INTRODUCTION
Precise estimation of blood loss has a direct impact on the extent of volume and coagulation therapy as both, and volume overload and delayed volume therapy may be harmful to patients. Appropriate and timely treatment is particularly important when children, very old or sick patients, and obstetric patients are involved.[1,2,3,4] However, visual estimation of external blood loss in pre- and in-hospital emergencies based on the assessment of blood puddle areas is difficult and frequently inaccurate independent of experience and qualification of professionals.[3,4,5] Overestimation of blood loss at low volumes and underestimation of blood loss at high volumes are commonly observed.[6] Quantification of external blood loss may be further hampered by spreading blood on surfaces with various degrees of absorptivity.[6] Dynamics of vital signs and clinical parameters further influence visual estimation and alter quantification of blood loss.[7] Using pictorial nomograms,[5] pictorial guidelines,[8] drapes[4] or one's fist to determine external blood loss[9] was reported to improve the accuracy of visual estimation.
The objective of this trial is to assess the significance of blood volume quantification after training with a visual estimation tool.
METHODS
A prospective, paired-control, single-blinded experimental study was conducted at the training center of the Medical University of Innsbruck. Anonymized participation of attendees was facilitated by encoding test results. Using convenience sampling technique participation was voluntary and based on the understanding that the results will be published in scientific journals. The experimental study corresponds to the STARD 2015 guidelines for reporting diagnostic accuracy studies.[10]
Study population
Eligible participants from the Department of Anesthesiology and Intensive Care Medicine, Innsbruck Medical University Hospital and from Innsbruck Emergency Medical Service (EMS), Red Cross Tyrol were contacted.
Inclusion criteria were: specialists and specialist trainees in anesthesiology, emergency physicians, emergency technicians, emergency assistants, voluntary participation, and written informed consent.
Exclusion criteria were: incomplete participation during the study phase, and lack of written informed consent.
Study design
On day 1, participants were asked to estimate the volume of blood puddles spread on four different surfaces in the examination room. The investigation was conducted without any previous supply of information to the attendees (pre-training). Then, participants were taught how to estimate the area of spread blood when using the visual estimation tool (training).
On day 2 and day 14 after the initial assessment and training, participants again had to estimate four randomly assigned blood volumes on identical surfaces. In order to assess the training effect, attendees were not allowed to use the visual estimation tool (post-training).
Experimental setting
Human packed red cell concentrates, anticoagulated with citrate phosphate glucose and hematocrit ranging between 33.0% and 42.0%, were poured slowly from 5 cm distance on the test surface. Four different test materials were used: carpet (loop fitted, 8 mm height, 100% polyamide), cotton towel, polyvinyl chloride (PVC) flooring, and wooden flooring (raw spruce board for timber piling). The investigation was performed indoors under dry conditions at room temperature with no wind or air conditioning to counteract the speed of evaporation. Materials were horizontally positioned. Surfaces were brightly colored, without pattern, with no grooves or gaps.
Visual estimation tool and questionnaire
In the current study, training was performed with a self-designed visual estimation tool in the shape of a DIN A4 sheet of paper (Figure 1). The tool can be folded either along the continuous line to provide one and two-thirds of the reference surface or along the dotted line to provide half of the reference surface for comparison of blood puddle sizes. For estimation of circular type blood puddles, the formula for calculation of the area of a circle was provided.
Figure 1.
Figure 1.
The visual estimation tool modified by converting areas of blood puddles to proportions of the standardized sheet of DIN A4.
For measurement of blood puddle diameters, two tape lines in cm units were perpendicularly arranged on the margins of the tool. Specific information with respect to absorbing properties of four common materials (carpet, towel, wood, PVC) at four common volumes was provided in the center of the tool. The reference surfaces were expressed as proportions of the surface area of a sheet of paper (standard DIN A4: 210 mm×297 mm=623.7 cm²). Areas indicated in this tool were based on results of a previous study,[11] in which the spread of pre-defined blood volumes on the surface of different everyday objects was analyzed.
The questionnaire contained three questions regarding certainty, experience, and need for training in the estimation of external blood loss, and five questions regarding the content, comprehensibility efficiency, complexity, and importance of the training program (each item provided a Likert-type scale with five response levels).
