Abdominal distention after cardiopulmonary resuscitation (CPR) is a common phenomenon that presents in the emergency department. It is caused by a long period of bag-valve mask ventilation or esophageal intubation. However, a rare but life-threating diagnosis should be considered when distention progresses rapidly. Here, we reported a patient who developed a fever and abdominal pain that couldn’t be relieved by gastric decompression.
CASE
A healthy 33-year-old male had fatigue that lasted for one month, cough and dizziness, and he suddenly developed cardiac arrest and was sent to the emergency department. His body mass index (BMI) was 26.4 kg/m2. He had no history of peptic ulcer, mental, infectious or hereditary disease. He never smoked and occasionally had social alcohol drinking. He was diagnosed with acute myocarditis and saved by CPR and defibrillation. A feeding tube was inserted into the duodenum to provide enteral nutrients. However, he developed abdominal distension with a fever of 39.2 ℃ after one week of observation in the intensive care unit (ICU).
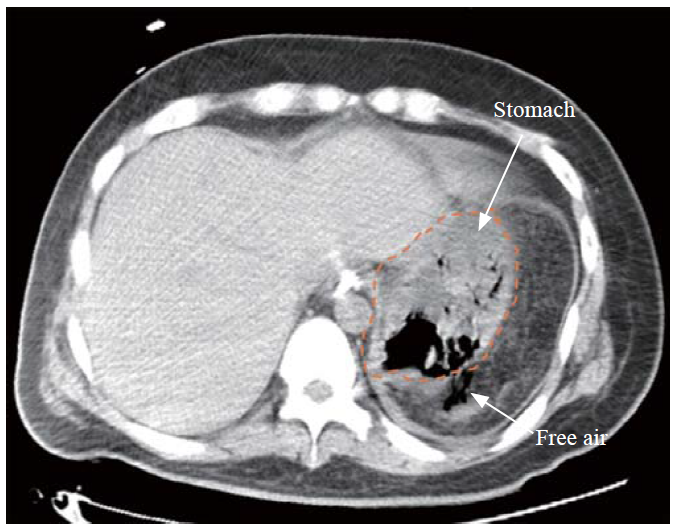
On examination, the patient had significant left upper quadrant tenderness and rebound tenderness on palpation. The laboratory examinations showed obvious elevations in the white blood cell count, C-reactive protein, and D-dimer, which were 18.7×109/L, 250.0 mg/L, and 13,990 μg/L, respectively. Then, acute abdominal computed tomography (CT) with intravenous contrast was performed, and a small amount of extragastric free air was found (Figure 1). Therefore, the initial diagnosis was gastric perforation of an unknown cause with acute peritonitis.
Figure 1.
Figure 1.
An abdominal computed tomography scan indicated extragastric free air (shown in axial view).
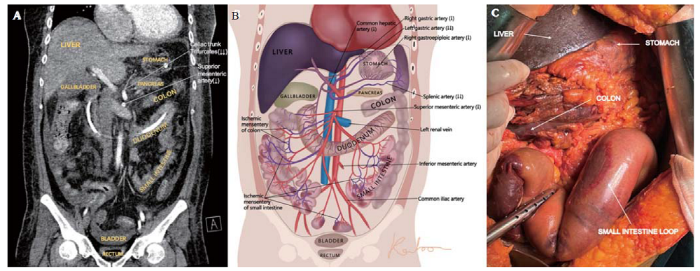
Since the disease was severe and complicated, a multidisciplinary team discussion was held. Upon rigorous observation of the CT images, the radiologist recognized that there was ischemia within the celiac trunk and the superior mesenteric artery (SMA) (Figures 2A and B), which was the main cause of the perforation. In addition, emergency exploratory laparotomy was suggested for perforation repair. A perforation in the fundus of the stomach was identified during the operation. Meanwhile, ischemia and necrosis were revealed in the entire stomach, liver, and most segments of the small intestine and colon (Figure 2C), and no arterial pulse was palpable in the hepatic or splenic artery.
Figure 2.
Figure 2.
Images of a computed tomography (CT) scan and intraoperative photograph. A: the contrast CT scan showed that there was no enhancement of the splenic artery and insufficient enhancement of the left gastric artery, the common hepatic artery and the superior mesenteric artery (shown in coronal view); B: the illustrative picture simulated different degrees of ischemia (↓: decreased blood flow; ↓↓: significantly decreased blood flow); C: intraoperative photograph demonstrated ischemia and necrosis of the entire perforated stomach, liver, and most segments of the small intestine and colon.
His family refused any additional intervention after a detailed intraoperative conversation, and unfortunately, the patient soon died of multiple organ dysfunction syndrome (MODS).
DISCUSSION
Gastric perforation or rupture with pneumoperitoneum was mostly related to massive gastric distension, esophageal intubation, a history of peptic ulcer or other underlying causes and was rarely reported after CPR.[1] Gastric perforation after CPR, if not recognized, is associated with a very high mortality risk.[2] For cases without underlying vascular factors, surgical exploration with primary closure or gastrostomy is indicated for patients with signs of peritonitis, and conservative therapy should be cautiously applied for non-peritonitis patients.[3]
Normally, the stomach is supplied by a rich system of arteries derived from the celiac trunk; thus, it is extremely rare to see entire gastric ischemia. Babu was the first to describe the term “ischemic gastritis”, which referred to acute or chronic mesenteric ischemia with a component of celiac territory ischemia syndrome (CTIS).[4] A previous study documented that perforation of the gastric fundus and splenic infarction could occur after acute occlusion of the celiac trunk or its branches or as a result of ischemia of the celiac artery due to aortic dissection.[5] Another retrospective study concluded that patients with ischemic gastritis would have vomiting, epigastric pain, bleeding or even gastric perforation. This patient developed severe abdominal distention and pain, whereas he had no vomiting or gastrointestinal bleeding. Revascularization of the celiac trunk and SMA via bypass surgery and percutaneous transluminal angioplasty are two alternative treatments for patients with ischemic gastritis.[6] We excluded the possibility of esophageal intubation or improper ventilation as the cause of gastric perforation, and no trauma was seen in the stomach. Although the mechanism of how thromboembolism was formed in the celiac trunk and SMA was unknown, gastric perforation due to CTIS was the most likely explanation based on the CT findings and the intraoperative manifestation of multi-organ ischemia. Emergency physicians should keep this rare complication of CPR in mind. Furthermore, consultations with vascular doctors are necessary to determine the best possible vascular interventions for such cases of ischemia.
CONCLUSIONS
We reported a case of gastric perforation due to CTIS after successful CPR treatment. Clinicians should be aware of this rare complication of CPR when abdominal distention persists with severe pain and fever because an emergency laparotomy and a vascular intervention are needed.
ACKNOWLEDGMENTS
The authors would like to sincerely thank Cong-cong Yu and Jia-ning Chen for their support.
Funding: This work was supported by the Basic Public Welfare Research Project of Zhejiang Province (LGF21H030005); the Zhejiang Provincial Key Project of Research and Development Fund (2019C03043).
Ethical approval: Ethical approval for this study was obtained from the Medical Ethics Committees of the Second Affiliated Hospital of Zhejiang University School of Medicine (approval number 2022-0075).
Conflicts of interest: The author(s) declare no potential conflicts of interest.
Contributors: GFC and KBC contributed equally to this study. GFC, KBC, and JC wrote the manuscript, drew the figures, gained ethical approval and revised the manuscript. All the authors have read and approved the final version of the manuscript.
Reference
Gastric perforation after cardiopulmonary resuscitation: review of the literature
DOI:10.1016/j.resuscitation.2009.11.023
PMID:20064683
[Cited within: 1]

