Spontaneous intracerebral hemorrhage (ICH) represents the second most common type of stroke, with high mortality and disability rates.[1,2] In 2010, there were approximately 5.3 million ICH cases, with 3 million deaths worldwide.[1] However, there is still no validated medical treatment for ICH, with the role of surgery remaining controversial.[2,3] Cusack et al[4] demonstrated that lowering blood pressure rapidly in hypertensive ICH patients may be safe and at least partially effective in inhibiting hematoma expansion.
For critically ill patients suffering from an emergent disease, the initial care provided in the emergency department (ED) strongly impacts their outcomes,[5]which has been the focus of many studies.[6⇓-8] In patients with spontaneous ICH, Elmer et al[9]demonstrated that no significantly worse outcome was found in patients with longer ED length of stay (EDLOS). Another study published that prolonged EDLOS can serve as a predictor for adverse outcomes in spontaneous ICH patients.[5] However, the conclusions from these studies were limited by their comparably small sample sizes. Early and aggressive management in the acute phase of spontaneous ICH may mitigate a secondary brain injury.[10] Thus, it is still disputed whether shortening the EDLOS would be beneficial to ICH patients.
The impact of the EDLOS in spontaneous ICH patients has not been well investigated in China, and a study with a sufficiently large sample size is needed to further demonstrate this issue. With a large number of patients in West China Hospital, the study aims to determine the association between the EDLOS and outcome in spontaneous ICH patients. We hypothesized that prolonged EDLOS was associated with a poor outcome.
METHODS
Study design and setting
We present a single-center, retrospective observational study of spontaneous ICH patients admitted to the ED within 24 h of onset between January 2017 and January 2019. Patients who were admitted to the ED and had complete data at admission and follow-up were included. Patients who were younger than 16 years old, hospitalized, or suffered in-hospital ICH were excluded. Acute hemorrhagic stroke care in the ED at West China Hospital is driven by an acute stroke emergency response system. After an initial assessment of the patients, the ED nurses triaged the ICH patients into the emergency room (ER) in an emergency procedure. A response team would be activated, which includes neuroradiology, neurosurgery, and neuro-intensive care specialists who actively manage patients in collaboration with the ED staff. These ICH patients received necessary rescue measures, including blood pressure maintenance, tracheal intubation, oxygen inhalation, urethral catheterization, and computed tomography angiography (CTA), until stable vital signs were reached. Basic admission examination and blood sample collection were conducted at the same time. Then, the patients left the ER and were assigned to the intensive care unit (ICU) or mostly to the neurologic ward. All patients or their relatives signed an informed consent document after the study procedures were explained in detail.
Data collection
Medical records of patients were reviewed by two researchers and documented in a personal computer tabulated database. The following information was recorded: demographics, vitals, complications, radiological characteristics, and laboratory data. The ICH volume was calculated using the ABC/2 method. A was the largest hemorrhage diameter by computed tomography (CT), B was the diameter 90° to A, and C was the approximate number of CT slices with hemorrhage multiplied by the slice thickness. The study population was divided into two groups based on their EDLOS. The EDLOS was calculated as the time in hours from ED triage to the time that the patient was physically transferred to the ICU or to the neurologic ward. The primary outcomes included mortality at discharge and three months after discharge, which we followed up via telephone or outpatient interviews. The secondary outcomes were defined as the the mRS score at discharge and three months after discharge.
Statistical analysis
Demographics and clinical characteristics were reported using median and interquartile range (IQR) for continuous variables and proportions for categorical variables. The Kolmogorov-Smirnov test was used to determine the normality and was performed for each continuous variable. Comparisons between groups were made using Student's t-test or Mann-Whitney U-test for continuous variables and Chi-square or Fisher's exact tests for categorical variables. A preliminary univariate logistic analysis for predictors of primary and secondary outcomes was performed, and multivariate models were then constructed using variables significant in the univariate analysis at a P-value <0.05. All analyses were performed with R software (version 3.6.2).