Study endpoints and null hypothesis
The primary study endpoint was to assess the pre- and post-training differences in percent error of estimated blood volume (accurate visual estimation of blood volume) when using the visual estimation tool. The secondary study endpoint was to compare the frequency of accurate visual estimation and various characters including age, profession, gender, and years of professional experience. The null hypothesis of the study was that the detection rate (significance) of actual blood volumes dispersed on different subsoils in an experimental setting does not differ between pre- and post-training.
Statistical analysis
The percent error of estimated blood volume was calculated as ([estimated blood volume-actual blood volume]/actual blood volume×100). Accurate estimation was defined as assessment within a deviation of 20% of actual blood volume. Consequently, overestimation and underestimation were defined as >+20% and <-20% of actual blood volume, respectively. Clinical experience was categorized as 0-5 years, >5-10 years, >10-15 years, or >15 years after graduation from a medical or professional school.
Data were entered into a Microsoft Excel spreadsheet Version 7.0.25 (Microsoft Corporation, Redmond, Washington, USA). Data were not normally distributed as assessed by Shapiro-Wilk test; results were expressed as median and range. The Wilcoxon signed-rank test was used to compare pre- and post-training results. To compare two independent groups, the Mann-Whitney U-test or the Kruskal-Wallis test was used if more than two groups were analyzed. For frequency analysis, Fisher's exact or the Chi-square test was performed, and correlations were calculated with Spearman's Rho. The tendency to overestimate or underestimate a series of blood volumes was assessed with the Jonckheere-Terpstra test. The significance level was defined as P<0.05.
RESULTS
Overall, 57 persons responded and participated in the pre-training assessment, but 13 persons did not attend the post-training assessment (inclusion rate 77.2%). Of 44 participants enrolled in the study, 18 (40.9%) were female, 34 (77.3%) were physicians, and 10 (22.7%) were EMS personnel. The median age was 32 years (range 18-56 years), and the median professional experience was six years (range 1-25 years).
Pre-training assessment
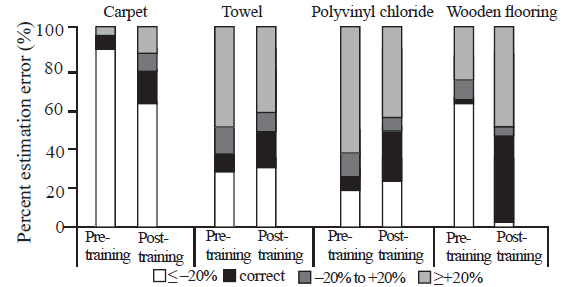
On PVC flooring, 28 (63.6%) estimations were exceeding 20% deviation, whereas on wood 27 (61.4%) estimations were below -20% deviation of actual blood volume. On carpet, 39 (88.7%) estimations were below -20% deviation, and on towel 22 (50.0%) estimations were exceeding 20% deviation of actual blood volume (Table 1, Figure 2). There was no association between the estimation results or estimation errors and age, profession, gender, and years of professional experience.
Table 1 Median estimation and percent error of estimated blood volume from actual blood quantities
| Variables | Pre-training | Variables | Post -training | P-value | ||
|---|---|---|---|---|---|---|
| Estimated blood volume, median (range), mL | Percent error of estimated blood volume, median (range), % | Estimated blood volume, median (range), mL | Percent error of estimated blood volume, median (range), % | |||
| Carpet 1,000 mL | 300 (40-1,600) | -70 (-96 to +60) | Carpet 1,500 mL | 1,050 (250-3,500) | -30 (-83 to +133) | <0.001 |
| Towel 500 mL | 800 (50-2,000) | +60 (-90 to +300) | Towel 1,000 mL | 1,000 (500-2,500) | 0 (-50 to +150) | 0.026 |
| PVC 100 mL | 175 (30-700) | +75 (-70 to +600) | PVC 250 mL | 250 (100-600) | 0 (-60 to +140) | <0.001 |
| Wood 250 mL | 140 (20-1,500) | -44 (-92 to +500) | Wood 100 mL | 125 (80-300) | +25 (-20 to +200) | 0.041 |
Figure 2.
Figure 2.
Changes in percent estimation error between pre-training and post-training assessments on various surfaces.
Post-training assessment
After being instructed on the application of the visual estimation tool, the percentage of accurate estimations within 20% deviation rose from 26 of 176 estimations to 58 of 176 estimations (P<0.001). The accuracy of estimation significantly improved regarding all four surfaces tested. Overall significance of blood volume quantification after training with the visual estimation tool was 33.0%. There was no association between the estimation results or estimation errors and age, profession, gender, or years of professional experience.
