognostic factors. Rotational thromboelastometry (ROTEM), a point-of-care testing (POCT) method, has been useful for predicting ROSC in patients with OHCA, but very few studies have focused on patients with non-shockable rhythm. We examined whether the parameters of POCT could predict ROSC in patients with OHCA and accompanying non-shockable rhythm.This is a single-center, retrospective observational study. Complete blood count, blood gas, and ROTEM POCT measurements were used. This study included patients with non-traumatic OHCA aged 18 years or older who were transported to the emergency department and evaluated using POCT between January 2013 and December 2021. The patients were divided into the ROSC and non-ROSC groups. Prehospital information and POCT parameters were compared using receiver operating characteristic (ROC) curve analysis, and further logistic regression analysis was performed.Sixty-seven and 135 patients were in the ROSC and non-ROSC groups, respectively. The ROC curves showed a high area under the curve (AUC) for K of 0.77 (95% confidence interval []: 0.71-0.83) and EXTEM amplitude 5 min after clotting time (A5) of 0.70 (95%: 0.62-0.77). The odds ratios for ROSC were as follows: female sex 3.67 (95%: 1.67-8.04); K 0.64 (95%: 0.48-0.84); and EXTEM A5 1.03 (95%: 1.01-1.06).In OHCA patients with non-shockable rhythm, K level and the ROTEM parameter EXTEM A5 may be useful in predicting ROSC.Copyright: © World Journal of Emergency Medicine.
Incidence and outcomes of rearrest following out-of-hospital cardiac arrest
DOI:10.1016/j.resuscitation.2014.10.011
PMID:25447433
[Cited within: 2]

Rearrest occurs when a patient experiences cardiac arrest after successful resuscitation. The incidence and outcomes of rearrest following out-of-hospital cardiac arrest have been estimated in limited local studies. We sought provide a large-scale estimate of rearrest incidence and its effect on survival.We obtained case data from emergency medical services-treated, out-of-hospital cardiac arrest from the Resuscitation Outcomes Consortium, a multi-site clinical research network with clinical centers in 11 regions in the US and Canada. The cohort comprised all cases captured between 2006 and 2008 at 10 of 11 regions with prehospital return of spontaneous circulation. We used three methods to ascertain rearrest via direct signal analysis, indirect signal analysis, and emergency department arrival vital status. Rearrest incidence was estimated as the proportion of cases with return of spontaneous circulation that experience rearrest. Regional rearrest incidence estimates were compared with the χ(2)-squared test. Multivariable logistic regression was used to assess the relationship between rearrest and survival to hospital discharge.Out of 18,937 emergency medical services-assessed cases captured between 2006 and 2008, 11,456 (60.5%) cases were treated by emergency medical services and 4396 (38.4%) had prehospital return of spontaneous circulation. Of these, rearrest ascertainment data was available in 3253 cases, with 568 (17.5%) experiencing rearrest. Rearrest differed by region (10.2% to 21.2%, p < 0.001). Rearrest was inversely associated with survival (OR: 0.19, 95% CI: 0.14-0.26).Rearrest was found to occur frequently after resuscitation and was inversely related to survival.Copyright © 2014 Elsevier Ireland Ltd. All rights reserved.
Rearrest after prehospital resuscitation
Effects of intra-resuscitation antiarrhythmic administration on rearrest occurrence and intra-resuscitation ECG characteristics in the ROC ALPS trial
DOI:S0300-9572(18)30239-9
PMID:29803703
[Cited within: 2]

