INTRODUCTION
Cardiac arrest (CA) is an important global public health issue and is associated with high mortality.[1,2] In-hospital CA occurs in more than 290,000 adults each year in the United States.[3] Cardiopulmonary resuscitation (CPR) is an effective emergency intervention for CA.[4] After CA treatment and the successful return of spontaneous circulation (ROSC), the neurological outcome of patients tends to be undesirable.[5] Approximately 50% of survivors suffer brain injury and consequent different severities of neurologic disability.[6] Targeted temperature management (TTM), also known as “temperature control”, which maintains the patient’s temperature from 32 ℃ to 36 ℃ for at least 24 h, was recommended by international guidelines to attenuate brain injury and improve the neurological outcome.[7,8] The development of fever before TTM occurs frequently and has previously been found to be associated with unfavorable outcomes.[9,10] With the implementation of TTM in recent years, post-arrest fever in the immediate period can be prevented. However, an important study, the TTM-2 trial, suggested that TTM did not lead to a lower mortality by 6 months than targeted normothermia in patients with coma after out-of-hospital cardiac arrest (OHCA).[11] Although recent guidelines suggested that there was insufficient evidence to provide advice for the implementation of TTM after CA.[8,12] Notably, the fever can also occur after the rewarming period following TTM and affect the outcome of CA patients.[13⇓⇓⇓⇓⇓⇓⇓⇓⇓⇓⇓-25] In this study, we mainly focus on the fever in the patients who completed TTM.
Post-rewarming fever (PRF), or rebound hyperthermia (RH), was observed in many patients who received TTM.[13⇓⇓⇓⇓⇓⇓⇓⇓⇓⇓⇓⇓-26] PRF was defined as a phenomenon of increased body temperature (>38.0 ℃ or greater) after the rewarming period following TTM.[14⇓⇓⇓⇓⇓⇓⇓-22,24,25] According to the European Resuscitation Council and European Society of Intensive Care Medicine (ERC-ESICM) guidelines, actively preventing fever (defined as body temperature >37.7 ℃) for at least 72 h is recommended for comatose patients after CA.[8] However, the influence of temperature control strategies after rewarming remains unclear. There is no sufficient evidence to support temperature control in CA patients after rewarming following TTM.[8,27] Previous studies on the influence of PRF on neurological outcomes have shown conflicting results. Some studies have suggested that PRF is related to unfavorable neurological outcomes.[15,18,24,25] However, recent studies have indicated that PRF may be a symbol of good neurological outcome.[19,20,28] Therefore, the clinical significance of PRF should be better understood.
The aim of this systematic review and meta-analysis is to investigate whether PRF could have an impact on clinically relevant outcomes, including neurological outcome and mortality, in patients suffering from CA. Meanwhile, this meta-analysis may provide a better understanding of temperature control strategies in patients who completed TTM.
METHODS
We conducted a systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis — Protocols (PRISMA-P) guidelines.[29] The protocol of this study was registered at www.inplasy.com (INPLASY202240052).
Data sources and search strategies
We performed the literature retrieval up to March 13, 2022, in the EMBASE, PubMed, and Cochrane Central databases using the following Medical Subject Headings (MeSH) terms: “cardiac arrest” AND “targeted temperature management” AND (“fever” OR “hyperthermia”) (supplementary Table 1).
Inclusion and exclusion criteria
The studies were selected for the meta-analysis according to the following requirements: (1) the participants of the study were adult patients with CA; (2) the TTM therapy was involved in the research; (3) the study observed and defined the phenomenon of PRF (body temperature >38.0 ℃ or greater); (4) the data about neurological outcome and mortality of patients who suffered PRF were available; (5) the studies were cohort studies or randomized controlled trials (RCTs); and (6) the study articles were written in English.
The studies were excluded if the following conditions were met: (1) the full text of the article could not be accessed; (2) only the abstract of articles was accessible; (3) only a citation or report on the study could be found in another publication; and (4) the neurological outcome and mortality data were not available.
We reviewed the articles that conformed to the above-mentioned criteria and extracted the relevant data about neurological outcome and/or mortality. In this meta-analysis, the definition of unfavorable neurological outcome was Glasgow-Pittsburgh cerebral performance category (CPC) > 2 or modified Rankin Scale (mRS) >3.[30,31] The primary outcome is unfavorable neurological outcome at discharge or at the end of the follow-up period. The secondary outcome is the mortality rate in the hospital or at the end of the follow-up period.
Research selection and data extraction
Two independent researchers (GQG and YNM) screened all the accessible articles based on the above-mentioned inclusion and exclusion criteria and extracted the relevant data of the studies. In the progress of the data extraction, the arising controversies about studies from two researchers were discussed with a third researcher (SX). The first author’s first name, the study’s year, the study’s host country, the study design type, the study period, the methods of TTM, the number of PRF patients and control patients, the definition of PRF, the type of neurological outcome assessment and mortality of the original studies were all extracted.
Risk of bias assessment
No RCTs were selected in this meta-analysis. The Newcastle-Ottawa Scale (NOS) was used to assess the risk of bias (ROB).[32] The NOS had a total score of 9 points and included cohort selection, cohort comparability, and outcome evaluation. Studies that scored at least 6 points were included in the meta-analysis (supplementary Table 2).
Statistical analysis
The degree of variability and heterogeneity of the meta-analysis were assessed using I2 and P values. When I2 was 50%, 51%-75%, or >76%, it was classified as low, moderate, or high heterogeneity, respectively. For high heterogeneity, the random effects model was used to calculate the merged odds ratios (ORs) and 95% confidence intervals (CIs), while the fixed effect model was used for low or moderate heterogeneity. The study model’s robustness was tested by sensitivity analysis. In this study, Review Manager 5.4 software was used to conduct statistical analysis.
RESULTS
Screening of relevant research
After electronic database searches and bibliographical inspections, 330 records were screened according to the retrieval strategies. Forty-two records were duplicated, and 277 of the remaining records were excluded on account of title, abstract, study design, unavailable data and other factors. As a result, 11 studies were selected for this meta-analysis (supplementary Figure 1).[14⇓⇓⇓⇓⇓⇓⇓-22,24,25]
Study characteristics
A total of 3,246 CA patients were selected in this meta-analysis, of whom 1,257 patients developed PRF and 1,989 patients maintained normothermia. The 11 included studies had different definitions of PRF. Eligible studies included seven articles that defined PRF as a body temperature >38.0 ℃ after TTM.[14,16⇓⇓⇓⇓-21] Four articles defined PRF as >38.5 ℃ after TTM.[15,22,24,25] The neurological outcome of patients was assessed in 10 studies,[15⇓⇓⇓⇓⇓⇓-22,24,25] while mortality was calculated in 9 studies.[14⇓⇓⇓⇓-19,21,24,25] More details and characteristics of the included studies are presented in Table 1.
Table 1. Summary of the included studies
| Author/year | Country | TTM strategies | Rate of rewarming | Definition of normothermia | Consciousness | Timing of onset of fever | Definition of PRF | Type of CA | Outcome assessment timing | Mortality | Patients (n) | PRF (n)/ normothermia (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Holm 2021[25] | Europe | 32-36 ℃ for 24 h or 48 h | 0.5 ℃/h | 37.0 ℃ | Coma | Within 72 h after rewarming | 38.5 ℃ | OHCA | CPC at 6 months | In-hospital | 338 | 103/235 |
| Lee 2020[20] | Korea | 32-36 ℃ for 24 h | 0.2-0.5 ℃/h | NA | All* | Within 72 h after rewarming | 38.0 ℃ | OHCA | CPC at 6 months | NA | 1,031 | 389/642 |
| Makker 2017[21] | America | 32-34 ℃ for 24 h | 0.25 ℃/h | 37.0 ℃ | All | Within 24 h after rewarming | 38.0 ℃ | OHCA | CPC in-hospital | In-hospital | 97 | 54/43 |
| Grossestreuer 2017[17] | America | <34 ℃ for unknown hours | NA | 36.5 ℃ | All | Within 72 h after rewarming | 38.0 ℃ | Both** | CPC at discharge | Discharge | 465 | 179/286 |
| Lee 2015[19] | Korea | 32-34 ℃ for 24 h | 0.2-0.5 ℃/h | 36.5 ℃ | All | Within 48 h after rewarming | 38.0 ℃ | Both | CPC at discharge | In-hospital | 277 | 81/196 |
| Nobile 2015[22] | Belgium | 32-34 ℃ for 24 h | 0.5 ℃/h | 37.0 ℃ | Coma | Within 24 h after rewarming | 38.5 ℃ | Both | CPC at 3 months | NA | 229 | 41/188 |
| Cocchi 2014[16] | America | 32-34 ℃ for unknown hours | NA | NA | All | Within 24 h after rewarming | 38.0 ℃ | OHCA | CPC in-hospital | In-hospital | 54 | 28/26 |
| Winters 2013[24] | America | 32-34 ℃ for 24 h | NA | NA | All | First 24 h of the re-warming process | 38.5 ℃ | OHCA | mRS at discharge | In-hospital | 141 | 42/99 |
| Leary 2013[18] | America | 32-34 ℃ for 24 h | NA | 37.0 ℃ | All | Within 24 h after rewarming | 38.0 ℃ | Both | CPC at discharge | discharge | 167 | 69/98 |
| Bro-Jeppesen 2013[15] | Denmark | 32-34 ℃ for 24 h | 0.5 ℃/h | 36.5 ℃ | Coma | Within 36 h after rewarming | 38.5 ℃ | OHCA | CPC at discharge | 30 days | 270 | 136/134 |
| Benz-Woerner 2012[14] | Switzerland | 32-34 ℃ for 24 h | NA | 37.0 ℃ | Coma | NA | 38.0 ℃ | Both | NA | In-hospital | 177 | 135/42 |
*All the conscious patients were included in the study. **Both the OHCA and IHCA were included in the study. NA: not applicable; OHCA: out-of-hospital cardiac arrest; IHCA: in-hospital cardiac arrest; CPC: cerebral performance category; mRS: modified Rankin Scale.
Assessing the risk of bias
The 11 included studies were observational cohort studies, and no RCTs were selected for this meta-analysis. The scores of all the eligible cohort studies were greater than or equal to 6 points based on the NOS (supplementary Table 2).
Primary outcome—unfavorable neurological outcome
Ten of the included studies reported the neurological outcome of patients. Six studies defined PRF as >38.0 °C,[16⇓⇓⇓⇓-21] and four studies defined PRF as >38.5 °C.[15,22,24,25] The neurological outcome was assessed at different timepoints in the respective original studies. We extracted the timing of neurological outcome data in accordance with Table 1.
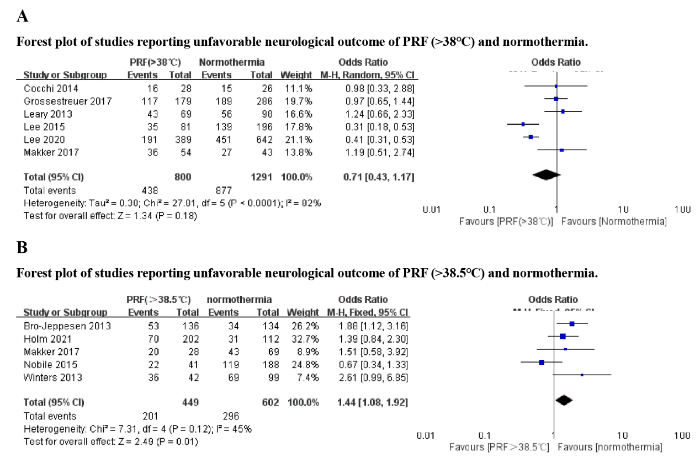
Articles defining PRF as >38.0 °C and >38.5 ℃ were selected for different meta-analyses of PRF and neurological outcomes. Six articles defined PRF as >38.0 °C[16⇓⇓⇓⇓-21] and analyzed it with a random effects model. Analysis of these six articles showed that PRF (> 38.0 °C) had no significant effect on the unfavorable neurological outcome of CA patients (OR 0.71; 95% CI 0.43-1.17; I2 82%) (Figure 1A).
Figure 1.
Figure 1.
Forest plot of studies reporting unfavorable neurological outcomes of PRF and normothermia.
Four articles defined PRF as >38.5 °C and investigated the effect of PRF on neurological outcome.[15,22,24,25] One study conducted by Makker et al[21] defined PRF as >38.0 °C but contained a subgroup that investigated the relationship between PRF >38.5 °C and the neurological outcome of CA patients. We used the fixed effects model to analyze data from the five studies. The results showed that PRF with higher body temperature (PRF >38.5 ℃) had a significant association with unfavorable neurological outcomes in CA patients (OR 1.44, 95% CI 1.08-1.92, I2 45%) (Figure 1B).
Secondary outcome—mortality
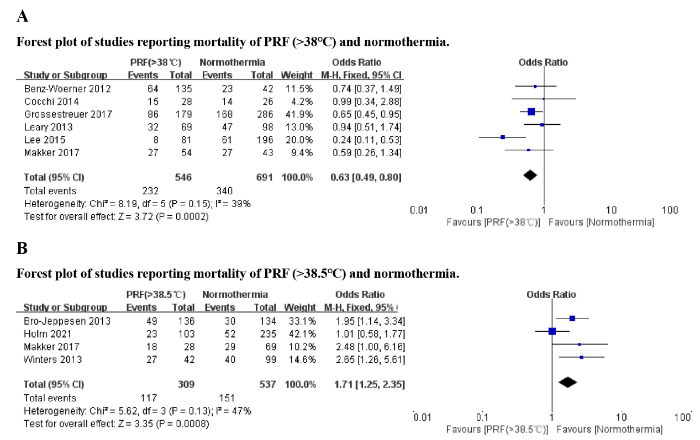
Mortality data were available in nine of the studies included in this meta-analysis. Six studies defined PRF as >38.0 °C,[14,16⇓⇓-19,21] and three studies defined PRF as >38.5 °C.[15,24,25] We examined the six studies (PRF >38.0 ℃) using a fixed effect model. The results suggested that PRF (body temperature >38.0 ℃) was associated with lower mortality (OR 0.63, 95% CI 0.49-0.80, I2 39%) (Figure 2A).
Figure 2.
Figure 2.
Forest plot of studies reporting mortality of PRF and normothermia.
Three studies investigated the association between PRF >38.5 ℃ and mortality.[15,24,25] One study conducted by Makker et al[21] contained a subgroup that investigated the effect of PRF >38.5 ℃ on mortality. A fixed-effect model was used to analyze the five studies. The results showed that PRF with higher body temperature was associated with higher mortality (OR 1.71, 95% CI 1.25-2.35, I2 47%) (Figure 2B).
Sensitivity analysis
None of the 11 studies were evaluated as having a high risk of bias. Therefore, sensitivity analysis was performed by removing the included studies one by one to see how they affected the pooled OR, 95% CI and heterogeneity. The results of the sensitivity analysis are shown in supplementary Tables 3-6. The studies conducted by Lee et al,[19] Nobile et al,[22] and Holm et al[25] influenced the heterogeneity in their respective analyses (supplementary Tables 4-6). However, these studies had no effect on the robustness of the results. Sensitivity analysis showed that the results of this meta-analysis had good robustness.
DISCUSSION
In this meta-analysis, 11 studies involving 3,246 patients analyzed the relationship between PRF and the prognosis of patients. The results of this meta-analysis suggest that CA patients who experienced PRF (>38.0 ℃) after TTM had similar neurological outcomes and lower mortality than normothermia patients. However, patients who experienced PRF, defined as a stricter body temperature (>38.5 °C), were associated with worse neurological outcomes and higher mortality.
The analysis of PRF >38.0 ℃ and neurological outcome had high heterogeneity, and sensitivity analysis was conducted to test the robustness of the merger results in the analysis (supplementary Table 3). The reasons for the high heterogeneity varied, such as the type of CA, the design of the TTM plan and the timing of outcome acquisition. It is noteworthy that the onset time of PRF may affect heterogeneity. The study conducted by Lee et al[20] observed the development of PRF in different periods after rewarming and divided the PRF patients into three subgroups. The results indicated that PRF occurring within 24 h after rewarming (but not within 24-48 h or 48-72 h) was associated with favorable neurologic outcomes and decreased mortality. This study suggests that the onset time of PRF may also be a critical factor affecting the prognosis of CA patients. It is difficult to avoid heterogeneity since the original studies had different research protocols for PRF.
A concise meta-analysis conducted by Makker et al[33] found that PRF (both >38.0 ℃ and >38.5 ℃) was associated with a significantly worse neurological outcome, which was not consistent with the present results. Possible reasons for the above discrepancy may be the inclusion of emerging studies. The studies that have emerged in recent years suggested that PRF may not be associated with unfavorable neurological outcomes. Several studies have even suggested that PRF is a favorable symbol for CA patients.[19,20,28]
This meta-analysis reveals that PRF has different effects on the mortality of CA patients when the definition of PRF is diverse. When the cutoff temperature of PRF was lower (>38.0 ℃), patients with moderate fever (38.0-38.5 ℃) were included in the study. Several included studies suggested that moderate PRF have no effect on the prognosis of CA patients and tended to be associated with favorable outcomes.[17,19,20] One probable explanation proposed by Murnin et al[34] was that more severe brain injury impacts the function of hypothalamus and thermoregulation, since the hypothalamus is not one of the especially vulnerable regions to ischemia-reperfusion injury. PRF reflects higher heat generation and preserved thermoregulatory function, which suggests less severe brain injury than that in patients with lower post-rewarming body temperatures.[27] This explanation was supported by the study conducted by Lee et al[19] that the prevalence of PRF was associated with favorable CA prognosis indicators, such as younger age and lower SOFA scores.
In the present study, PRF with a stricter definition (body temperature >38.5 ℃) was associated with worse neurological outcome and higher mortality. Fever, as is well known, has a significant association with poor prognosis in patients with brain injury. Before TTM was recommended by the guidelines and widely used as a clinical strategy, fever was a marker for worse outcomes in CA patients.[35] In an in vitro study, the prevention of PRF aggravated apoptosis of cells and release of inflammatory factors.[36] Meanwhile, post-cardiac arrest syndrome (PCAS) is characterized by multi-organ ischemia-reperfusion injury and the production of inflammatory cytokines, which can cause fever in CA patients.[37] These studies indicated that PRF was related to the activation of the inflammatory response and programmed cell death following ischemia-reperfusion injury caused by CA. This is a reasonable explanation for the relationship between severe fever and worse outcomes in CA patients who completed TTM. The study conducted by Grossestreuer et al[17] indicated that higher body temperature was linearly associated with increased mortality.
The results of this meta-analysis suggest that preventing fever after rewarming is necessary when the body temperature was >38.5 ℃. However, one study conducted by Kim et al[27] indicated that the implementation of controlled normothermia to prevent PRF was not associated with favorable neurological outcome. Although this study conducted by Kim et al[27] had some limitations, such as the nonstandard controlled normothermia protocols and the incomplete data of included patients, the results showed that the post-rewarming active temperature control could prevent the high fever after the rewarming period of TTM.
Most previous studies were focused on the clinical application of TTM, including optimal cooling temperature,[38] practical methods of cooling for temperature control[39] and rate of rewarming following TTM.[40] The guidelines rarely mention body temperature control strategies after the rewarming period.[8] In this meta-analysis, we focused on active body temperature management strategies after TTM. The results suggest that therapeutic intervention is necessary to prevent high fever after the completion of TTM.
The following are the advantages of this study: (1) this meta-analysis evaluated PRF after TTM in CA patients and assisted physicians in recognizing the clinical effects of PRF and patient prognosis following ROSC; (2) the PRF group was divided into subgroups >38.0 °C and >38.5 °C so that physicians could better understand the severity of fever and make corresponding treatment decisions.
Nonetheless, the following are the limitations of this meta-analysis: (1) meta-analysis was a secondary analysis of original studies, and high heterogeneity caused by many reasons existed among different studies; (2) the TTM therapy methods of the included studies were different, which may contribute to the high heterogeneity. Therefore, more RCTs with standard TTM treatment are needed in the future to investigate the effect of PRF.
CONCLUSION
This study provides a specific understanding of the PRF phenomenon and suggests that PRF with a broader definition (body temperature >38.0 ℃) is associated with favorable neurological outcomes and lower mortality. However, PRF was associated with worse neurological outcomes and higher mortality when PRF was defined as >38.5 ℃. It is necessary to prevent fever after rewarming when the body temperature of CA patients is >38.5 ℃.
Funding: This study was supported by the National Natural Science Foundation of China (82072137; 81571866).
Ethical approval: Not needed.
Conflicts of interest: The authors have no conflicts of interest to disclose.
Contributors: GQG conceived the study concept and design and was involved in the drafting and critical revision of the manuscript. All authors contributed to the design and interpretation of the study and to further drafts.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Survival disparities in pediatric out-of-hospital cardiac arrest: still a "night and day difference"
DOI:10.1016/j.jacasi.2022.02.007 PMID:36339353 [Cited within: 1]
Survival from pediatric out-of-hospital cardiac arrest during nights and weekends: an updated Japanese registry-based study
DOI:10.1016/j.jacasi.2022.01.005 URL [Cited within: 1]
In-hospital cardiac arrest: a review
DOI:10.1001/jama.2019.1696
PMID:30912843
[Cited within: 1]