RESULTS
Demographic characteristics of patients and controls
A total of 739 spontaneous ICH patients were included in the study. The demographic data of the subjects are presented in supplementary Table 1. The median age of the patients was 55 years, ranging from 46 to 67 years. The median volume of bleeding was 25.0 mL, ranging from 15.0 to 39.5 mL. For Glasgow Coma Scale (GCS) and mRS scores at ED admission, the median and range were 13.0 (IQR 8.0-15.0) and 2.0 (IQR 1.0-3.0), respectively. The length of the EDLOS was 0.9 (IQR 0.6-1.9) h, so the patients were divided by the median EDLOS (1 h). Similarly, the discharge mRS score was dichotomized at a median score of 2. Continuous covariates, such as heart rate and glucose, were significantly different in the EDLOS <1 h group and the EDLOS ≥1 h group (P<0.01). No dichotomous covariates except survival at discharge and survival three months after discharge were significantly different between the two groups.
Table 1. Univariate and multivariate logistic regression analysis results of significant predictors for discharge mortality and three-month mortality
| Parameters | Survival at discharge | Survival at three months after discharge | ||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Univariate | ||||
| Age | 1.05 (1.03-1.07) | <0.01 | 1.05 (1.03-1.06) | <0.01 |
| Bleeding volume | 1.04 (1.02-1.05) | <0.01 | 1.04 (1.02-1.05) | <0.01 |
| Intraventricular hemorrhage | 2.27 (1.33-3.99) | <0.01 | 2.47 (1.48-4.27) | <0.01 |
| Diabetes | 2.58 (1.32-4.81) | <0.01 | 2.56 (1.33-4.68) | <0.01 |
| Kidney disease* | 2.95 (1.33-6.03) | <0.01 | 2.64 (1.20-5.38) | 0.01 |
| Anti-platelet drugs | 4.37 (0.93-16.14) | 0.04 | - | - |
| GCS score | 0.76 (0.70-0.82) | <0.01 | 0.73 (0.67-0.79) | <0.01 |
| Initial mRS scores | 2.23 (1.76-2.85) | <0.01 | 2.64 (2.08-3.41) | <0.01 |
| Intubation | 3.66 (2.17-6.39) | <0.01 | 4.03 (2.42-6.91) | <0.01 |
| Re-intubation | 4.14 (1.56-9.91) | <0.01 | 3.67 (1.39-8.76) | <0.01 |
| Glucose | 1.15 (1.09-1.22) | <0.01 | 1.14 (1.08-1.21) | <0.01 |
| LDL-C* | 0.75 (0.56-0.99) | 0.04 | - | - |
| Cl | 0.92 (0.87-0.97) | <0.01 | 0.93 (0.88-0.97) | <0.01 |
| WBC | 1.08 (1.03-1.13) | <0.01 | 1.08 (1.03-1.13) | <0.01 |
| NC | 1.06 (1.01-1.12) | 0.02 | 1.07 (1.02-1.12) | 0.01 |
| LC | 1.39 (1.15-1.68) | <0.01 | 1.36 (1.13-1.64) | <0.01 |
| Hematocrit* | 0.01 (0.00-0.56) | 0.02 | - | - |
| EDLOS ≥1 h | 1.88 (1.14-3.14) | 0.01 | 1.99 (1.23-3.27) | 0.01 |
| Multivariate | ||||
| Age | 1.06 (1.03-1.08) | <0.01 | 1.07 (1.05-1.10) | <0.01 |
| Kidney disease | 3.48 (1.20-9.49) | 0.02 | 2.84 (1.00-7.53) | 0.04 |
| GCS score | 0.69 (0.53-0.90) | 0.01 | 0.73 (0.57-0.94) | 0.02 |
| Intubation | - | - | 2.19 (1.14-4.28) | 0.02 |
| Re-Intubation | 3.31 (1.03-10.09) | 0.04 | - | - |
| Cl* | 0.91 (0.85-0.97) | <0.01 | 0.93 (0.87-0.99) | 0.02 |
| EDLOS ≥1 h | 2.60 (1.39-4.97) | <0.01 | 2.82 (1.54-5.28) | <0.01 |
OR: odds ratio; CI: confidence interval; GCS: Glasgow Coma Scale; mRS: modified Ranking Scale; LDL-C: low-density lipoprotein cholesterol; Cl: chlorine; WBC: white blood cell; NC: neutrophil; LC: leukocyte; EDLOS: emergency department length of stay. *: the predictors were not statistically significant in the logistics regression analysis for three-month mortality.