Intra-resuscitation antiarrhythmic drugs may improve resuscitation outcomes, in part by avoiding rearrest, a condition associated with poor out-of-hospital cardiac arrest (OHCA) outcomes. However, antiarrhythmics may also alter defibrillation threshold. The objective of this study was to investigate the relationship between rearrest and intra-resuscitation antiarrhythmic drugs in the context of the Resuscitation Outcomes Consortium (ROC) amiodarone, lidocaine, and placebo (ALPS) trial.Rearrest rates would be lower in cases treated with amiodarone or lidocaine, versus saline placebo, prior to first return of spontaneous circulation (ROSC). We also hypothesized antiarrhythmic effects would be quantifiable through analysis of the prehospital electrocardiogram.We conducted a secondary analysis of the ROC ALPS trial. Cases that first achieved prehospital ROSC after randomized administration of study drug were included in the analysis. Rearrest, defined as loss of pulses following ROSC, was ascertained from emergency medical services records. Rearrest rate was calculated overall, as well as by ALPS treatment group. Multivariable logistic regression models were constructed to assess the association between treatment group and rearrest, as well as rearrest and both survival to hospital discharge and survival with neurologic function. Amplitude spectrum area, median slope, and centroid frequency of the ventricular fibrillation (VF) ECG were calculated and compared across treatment groups.A total of 1144 (40.4%) cases with study drug prior to first ROSC were included. Rearrest rate was 44.0% overall; 42.9% for placebo, 45.7% for lidocaine, and 43.0% for amiodarone. In multivariable logistic regression models, ALPS treatment group was not associated with rearrest, though rearrest was associated with poor survival and neurologic outcomes. AMSA and median slope measures of the first available VF were associated with rearrest case status, while median slope and centroid frequency were associated with ALPS treatment group.Rearrest rates did not differ between antiarrhythmic and placebo treatment groups. ECG waveform characteristics were correlated with treatment group and rearrest. Rearrest was inversely associated with survival and neurologic outcomes.Copyright © 2018 Elsevier B.V. All rights reserved.
The association of extreme tachycardia and sustained return of spontaneous circulation after nontraumatic out-of-hospital cardiac arrest
Correlation of end-tidal CO2 to cerebral perfusion during CPR
PMID:1514728
[Cited within: 1]

A number of studies have demonstrated a correlation between end-tidal carbon dioxide (ETCO2), cardiac output, and return of spontaneous circulation in experimental animals and in patients undergoing closed-chest CPR. Our study attempted to correlate ETCO2 to cerebral blood flow during cardiac arrest.Sixteen piglets were anesthetized, intubated, and instrumented for cerebral blood flow studies. An ultrasonic flow probe was placed on both internal carotid arteries for continuous flow measurements. The animal was fibrillated, and closed-chest CPR was begun. Continuous ETCO2 measurements were obtained and compared with simultaneous internal carotid, cardiac output, and cerebral blood flow measurements.Correlations between ETCO2 and carotid and cerebral blood flow were determined using Pearson's method. The correlation between ETCO2 and total internal carotid flow was.58 (P =.01, Bonferroni's adjusted P =.30). Correlation between ETCO2 and cerebral blood flow was.64 (P =.01, Bonferroni's adjusted P =.09). A partial correlation coefficient for ETCO2 versus cardiac output was.70, whereas it was only.30 for ETCO2 versus cerebral blood flow.Partial correlation coefficients suggest that ETCO2 correlates with cerebral blood flow when changes in cerebral blood flow parallel changes in cardiac output.
End-tidal carbon dioxide monitoring during cardiopulmonary resuscitation
End-tidal carbon dioxide and outcome of out-of-hospital cardiac arrest
DOI:10.1056/NEJM199712043372314 URL [Cited within: 2]
Partial pressure of end-tidal carbon dioxide successful predicts cardiopulmonary resuscitation in the field: a prospective observational study
DOI:10.1186/cc7009 URL [Cited within: 1]
Association between prehospital CPR quality and end-tidal carbon dioxide levels in out-of-hospital cardiac arrest
DOI:10.3109/10903127.2015.1115929
PMID:26830353
[Cited within: 1]