In-hospital cardiac arrest is common and associated with a high mortality rate. Despite this, in-hospital cardiac arrest has received little attention compared with other high-risk cardiovascular conditions, such as stroke, myocardial infarction, and out-of-hospital cardiac arrest.In-hospital cardiac arrest occurs in over 290 000 adults each year in the United States. Cohort data from the United States indicate that the mean age of patients with in-hospital cardiac arrest is 66 years, 58% are men, and the presenting rhythm is most often (81%) nonshockable (ie, asystole or pulseless electrical activity). The cause of the cardiac arrest is most often cardiac (50%-60%), followed by respiratory insufficiency (15%-40%). Efforts to prevent in-hospital cardiac arrest require both a system for identifying deteriorating patients and an appropriate interventional response (eg, rapid response teams). The key elements of treatment during cardiac arrest include chest compressions, ventilation, early defibrillation, when applicable, and immediate attention to potentially reversible causes, such as hyperkalemia or hypoxia. There is limited evidence to support more advanced treatments. Post-cardiac arrest care is focused on identification and treatment of the underlying cause, hemodynamic and respiratory support, and potentially employing neuroprotective strategies (eg, targeted temperature management). Although multiple individual factors are associated with outcomes (eg, age, initial rhythm, duration of the cardiac arrest), a multifaceted approach considering both potential for neurological recovery and ongoing multiorgan failure is warranted for prognostication and clinical decision-making in the post-cardiac arrest period. Withdrawal of care in the absence of definite prognostic signs both during and after cardiac arrest should be avoided. Hospitals are encouraged to participate in national quality-improvement initiatives.An estimated 290 000 in-hospital cardiac arrests occur each year in the United States. However, there is limited evidence to support clinical decision making. An increased awareness with regard to optimizing clinical care and new research might improve outcomes.
Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care
Post-cardiac arrest syndrome
PMID:20395899
[Cited within: 1]