Questionnaire
Twenty-five (56.8%) participants stated that they had little or very little experience in estimating blood loss and 42 (95.5%) quoted the need to be trained in blood loss estimation. Forty-three (97.7%) participants reported a good to very positive training effect and considered the training content to be comprehensible to very comprehensible. Twenty-three (52.4%) participants reported that they had learned much or very much, and 27 (61.4%) participants ranked the level of difficulty of the training program between low and mean. In sum, 36 (83.7%) participants graded the training program very good or good.
DISCUSSION
The results of our experimental study underline that training with a tool for visual estimation has a lasting effect and may improve the estimation accuracy of blood volumes spread on surfaces with varying absorptivity. Such training has education value for prehospital providers. As emergency cases with blood scattered on various surfaces are rare, even the very experienced emergency physicians and technicians have difficulties in the quantification of external blood losses.[1,2,3,4] Estimated volumes differed considerably regardless of age, profession, gender, or years of professional experience during the pre-training assessment. Overestimations of up to about 11 folds (1,500 mL vs. 140 mL) on wood and underestimations of up to 16 folds (50 mL vs. 800 mL) on the towel were observed (Table 1). Interestingly, there were 63.6% overestimations regarding blood on PVC flooring but 61.4% underestimations regarding blood on wood although both materials have minimally absorbent surfaces. Similar, there were 50.0% overestimations regarding blood on the towel but 88.7% underestimations regarding blood on carpet although both materials are highly absorbent. However, it is still a question of debate whether the accuracy of measuring blood loss has direct effects on outcomes.[12]
Majority of participants quoted that the comprehensible training increased their subjective certainty concerning how to estimate external blood loss. There was an impressive training effect in this and in similar studies.[13,14,15] Pre-hospital assessment of blood loss relies on visual estimation and clinical parameters such as heart rate, blood pressure, capillary refill time, characteristics of the pulse wave in oxygraphy, turgor, and venous filling status. This differs substantially from the in-hospital assessment of blood loss focusing on laboratory results such as hemoglobin, hematocrit, clotting factor concentrations, and coagulation intervals. The results of our study corresponded with the improved estimation of external blood loss when training was performed with a nomogram, as reported recently.[5]
Presumably, the estimation may be even more precise using a cell-phone-based software for planimetry of blood puddles in dependency of surface properties corrected with a specific coefficient. When considering age and weight of the patient, the amount of blood loss can even be assessed as percentage of circulating blood.
The limitations of this study are numerous. The study population was small although the results were within the range of similar studies.[5,12,13,16] Selection bias cannot be excluded as the majority of participants quoted the need to be trained in blood loss estimation. Factors that may influence blood puddle sizes were blood viscosity, coagulation, air humidity, temperature, and evaporation. In addition, surface characteristics may vary substantially, e.g., the thickness and absorbability of carpets, unevenness, and dimples may change area and expansiveness of blood puddles.[5] Accuracy of visual blood volume estimation may be further influenced by optical illusion arising from the color or pattern of surfaces.
The quantity of scattered blood on various surfaces is still difficult to estimate, but training with the visual estimation tool might help to consider the varying degrees of absorption into the overall assessment.
CONCLUSIONS
Training with a visual estimation tool by professional rescuers can improve the estimation accuracy of blood volumes spread on surfaces with varying absorptivity.
ACKNOWLEDGMENTS
The authors thank all participants for their attendance and for having contributed valuable feedback.
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board and the Ethics Committee of the Medical University of Innsbruck and complied with the Declaration of Helsinki.
Conflicts of interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors: JK wrote the main body of the report. All authors approved the final version.
Reference
The accuracy of external blood loss estimation by ambulance and hospital personnel
DOI:10.1046/j.1442-2026.2003.00469.x URL [Cited within: 2]
Estimation of external blood loss by paramedics: is there any point?
