INTRODUCTION
Cardiac arrest (CA) is the leading cause of morbidity and mortality worldwide.[1,2] It has been reported that approximately 9.1% of individuals with out-of-hospital CA (OHCA) and 18.8% of patients with in-hospital CA (IHCA) survive to hospital discharge.[3] Despite the main advances in cardiopulmonary resuscitation (CPR) practice over the past few decades, the rate of survival with favorable neurological outcomes after CA has remained poor.[3] Extracorporeal CPR (ECPR) can be initiated to restore perfusion, taking the limit of hypoxic-ischemic brain injury and allowing for the possible identification and treatment of the underlying causes of CA as its goal.[4] ECPR may be considered a rescue therapy for selected patients when conventional CPR (CCPR) fails.[5] A meta-analysis suggested that when compared to CCPR, ECPR produced more survivors at hospital discharge, and among those survivors, more were neurologically intact.[6] Early neuro-prognostication after CA would help clinicians choose a proper therapy strategy and perform early assessment of outcomes for patients.[7]
Various serum biomarkers, such as neuron-specific enolase (NSE) and S-100β protein, appear to have prognostic value in the prediction of unfavorable outcomes after CA.[8] However, no consensus has been reached on a threshold value.[9] The ion shift index (ISI) is recommended as a prognostic indicator of ischemic injury severity, defined as the ratio between the ion concentrations of intracellular fluid (ICF), including serum potassium, magnesium, and phosphate, and those of extracellular fluid (ECF), namely, serum calcium.[10] The present study was designed to assess the prognostic value of the ISI in the prediction of unfavorable neurological outcomes at hospital discharge in comatose CA patients following ECPR and to compare the power to other prognostic predictors.
METHOD
Study population
A retrospective observational study of adult (age ≥18 years old) refractory OHCA and IHCA patients who underwent ECPR from January 2018 to December 2022 in a tertiary hospital was conducted. According to the inclusion criteria of ECPR implementation,[11] eligible patients were treated with veno-arterial extracorporeal membrane oxygenation (ECMO) through the femoral vein and artery if return of spontaneous circulation (ROSC) was not achieved more than 10 min after CCPR. Among these, the following patients were excluded: (1) those whose ECMO support duration was less than 12 h; (2) those who experienced CA due to electrolyte/acid-base disturbances, such as hyperkalemia/hypokalemia or diabetic ketoacidosis; (3) those whose levels of serum electrolytes within 6 h following ECMO pump-on were not available; (4) those who had pre-existing medical conditions that might affect the levels of serum electrolytes, such as chronic kidney disease; (5) those who received potassium, magnesium, calcium or sodium bicarbonate ahead of blood sampling; or (6) those whose information about CA characteristics and other prognostic predictors were incomplete.
This study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2020-SR-226).
Data collection
Clinical data, including age, sex, comorbidities, CA location, witnessed status, bystander CPR, etiology of CA, initial rhythm, resuscitation duration (from CCPR to ECMO pump-on), Glasgow Coma Scale (GCS) score after ECPR, and ECMO duration, were systematically collected from patients’ medical records. Laboratory data were obtained within 6 h after ECMO pump-on, including serum electrolytes (potassium, magnesium, phosphate and calcium), hemoglobin, pH, lactate, glucose, albumin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin, and creatinine. The levels of serum electrolytes were detected by an automatic biochemical analyzer (AU5400, Olympus, Japan) at the hospital laboratory. The ISI was obtained by the following equation [9]:
The available prognostic predictors, including clinical examination, gray-to-white matter ratio (GWR) through brain computed tomography scan and serum NSE, were evaluated so that the prognostic performance of ISI can be compared with that of other prognostic predictors. The indicators of unfavorable neurological outcome were considered when either of the following appeared: pupillary/corneal reflex absence, absent motor response or extensor posturing to external stimuli (GCS-motor response [GCS-M]≤2). Excluding the effects of sedatives or neuromuscular blocking drugs, pupillary/corneal reflexes and GCS-M should be confirmed at least 72 h after CA. Moreover, the GWR at the level of the basal ganglia was obtained using the method mentioned in our previous study.[12] The highest values of serum NSE within 72 h after CA were collected for neuro-prognostication.[13]
Outcome
The primary endpoint of our study was neurological status at hospital discharge, which was assessed according to the Cerebral Performance Category (CPC) score.[14] An investigator blinded to the study hypothesis determined the CPC score by reviewing electronic medical records. The patients were classified into either a favorable neurological outcome (CPC 1-2) group or an unfavorable outcome (CPC 3-5) group.