Following successful resuscitation from cardiac arrest, neurological impairment as well as other types of organ dysfunction still cause significant morbidity and mortality. The whole-body ischemia-reperfusion response that occurs during cardiac arrest and subsequent restoration of systemic circulation results in a series of pathophysiological processes that have been termed the post-cardiac arrest syndrome. The components of the post-cardiac arrest syndrome comprise post-cardiac arrest brain injury, post-cardiac arrest myocardial dysfunction, the systemic ischemia-reperfusion response and persistent precipitating pathology. Management of the post-cardiac arrest syndrome involves intensive care support with input from various other medical specialties in a coordinated fashion. Management of ventilation aims for normal carbon dioxide values and normoxia rather than hyperoxia. Management of the circulation commonly requires vasoactive support to overcome (often transient) myocardial dysfunction. Particular attention should be given to evidence of cardiac ischemia and referral for urgent angiography and percutaneous coronary intervention, if appropriate, should be available to all. Optimizing neurological recovery will involve seizure control, management of hyperglycemia and therapeutic hypothermia. Prognostication following cardiac arrest remains difficult, but there are diagnostic tests that may be used with some degree of accuracy.
Cognitive impairments in survivors of out-of-hospital cardiac arrest: a systematic review
DOI:10.1016/j.resuscitation.2008.10.034
PMID:19117659
[Cited within: 1]