International Guidelines recommend measurement of end-tidal carbon dioxide (EtCO2) to enhance cardiopulmonary resuscitation (CPR) quality and optimize blood flow during CPR. Numerous factors impact EtCO2 (e.g., ventilation, metabolism, cardiac output), yet few clinical studies have correlated CPR quality and EtCO2 during actual out-of-hospital cardiac arrest (OHCA) resuscitations. The purpose of this study was to describe the association between EtCO2 and CPR quality variables during OHCA.This is an observational study of prospectively collected CPR quality and capnography data from two EMS agencies participating in a statewide resuscitation quality improvement program. CPR quality and capnography data from adult (≥18 years) cardiac resuscitation attempts (10/2008-06/2013) were collected and analyzed on a minute-by-minute basis using RescueNet™ Code Review. Linear mixed effect models were used to evaluate the association between (log-transformed) EtCO2 level and CPR variables: chest compression (CC) depth, CC rate, CC release velocity (CCRV), ventilation rate.Among the 1217 adult OHCA cases of presumed cardiac etiology, 925 (76.0%) had a monitor-defibrillator file with CPR quality data, of which 296 (32.0%) cases had >1 minute of capnography data during CPR. After capnography quality review, 66 of these cases (22.3%) were excluded due to uninterpretable capnography, resulting in a final study sample of 230 subjects (mean age 68 years; 69.1% male), with a total of 1581 minutes of data. After adjustment for other CPR variables, a 10 mm increase in CC depth was associated with a 4.0% increase in EtCO2 (p < 0.0001), a 10 compression/minute increase in CC rate with a 1.7% increase in EtCO2 (p = 0.02), a 10 mm/second increase in CCRV with a 2.8% increase in EtCO2 (p = 0.03), and a 10 breath/minute increase in ventilation rate with a 17.4% decrease in EtCO2 (p < 0.0001).When controlling for known CPR quality variables, increases in CC depth, CC rate and CCRV were each associated with a statistically significant but clinically modest increase in EtCO2. Given the small effect sizes, the clinical utility of using EtCO2 to guide CPR performance is unclear. Further research is needed to determine the practicality and impact of using real-time EtCO2 to guide CPR delivery in the prehospital environment.
The use of end-tidal carbon dioxide (ETCO2) measurement to guide management of cardiac arrest: a systematic review
DOI:10.1016/j.resuscitation.2017.12.003 URL [Cited within: 2]
Pulse oximetry waveform: a non-invasive physiological predictor for the return of spontaneous circulation in cardiac arrest patients —A multicenter, prospective observational study
DOI:10.1016/j.resuscitation.2021.09.032 URL [Cited within: 5]
Cardiopulmonary resuscitation quality: [corrected]improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association
DOI:10.1161/CIR.0b013e31829d8654
PMID:23801105
[Cited within: 1]

The "2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care" increased the focus on methods to ensure that high-quality cardiopulmonary resuscitation (CPR) is performed in all resuscitation attempts. There are 5 critical components of high-quality CPR: minimize interruptions in chest compressions, provide compressions of adequate rate and depth, avoid leaning between compressions, and avoid excessive ventilation. Although it is clear that high-quality CPR is the primary component in influencing survival from cardiac arrest, there is considerable variation in monitoring, implementation, and quality improvement. As such, CPR quality varies widely between systems and locations. Victims often do not receive high-quality CPR because of provider ambiguity in prioritization of resuscitative efforts during an arrest. This ambiguity also impedes the development of optimal systems of care to increase survival from cardiac arrest. This consensus statement addresses the following key areas of CPR quality for the trained rescuer: metrics of CPR performance; monitoring, feedback, and integration of the patient's response to CPR; team-level logistics to ensure performance of high-quality CPR; and continuous quality improvement on provider, team, and systems levels. Clear definitions of metrics and methods to consistently deliver and improve the quality of CPR will narrow the gap between resuscitation science and the victims, both in and out of the hospital, and lay the foundation for further improvements in the future.
Age and sex differences in outcomes after in-hospital cardiac arrest
DOI:10.1016/j.resuscitation.2021.05.017
PMID:34098034
[Cited within: 1]

