Cardiovascular implantable electronic devices (CIEDs) are widely used in the modern era. Every year, about 730,000 permanent pacemakers and 330,000 CIEDs are implanted worldwide. CIEDs have been known to increase the life expectancy of millions of people and improve their quality of life by controlling the heart rate and atrioventricular and interventricular synchronization and preventing sudden cardiac death.[1] The tricuspid valve consists of the annulus, leaflets, chordae tendineae, and papillary muscles. Interaction between the endocardial lead and any component of this structure can lead to tricuspid valve dysfunction, thereby resulting in tricuspid regurgitation (TR).[2] CIED-related TR has been shown to be an independent predictor of hospitalization for heart failure.[3,4]
In this study, we reviewed the records of patients who had a CIED inserted in our hospital and used three-dimensional (3D) echocardiography to locate the relative position of the endocardial lead to the tricuspid valve, in order to investigate the factors and mechanisms influencing device lead-related TR.
METHODS
Study design
This study included patients who experienced moderate or severe TR following CIED implantation in our hospital from January 2018 to December 2021. Ethical approval was obtained from the research ethics committee of the hospital.
All eligible patients had indications for CIED placement. Patients were excluded for any of the following reasons: cardiogenic shock or those scheduled for cardioversion within 24 h after the procedure; patients with a history of pulmonary embolism, heart surgery, dialysis, acute coronary artery syndrome, or revascularization. After applying similar inclusion criteria, controls who experienced mild TR following CIED implantation were matched (1:3) to cases according to age, sex, and index year.
Data collection
Patient demographic data and device information were collected from the electronic medical records using a standardized form. All the echo assessments were performed by a single investigator, and the acquired data were reanalyzed by another operator (blinded to the patients’ former results). TR was quantified in three grades (mild, moderate, and severe) using the classical variables of regurgitant volume calculated using the proximal isovelocity surface area method. The device lead position at the level of the tricuspid annulus was identified using 3D images obtained from the apical 4-chamber view.
Statistical analysis
Continuous data are presented as the mean±standard deviation (SD), while categorical variables are shown as frequencies (percentages). Differences between two groups were assessed using Student’s t-test for continuous variables and Chi-square test for categorical variables. Logistic regression was used to estimate the association between CIEDs and TR and to calculate the odds ratios (ORs) and 95% confidence intervals (CIs). The kappa (κ) coefficient was calculated to determine interobserver agreement. Statistical significance was set at a P-value <0.05. All statistical analyses were performed using SPSS version 20 (SPSS Inc., USA).
RESULTS
Clinical and two-dimensional (2D) echocardiographic features
Overall, 35 patients (the moderate and severe TR group) and 105 controls (the mild TR group) were included in the analysis. The baseline clinical characteristics of the study sample were presented in supplementary Table 1. Most patients exhibited New York Heart Association (NYHA) class II symptoms, and approximately half of the patients had sinus-node dysfunction.
The 2D echocardiographic characteristics were compared in supplementary Table 2. No significant differences between pre- and post-implantation echocardiograms were observed in the mild TR group, indicating preservation of cardiac structure and function following CIED implantation. Nevertheless, structural parameters, including the left atrium area, right atrium area, right ventricular diameter, and subsequent pulmonary artery systolic pressure, were significantly increased in the moderate and severe TR group. Perfect interobserver (κ=0.93) agreement was achieved for echocardiography measurements.