To describe the current evidence on the frequency and nature of cognitive impairments in survivors of out-of-hospital cardiac arrest.Systematic review.Pubmed, Embase, PsychInfo and Cinahl (1980-2006). No language restriction was imposed.The following inclusion criteria were used: participants had to be survivors of out-of-hospital cardiac arrest, 18 years or older, and there had to be least one cognitive outcome measure with a follow-up of 3 months or more. Case reports and qualitative studies were excluded. The articles were screened on title, abstract and full text by two reviewers. All selected articles were reviewed and assessed by two reviewers independently using a quality criteria list.Out of the 286 articles initially identified, 28 were selected for final evaluation. There was a high heterogeneity between the studies with regard to study design, number of participants, outcome measures and duration of follow-up. In general, the quality of the articles appeared low, with a few positive exceptions. The reported frequency of cognitive impairments in survivors of out-of-hospital cardiac arrest ranged from 6% to 100%. Memory problems were the most common cognitive impairment, followed by impairments in attention and executive functioning. Three high-quality prospective studies found that cognitive problems occurred in about half of the survivors of out-of-hospital cardiac arrest.There are few good studies on the frequency of cognitive impairments after out-of-hospital cardiac arrest. However, cognitive problems, in particular memory problems, seem common in survivors of out-of-hospital cardiac arrest.
High quality targeted temperature management (TTM) after cardiac arrest
DOI:10.1186/s13054-019-2721-1
[Cited within: 1]

Targeted temperature management (TTM) is a complex intervention used with the aim of minimizing post-anoxic injury and improving neurological outcome after cardiac arrest. There is large variability in the devices used to achieve cooling and in protocols (e.g., for induction, target temperature, maintenance, rewarming, sedation, management of post-TTM fever). This variability can explain the limited benefits of TTM that have sometimes been reported. We therefore propose the concept of “high-quality TTM” as a way to increase the effectiveness of TTM and standardize its use in future interventional studies.
ERC-ESICM guidelines on temperature control after cardiac arrest in adults
DOI:10.1007/s00134-022-06620-5
PMID:35089409
[Cited within: 5]

The aim of these guidelines is to provide evidence‑based guidance for temperature control in adults who are comatose after resuscitation from either in-hospital or out-of-hospital cardiac arrest, regardless of the underlying cardiac rhythm. These guidelines replace the recommendations on temperature management after cardiac arrest included in the 2021 post-resuscitation care guidelines co-issued by the European Resuscitation Council (ERC) and the European Society of Intensive Care Medicine (ESICM). The guideline panel included thirteen international clinical experts who authored the 2021 ERC-ESICM guidelines and two methodologists who participated in the evidence review completed on behalf of the International Liaison Committee on Resuscitation (ILCOR) of whom ERC is a member society. We followed the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach to assess the certainty of evidence and grade recommendations. The panel provided suggestions on guideline implementation and identified priorities for future research. The certainty of evidence ranged from moderate to low. In patients who remain comatose after cardiac arrest, we recommend continuous monitoring of core temperature and actively preventing fever (defined as a temperature > 37.7 °C) for at least 72 h. There was insufficient evidence to recommend for or against temperature control at 32-36 °C or early cooling after cardiac arrest. We recommend not actively rewarming comatose patients with mild hypothermia after return of spontaneous circulation (ROSC) to achieve normothermia. We recommend not using prehospital cooling with rapid infusion of large volumes of cold intravenous fluids immediately after ROSC.© 2022. Springer-Verlag GmbH Germany, part of Springer Nature.
Hyperthermia after cardiac arrest is associated with an unfavorable neurologic outcome
DOI:10.1001/archinte.161.16.2007
PMID:11525703
[Cited within: 1]

Moderate elevation of brain temperature, when present during or after ischemia, may markedly worsen the resulting injury.To evaluate the impact of body temperature on neurologic outcome after successful cardiopulmonary resuscitation.In patients who experienced a witnessed cardiac arrest of presumed cardiac cause, the temperature was recorded on admission to the emergency department and after 2, 4, 6, 12, 18, 24, 36, and 48 hours. The lowest temperature within 4 hours and the highest temperature during the first 48 hours after restoration of spontaneous circulation were recorded and correlated to the best-achieved cerebral performance categories' score within 6 months.Over 43 months, of 698 patients, 151 were included. The median age was 60 years (interquartile range, 53-69 years); the estimated median no-flow duration was 5 minutes (interquartile range, 0-10 minutes), and the estimated median low-flow duration was 14.5 minutes (interquartile range, 3-25 minutes). Forty-two patients (28%) underwent bystander-administered basic life support. Within 6 months, 74 patients (49%) had a favorable functional neurologic recovery, and a total of 86 patients (57%) survived until 6 months after the event. The temperature on admission showed no statistically significant difference (P =.39). Patients with a favorable neurologic recovery showed a higher lowest temperature within 4 hours (35.8 degrees C [35.0 degrees C-36.1 degrees C] vs 35.2 degrees C [34.5 degrees C-35.7 degrees C]; P =.002) and a lower highest temperature during the first 48 hours after restoration of spontaneous circulation (37.7 degrees C [36.9 degrees C-38.6 degrees C] vs 38.3 degrees C [37.8 degrees C-38.9 degrees C]; P<.001) (data are given as the median [interquartile range]). For each degree Celsius higher than 37 degrees C, the risk of an unfavorable neurologic recovery increases, with an odds ratio of 2.26 (95% confidence interval, 1.24-4.12).Hyperthermia is a potential factor for an unfavorable functional neurologic recovery after successful cardiopulmonary resuscitation.
Body temperature changes are associated with outcomes following in-hospital cardiac arrest and return of spontaneous circulation
DOI:10.1016/j.resuscitation.2009.08.020
PMID:19804929
[Cited within: 1]

Spontaneous changes in body temperature after return of circulation (ROSC) from cardiac arrest are common, but the association of these changes with outcomes in hospitalized patients who survive to 24h post-ROSC is not known. We tested the hypothesis that adults who experience temperature lability in the first 24h have worse outcomes compared with those who maintain normothermia.A prospective observational study from a multicenter registry of cardiac arrests (National Registry of Cardiopulmonary Resuscitation) from 355 US and Canadian hospitals. 14,729 adults with return of circulation from a pulseless cardiac arrest. We excluded those who died or were discharged before 24h post-event, those made Do-Not-Resuscitate (DNR) within 24h of event, those that had a preceding trauma, and those with multiple cardiac arrests. Finally, we included only subjects that had both a lowest (T(min)) and highest (T(max)) body temperature value recorded during the first 24-h after ROSC, resulting in a study sample of 3426 patients.After adjustment for potential covariates, there was a lower odds of survival in those having an episode of hypothermia (adjusted odds ratio [OR], 0.62; 95% confidence interval [CI], 0.48-0.80), those having an episode of hyperthermia (OR, 0.67; 95% CI, 0.48-0.80), and those having an episode of both (OR, 0.59; 95% CI, 0.39-0.91). Among those who survived to discharge, there was also a lower odds of favorable neurologic performance in those who had an episode of hyperthermia (OR, 0.71; 95% CI, 0.51-0.98).Episodes of temperature lability following in-hospital resuscitation from cardiac arrest are associated with lower odds of surviving to discharge. Hyperthermia is also associated with fewer patients leaving the hospital with favorable neurologic performance. Further studies should identify whether therapeutic control over changes in body temperature after in-hospital cardiac arrest improves outcomes.
Hypothermia versus normothermia after out-of-hospital cardiac arrest
DOI:10.1056/NEJMoa2100591 URL [Cited within: 1]
2023 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; neonatal life support; education, implementation, and teams; first aid task forces; and the COVID-19 working group
Clinical predictors of outcome in survivors of out-of-hospital cardiac arrest treated with hypothermia
Body temperature regulation and outcome after cardiac arrest and therapeutic hypothermia
DOI:10.1016/j.resuscitation.2011.10.026
PMID:22079947
[Cited within: 8]