Statistical analysis
Continuous variables are presented as the mean±standard deviation (SD) or median with interquartile range (IQR) depending on their normality, which was assessed by the Kolmogorov-Smirnov test. Categorical variables were described as frequencies with percentages (%). Comparisons of the characteristics between the two groups were made using the χ2 test for categorical variables and the t-test or non-parametric Mann-Whitney U-test for continuous variables, as appropriate. Correlation analysis was performed using Spearman’s rank correlation coefficient. A multivariate logistic regression model was constructed by variable selection following a backward stepwise procedure. Variables with P<0.10 in the univariate analysis (i.e., OHCA, resuscitation duration, ALT, pH, lactate, and ISI) were included in the multivariate regression model. Variables that were closely related to those already included in the model were excluded. The results of the logistic regression analysis were summarized using odds ratios (ORs) and 95% confidence intervals (95% CIs). Receiver-operating characteristic (ROC) curves were plotted to determine the performances of ISI alone, the multivariate logistic regression model (i.e., ISI in combination with other predictors), individual electrolytes in the index (potassium, magnesium, phosphate, and calcium), lactate, and those of other indicators in predicting unfavorable neurological outcome (GWR and NSE). The area under the curve (AUC) of ISI and those of other variables were calculated and compared by using DeLong’s test.[15] The optimal cutoff values of variables were determined on the basis of the maximal sensitivity and specificity. All statistical tests were processed using SPSS (version 23.0, SPSS Inc., USA) and MedCalc (version 20, MedCalc Software Ltd., Belgium) software. A two-tailed P-value <0.05 was considered statistically significant.
RESULTS
Clinical and laboratory characteristics
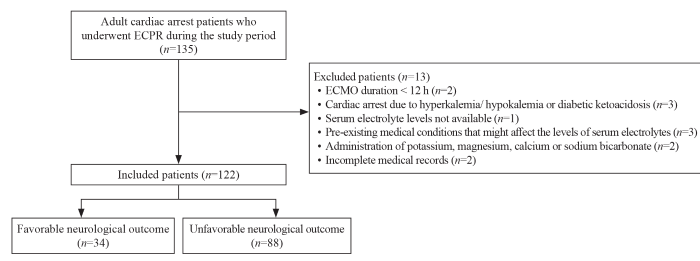
A total of 135 adult CA patients who underwent ECPR were enrolled during the study period. Among them, 13 patients were excluded, as described in Figure 1, and 122 patients were included in our study. Forty-six (37.7%) patients experienced OHCA. According to the CPC score at hospital discharge, 34 patients (27.9%) were in the favorable neurological outcome group, and 88 (72.1%) were in the unfavorable outcome group. The clinical and laboratory characteristics of the involved patients are presented in Table 1.
Figure 1.
Figure 1.
Flow chart of patient enrollment. ECPR: extracorporeal cardiopulmonary resuscitation; ECMO: extracorporeal membrane oxygenation.
Table 1. Clinical and laboratory characteristics of enrolled patients
| Characteristics | Favorable neurological outcome (n=34) | Unfavorable neurological outcome (n=88) | t/χ2/Z | P-value |
|---|---|---|---|---|
| Age, years, mean±SD | 52.35±14.76 | 49.28±17.02 | 0.925 | 0.357 |
| Male, n (%) | 22 (64.7) | 67 (76.1) | 1.624 | 0.203 |
| Comorbidities, n (%) | ||||
| Hypertension | 14 (41.2) | 30 (34.1) | 0.534 | 0.465 |
| Diabetes | 8 (23.5) | 17 (19.3) | 0.267 | 0.605 |
| Coronary artery disease | 2 (5.9) | 8 (9.1) | 0.045 | 0.833 |
| OHCA, n (%) | 7 (20.6) | 39 (44.3) | 5.880 | 0.015 |
| Witnessed, n (%) | 34 (100) | 80 (90.9) | 1.991 | 0.158 |
| Bystander CPR, n (%) | 34 (100) | 73 (83.0) | 5.122 | 0.024 |
| Cardiac etiology, n (%) | 27 (79.4) | 68 (77.3) | 0.065 | 0.799 |
| Initial non-shockable rhythm, n (%) | 23 (67.6) | 44 (50.0) | 3.085 | 0.079 |
| Resuscitation duration, min, median (IQR) | 40.5 (17.5-55.0) | 50.0 (34.0-82.3) | -2.639 | 0.008 |
| ECMO duration, h, median (IQR) | 141.5 (122.8-187.8) | 94.4 (49.3-169.3) | -3.278 | 0.001 |
| Length of stay in hospital, d, median (IQR) | 19 (15-27) | 5 (3-11) | -6.609 | <0.001 |