Device information and 3D echocardiographic characteristics
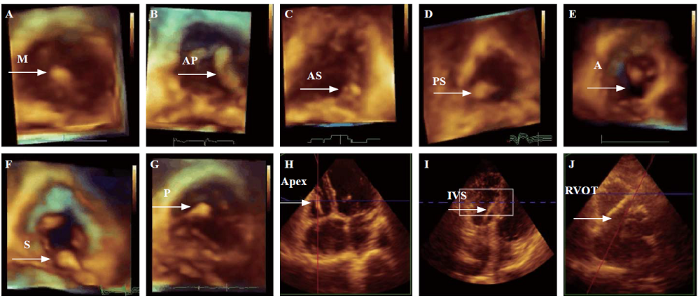
Device information and 3D echocardiographic characteristics were presented in supplementary Table 3. The majority of patients in the moderate and severe TR group received ventricular pacing or implantable cardioverter-defibrillator (ICD) implantation, whereas most patients in the mild TR group received dual-chamber pacing (P<0.01). Furthermore, 3D echocardiography revealed that patients with moderate or severe TR had a significantly greater incidence of interfering leads than those with mild TR. Approximately 65.7% of patients who developed moderate or severe TR had lead-leaflet interference, while this rate was only 10.5% in patients with mild TR. The posterior leaflet was most commonly affected, followed by the septal leaflet. In both groups, the anterior leaflet was the least affected. Representative images were shown in Figure 1. Notably, the location of the lead tip did not differ significantly between the groups.
Figure 1.
Figure 1.
Three-dimensional echocardiography depicts the location of the device lead (A to D: representative images from the mild TR group; E to G: representative images from the moderate and severe TR group) and lead tips (H and I: representative images of lead tips from the mild TR group; J: representative image from the moderate and severe TR group). M: device lead in the middle of the valve; AP: device lead in the anteroposterior commissure; AS: device lead in the anteroseptal commissure; PS: device lead in the posterior-septal commissure; A: anterior leaflet impingement; S: septal leaflet impingement; P: posterior leaflet impingement; IVS: interventricular septal; RVOT: right ventricular outflow tract.
Predictors of CIED-related TR
The associations between CIEDs and TR were shown in Table 1. An increase in risk was observed with atrial fibrillation involving forward rotation (OR 1.814, 95% CI 1.731-1.897). In addition, we investigated the associations with device information. A modest increase in risk was observed who underwent single-chamber pacemaker (OR 1.811, 95% CI 1.732-1.890) and ICD implantation (OR 1.790, 95% CI 1.713-1.867). The association between device lead location and TR was examined. Reduced risks were observed for the presence of inter-leaflet lead (OR 0.440, 95% CI 0.298-0.582).
Table 1. Association between the cardiovascular implantable electronic devices and tricuspid regurgitation
| Variables | Odds ratios | 95% confidence interval | P-value |
|---|---|---|---|
| Atrial fibrillation | 1.814 | 1.731-1.897 | 0.009 |
| Device types | |||
| VVI | 1.811 | 1.732-1.890 | 0.010 |
| DDD | 0.358 | 0.218-0.497 | 0.008 |
| ICD | 1.790 | 1.713-1.867 | 0.012 |
| Device lead locations | |||
| Inter-leaflet | 0.440 | 0.298-0.582 | 0.006 |
| A | 1.761 | 1.687-1.835 | 0.015 |
| P | 1.811 | 1.739-1.884 | 0.013 |
| S | 1.792 | 1.722-1.863 | 0.009 |
VVI: ventricular sensing, ventricular pacing, and ventricular inhibition; DDD: dual-chamber sensing, dual-chamber pacing, and dual-chamber triggering/inhibition; ICD: implantable cardioverter defibrillator; A: anterior leaflet impingement; P: posterior leaflet impingement; S: septal leaflet impingement.
DISCUSSION
In this retrospective study, we evaluated the presence of TR following CIED implantation by using 3D echocardiography. Our results indicated that atrial fibrillation, device type, and interfering leads were associated with post-implantation TR. We did not observe any difference in TR severity in relation to the lead tip location.
The present study showed the useful application of 3D transthoracic echocardiography in the identification of device lead-related TR. By allowing a more detailed assessment of the tricuspid valve and its subvalvular apparatus, 3D was found to be superior to 2D echocardiography in the evaluation of tricuspid valve pathology.[5,6] An en face view of the tricuspid valve leaflets from both the atrial and ventricular aspects can be obtained by 3D echocardiography, allowing the evaluation of all three leaflets from the base to the tip, including the posterior leaflet.[7]
We also found that interfering lead was a major contributor to post-implantation TR. The posterior and septal leaflets were most likely impinged on by device leads, resulting in insufficient valve closure. A previous study indicated that the presence of an interfering lead was the most important factor associated with worsening TR, increasing the likelihood of developing moderate or severe TR by 15- and 11-fold, respectively.[8] As lead positions can be identified with 3D echocardiography, it could be an effective tool for detecting device lead-related TR in patients with CIEDs.