Therapeutic temperature modulation is recommended after cardiac arrest (CA). However, body temperature (BT) regulation has not been extensively studied in this setting. We investigated BT variation in CA patients treated with therapeutic hypothermia (TH) and analyzed its impact on outcome.A prospective cohort of comatose CA patients treated with TH (32-34°C, 24h) at the medical/surgical intensive care unit of the Lausanne University Hospital was studied. Spontaneous BT was recorded on hospital admission. The following variables were measured during and after TH: time to target temperature (TTT=time from hospital admission to induced BT target <34°C), cooling rate (spontaneous BT-induced BT target/TTT) and time of passive rewarming to normothermia. Associations of spontaneous and induced BT with in-hospital mortality were examined.A total of 177 patients (median age 61 years; median time to ROSC 25 min) were studied. Non-survivors (N=90, 51%) had lower spontaneous admission BT than survivors (median 34.5 [interquartile range 33.7-35.9]°C vs. 35.1 [34.4-35.8]°C, p=0.04). Accordingly, time to target temperature was shorter among non-survivors (200 [25-363]min vs. 270 [158-375]min, p=0.03); however, when adjusting for admission BT, cooling rates were comparable between the two outcome groups (0.4 [0.2-0.5]°C/h vs. 0.3 [0.2-0.4]°C/h, p=0.65). Longer duration of passive rewarming (600 [464-744]min vs. 479 [360-600]min, p<0.001) was associated with mortality.Lower spontaneous admission BT and longer time of passive rewarming were associated with in-hospital mortality after CA and TH. Impaired thermoregulation may be an important physiologic determinant of post-resuscitation disease and CA prognosis. When assessing the benefit of early cooling on outcome, future trials should adjust for patient admission temperature and use the cooling rate rather than the time to target temperature.Copyright © 2011 Elsevier Ireland Ltd. All rights reserved.
Post-hypothermia fever is associated with increased mortality after out-of-hospital cardiac arrest
DOI:10.1016/j.resuscitation.2013.07.023
PMID:23917079
[Cited within: 13]

Post-cardiac arrest fever has been associated with adverse outcome before implementation of therapeutic hypothermia (TH), however the prognostic implications of post-hypothermia fever (PHF) in the era of modern post-resuscitation care including TH has not been thoroughly investigated. The aim of the study was to assess the prognostic implication of PHF in a large consecutive cohort of comatose survivors after out-of-hospital cardiac arrest (OHCA) treated with TH.In the period 2004-2010, a total of 270 patients resuscitated after OHCA and surviving a 24-h protocol of TH with a target temperature of 32-34°C were included. The population was stratified in two groups by median peak temperature (≥38.5°C) within 36h after rewarming: PHF and no-PHF. Primary endpoint was 30-days mortality and secondary endpoint was neurological outcome assessed by Cerebral Performance Category (CPC) at hospital discharge.PHF (≥38.5°C) was associated with a 36% 30-days mortality rate compared to 22% in patients without PHF, plog-rank=0.02, corresponding to an adjusted hazard rate (HR) of 1.8 (95% CI: 1.1-2.7), p=0.02). The maximum temperature (HR=2.0 per °C above 36.5°C (95% CI: 1.4-3.0), p=0.0005) and the duration of PHF (HR=1.6 per 8h (95% CI: 1.3-2.0), p<0.0001) were also independent predictors of 30-days mortality in multivariable models. Good neurological outcome (CPC1-2) versus unfavourable outcome (CPC3-5) at hospital discharge was found in 61% vs. 39% in the PHF group compared to 75% vs. 25% in the No PHF group, p=0.02.Post-hypothermia fever ≥38.5°C is associated with increased 30-days mortality, even after controlling for potential confounding factors. Avoidance of PHF as a therapeutic target should be evaluated in prospective randomized trials.Copyright © 2013 Elsevier Ireland Ltd. All rights reserved.
Fever after rewarming: incidence of pyrexia in postcardiac arrest patients who have undergone mild therapeutic hypothermia
DOI:10.1177/0885066613491932
PMID:23783999
[Cited within: 11]

Induction of mild therapeutic hypothermia (TH; temperature 32-34°C) has become standard of care in many hospitals for comatose survivors of cardiac arrest. Pyrexia, or fever, is known to be detrimental in patients with neurologic injuries such as stroke or trauma. The incidence of pyrexia in the postrewarming phase of TH is unknown. We attempted to determine the incidence of fever after TH and hypothesized that those patients who were febrile after rewarming would have worse clinical outcomes than those who maintained normothermia in the postrewarming period.Retrospective data analysis of survivors of out-of-hospital cardiac arrest (OHCA) over a period of 29 months (December 2007 to April 2010).OHCA, age >18, return of spontaneous circulation, and treatment with TH.traumatic arrest and pregnancy. Data collected included age, sex, neurologic outcome, mortality, and whether the patient developed fever (temperature > 100.4°F, 38°C) within 24 hours after being fully rewarmed to a normal core body temperature after TH. We used simple descriptive statistics and Fisher exact test to report our findings.A total of 149 patients were identified; of these, 82 (55%) underwent TH. The mean age of the TH cohort was 66 years, and 28 (31%) were female. In all, 54 patients survived for >24 hours after rewarming and were included in the analysis. Among the analyzed cohort, 28 (52%) of 54 developed fever within 24 hours after being rewarmed. Outcome measures included in-hospital mortality as well as neurologic outcome as defined by a dichotomized Cerebral Performance Category (CPC) score. When comparing neurologic outcomes between the groups, 16 (57%) of 28 in the postrewarming fever group had a poor outcome (CPC score 3-5), while 15 (58%) of 26 in the no-fever group had a favorable outcome (P =.62). In the fever group, 15 (52%) of 28 died, while in the no-fever group, 14 (54%) of 26 died (P =.62).Among a cohort of patients who underwent mild TH after OHCA, more than half of these patients developed pyrexia in the first 24 hours after rewarming. Although there were no significant differences in outcomes between febrile and nonfebrile patients identified in this study, these findings should be further evaluated in a larger cohort. Future investigations may be needed to determine whether postrewarming temperature management will improve the outcomes in this population.© The Author(s) 2013.
Magnitude of temperature elevation is associated with neurologic and survival outcomes in resuscitated cardiac arrest patients with postrewarming pyrexia
DOI:S0883-9441(16)30362-8
PMID:27866109
[Cited within: 13]

Avoidance of pyrexia is recommended in resuscitation guidelines, including after treatment with targeted temperature management (TTM). Which aspects of postresuscitation pyrexia are harmful and modifiable have not been conclusively determined.This retrospective multicenter registry study collected serial temperatures during 72 hours postrewarming to assess the relationship between 3 aspects of pyrexia (maximum temperature, pyrexia duration, timing of first pyrexia) and neurologic outcome (primary) and survival (secondary) at hospital discharge. Adult TTM-treated patients from 13 US hospitals between 2005 and 2015 were included.One hundred seventy-nine of 465 patients had at least 1 temperature greater than or equal to 38°C. Pyrexic temperatures were associated with better survival than nonpyrexic temperatures (adjusted odds ratio [aOR], 1.54; 95% confidence interval [CI], 1.00-2.35). Higher maximum temperature was associated with worse outcome (neurologic aOR, 0.30 [95% CI, 0.10-0.84]; survival aOR, 0.25 [95% CI, 0.10-0.59]) in pyrexic patients. There was no significant relationship between pyrexia duration and outcomes unless duration was calculated as hours greater than or equal to 38.8°C, when longer duration was associated with worse outcomes (neurologic aOR, 0.86 [95% CI, 0.75-1.00]; survival aOR, 0.82 [95% CI, 0.72-0.93]).In postarrest TTM-treated patients, pyrexia was associated with increased survival. Patients experiencing postrewarming pyrexia had worse outcomes at higher temperatures. Longer pyrexia duration was associated with worse outcomes at higher temperatures.Copyright © 2016 Elsevier Inc. All rights reserved.
Pyrexia and neurologic outcomes after therapeutic hypothermia for cardiac arrest
DOI:10.1016/j.resuscitation.2012.11.003
PMID:23153649
[Cited within: 12]

Therapeutic hypothermia, also known as targeted temperature management (TTM), improves clinical outcomes in patients resuscitated from cardiac arrest. Hyperthermia after discontinuation of active temperature management ("rebound pyrexia") has been observed, but its incidence and association with clinical outcomes is poorly described. We hypothesized that rebound pyrexia is common after rewarming in post-arrest patients and is associated with poor neurologic outcomes.Retrospective multicenter US clinical registry study of post-cardiac arrest patients treated with TTM at 11 hospitals between 5/2005 and 10/2011. We assessed the incidence of rebound pyrexia (defined as temperature >38°C) in post-arrest patients treated with TTM and subsequent clinical outcomes of survival to discharge and "good" neurologic outcome at discharge, defined as cerebral performance category (CPC) 1-2.In this cohort of 236 post-arrest patients treated with TTM, mean age was 58.1 ± 15.7 y and 106/236 (45%) were female. Of patients who survived at least 24h after TTM discontinuation (n=167), post-rewarming pyrexia occurred in 69/167 (41%), with a median maximum temperature of 38.7 (IQR 38.3-38.9). There were no significant differences between patients experiencing any pyrexia and those without pyrexia regarding either survival to discharge (37/69 (54%) v 51/98 (52%), p=0.88) or good neurologic outcomes (26/37 (70%) v 42/51 (82%), p=0.21). We compared patients with marked pyrexia (greater than the median pyrexia of 38.7°C) versus those who experienced no pyrexia or milder pyrexia (below the median) and found that survival to discharge was not statistically significant (40% v 56% p=0.16). However, marked pyrexia was associated with a significantly lower proportion of CPC 1-2 survivors (58% v 80% p=0.04).Rebound pyrexia occurred in 41% of TTM-treated post-arrest patients, and was not associated with lower survival to discharge or worsened neurologic outcomes. However, among patients with pyrexia, higher maximum temperature (>38.7°C) was associated with worse neurologic outcomes among survivors to hospital discharge.Copyright © 2012 Elsevier Ireland Ltd. All rights reserved.
The influence of post-rewarming temperature management on post-rewarming fever development after cardiac arrest
DOI:10.1016/j.resuscitation.2015.09.381
PMID:26410566
[Cited within: 16]