Predictors of outcome
In the univariate analysis, the following variables were predictors of mortality at discharge: age, bleeding volume, intraventricular hemorrhage, diabetes, kidney disease, lung disease, the use of antiplatelet drugs, initial mRS scores, intubation, re-intubation, glucose, and longer EDLOS. There were also some good outcome predictors: GCS score, low-density lipoprotein cholesterol (LDL-C), chlorine (Cl) concentration, and hematocrit (HCT). Our multivariable analysis revealed that prolonged EDLOS was still significantly associated with survival at discharge after controlling for the above covariates. In this model, predictors, including age, intubation, and reintubation, were significantly associated with a poor outcome (Table 1). The GCS score and Cl concentration were independent predictors associated with better outcome.
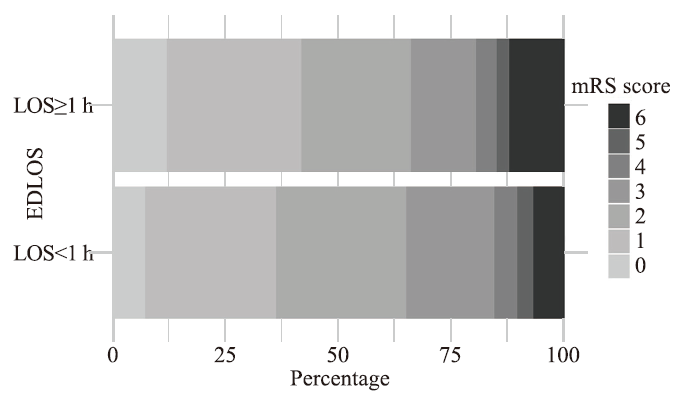
As shown in Figure 1, EDLOS ≥1 h predicted higher discharge mRS, which was driven primarily by the increased proportion of mortality (mRS=6) and a decreased proportion of moderate disability (mRS=3). Notably, the number of patients with no symptoms (mRS=0) in the EDLOS ≥1 h group was outnumbered that in the EDLOS <1 h group.
Figure 1.
Figure 1.
The distribution of the mRS score on hospital discharge stratified by a quartile of emergency department length of stay. EDLOS: emergency department length of stay; mRS: modified Rankin scale.
DISCUSSION
In our study, EDLOS was strongly associated with both discharge mortality and three-month mortality: patients with EDLOS >1 h were more likely to have a poor prognosis. We identified some covariates that were associated with both discharge and three-month outcome, including age, GCS score, and intubation.
The prognostic value of EDLOS was in dispute in previous studies and different conditions. Rincon et al[6]demonstrated that critically ill stroke patients with EDLOS >5 h before transfer to the neuro-ICU were prone to poor hospital discharge outcomes. However, Agustin et al[11] showed an insignificant impact of EDLOS on in-hospital mortality and the number of patients achieving optimal resuscitation within 12 h in septic patients. For spontaneous ICH patients, a study by Elmer et al[9]found no effect of EDLOS on the neurologic outcome or resource utilization after controlling for disease severity, while another group by Jones et al[5] proved to have worsened outcomes after prolonged EDLOS. The possible reason for these discrepancies could be the different nature of disease, hospital conditions, population, and sample size. Our study gained similar results to Jones et al;[5] nonetheless, the cut-off points and length of EDLOS had significant deviations. In their results, the increased EDLOS (> 5 h) means an almost 4-fold increased odds of worse functional outcomes. Prolonged ED visits have been variously defined as >4 h in the United Kingdom, >6 h in Canada/US, and > 8 h in Australia.[11] The present study showed that patients with EDLOS >1 h were more likely to have a poor prognosis. The potential reason could be deficits in advanced neurological intensive care in the ED compared to the ICU or stroke unit ward during the early hours after onset.[5] However, high-quality studies focusing on the actual dangerous EDLOS length and the extent of EDLOS's influence on the prognosis are still needed to provide further evidence on this issue.
This study was limited by its retrospective nature, and therefore we could not identify the primary cause of the delay in EDLOS, which could also be important factors affecting the patients' outcome. Second, the enrollment of patients in a single hospital setting prevented the generalization of the results to other health centers. Besides, we failed to analyze time from onset to ED arrival, which has been demonstrated to be predictive of higher mortality and worse neurologic outcomes.[12] Additionally, as mentioned before, some potential associations or interactions among other variables could not be analyzed.
CONCLUSION
In summary, the present study proves that a prolonged EDLOS may be correlated with mortality and a worse outcome in spontaneous ICH patients.
Funding: This work was supported by a grant from Sichuan Science and Technology Program, China (2019YFS0251).