Patients with ventricular pacing and ICD implantation were more likely to develop considerable TR than those with dual-chamber pacing. These results agree with a prior study showing that dual-chamber pacing was superior to ventricular pacing in potentially attenuating electromechanical dyssynchrony and long-term cardiac function decline.[9] ICD leads to more fibrosis and hence more interference with the tricuspid valve results in higher TR.[3] Meanwhile, the transvalvular lead of the ICD may generate additional weight and rigidity to the tricuspid valve due to its calibre.[10]
Our findings revealed that preimplantation atrial fibrillation was involved in the presence of post-implantation TR. Some studies have reported that atrial fibrillation is associated with annular dilation and results in TR even in the absence of device leads.[11]
CONCLUSIONS
Preimplantation atrial fibrillation, device type, and interfering leads are associated with post-implantation TR. To better detect device lead-related TR, 3D echocardiography is recommended for patients with CIEDs.
Funding: This work was supported by grants from the Planned Science and Technology Project of Zhejiang Province, China (2020KY216); Hangzhou City Health Science and Technique Program (OO20190126).
Ethical approval: All these cases provided informed consent, and the study was approved by the Ethics Review Committee of the First Affiliated Hospital, Zhejiang University School of Medicine.
Conflicts of interest: None.
Contributors: LRZ designed the study. YYZ and YC collected the patient data. YYZ wrote the article. All authors read and approved the final manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Evaluating and managing bradycardia
DOI:10.1016/j.tcm.2019.07.001 URL [Cited within: 1]
Comparison of outcomes in patients with heart failure with versus without lead-induced tricuspid regurgitation after cardiac implantable electronic devices implantations
DOI:10.1016/j.amjcard.2020.05.039 URL [Cited within: 1]
Long-term follow-up of mortality and heart failure hospitalisation in patients with intracardiac device-related tricuspid regurgitation
DOI:10.1016/j.hlc.2020.08.028
PMID:33132050
[Cited within: 2]

Tricuspid regurgitation (TR) is a known complication of cardiac implantable electronic devices (CIED). A better understanding of the patient population affected by this complication and their outcomes is needed. The aims of our study were to: 1) describe the incidence of CIED-related tricuspid regurgitation; 2) identify patient characteristics conferring risk; 3) assess the long-term risk of hospitalisation for heart failure and mortality in patients with this complication.This was a retrospective cohort study of 2,265 patients that had a de novo device implantation at a tertiary referral centre between January 2010 and December 2017. Patients with echocardiograms prior to and at least 3 months after device implantation were included. Patients with moderate or severe TR at baseline were excluded.Following screening of medical records, 165 patients were analysed. Forty-four (44) (27%) patients developed new-onset moderate or severe device-related TR, without a significant difference between patients with permanent pacemaker (PPM) and implantable cardioverter-defibrillator (ICD). Patients with CIED-related tricuspid regurgitation had a higher rate of hospitalisation for heart failure than those without (63.6% vs 34.7%, p=0.001) during a median follow-up of 29 months (IQR 13-60 months). Subsequent analyses showed that the association between CIED-related TR and heart failure hospitalisation only became significant in the period beyond 12 months following CIED implantation. Piecewise Cox regression analysis stratified at 12 months of follow-up showed that CIED-related TR was associated with an increased risk of heart failure hospitalisation beyond 12 months after adjustment for differences in baseline characteristics (HR 1.99, 95% CI 1.05-3.76, p=0.03). There was a higher mortality rate in the group with CIED-related TR; however, this did not reach significance (36.3% vs 22.3%, p=0.09).CIED-related TR is common and clinically significant with serious implications for long-term outcomes, especially congestive heart failure.Copyright © 2020 Australian and New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) and the Cardiac Society of Australia and New Zealand (CSANZ). Published by Elsevier B.V. All rights reserved.