We evaluated the influence of post-rewarming temperature management (PRTM) on post-rewarming fever development and determined the association between the temperature in the immediate post-targeted temperature management (TTM) period and outcomes.This retrospective observational study included consecutive adult cardiac arrest survivors treated with TTM from January 2008 to December 2013. Beginning in August 2010, our institution implemented a PRTM protocol involving continued use of temperature management device to maintain normothermia during the first 24h after rewarming. The outcomes were in-hospital mortality and neurologic outcome at discharge. We evaluated the effect on clinical outcomes of post-rewarming fever defined at a temperature over 38 °C within 48 h after rewarming.Of 277 included patients, 55.2% underwent PRTM. The incidence of post-rewarming fever did not differ between the PRTM and no-PRTM groups (odds ratio [OR] 0.963, confidence interval [CI] 0.519, 1.787). Post-rewarming fever was associated with decreased in-hospital mortality (OR 0.243, CI 0.110, 0.534) and decreased rate of unfavorable neurologic outcome (OR 0.312, CI 0.182, 0.534). During 48 h following rewarming, mean temperature was 36.5 °C (36.2-36.8 °C), and peak temperature was 37.5 °C (36.8-38.1 °C). On multivariate analyses, lower mean temperature was associated with increased in-hospital mortality (OR 0.099, CI 0.037, 0.262) and unfavorable neurologic outcome (OR 0.071, CI 0.026, 0.193).It appeared that PRTM did not prevent post-rewarming fever development. Post-rewarming fever was associated with favorable outcomes while lower body temperature after rewarming was associated with unfavorable outcomes. Our results require further confirmation by larger prospective studies.Copyright © 2015 Elsevier Ireland Ltd. All rights reserved.
Early post-rewarming fever is associated with favorable 6-month neurologic outcomes in patients with out-of-hospital cardiac arrest: a multicenter registry study
DOI:10.3390/jcm9092927
URL
[Cited within: 13]

We investigated the association between post-rewarming fever (PRF) and 6-month neurologic outcomes in cardiac arrest survivors. This was a multicenter study based on a registry of comatose adult (³ 18years) out-of-hospital cardiac arrest (OHCA) survivors who underwent targeted temperature management between October 2015 to December 2018. PRF was defined as peak temperature ≥ 38.0 °C within 72 h after completion of rewarming, and PRF timing was categorized as within 24, 24–48, and 48–72 h epochs. The primary outcome was neurologic outcomes at six months after cardiac arrest. Unfavorable neurologic outcome was defined as cerebral performance categories three to five. A total of 1031 patients were included, and 642 (62.3%) had unfavorable neurologic outcomes. PRF developed in 389 (37.7%) patients in 72 h after rewarming: within 24 h in 150 (38.6%), in 24–48 h in 155 (39.8%), and in 48–72 h in 84 (21.6%). PRF was associated with improved neurologic outcomes (odds ratio (OR), 0.633; 95% confidence interval (CI), 0.416–0.963). PRF within 24 h (OR, 0.355; 95% CI, 0.191–0.659), but not in 24–48 h or 48–72 h, was associated with unfavorable neurologic outcomes. Early PRF within 24 h after rewarming was associated with favorable neurologic outcomes.
Clinical effect of rebound hyperthermia after cooling postcardiac arrest: a meta-analysis
DOI:10.1089/ther.2017.0009
PMID:28731840
[Cited within: 13]

Rebound hyperthermia (RH) is frequently seen after completion of targeted temperature management (TTM) in comatose survivors of cardiac arrest. However, its clinical significance is not well understood. Previous studies analyzing the association of RH with clinical outcome have reported conflicting results. The purpose of this meta-analysis is to examine the impact of RH after completion of TTM in patients postcardiac arrest. We reviewed six studies that evaluated the incidence of RH (T > 38°C) with documentation of outcome based on the presence of hyperthermia. We reviewed all six articles and extracted the data for mortality and neurological outcome. A total of 729 patients were analyzed for neurological outcome and 950 patients were analyzed for mortality. RH was found to be associated with a significantly worse neurological outcome (odds ratio [OR] 1.55; 95% confidence interval [CI] 1.13-2.14). RH was not significantly associated with a higher mortality (OR 1.31; 95% CI 1.00-1.72). We also analyzed three studies totaling 206 patients for neurological outcomes and mortality that included patients with severe RH (T > 38.5°C). Severe RH was found to be associated with significantly worse neurological outcome (OR 1.92, 95% CI 1.28-1.90) and significantly worse mortality (OR 2.22, 95% CI 1.50-3.29). RH is common after completion of TTM in comatose patients because of cardiac arrest and is associated with poor neurological outcomes. The clinical impact of RH is likely proportional to the magnitude of RH.
Greater temperature variability is not associated with a worse neurological outcome after cardiac arrest
DOI:10.1016/j.resuscitation.2015.09.004
PMID:26386374
[Cited within: 10]

Spontaneous alterations in temperature homeostasis after cardiac arrest (CA) are associated with worse outcome. However, it remains unclear the prognostic role of temperature variability (TV) during cooling procedures. We hypothesized that low TV during targeted temperature management (TTM) would be associated with a favourable neurological outcome after CA.We reviewed data from all comatose patients after in-hospital or out-of-hospital CA admitted to our Department of Intensive Care between December 2006 and January 2014 who underwent TTM (32-34°C) and survived at least 24h. We collected demographic data, CA characteristics, intensive care unit (ICU) survival and neurological outcome at three months (favourable neurological outcome was defined as cerebral performance category 1-2). TV was expressed using the standard deviation (SD) of all temperature measurements during hypothermia; high TV was defined as an SD >1°C.Of the 301 patients admitted over the study period, 72 patients were excluded and a total of 229 patients were studied; 88 had a favourable neurological outcome. The median temperature on ICU admission was 35.8 [34.9-36.9]°C and the median time to hypothermia (body temperature <34°C), was 4 [3-7] h. Median TV was 0.9 [0.6-1.0]°C and 57 patients (25%) had high TV. In multivariable logistic regression, witnessed CA, ventricular fibrillation/tachycardia and previous neurological disease were independent risk factors for high TV. Younger age, bystander cardiopulmonary resuscitation, shorter time to return of spontaneous circulation, cardiac origin of arrest, shockable rhythm and longer time to target temperature were independent predictors of favourable neurological outcome, but TV was not.Among comatose survivors treated with TTM after CA, 25% of patients had high TV; however, this was not associated with a worse neurologic outcome.Copyright © 2015 Elsevier Ireland Ltd. All rights reserved.
A 4-year implementation strategy of aggressive post-resuscitation care and temperature management after cardiac arrest
DOI:10.1016/j.resuscitation.2014.05.019
PMID:24892264
[Cited within: 2]