| GCS score after ECPR, median (IQR) | 9 (8-12) | 3 (3-4) | -7.765 | <0.001 |
| Prognostic predictors | ||||
| GCS-M ≤2, n (%) | 5 (14.7) | 81 (92.0) | 70.522 | <0.001 |
| Pupillary/corneal reflex absence, n (%) | 0 (0) | 51 (58.0) | 33.859 | <0.001 |
| GWR-basal ganglia, median (IQR) | 1.25 (1.20-1.27) | 1.14 (1.08-1.19) | -5.977 | <0.001 |
| NSE, ng/mL, median (IQR) | 44.6 (38.3-60.7) | 188.5 (88.1-370.0) | -6.972 | <0.001 |
| Laboratory parameters, median (IQR) | ||||
| Hemoglobin, g/L | 116.5 (101.0-132.3) | 111.0 (84.0-129.0) | -1.385 | 0.166 |
| pH | 7.41 (7.31-7.52) | 7.22 (6.96-7.36) | -4.046 | <0.001 |
| Lactate, mmol/L | 3.1 (1.1-11.5) | 10.2 (4.0-15.6) | -2.854 | 0.004 |
| Glucose, mmol/L | 9.5 (6.7-11.7) | 10.1 (7.1-13.5) | -0.504 | 0.614 |
| Albumin, g/L | 33.8 (30.3-39.3) | 31.8 (26.5-39.2) | -1.008 | 0.313 |
| ALT, U/L | 159.0 (102.1-309.6) | 306.1 (120.5-801.5) | -2.438 | 0.015 |
| Aspartate aminotransferase, U/L | 420.3 (170.1-932.0) | 926.7 (364.6-2176.5) | -2.889 | 0.004 |
| Total bilirubin, μmol/L | 14.0 (10.8-19.9) | 20.1 (13.1-32.2) | -2.204 | 0.028 |
| Creatinine, μmol/L | 96.1 (69.0-137.7) | 76.5 (103.2-148.2) | -1.074 | 0.283 |
| Potassium, mmol/L | 3.9 (3.6-4.3) | 4.5 (3.8-5.2) | -3.489 | <0.001 |
| Magnesium, mmol/L | 0.9 (0.8-1.0) | 1.0 (0.9-1.1) | -1.994 | 0.046 |
| Phosphate, mmol/L | 1.0 (0.7-1.2) | 1.2 (0.8-2.1) | -2.778 | 0.005 |
| Calcium, mmol/L | 2.1 (2.0-2.2) | 1.9 (1.6-2.1) | -3.907 | <0.001 |
| Ion shift index | 2.69 (2.51-3.07) | 3.74 (3.15-4.57) | -6.504 | <0.001 |
SD: standard deviation; OHCA: out-of-hospital cardiac arrest; CPR: cardiopulmonary resuscitation; IQR: interquartile range; ECMO: extracorporeal membrane oxygenation; GCS: Glasgow Coma Scale; ECPR: extracorporeal cardiopulmonary resuscitation; GCS-M: Glasgow Coma Scale motor score; GWR: gray-to-white matter ratio; NSE: neuron-specific enolase; ALT: alanine aminotransferase.
Prognostic factors related to unfavorable neurological outcome
In the univariate analysis, OHCA, initial non-shockable rhythm, resuscitation duration, ALT, pH, lactate, and ISI were related to an unfavorable neurological outcome at hospital discharge. In the multivariate logistic regression analysis (Table 2), a higher ISI level was independently related to unfavorable outcome at hospital discharge (OR 6.529, 95% CI 2.239-19.044, P=0.001).
Table 2. Final model of the multivariate logistic regression analyses for unfavorable neurological outcome
| Parameters | Coefficient | OR | 95% CI | P-value |
|---|---|---|---|---|
| Initial non-shockable rhythm | 1.581 | 4.862 | 1.249-18.927 | 0.023 |
| ALT, U/L | 0.002 | 1.002 | 0.999-1.005 | 0.065 |
| pH | 8.986 | 0.001 | 0.001-0.036 | 0.002 |
| Lactate, mmol/L | 0.155 | 1.168 | 0.990-1.378 | 0.066 |
| Ion shift index | 1.876 | 6.529 | 2.239-19.044 | 0.001 |
ALT: alanine aminotransferase; OR: odds ratio; CI: confidence interval.
Prognostic performance of ISI
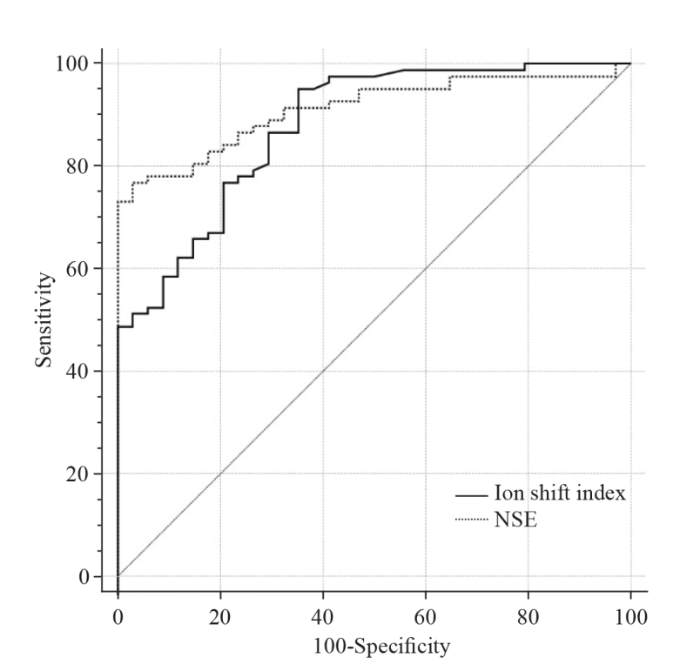
Spearman’s correlation analysis showed that the level of ISI was significantly correlated with resuscitation duration (r=0.408, P<0.001) and lactate (r=0.431, P<0.001). The prognostic performances of variables in the prediction of unfavorable neurological outcome are summarized in supplementary Table 1 and Figure 2. An ISI level >3.12 predicted unfavorable outcomes with a sensitivity and specificity of 74.6% and 85.2%, respectively (P<0.001). The AUC of ISI was 0.887 (95% CI 0.817-0.956), which was significantly greater than that of individual electrolytes included in the index as well as that of lactate (P<0.05). Moreover, the AUC of ISI was comparable to that of other predictors, such as GWR (0.850, 95% CI 0.783-0.918, P=0.433) and NSE (0.925, 95% CI 0.876-0.975, P=0.394).