While specific factors have been associated with outcomes after in-hospital cardiac arrest, the association between sex and outcomes remains debated. Moreover, age-specific sex differences in outcomes have not been fully characterized in this population.Adult patients (≥18 years) with an index in-hospital cardiac arrest were included from the Danish In-Hospital Cardiac Arrest Registry (DANARREST) from January 1st, 2017 to December 31st, 2018. Population-based registries were used to obtain data on patient characteristics, cardiac arrest characteristics, and outcomes. Unadjusted and adjusted estimates for return of spontaneous circulation (ROSC), survival to 30 days, survival to one year, duration of resuscitation, and post-cardiac arrest time-to-death were computed.A total of 3266 patients were included, of which 2041 (62%) patients were male with a median age of 73 years (quartiles: 64, 80). Among 1225 (38%) female patients, the median age was 76 years (quartiles: 67, 83). Younger age was associated with higher odds of ROSC and survival. Sex was not associated with ROSC and survival in the unadjusted analyses. In the adjusted analyses, women had 1.32 (95%CI: 1.12, 1.54) times the odds of survival to 30 days and 1.26 (95%CI: 1.02, 1.57) times the odds of survival to one year compared to men. The overall association between sex and survival did not vary substantially across age categories, although female sex was associated with a higher survival within certain age categories. Among patients who did not achieve ROSC, female sex was associated with a shorter duration of resuscitation, which was more pronounced in younger age categories.In this study of patients with in-hospital cardiac arrest, female sex was associated with a shorter duration of resuscitation among patients without ROSC but a higher survival to 30 days and one year. While the overall association between sex and outcomes did not vary substantially across age categories, female sex was associated with a higher survival within certain age categories.Copyright © 2021 Elsevier B.V. All rights reserved.
Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Councils of Southern Africa)
DOI:10.1161/01.CIR.0000147236.85306.15
PMID:15557386
[Cited within: 1]

Outcome after cardiac arrest and cardiopulmonary resuscitation is dependent on critical interventions, particularly early defibrillation, effective chest compressions, and advanced life support. Utstein-style definitions and reporting templates have been used extensively in published studies of cardiac arrest, which has led to greater understanding of the elements of resuscitation practice and progress toward international consensus on science and resuscitation guidelines. Despite the development of Utstein templates to standardize research reports of cardiac arrest, international registries have yet to be developed. In April 2002, a task force of the International Liaison Committee on Resuscitation (ILCOR) met in Melbourne, Australia, to review worldwide experience with the Utstein definitions and reporting templates. The task force revised the core reporting template and definitions by consensus. Care was taken to build on previous definitions, changing data elements and operational definitions only on the basis of published data and experience derived from those registries that have used Utstein-style reporting. Attention was focused on decreasing the complexity of the existing templates and addressing logistical difficulties in collecting specific core and supplementary (ie, essential and desirable) data elements recommended by previous Utstein consensus conferences. Inconsistencies in terminology between in-hospital and out-of-hospital Utstein templates were also addressed. The task force produced a reporting tool for essential data that can be used for both quality improvement (registries) and research reports and that should be applicable to both adults and children. The revised and simplified template includes practical and succinct operational definitions. It is anticipated that the revised template will enable better and more accurate completion of all reports of cardiac arrest and resuscitation attempts. Problems with data definition, collection, linkage, confidentiality, management, and registry implementation are acknowledged and potential solutions offered. Uniform collection and tracking of registry data should enable better continuous quality improvement within every hospital, emergency medical services system, and community.
An evaluation of pediatric in-hospital advanced life support interventions using the pediatric Utstein guidelines: a review of 203 cardiorespiratory arrests
DOI:10.1007/BF03018242 URL [Cited within: 1]
Prehospital predictors for return of spontaneous circulation in traumatic cardiac arrest
DOI:10.1097/TA.0000000000003474
PMID:34797815
[Cited within: 1]