target temperature management (TTM) not only improves neurological outcome and survival but has given momentum to a more aggressive and comprehensive treatment after resuscitation. Yet, implementation issues represent the main obstacle to systematic treatment with TTM and aggressive post-resuscitation care. We devised a strategy to introduce, monitor and improve the quality of aggressive treatment after resuscitation, including TTM.standard operative procedures on aggressive post-resuscitation care, written jointly by physicians and nurses, were introduced in November 2004. Data of all resuscitated patients admitted to the ICU were prospectively acquired for 4 years. Periodic audits (every 16 months) were programmed, leading to three equally long periods. Several critical issues were identified after each audit and addressed subsequently, leading to a growing complexity of care. Moreover, after 2 years we introduced an educational programme with medical credits for all staff attending critically ill patients. Neurological outcome and survival at hospital discharged were compared to historical controls of the preceding 22 months.129 consecutively resuscitated patients were admitted to the ICU in the 4-year study period. Of these, 96 (74%) were treated with TTM and aggressive post-resuscitation care. Favourable neurological recovery among patients discharged alive significantly improved in the 4-year intervention period (81% vs. 50% in historical controls, p<0.01). A composite endpoint of mortality and poor neurological outcome also improved (64% vs. 82% respectively, p<0.05). Overall survival increased throughout the 4 years, leading to a significant improvement in the 3rd period compared to historical controls (60% vs. 35%; p<0.05).we propose a strategy to successfully introduce and implement TTM and aggressive post-resuscitation care via standard operative procedures, periodic audits and feedback. Continuous education among other factors contributed to a significant improvement in neurological outcome and a progressive increase in survival.Copyright © 2014 Elsevier Ireland Ltd. All rights reserved.
Assessment of risk factors for post-rewarming rebound hyperthermia in cardiac arrest patients undergoing therapeutic hypothermia
DOI:10.1016/j.resuscitation.2013.03.027
PMID:23567472
[Cited within: 13]

The outcomes associated with therapeutic hypothermia (TH) after cardiac arrest, while overwhelmingly positive, may be associated with adverse events. The incidence of post-rewarming rebound hyperthermia (RH) has been relatively unstudied and may worsen survival and neurologic outcome. The purpose of this study was to determine the incidence and risk factors associated with RH as well as its relationship to mortality, neurologic morbidity, and hospital length of stay (LOS).A retrospective, observational study was performed of adult patients who underwent therapeutic hypothermia after an out-of-hospital cardiac arrest. Data describing 17 potential risk factors for RH were collected. The primary outcome was the incidence of RH while the secondary outcomes were mortality, discharge neurologic status, and LOS.141 patients were included. All 17 risk factors for RH were analyzed and no potential risk factors were found to be significant at a univariate level. 40.4% of patients without RH experienced any cause of death during the initial hospitalization compared to 64.3% patients who experienced RH (OR: 2.66; 95% CI: 1.26-5.61; p=0.011). The presence of RH is not associated with an increase in LOS (10.67 days vs. 9.45 days; absolute risk increase=-1.21 days, 95% CI: -1.84 to 4.27; p=0.434). RH is associated with increased neurologic morbidity (p=0.011).While no potential risk factors for RH were identified, RH is a marker for increased mortality and worsened neurologic morbidity in cardiac arrest patients who have underwent TH.Copyright © 2013 Elsevier Ireland Ltd. All rights reserved.
Factors associated with rebound hyperthermia after targeted temperature management in out-of-hospital cardiac arrest patients: an explorative substudy of the time-differentiated therapeutic hypothermia in out-of-hospital cardiac arrest survivors trial
DOI:10.1097/CCE.0000000000000458
PMID:34250498
[Cited within: 14]

To investigate rebound hyperthermia following targeted temperature management after cardiac arrest and its impact on functional outcome.Post hoc analysis.Ten European ICUs.Patients included in the time-differentiated therapeutic hypothermia in out-of-hospital cardiac arrest survivors trial treated with targeted temperature management at 33°C for 48 or 24 hours. Favorable functional outcome was defined as a Cerebral Performance Category of 1 or 2 at 6 months.None.Of 338 included patients, 103 (30%) experienced rebound hyperthermia defined as a maximum temperature after targeted temperature management and rewarming exceeding 38.5°C. Using multivariate logistic regression analysis, increasing age (odds ratio, 0.97; 95% CI, 0.95-0.99; = 0.02) and severe acute kidney injury within 72 hours of ICU admission (odds ratio, 0.35; 95% CI, 0.13-0.91; = 0.03) were associated with less rebound hyperthermia, whereas male gender (odds ratio, 3.94; 95% CI, 1.34-11.57; = 0.01), highest C-reactive protein value (odds ratio, 1.04; 95% CI, 1.01-1.07; = 0.02), and use of mechanical chest compression during cardiopulmonary resuscitation (odds ratio, 2.00; 95% CI, 1.10-3.67; = 0.02) were associated with more rebound hyperthermia. Patients with favorable functional outcome spent less time after rewarming over 38.5°C (2.5% vs 6.3%; = 0.03), 39°C (0.14% vs 2.7%; < 0.01), and 39.5°C (0.03% vs 0.71%; < 0.01) when compared with others. Median time to rebound hyperthermia was longer in the unfavorable functional outcome group (33.2 hr; interquartile range, 14.3-53.0 hr vs 6.5 hr; interquartile range, 2.2-34.1; < 0.01). In a predefined multivariate binary logistic regression model, rebound hyperthermia was associated with decreased odds of favorable functional outcome (odds ratio, 0.42; 95% CI, 0.22-0.79).One-third of targeted temperature management patients experience rebound hyperthermia, and it is more common in younger male patients with an aggravated inflammatory response and those treated with a mechanical chest compression device. Later onset of rebound hyperthermia and temperatures exceeding 38.5°C associate with unfavorable outcome.Copyright © 2021 The Authors. Published by Wolters Kluwer Health, Inc. on behalf of the Society of Critical Care Medicine.
Prevalence and effect of fever on outcome following resuscitation from cardiac arrest
DOI:10.1016/j.resuscitation.2013.03.038
PMID:23619740
[Cited within: 1]

Evaluate the prevalence of fever in the first 48 h after cardiac arrest and its effect on outcomes.Review of patients treated between 1/1/2005 and 6/30/2010. Fever was defined as T ≥ 38.0°C. We classified categories of post-cardiac arrest illness severity as (I) awake, (II) coma+mild cardiopulmonary dysfunction (SOFA cardiac+respiratory score <4), (III) coma+moderate-severe cardiopulmonary dysfunction, and (IV) deep coma. Associations between fever and survival or good neurologic outcome were examined between hypothermia (TH) and non-TH groups.In 336 patients, mean age was 60 years (SD 16), 63% experienced out-of-hospital cardiac arrest and 65% received TH. A shockable rhythm was present in 40%. Post arrest illness severity was category II in 38%, category III in 20%, and category IV in 42%. Fever was present in 42% of subjects, with a post-arrest median onset of 15 h in the non-TH cohort and 36 h in TH cohort. Fever was not associated with survival within the whole cohort (OR 0.32, CI 0.15, 0.68) or TH cohort (OR 1.21, CI 0.69, 2.14), but was associated with survival in non-TH cohort (OR 0.47, CI 0.20, 1.10). Fever was not associated with good outcomes in the whole cohort (OR 0.83, CI 0.49, 1.40), TH cohort (OR 1.09, CI 0.56, 2.12) or non-TH cohort (OR 0.34, CI 0.11, 1.06).The development of fever within the first 48 h after ROSC is common. Fever is associated with death in non-TH patients. TH treatment appears to mitigate this effect, perhaps by delaying fever onset.Copyright © 2013 Elsevier Ireland Ltd. All rights reserved.
Impact of controlled normothermia following hypothermic targeted temperature management for post-rewarming fever and outcomes in post-cardiac arrest patients: a propensity score-matched analysis from a multicentre registry
DOI:10.1016/j.resuscitation.2021.03.006
PMID:33766661
[Cited within: 4]