Figure 2.
Figure 2.
Receiver-operating characteristic curves for the ion shift index and NSE in predicting unfavorable outcome. NSE: neuron-specific enolase.
Prognostic performance of ISI in combination with other predictors
The AUC of the multivariate logistic regression model involving ISI was 0.945 (95% CI 0.899-0.990), which was significantly higher than that of ISI alone (P<0.001). ISI in combination with other predictors (OHCA, initial non-shockable rhythm, resuscitation duration, ALT, pH, and lactate) showed a more promising prognostic performance.
DISCUSSION
ECPR is an invasive and resource-intensive therapy that requires highly specialized equipment and personnel and is expensive. Therefore, accurate prognostication is necessary to avoid an improper withdrawal of life-sustaining treatment in patients still having the possibility of a neurologically meaningful recovery and to avoid excessive treatment in those patients undergoing a severe and irreversible neurological injury.[16] Several approaches, including electrophysiological tests, neuroimaging, and serum brain-specific biomarkers, have been applied to accurately predict the outcomes of CA survivors. However, the application of these tools is not available during the early hours after ROSC.
Electrolyte disturbances are common in CA survivors. The maintenance of cellular ion homeostasis is achieved by membrane-bound energy-dependent ion pumps. Hypoxic-ischemic injury due to CA leads to cell membrane dysfunction and homeostasis loss.[9] The depletion of high-energy phosphate in the process of ischemia results in failure of the ion pumps that are used to keep ionic gradients across cell membranes. As a result, ion shifts between the compartments of ICF and ECF occur. In the early stage of hypoxia, when there is no inhibition of the sodium-potassium-adenosine triphosphate (ATP) pump or cell injury, ATP breakdown leads to rapid production of phosphate, and the potassium and magnesium ions in the ICF flow out. This is followed by the inflow of calcium, sodium, and chloride ions in the ECF and a further loss of magnesium and potassium ions in the cytoplasm in accordance with ion pump dysfunction and cell injury.[17] In the irreversible stage of cell injury, the increased permeability of the cell membrane causes the influx of extracellular calcium, and as a result, the damage to the cytoskeleton and mitochondria deteriorates, which finally leads to cell death.[18]
Electrolyte levels have been studied as predictors of outcome and cell injury severity. Previous studies demonstrated that mono-electrolyte levels, such as potassium and phosphate, were significantly associated with outcomes among CA survivors.[19] However, because the denominator and numerator in the ratio alter in opposite directions, ISI may be better in reflecting the extent of ion shift after ischemia than a single electrolyte level. In previous studies, it was shown that a higher ISI was related to unfavorable neurological outcomes in CA survivors,[10,17] suggesting that the ISI may be a new alternative choice for assessing prognosis. Similar to those findings, our study demonstrated that the ISI was significantly higher in the unfavorable neurological outcome group than in the favorable outcome group in an ECPR setting. An ISI level >3.12 predicted unfavorable outcome with a sensitivity of 74.6% and a specificity of 85.2%. In addition, the ISI had significantly better prognostic power in the prediction of unfavorable outcome than mono-electrolyte levels, indicating the advantage of ISI as a prognostic indicator compared to a single electrolyte.
The levels of lactate have been traditionally chosen as a biomarker of hypoxic-ischemic damage and are a known predictor related to outcomes in CA survivors.[20] In the present study, ISI showed significantly better predictive power than lactate. Furthermore, current guidelines suggest that prognostic predictors, i.e., reduced GWR on brain CT as well as high values of NSE within 72 h after CA should be applied in predicting unfavorable neurological outcomes.[21] Our study demonstrated that ISI exhibited comparable prognostic performance to GWR and NSE in predicting neurological outcomes at hospital discharge in CA patients following ECPR, indicating that the ISI level could be used as an objective prognostic biomarker that can be available early after ECPR. Apart from that, the calculation of ISI is relatively easy and only needs information on serum levels of electrolytes, which can be promptly determined in most hospital laboratories.