Traumatic cardiac arrests (TCA) are associated with high mortality and the majority of deaths occur at the prehospital scene. The aim of the present study was to assess, in a pre-hospital physician-led emergency medical system, the factors associated with sustained return of spontaneous circulation (ROSC) in TCA, including advanced life procedures. The secondary objectives were to assess factors associated with 30-day survival in TCA, evaluate neurological recovery in survivors, and describe the frequency of organ donation among patients experiencing a TCA.We conducted a retrospective study of all TCA patients included in the French nationwide cardiac arrest registry from 07/2011 to 11/2020. Multivariable logistic regression analysis was used to identify factors independently associated with ROSC.A total of 120,045 OHCA were included in the registry among which 4,922 TCA were eligible for analysis. ROSC was sustained on-scene in 21.1% (n = 1,037) patients. Factors significantly associated with sustained ROSC were not-asystolic initial rhythms (pulseless electric activity (OR = 1.81, 95%CI [1.40;2.35], p < 0.001), shockable rhythm (1.83 [1.12;2.98], p = 0.016) and spontaneous activity (3.66 [2.70;4.96], p < 0.001)) and gasping at the mobile medical team (MMT) arrival (1.40 [1.02;1.94], p = 0.042). The MMT interventions significantly associated with ROSC were: intravenous fluid resuscitation (3.19 [2.69;3.78], p < 0.001), packed red cells transfusion (2.54 [1.84;3.51], p < 0.001), and external haemorrhage control (1.74 [1.31;2.30], p < 0.001). Among patients who survived (n = 67), neurological outcome at day 30 was favourable (cerebral performance category 1-2) in 72.2% cases (n = 39/54) and 1.4% (n = 67/4,855) of deceased patients donated ≥1 organ.Sustained ROSC was frequently achieved in patients not in asystole at MMT arrival and higher ROSC rates were achieved in patients benefiting from specific advanced life support interventions. Organ donation was somewhat possible in TCA patients undergoing on-scene resuscitation.level III, prognostic and epidemiologic.Copyright © 2021 Lippincott Williams & Wilkins, Inc.
Significant factors in predicting sustained ROSC in paediatric patients with traumatic out-of-hospital cardiac arrest admitted to the emergency department
DOI:10.1016/j.resuscitation.2006.11.022 URL [Cited within: 1]
Factors associated with re-arrest following initial resuscitation from cardiac arrest
DOI:S0300-9572(16)30584-6
PMID:27992736
[Cited within: 2]

To examine patient- and arrest-level factors associated with the incidence of re-arrest in the hospital setting, and to measure the association between re-arrest and survival to discharge.This work represents a retrospective cohort study of adult patients who were successfully resuscitated from an initial out-of-hospital cardiac arrest (OHCA) or in-hospital cardiac arrest (ICHA) of non-traumatic origin at two urban academic medical centers. In this study, re-arrest was defined as loss of a pulse following 20min of sustained return of spontaneous circulation (ROSC).Between 01/2005 and 04/2016, 1961 patients achieved ROSC following non-traumatic cardiac arrest. Of those, 471 (24%) experienced at least one re-arrest. In re-arrest patients, the median time from initial ROSC to first re-arrest was 5.4h (IQR: 1.1, 61.8). The distribution of initial rhythms between single- and re-arrest patients did not vary, nor did the median duration of initial arrest. Among 108 re-arrest patients with an initial shockable rhythm, 60 (56%) experienced a shockable re-arrest rhythm. Among 273 with an initial nonshockable rhythm, 31 (11%) experienced a shockable re-arrest rhythm. After adjusting for significant covariates, the incidence of re-arrest was associated with a lower likelihood of survival to discharge (OR: 0.32; 95% CI: 0.24-0.43; p<0.001).Re-arrest is a common complication experienced by cardiac arrest patients that achieve ROSC, and occurs early in the course of their post-arrest care. Moreover, re-arrest is associated with a decreased likelihood of survival to discharge, even after adjustments for relevant covariates.Copyright © 2016 Elsevier Ireland Ltd. All rights reserved.
Rearrest during hospitalisation in adult comatose out-of-hospital cardiac arrest patients: risk factors and prognostic impact, and predictors of favourable long-term outcomes
DOI:10.1016/j.resuscitation.2021.11.037 URL [Cited within: 1]
A sudden increase in partial pressure end-tidal carbon dioxide (P(ET)CO(2)) at the moment of return of spontaneous circulation
DOI:10.1016/j.jemermed.2009.04.064
PMID:19570645
[Cited within: 1]