We investigated whether controlled normothermia (CN) after the rewarming phase of targeted temperature management (TTM) is associated with preventing post-rewarming fever and outcomes 6 months after out-of-hospital cardiac arrest (OHCA).This was an analysis of a prospective registry comprising OHCA patients treated with TTM at 22 academic hospitals between October 2015 and December 2018. We calculated the incremental area under the curve (iAUC) for body temperature greater than or equal to 37.5 °C for each patient during the first 24 h after the end of rewarming. The relationships among CN and iAUC, 6-month survival and good neurological outcome were analysed. To minimize differences in the baseline characteristics of the patients, we used propensity score-matched analysis.In total, 1144 patients were enrolled. After propensity score matching, 646 patients (comprising 323 pairs) were obtained. In the unmatched cohort, post-rewarming CN was significantly associated with a lower iAUC (0.34 [1.38] vs. 1.19 [2.27]; p < 0.001) but not 6-month survival (adjusted odds ratio (OR): 1.121; 95% confidence interval (CI): 0.836-1.504; p = 0.446) and good neurological outcome (adjusted OR: 1.030; 95% CI: 0.734-1.446; p = 0.863). The results were similar in the propensity score-matched cohort (0.38 [1.56] vs. 1.03 [2.21], p < 0.001, OR: 1.347, 95% CI: 0.989-1.835, p = 0.059 and OR: 1.280, 95% CI 0.925-1.772, p = 0.137, respectively).Post-rewarming CN prevents high fever in the normothermia phase of TTM. However, our data suggest the lack of association between CN and the patient's 6-month survival and good neurological outcome.Copyright © 2021. Published by Elsevier B.V.
High heat generation is associated with good neurologic outcome in out-of-hospital cardiac arrest survivors underwent targeted temperature management at 33 °C
DOI:10.1016/j.resuscitation.2020.06.014 URL [Cited within: 2]
Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement
DOI:10.1186/2046-4053-4-1 [Cited within: 1]
Reliability of the Cerebral Performance Category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study
DOI:10.1186/1757-7241-19-1 URL [Cited within: 1]
Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis
DOI:10.1161/01.STR.0000258355.23810.c6
PMID:17272767
[Cited within: 1]

The modified Rankin scale (mRS), a clinician-reported measure of global disability, is widely applied for evaluating stroke patient outcomes and as an end point in randomized clinical trials. Extensive evidence on the validity of the mRS exists across a large but fragmented literature. As new treatments for acute ischemic stroke are submitted for agency approval, an appreciation of the mRS's attributes, specifically its relationship to other stroke evaluation scales, would be valuable for decision-makers to properly assess the impact of a new drug on treatment paradigms. The purpose of this report is to assemble and systematically assess the properties of the mRS to provide decision-makers with pertinent evaluative information.A Medline search was conducted to identify reports in the peer-reviewed medical literature (1957-2006) that provide information on the structure, validation, scoring, and psychometric properties of the mRS and its use in clinical trials. The selection of articles was based on defined criteria that included relevance, study design and use of appropriate statistical methods.Of 224 articles identified by the literature search, 50 were selected for detailed assessment. Inter-rater reliability with the mRS is moderate and improves with structured interviews (kappa 0.56 versus 0.78); strong test-re-test reliability (kappa=0.81 to 0.95) has been reported. Numerous studies demonstrate the construct validity of the mRS by its relationships to physiological indicators such as stroke type, lesion size, perfusion and neurological impairment. Convergent validity between the mRS and other disability scales is well documented. Patient comorbidities and socioeconomic factors should be considered in properly applying and interpreting the mRS. Recent analyses suggest that randomized clinical trials of acute stroke treatments may require a smaller sample size if the mRS is used as a primary end point rather than the Barthel Index.Multiple types of evidence attest to the validity and reliability of the mRS. The reported data support the view that the mRS is a valuable instrument for assessing the impact of new stroke treatments.
Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses
DOI:10.1007/s10654-010-9491-z PMID:20652370 [Cited within: 1]
Clinical effect of rebound hyperthermia after cooling postcardiac arrest: a meta-analysis
DOI:10.1089/ther.2017.0009
PMID:28731840
[Cited within: 1]

Rebound hyperthermia (RH) is frequently seen after completion of targeted temperature management (TTM) in comatose survivors of cardiac arrest. However, its clinical significance is not well understood. Previous studies analyzing the association of RH with clinical outcome have reported conflicting results. The purpose of this meta-analysis is to examine the impact of RH after completion of TTM in patients postcardiac arrest. We reviewed six studies that evaluated the incidence of RH (T > 38°C) with documentation of outcome based on the presence of hyperthermia. We reviewed all six articles and extracted the data for mortality and neurological outcome. A total of 729 patients were analyzed for neurological outcome and 950 patients were analyzed for mortality. RH was found to be associated with a significantly worse neurological outcome (odds ratio [OR] 1.55; 95% confidence interval [CI] 1.13-2.14). RH was not significantly associated with a higher mortality (OR 1.31; 95% CI 1.00-1.72). We also analyzed three studies totaling 206 patients for neurological outcomes and mortality that included patients with severe RH (T > 38.5°C). Severe RH was found to be associated with significantly worse neurological outcome (OR 1.92, 95% CI 1.28-1.90) and significantly worse mortality (OR 2.22, 95% CI 1.50-3.29). RH is common after completion of TTM in comatose patients because of cardiac arrest and is associated with poor neurological outcomes. The clinical impact of RH is likely proportional to the magnitude of RH.
Determinants of heat generation in patients treated with therapeutic hypothermia following cardiac arrest
Hyperthermia: is it an ominous sign after cardiac arrest
PMID:11719121
[Cited within: 1]

To clarify the clinical characteristics of hyperthermia at an early stage after resuscitation from cardiac arrest (CA).We reviewed the medical records of 43 adult patients with non-traumatic out-of-hospital CA, who survived for longer than 24 h after admission to our intensive care unit (ICU) between January, 1995, and December, 1998. The patients were divided into two groups: a clinical brain death (CBD) group (n=23) and a non-CBD group (n=20), and various factors relating to hyperthermia were compared between the two groups.The mean value of peak axillary temperatures within 72 h of admission was 39.8+/-0.9 degrees C for the CBD group, which was significantly greater than 38.3+/-0.6 degrees C for the non-CBD group (P<0.0001). The time of occurrence of the peak axillary temperature was at 19+/-16 h of admission in the CBD group and 20+/-18 h in the non-CBD group (not significantly different). There were no significant differences in risk factors relating to the occurrence of hyperthermia between the two groups, except for the number of patients who received epinephrine at ICU. In 23 patients with a peak axillary temperature of > or =39 degrees C during the first 72 h of hospitalization, brain death was diagnosed in 20 patients, whereas only 3 of 20 patients having a peak axillary temperature of <39 degrees C developed brain death (odds ratio, 37.8; 95% confidence interval, 6.72-212.2).Hyperthermia at an early stage after resuscitation from CA may be associated with the outcome of brain death.
Post-TTM rebound pyrexia after ischemia-reperfusion injury results in sterile inflammation and apoptosis in cardiomyocytes
The immunology of the post-cardiac arrest syndrome
DOI:10.1016/j.resuscitation.2022.08.013 URL [Cited within: 1]
Changing target temperature from 33 ℃ to 36 ℃ in the ICU management of out-of-hospital cardiac arrest: a before and after study
DOI:10.1016/j.resuscitation.2017.01.016 URL [Cited within: 1]
Intravascular versus surface cooling in patients resuscitated from cardiac arrest: a systematic review and network meta-analysis with focus on temperature feedback
DOI:10.1097/CCM.0000000000005463 URL [Cited within: 1]
The influence of rewarming after therapeutic hypothermia on outcome after cardiac arrest
DOI:10.1016/j.resuscitation.2012.04.006
PMID:22521448
[Cited within: 1]

Treatment with hypothermia has been shown to improve outcome after cardiac arrest (CA). Current consensus is to rewarm at 0.25-0.5 °C/h and avoid fever. The aim of this study was to investigate whether active rewarming, the rate of rewarming or development of fever after treatment with hypothermia after CA was correlated with poor outcome.This retrospective cohort study included adult patients treated with hypothermia after CA and admitted to the intensive care unit between January 2006 and January 2009. The average rewarming rate from end of hypothermia treatment (passive rewarming) or start active rewarming until 36 °C was dichotomized in a high (≥ 0.5 °C/h) or normal rate (<0.5 °C/h). Fever was defined as >38 °C within 72 h after admission. Poor outcome was defined as death, vegetative state, or severe disability after 6 months.From 128 included patients, 56% had a poor outcome. Actively rewarmed patients (38%) had a higher risk for poor outcome, OR 2.14 (1.01-4.57), p<0.05. However, this effect disappeared after adjustment for the confounders age and initial rhythm, OR 1.51 (0.64-3.58). A poor outcome was found in 15/21 patients (71%) with a high rewarming rate, compared to 54/103 patients (52%) with a normal rewarming rate, OR 2.61 (0.88-7.73), p = 0.08. Fever was not associated with outcome, OR 0.64 (0.31-1.30), p = 0.22.This study showed that patients who needed active rewarming after therapeutic hypothermia after CA did not have a higher risk for a poor outcome. In addition, neither speed of rewarming, nor development of fever had an effect on outcome.Copyright © 2012 Elsevier Ireland Ltd. All rights reserved.