In this study, the multivariate analysis revealed that higher ISI levels were significantly associated with unfavorable outcomes, and the multivariate model involving the ISI and other significant indicators presented an enhanced prognostic performance compared to the ISI alone. These findings suggested a possible role for ISI in conjunction with other predictors instead of ISI alone. ISI could provide additional prognostic information and could be used in combination with other indicators (clinical examination, neurophysiology, and neuroimaging) to predict outcome after CA. Further studies that combine the ISI with other variables to predict neurological outcomes in CA survivors are needed.
Limitations
There are several limitations in our study. First, this was a retrospective study of ECPR patients from a single center with a relatively small sample size. Some CA variables (witnessed status and initial non-shockable rhythm) showed no significant differences between the two groups. Further prospective multicenter studies are needed to enhance the generalizability of these findings. Second, the serum total calcium level was involved in the ISI calculation, as most of the patients had no available data on ionized calcium levels. It might have some effect on the results since the concentration of total calcium may not precisely embody the physiologic changes after ECPR. Third, the serum electrolyte levels and other prognostic factors were accessible to treating physicians and might have interfered with clinical decision-making, which may possibly result in a self-fulfilling prophecy. Fourth, although this study excluded patients who had pre-existing chronic kidney disease and those who had experienced CA secondary to electrolyte/acid-base disturbances, other medical conditions, such as parathyroid disease and chronic diarrhea, as well as medications, including furosemide and spironolactone, may lead to pre-CA electrolyte derangements and could affect the results. Finally, the endpoint was neurological status at hospital discharge in this study. Longer-term endpoints should be determined for more accurate prediction.
CONCLUSIONS
A higher ISI level was independently related to unfavorable neurological outcome at hospital discharge. ISI in combination with other prognostic indicators could be used as an alternative approach in the prediction of neurological outcomes in CA patients following ECPR.
Funding: This study was supported by the Key Laboratory of Emergency and Trauma (Hainan Medical University), Ministry of Education (KLET-202202).
Ethical approval: The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2020-SR-226).
Conflicts of interest: The authors have no conflicts of interest to declare.
Contributors: GNW and ZW contributed equally to this work and share first authorship. GNW and YM proposed and designed the study. YZ, ZMZ and WL analyzed and interpreted the data. GNW and ZW wrote the primary draft of the manuscript. XFC and YM revised the manuscript. All authors read and approved the final version of the manuscript.
Reference
Heart disease and stroke statistics-2023 update: a report from the American heart association
Survival from pediatric out-of-hospital cardiac arrest during nights and weekends: an updated Japanese registry-based study
DOI:10.1016/j.jacasi.2022.01.005 URL [Cited within: 1]
Heart disease and stroke statistics-2023 update: a report from the American Heart Association
Early extracorporeal CPR for refractory out-of-hospital cardiac arrest
DOI:10.1056/NEJMoa2204511 URL [Cited within: 1]
Extracorporeal cardiopulmonary resuscitation in adults: evidence and implications
DOI:10.1007/s00134-021-06514-y [Cited within: 1]
Refractory out-of-hospital cardiac arrest and extracorporeal cardiopulmonary resuscitation: a meta-analysis of randomized trials
DOI:10.1111/aor.v47.5 URL [Cited within: 1]
Outcome and prognostication after cardiac arrest
DOI:10.1111/nyas.v1508.1 URL [Cited within: 1]
Neuron-specific enolase and S100B: the earliest predictors of poor outcome in cardiac arrest
DOI:10.3390/jcm11092344
URL
[Cited within: 1]

Background: Proper prognostication is critical in clinical decision-making following out-of-hospital cardiac arrest (OHCA). However, only a few prognostic tools with reliable accuracy are available within the first 24 h after admission. Aim: To test the value of neuron-specific enolase (NSE) and S100B protein measurements at admission as early biomarkers of poor prognosis after OHCA. Methods: We enrolled 82 consecutive patients with OHCA who were unconscious when admitted. NSE and S100B levels were measured at admission, and routine blood tests were performed. Death and poor neurological status at discharge were considered as poor clinical outcomes. We evaluated the optimal cut-off levels for NSE and S100B using logistic regression and receiver operating characteristic (ROC) analyses. Results: High concentrations of both biomarkers at admission were significantly associated with an increased risk of poor clinical outcome (NSE: odds ratio [OR] 1.042 per 1 ng/dL, [1.007–1.079; p = 0.004]; S100B: OR 1.046 per 50 pg/mL [1.004–1.090; p < 0.001]). The dual-marker approach with cut-off values of ≥27.6 ng/mL and ≥696 ng/mL for NSE and S100B, respectively, identified patients with poor clinical outcomes with 100% specificity. Conclusions: The NSE and S100B-based dual-marker approach allowed for early discrimination of patients with poor clinical outcomes with 100% specificity. The proposed algorithm may shorten the time required to establish a poor prognosis and limit the volume of futile procedures performed.
Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis
DOI:10.1007/s00134-021-06548-2
PMID:34705079
[Cited within: 3]

Post-cardiac arrest brain injury (PCABI) is caused by initial ischaemia and subsequent reperfusion of the brain following resuscitation. In those who are admitted to intensive care unit after cardiac arrest, PCABI manifests as coma, and is the main cause of mortality and long-term disability. This review describes the mechanisms of PCABI, its treatment options, its outcomes, and the suggested strategies for outcome prediction.© 2021. The Author(s).
Ion shift index as a promising prognostic indicator in adult patients resuscitated from cardiac arrest
DOI:S0300-9572(18)31038-4
PMID:30807816
[Cited within: 2]

Several studies reported that disturbances in cellular ion homeostasis occur following ischaemia, the magnitude of which was proportional to illness severity. The changes in serum electrolyte levels following ischaemia were minor compared with the changes in ion concentrations in the extracellular fluid. To amplify the serum electrolyte changes, we devised a new index (ion shift index), which could be calculated using commonly measured serum electrolyte levels, and explored its prognostic value in adult cardiac arrest patients.This retrospective observational study included adult cardiac arrest survivors treated at a tertiary university hospital between January 2014 and December 2017. Using the first available serum electrolyte levels, the ion shift index was calculated as follows: ion shift index = (potassium + phosphate + magnesium) / calcium. The primary outcome was poor outcome at hospital discharge (cerebral performance categories 3-5).The area under the receiver operating characteristic curve (AUC) of ion shift index for predicting poor outcome was 0.878 (95% confidence interval [CI], 0.849-0.907). The AUC of ion shift index was greater than those of individual electrolytes (all p < 0.001). In multivariate analysis, higher ion shift index levels were independently associated with poor outcome (odds ratio, 2.916; 95% CI, 1.798-4.730; p < 0.001). The AUC of multivariate model including ion shift index was greater than that of multivariate model after excluding ion shift index (p = 0.007).Our results suggest that the ion shift index can be helpful in the early prognostication of adult cardiac arrest patients.Copyright © 2019 Elsevier B.V. All rights reserved.
Recommendations for extracorporeal cardiopulmonary resuscitation (eCPR): consensus statement of DGIIN, DGK, DGTHG, DGfK, DGNI, DGAI, DIVI and GRC
DOI:10.1007/s00392-018-1366-4
PMID:30361819
[Cited within: 1]

Extracorporeal cardiopulmonary resuscitation (eCPR) may be considered as a rescue attempt for highly selected patients with refractory cardiac arrest and potentially reversible aetiology. Currently, there are no randomised, controlled studies on eCPR. Thus, prospective validated predictors of benefit and outcome are lacking. Currently, selection criteria and procedure techniques differ across hospitals and standardised algorithms are lacking. Based on expert opinion, the present consensus statement provides a first standardised treatment algorithm for eCPR.
The prognostic value of gray-white matter ratio on brain computed tomography in adult comatose cardiac arrest survivors
DOI:10.1016/j.jcma.2018.03.003 URL [Cited within: 1]
The neuron specific enolase (NSE) ratio offers benefits over absolute value thresholds in post-cardiac arrest coma prognosis
DOI:S0967-5868(18)30642-8
PMID:30145080
[Cited within: 1]

Serum neuron-specific enolase (NSE) levels have been shown to correlate with neurologic outcome in comatose survivors of cardiac arrest but use of absolute NSE thresholds is limited. This study describes and evaluates a novel approach to analyzing NSE, the NSE ratio, and evaluates the prognostic utility of NSE absolute value thresholds and trends over time.100 consecutive adult comatose cardiac arrest survivors were prospectively enrolled. NSE levels were assessed at 24, 48, and 72 h post-arrest. Primary outcome was the Glasgow Outcome Score (GOS) at 6 months post-arrest; good outcome was defined as GOS 3-5. Absolute and relative NSE values (i.e. the NSE ratio), peak values, and the trend in NSE over 72 h were analyzed.98 patients were included. 42 (43%) had a good outcome. Five good outcome patients had peak NSE >33 µg/L (34.9-46.4 µg/L). NSE trends between 24 and 48 h differed between outcome groups (decrease by 3.0 µg/L (0.9-7.0 µg/L) vs. increase by 13.4 µg/L (-3.7 to 69.4 µg/L), good vs. poor, p = 0.004). The 48:24 h NSE ratio differed between the good and poor outcome groups (0.8 (0.6-0.9) vs. 1.4 (0.8-2.5), p = 0.001), and a 48:24 h ratio of ≥1.7 was 100% specific for poor outcome.The NSE ratio is a unique method to quantify NSE changes over time. Values greater than 1.0 indicate increasing NSE and may be reflective of ongoing neuronal injury. The NSE ratio obviates the need for an absolute value cut-off.Copyright © 2018 Elsevier Ltd. All rights reserved.