Previous studies established that a level of partial pressure end-tidal carbon dioxide (P(ET)CO(2)) of 10 mm Hg divided patients undergoing advanced life support (ALS) into those likely to be resuscitated (values > 10 mm Hg) and those likely to die during ALS (values < 10 mm Hg).The study tested the significance of a sudden increase in the P(ET)CO(2) in signaling the return of spontaneous circulation (ROSC) during ALS.P(ET)CO(2) values were continuously recorded during ALS in out-of-hospital patients with cardiac arrest. Constant ventilation was maintained by an automatic device. There were 108 patients, representing two extreme outcomes of ALS, who were subdivided into two groups. The first group included 59 patients with a single ROSC followed by a stable spontaneous circulation. The second group included 49 patients with no signs of ROSC.ROSC was associated with a sudden increase in P(ET)CO(2) that remained significantly higher than before ROSC. P(ET)CO(2) did not rise during the entire ALS in the second group of patients without ROSC and was lower than in the first group of patients.In constantly ventilated patients, P(ET)CO(2) is significantly higher (about 10 mm Hg) after ROSC than before ROSC. A sudden increase in P(ET)CO(2) exceeding 10 mm Hg may indicate ROSC. Consequently, the rule of 10 mm Hg may be extended to include a sudden increase in continuously recorded P(ET)CO(2) by more than 10 mm Hg as an indicator of the possibility of ROSC.Copyright 2010 Elsevier Inc. All rights reserved.
Expired carbon dioxide: a noninvasive monitor of cardiopulmonary resuscitation
PMID:3121209
[Cited within: 1]

End-tidal CO2 concentration (ETCO2) may serve as a simple noninvasive measurement of the blood flow generated by precordial compression during cardiopulmonary resuscitation (CPR). In a mechanically ventilated porcine preparation of ventricular fibrillation, onset of fibrillation was associated with a rapid decrease in ETCO2 from 4.0 +/- 0.2% to less than 0.7 +/- 0.2%. With precordial compression, it increased to 1.9 +/- 0.3%. Animals that were successfully defibrillated after 12 min of CPR demonstrated an immediate increase in ETCO2. The ETCO2 increased from 1.9 +/- 0.3% to 4.9 +/- 0.3% over an interval of between 30 and 60 sec. These changes in ETCO2 were closely related to proportionally similar decreases and increases in cardiac output (CO), and a close correlation between ETCO2 and CO was demonstrated (r =.92). A similar highly significant correlation between ETCO2 and CO was also demonstrated during open-chest cardiac massage (r =.95). ETCO2 therefore serves as a noninvasive measure of pulmonary blood flow and therefore CO. In 17 successfully resuscitated animals. ETCO2 during precordial compression averaged 1.7 +/- 0.2%, whereas it was only 0.5 +/- 0.1% in five animals in whom resuscitation procedures were unsuccessful (p less than.001). Accordingly, ETCO2 prognosticates outcome during CPR and immediately identifies restoration of spontaneous circulation.
Analysis of the ear pulse oximeter waveform
DOI:10.1007/s10877-006-9018-z
PMID:16612551
[Cited within: 1]