The risk of complications of cardiopulmonary resuscitation (CPR) does not outweigh the benefit of a successful restoration of a spontaneous circulation. Despite the frequent occurrence of gastric distension (caused by air entering the stomach because of too forceful and/or too quick rescue breathing), there are few reports of massive gastric distension causing gastric rupture and pneumoperitoneum after CPR. We reviewed all 67 case reports of gastric perforation that have been reported after CPR. Although uncommon, this review stresses the need to consider this potentially lethal complication after initial successful resuscitation.Copyright 2010. Published by Elsevier Ireland Ltd.
An unusual complication of cardiopulmonary resuscitation: Stomach perforation
Gastric perforation after cardiopulmonary resuscitation
Celiac territory ischemic syndrome in visceral artery occlusion
PMID:8352420
[Cited within: 1]

Abdominal angina that is characterized by postprandial pain, and often associated with weight loss, is a well-recognized symptom complex of mesenteric artery insufficiency (mesenteric territory symptoms). In the past 5 years, we have observed six patients with atypical symptoms who had mesenteric artery occlusion combined with stenosis or occlusion of the celiac artery. Atypical symptoms included severe nausea and vomiting at the sight or smell of food, anorexia, weight loss, and right upper quadrant or epigastric discomfort (celiac territory symptoms). An extensive work-up to rule out gastric, pancreatic, biliary, or colonic pathology was undertaken in these patients. The findings included gallbladder dysfunction, diffuse micro-ulceration of gastric mucosa, and colonic mucosal ulceration. The diagnosis of visceral artery occlusion was initially missed in all six patients. Four patients had cholecystectomy. Visceral angiography confirmed occlusion of the celiac, superior, and inferior mesenteric arteries. Five patients had dramatic resolution of symptoms after restoration of visceral circulation. One patient who developed intestinal infarction before revascularization died. Symptoms suggesting upper abdominal visceral pathology may be a manifestation of celiac artery stenosis/occlusion coexisting with mesenteric artery occlusive disease. Visceral angiography should be part of the work-up in these patients for early diagnosis and prompt management.
Rare case of gastric perforation due to ischemic gastropathy
DOI:10.1016/j.gie.2020.06.061 PMID:32598964 [Cited within: 1]
Ischemic gastritis: a rare but lethal consequence of celiac territory ischemic syndrome
PMID:23232480
[Cited within: 1]

Ischemic gastritis is poorly known by physicians and is often fatal if not correctly diagnosed. Here, we report on the clinical, endoscopic and imaging features and treatment outcomes for five ischemic gastritis patients.This was a retrospective, single-centre study of patients treated for ischemic gastritis between January 2009 and April 2012. All patients underwent transluminal angioplasty or open revascularization surgery.Five patients (4 men, 1 female) were included in the present study. The condition was diagnosed in two cases of peritonitis with gastric or duodenal perforation, two cases of acute epigastric pain and one case of gastric bleeding, profuse vomiting and hypovolemic shock. Three of the five patients had endoscopically proven gastric ulcerations or necrosis. A computed tomography scan contributed to the diagnosis in all cases. The symptoms resolved in all cases after gastric revascularization via an aortohepatic bypass (N.=1), a renohepatic bypass (N.=1), a retrograde iliosuperior mesenteric bypass (N.=2) with associated celiac artery angioplasty (N.=1) and celiac and superior mesenteric artery angioplasty (N.=1). During follow-up, three patients died of starvation due to short bowel syndrome (N.=1) or metastatic lung cancer (N.=2).Ischemic gastritis is a component of celiac territory ischemia syndrome and is closely associated with chronic or acute mesenteric ischemia. Computed tomography always informs the diagnosis. The rapid healing observed here after revascularization confirmed the ischemic nature of the condition and the inappropriateness of gastric resection in this context.