Reliability of the cerebral performance category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study
DOI:10.1186/1757-7241-19-38
[Cited within: 1]

The Cerebral Performance Category (CPC) score is widely used in research and quality assurance to assess neurologic outcome following cardiac arrest. However, little is known about the inter- and intra-reviewer reliability of the CPC.
Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach
PMID:3203132
[Cited within: 1]

Methods of evaluating and comparing the performance of diagnostic tests are of increasing importance as new tests are developed and marketed. When a test is based on an observed variable that lies on a continuous or graded scale, an assessment of the overall value of the test can be made through the use of a receiver operating characteristic (ROC) curve. The curve is constructed by varying the cutpoint used to determine which values of the observed variable will be considered abnormal and then plotting the resulting sensitivities against the corresponding false positive rates. When two or more empirical curves are constructed based on tests performed on the same individuals, statistical analysis on differences between curves must take into account the correlated nature of the data. This paper presents a nonparametric approach to the analysis of areas under correlated ROC curves, by using the theory on generalized U-statistics to generate an estimated covariance matrix.
Prediction of poor neurological outcome in comatose survivors of cardiac arrest: a systematic review
DOI:10.1007/s00134-020-06198-w
PMID:32915254
[Cited within: 1]

To assess the ability of clinical examination, blood biomarkers, electrophysiology, or neuroimaging assessed within 7 days from return of spontaneous circulation (ROSC) to predict poor neurological outcome, defined as death, vegetative state, or severe disability (CPC 3-5) at hospital discharge/1 month or later, in comatose adult survivors from cardiac arrest (CA).PubMed, EMBASE, Web of Science, and the Cochrane Database of Systematic Reviews (January 2013-April 2020) were searched. Sensitivity and false-positive rate (FPR) for each predictor were calculated. Due to heterogeneities in recording times, predictor thresholds, and definition of some predictors, meta-analysis was not performed.Ninety-four studies (30,200 patients) were included. Bilaterally absent pupillary or corneal reflexes after day 4 from ROSC, high blood values of neuron-specific enolase from 24 h after ROSC, absent N20 waves of short-latency somatosensory-evoked potentials (SSEPs) or unequivocal seizures on electroencephalogram (EEG) from the day of ROSC, EEG background suppression or burst-suppression from 24 h after ROSC, diffuse cerebral oedema on brain CT from 2 h after ROSC, or reduced diffusion on brain MRI at 2-5 days after ROSC had 0% FPR for poor outcome in most studies. Risk of bias assessed using the QUIPS tool was high for all predictors.In comatose resuscitated patients, clinical, biochemical, neurophysiological, and radiological tests have a potential to predict poor neurological outcome with no false-positive predictions within the first week after CA. Guidelines should consider the methodological concerns and limited sensitivity for individual modalities. (PROSPERO CRD42019141169).
Ion shift index at the immediate post-cardiac arrest period as an early prognostic marker in out-of-hospital cardiac arrest survivors
DOI:10.3390/jcm11206187
URL
[Cited within: 2]

The ion shift index (ISI) is a suggested marker to reflect the magnitude of ischemic damage. This study aimed to investigate the prognostic value of the ISI for predicting poor neurological outcomes at 6 months in comatose out-of-hospital cardiac arrest (OHCA) survivors by comparing it with the OHCA and Cardiac Arrest Hospital Prognosis (CAHP) scores. This observational registry-based cohort study included adult comatose OHCA survivors admitted to a tertiary care hospital in Korea between 2015 and 2021. The ISI was calculated using the serum electrolyte levels obtained within one hour of resuscitation. The primary outcome was poor neurological function (Cerebral Performance Category score of 3–5) at 6 months. Of the 250 OHCA survivors, 164 (65.6%) had poor neurological outcomes. These patients had a higher median ISI than those with good neurological outcomes (4.95 vs. 3.26, p < 0.001). ISI (adjusted odds ratio, 2.107; 95% confidence interval, 1.350–3.288, p = 0.001) was associated with poor neurological outcomes. The prognostic performance of ISI (area under the curve [AUC], 0.859) was similar to that of the OHCA score (AUC, 0.858; p = 0.968) and the CAHP score (AUC, 0.894; p = 0.183). ISI would be a prognostic biomarker for comatose OHCA survivors that is available during the immediate post-cardiac arrest period.