For years researchers have been attempting to understand the relationship between central hemodynamics and the resulting peripheral waveforms. This study is designed to further understanding of the relationship between ear pulse oximeter waveforms, finger pulse oximeter waveforms and cardiac output (CO). It is hoped that with appropriate analysis of the peripheral waveforms, clues can be gained to help to optimize cardiac performance.Part 1: Studying the effect of cold immersion test on plethysmographic waveforms. Part 2: Studying the correlation between ear and finger plethysmographic waveforms and (CO) during CABG surgery. The ear and finger plethysmographic waveforms were analyzed to determine amplitude, width, area, upstroke and downslope. The CO was measured using continuous PA catheter. Using multi-linear regression, ear plethysmographic waveforms, together with heart rate (HR), were used to determine the CO Agreement between the two methods of CO determination was assessed.Part 1: On contralateral hand immersion, all finger plethysmographic waveforms were reduced, there was no significant change seen in ear plethysmographic waveforms, except an increase in ear plethysmographic width. Part 2: Phase 1: Significant correlation detected between the ear plethysmographic width and other ear and finger plethysmographic waveforms. Phase 2: The ear plethysmographic width had a significant correlation with the HR and CO. The correlation of the other ear plethysmographic waveforms with CO and HR are summarized (Table 5). Multi-linear regression analysis was done and the best fit equation was found to be: CO=8.084 - 14.248 x Ear width + 0.03 x HR+ 92.322 x Ear down slope+0.027 x Ear Area Using Bland & Altman, the bias was (0.05 L) but the precision (2.46) is large to be clinically accepted.The ear is relatively immune to vasoconstrictive challenges which make ear plethysmographic waveforms a suitable monitor for central hemodynamic changes. The ear plethysmographic width has a good correlation with CO.
Utility of the photoplethysmogram in circulatory monitoring
DOI:10.1097/ALN.0b013e31816c89e1
PMID:18431132
[Cited within: 1]

The photoplethysmogram is a noninvasive circulatory signal related to the pulsatile volume of blood in tissue and is displayed by many pulse oximeters and bedside monitors, along with the computed arterial oxygen saturation. The photoplethysmogram is similar in appearance to an arterial blood pressure waveform. Because the former is noninvasive and nearly ubiquitous in hospitals whereas the latter requires invasive measurement, the extraction of circulatory information from the photoplethysmogram has been a popular subject of contemporary research. The photoplethysmogram is a function of the underlying circulation, but the relation is complicated by optical, biomechanical, and physiologic covariates that affect the appearance of the photoplethysmogram. Overall, the photoplethysmogram provides a wealth of circulatory information, but its complex etiology may be a limitation in some novel applications.
Pulse oximeter plethysmographic waveform changes in awake, spontaneously breathing, hypovolemic volunteers
DOI:10.1213/ANE.0b013e3181cb3f4a
PMID:20103539
[Cited within: 1]

The primary objective of this study was to determine whether alterations in the pulse oximeter waveform characteristics would track progressive reductions in central blood volume. We also assessed whether changes in the pulse oximeter waveform provide an indication of blood loss in the hemorrhaging patient before changes in standard vital signs.Pulse oximeter data from finger, forehead, and ear pulse oximeter sensors were collected from 18 healthy subjects undergoing progressive reduction in central blood volume induced by lower body negative pressure (LBNP). Stroke volume measurements were simultaneously recorded using impedance cardiography. The study was conducted in a research laboratory setting where no interventions were performed. Pulse amplitude, width, and area under the curve (AUC) features were calculated from each pulse wave recording. Amalgamated correlation coefficients were calculated to determine the relationship between the changes in pulse oximeter waveform features and changes in stroke volume with LBNP.For pulse oximeter sensors on the ear and forehead, reductions in pulse amplitude, width, and area were strongly correlated with progressive reductions in stroke volume during LBNP (R(2) ≥ 0.59 for all features). Changes in pulse oximeter waveform features were observed before profound decreases in arterial blood pressure. The best correlations between pulse features and stroke volume were obtained from the forehead sensor area (R(2) = 0.97). Pulse oximeter waveform features returned to baseline levels when central blood volume was restored.These results support the use of pulse oximeter waveform analysis as a potential diagnostic tool to detect clinically significant hypovolemia before the onset of cardiovascular decompensation in spontaneously breathing patients.