Ethical approval: The Institutional Review Board of West China Hospital approved the current study.
Conflicts of interests: There are no competing interests involving this work.
Contributors: QH and RG contributed equally to this study and are co-first authors. All authors approved the final version.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Global and regional burden of first-ever ischemic and hemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010
Prognostic value of intracranial pressure monitoring for the management of hypertensive intracerebral hemorrhage following minimally invasive surgery
DOI:10.5847/wjem.j.1920-8642.2020.03.007 URL [Cited within: 2]
Intracerebral haemorrhage: current approaches to acute management
DOI:S0140-6736(18)31878-6
PMID:30319113
[Cited within: 1]

Acute spontaneous intracerebral haemorrhage is a life-threatening illness of global importance, with a poor prognosis and few proven treatments. As a heterogeneous disease, certain clinical and imaging features help identify the cause, prognosis, and how to manage the disease. Survival and recovery from intracerebral haemorrhage are related to the site, mass effect, and intracranial pressure from the underlying haematoma, and by subsequent cerebral oedema from perihaematomal neurotoxicity or inflammation and complications from prolonged neurological dysfunction. A moderate level of evidence supports there being beneficial effects of active management goals with avoidance of early palliative care orders, well-coordinated specialist stroke unit care, targeted neurointensive and surgical interventions, early control of elevated blood pressure, and rapid reversal of abnormal coagulation.Copyright © 2018 Elsevier Ltd. All rights reserved.
Update on the treatment of spontaneous intraparenchymal hemorrhage: medical and interventional management
DOI:10.1007/s11940-018-0486-5 URL [Cited within: 1]
Prolonged emergency department length of stay as a predictor of adverse outcomes in patients with intracranial hemorrhage
Impact of delayed transfer of critically ill stroke patients from the emergency department to the neuro-ICU
DOI:10.1007/s12028-010-9347-0
PMID:20428969
[Cited within: 2]

We sought to determine the effect of emergency department length of stay (ED-LOS) on outcomes in stroke patients admitted to the Neurological Intensive Care Unit (NICU).We collected data on all patients who presented to the ED at a single center from 1st February 2005 to 31st May 2007 with acute ischemic stroke (AIS), intracerebral hemorrhage (ICH), or transient ischemic attack (TIA) within 12 h of symptom onset. Data collected included demographics, admission/discharge National Institutes of Health Stroke Scale (NIHSS), discharge modified Rankin Score (mRS), and total ED length of stay. The effect of ED-LOS on discharge mRS, discharge NIHSS, and hospital LOS was assessed by logistic regression. Poor outcome was defined as mRS > or =4 at discharge.Of 519 patients presenting to the ED, 75 (15%) were critically ill and admitted to the NICU (mean age 65 +/- 14 years, 31% men, and 37% Hispanic). Admission diagnosis included AIS (49%), ICH (47%), TIA (1%), and others (3%). Median ED-LOS was 5 h (IQR 3-8 h) and median hospital LOS was 7 days (IQR 3-15 days). In multivariate analysis, predictors of poor outcome included admission ICH (OR, 2.1; 95% CI, 1.1-4.3), NIHSS > or =6 (OR, 6.4; 95% CI, 2.3-17.9), and ED-LOS > or =5 h (OR, 3.8; 95% CI, 1.6-8.8). There was no association between ED-LOS and discharge NIHSS among survivors or total hospital LOS.Among critically ill stroke patients, ED-LOS > or =5 h before transfer to the NICU is independently associated with poor outcome at hospital discharge.
Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit
Trends and challenges of emergency and acute care in Chinese mainland: 2005-2017
DOI:10.5847/wjem.j.1920-8642.2021.01.001 URL [Cited within: 1]
Prolonged emergency department length of stay is not associated with worse outcomes in patients with intracerebral hemorrhage
DOI:10.1007/s12028-011-9629-1 URL [Cited within: 2]
The critical care management of spontaneous intracranial hemorrhage: a contemporary review
DOI:10.1186/s13054-016-1432-0 URL [Cited within: 1]
Impact of delayed admission to the intensive care unit from the emergency department upon sepsis outcomes and sepsis protocol compliance
Emergency department neurologic deterioration in patients with spontaneous intracerebral hemorrhage: incidence, predictors, and prognostic significance
DOI:10.1111/j.1553-2712.2011.01285.x URL [Cited within: 1]