Hypocalcemia following resuscitation from cardiac arrest revisited
DOI:10.1016/j.resuscitation.2009.10.002
PMID:19913975
[Cited within: 1]

Hypocalcemia associated with cardiac arrest has been reported. However, mechanistic hypotheses for the decrease in ionized calcium (iCa) vary and its importance unknown. The objective of this study was to assess the relationships of iCa, pH, base excess (BE), and lactate in two porcine cardiac arrest models, and to determine the effect of exogenous calcium administration on post-resuscitation hemodynamics.Swine were instrumented and VF was induced either electrically (EVF, n=65) or spontaneously, ischemically induced (IVF) with balloon occlusion of the LAD (n=37). Animals were resuscitated after 7 min of VF. BE, iCa, and pH, were determined prearrest and at 15, 30, 60, 90, 120 min after ROSC. Lactate was also measured in 26 animals in the EVF group. Twelve EVF animals were randomized to receive 1g of CaCl(2) infused over 20 min after ROSC or normal saline.iCa, BE, and pH declined significantly over the 60 min following ROSC, regardless of VF type, with the lowest levels observed at the nadir of left ventricular stroke work post-resuscitation. Lactate was strongly correlated with BE (r=-0.89, p<0.0001) and iCa (r=-0.40, p<0.0001). In a multivariate generalized linear mixed model, iCa was 0.005 mg/dL higher for every one unit increase in BE (95% CI 0.003-0.007, p<0.0001), while controlling for type of induced VF. While there was a univariate correlation between iCa and BE, when BE was included in the regression analysis with lactate, only lactate showed a statistically significant relationship with iCa (p=0.02). Post-resuscitation CaCl(2) infusion improved post-ROSC hemodynamics when compared to saline infusion (LV stroke work control 8+/-5 gm vs 23+/-4, p=0.014, at 30 min) with no significant difference in tau between groups.Ionized hypocalcemia occurs following ROSC. CaCl(2) improves post-ROSC hemodynamics suggesting that hypocalcemia may play a role in early post-resuscitation myocardial dysfunction.Copyright 2009 Elsevier Ireland Ltd. All rights reserved.
Prognostic value of serum phosphate level in adult patients resuscitated from cardiac arrest
DOI:S0300-9572(18)30183-7
PMID:29702189
[Cited within: 1]

Several studies have reported increased levels of phosphate after cardiac arrest. Given the relationship between phosphate level and the severity of ischaemic injury reported in previous studies, higher phosphate levels may be associated with worse outcomes. We investigated the prognostic value of phosphate level after the restoration of spontaneous circulation (ROSC) in adult cardiac arrest patients.This study was a retrospective observational study including adult cardiac arrest survivors treated at the Chonnam National University Hospital between January 2014 and June 2017. From medical records, data regarding clinical characteristics, outcome at hospital discharge, and laboratory parameters including phosphate levels after ROSC were collected. The primary outcome was poor outcome at hospital discharge, defined as Cerebral Performance Categories 3-5.Of the 674 included patients, 465 had poor outcome at hospital discharge. Serum phosphate level was significantly higher in patients with poor outcome than in those with good outcome (p < 0.001). Phosphate level was correlated with time to ROSC (r = 0.350, p < 0.001). Receiver operating characteristic curve analysis revealed an area under the curve of 0.805 (95% confidence interval [CI], 0.777-0.838) for phosphate level. In multivariate analysis, a higher phosphate level was independently associated with poor outcome at hospital discharge (odds ratio, 1.432; 95% CI, 1.245-1.626; p < 0.001).A higher phosphate level after ROSC was independently associated with poor outcome at hospital discharge in adult cardiac arrest patients. However, given its modest prognostic performance, phosphate level should be used in combination with other prognostic indicators.Copyright © 2018 Elsevier B.V. All rights reserved.
Correlation between initial serum levels of lactate after return of spontaneous circulation and survival and neurological outcomes in patients who undergo therapeutic hypothermia after cardiac arrest
DOI:10.1016/j.resuscitation.2014.11.005
PMID:25450570
[Cited within: 1]

We analysed the relationship between serum levels of lactate within 1h of return of spontaneous circulation (ROSC) and survival and neurological outcomes in patients who underwent therapeutic hypothermia (TH).This was a multi-centre retrospective and observational study that examined data from the first Korean Hypothermia Network (KORHN) registry from 2007 to 2012. The inclusion criteria were out-of-hospital cardiac arrest (OHCA) and examination of serum levels of lactate within 1h after ROSC, taken from KORHN registry data. The primary endpoint was survival outcome at hospital discharge, and the secondary endpoint was poor neurological outcome (Cerebral Performance Category, CPC, 3-5) at hospital discharge. Initial lactate levels and other variables collected within 1h of ROSC were analysed via multivariable logistic regression.Data from 930 cardiac arrest patients who underwent TH were collected from the KORHN registry. In a total of 443 patients, serum levels of lactate were examined within 1h of ROSC. In-hospital mortality was 289/443 (65.24%), and 347/443 (78.33%) of the patients had CPCs of 3-5 upon hospital discharge. The odds ratios of lactate levels for CPC and in-hospital mortality were 1.072 (95% confidence interval (CI) 1.026-1.121) and 1.087 (95% CI=1.031-1.147), respectively, based on multivariate ordinal logistic regression analyses.High levels of lactate in serum measured within 1h of ROSC are associated with hospital mortality and high CPC scores in cardiac arrest patients treated with TH.Copyright © 2014 Elsevier Ireland Ltd. All rights reserved.
2021 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; neonatal life support; education, implementation, and teams; First Aid Task Forces; and the COVID-19 Working Group