Transcatheter aortic valve replacement in Asia: present status and future perspectives
DOI:10.1016/j.jacasi.2021.10.006 URL [Cited within: 1]
Tricuspid valve geometry in patients with functional tricuspid regurgitation: a three-dimensional echocardiographic study
DOI:10.1111/echo.14747
PMID:32472613
[Cited within: 1]

Tricuspid valve (TV) has a complex anatomy causing some difficulties in echocardiographic evaluation. In this study, we sought to assess the geometry of TV in patients with functional tricuspid regurgitation (TR) by the implementation of 2- and 3-dimennsional (2D and 3D) echocardiography.In a case-control study, the geometrical features of TV were evaluated in forty patients with functional TR using echocardiographic examinations, and those data compared with twenty-five age- and sex-matched healthy individuals.The mean age of patients was 50 ± 12 years, and 75% were female. All echocardiographic features of TV geometry were significantly greater in TR compared to control group. The 3D evaluation of TV annulus showed that the annulus shape was more circular in the TR compared to the control group. When compared patients with moderate and severe TR, there was a significant difference between groups regarding the size of the TV septolateral annulus diameter (3.5 ± 0.4 vs 3.9 ± 0.7 cm; P =.048), and the angle between mitral valve and TV annuluses (12.5 ± 4.3 vs 17 ± 9º; P =.048). Tenting areas measured by 2D echocardiography and obtained by TomTec software were significantly greater in severe TR compared to moderate TR group. The diameter of TV by 2D echocardiography was significantly higher in atrial fibrillation than that in sinus rhythm group among patients with TR.The implementation of 3D echocardiography is useful in the determination of TV geometry in patients with functional TR. The accurate evaluation of anatomical features of TV might provide valuable tools in the evaluation of patients with functional TR.© 2020 Wiley Periodicals LLC.
Clinical impact of size, shape, and orientation of the tricuspid annulus in tricuspid regurgitation as assessed by three-dimensional echocardiography
DOI:10.1016/j.echo.2019.09.016 URL [Cited within: 1]
Mechanisms of Mitral Regurgitation: New insights from 3D echocardiography and implications for transcatheter repair
DOI:10.1016/j.jacasi.2021.04.004 URL [Cited within: 1]
Features of lead-induced tricuspid regurgitation in patients with heart failure events after cardiac implantation of electronic devices: a three-dimensional echocardiographic study
DOI:10.1253/circj.CJ-20-0620
PMID:33071243
[Cited within: 1]

Lead-induced tricuspid regurgitation (TR) after cardiac implantable electronic device (CIED) implantation is not fully understood. This study aimed to reveal the features of lead-induced TR by 3-dimensional echocardiography (3DE) in patients with heart failure (HF) events after CIED implantation.Methods and Results:In 143 patients, 3DE assessments for the tricuspid valve (TV) and right ventricular morphologies were sequentially performed within 3 days after CIED implantations, during TR exacerbations, and at ≥6 months after TR exacerbations. TR exacerbations were observed in 29 patients (median 10 months after CIED implantation, range 1-28 months), 15 of whom had lead-induced TR. In the 29 patients, the tenting height of the TV, tricuspid annular (TA) height, and TA area at baseline were independent predictors for worsening TR. In patients with lead-induced TR, tenting height of the TV and TA area were identified as the risk factors. In addition, all patients with a lead positioned on a leaflet immediately after CIED implantations developed lead-induced TR. At follow up, TR exacerbation of lead-induced TR persisted with TA remodeling, but it was improved in the lead non-related-TR group.TA remodeling at baseline and a lead location on a leaflet immediately after CIED implantation were associated with lead-induced TR in patients with HF events after CIED implantation. Persistent TA remodeling may make lead-induced TR refractory against HF treatments.
Update in cardiac pacing
DOI:10.15420/aer.2019.15.3 URL [Cited within: 1]
Tricuspid regurgitation associated with implantable electrical device insertion: a systematic review and meta-analysis
DOI:10.1111/pace.14287 URL [Cited within: 1]
Influence of atrial fibrillation on functional tricuspid regurgitation in patients with HeartMate 3
DOI:10.1161/JAHA.120.018334 URL [Cited within: 1]