PMID:18709938
[Cited within: 2]

There are many patient assessment challenges in the prehospital setting, especially the estimation of external blood loss. Previous studies of experienced paramedics have demonstrated that external blood loss estimation is highly inaccurate. The objective of this study was to determine if undergraduate paramedic students could accurately estimate external blood loss on four surfaces commonly found in the prehospital environment.This prospective, observational, blinded study used a convenience sample of undergraduate students studying at Monash University during 2006. Students were provided with four clinical vignettes using four different surfaces and varying simulated blood amounts.Accurate estimation occurred with the vinyl simulation (100 ml), with a mean value of the estimations of 98 ml (95% Confidence Interval (CI) 84-113 ml). Carpet and concrete surfaces were both associated with large under-estimations. The carpet simulation (1,000 ml) had a mean value for the estimations of 347 ml (95% CI 320-429 ml). The concrete simulation (1,500 ml) had a mean value for the estimations of 885ml (95% CI 771-999 ml). Conversely, the clothing simulation (500 ml) emphasized over-estimation, with a mean value for the estimations of 1,253 ml (95% CI 1,093-1,414 ml). There was no relationship between increased accuracy and clinical experience, exposure, educational qualifications, or age of students.External blood loss estimation by undergraduate paramedic students generally is too inaccurate to be of any clinical benefit. Particularly, absorbent and impermeable surfaces precipitated inaccuracies by undergraduate paramedic students.
Improved accuracy of postpartum blood loss estimation as assessed by simulation
DOI:10.1080/00016340802317794
PMID:18720041
[Cited within: 3]

Caregivers underestimate the amount of blood loss, but this almost five decades-old assumption has not been validated. We aimed at assessing the accuracy of estimated blood loss by obstetrical teams during a simulated Postpartum hemorrhage (PPH) scenario.a prospective study conducted as part of the simulation-based training course, using sophisticated mannequin simulators adapted for obstetrical training by specially designed devices.Part of the simulation-based training course.Obstetrical teams consisted of physicians and obstetrical nurses.Each of the participating obstetrical teams assessed blood loss during PPH scenarios. Their estimates were compared to the actual predefined 3.5-liter blood loss. An intervention group underwent a similar course in which they recorded their estimations after 1, 2 and 3.5 liters were lost.Blood loss estimates after completion of the scenario in both groups.Fifty obstetrical teams took part in the study. Eight comprised the interventional group. The average estimated blood loss was 1,780 ml (49% underestimation) for non-interventional teams. The interventional groups estimated blood loss to be 2,400 ml (32% underestimation). The main method of estimating blood loss was 'gut feeling', followed by verbalized guesses of team members and assessments of the 'patient's' hemodynamic status.Accuracy of blood loss estimations by a simulation-based PPH scenario was 50-60%. Measurements at predetermined intervals significantly improved accuracy of these estimations. Our study suggests that implementation of periodic estimations of blood loss in the management of PPH might improve clinical judgment.
Postpartum blood loss: visual estimation versus objective quantification with a novel birthing drape
DOI:10.11622/smedj.2016107 URL [Cited within: 4]
Improvement of blood loss volume estimation by paramedics using a pictorial nomogram: a developmental study
DOI:S0020-1383(17)30751-9
PMID:29108791
[Cited within: 5]

To propose and evaluate a nomogram to assist paramedics to visually estimate the external blood loss on a non-absorbent surface and to identify whether the nomogram improves visual estimation.The study was a prospective, paired-control design (pre-training control group & post-training group), utilizing Emergency Medical Assistant (EMA) I and II trainees from the Hong Kong Fire Services Ambulance Command Training School. A nomogram (blood loss volume to area on a non-absorbent surface) was prepared to aid blood loss estimation. All participants estimated four scenarios of blood pools twice (A: 180mL; B: 470mL;C: 940mL; D: 1550mL) before and after using the nomogram. Every participant received two-minute training on how to use the nomogram correctly. The difference between the estimations and the actual volume in each scenario was calculated. The absolute percentage errors were used for direct comparison and identification of improvement between visual estimation and the use of the nomogram.Sixty-one participants with an average of 3-year paramedic field experience were recruited by convenience sampling. In combining all scenarios, the median of absolute percentage error of 61 participants was 43% (95%CI 38.0-50.9%) in visual estimation, while it was 23% (95%CI 17.4-27.0%) when using the nomogram. There was a significant reduction in absolute percentage error between visual estimation and the use of the nomogram (p<0.0001).The nomogram significantly improved the estimation of external blood loss volume.Copyright © 2017 Elsevier Ltd. All rights reserved.
Clinical image: visual estimation of blood loss
Proper estimation of blood loss on scene of trauma: tool or tale?
Improving the accuracy of estimated blood loss at obstetric haemorrhage using clinical reconstructions
DOI:10.1111/bjo.2006.113.issue-8 URL [Cited within: 1]
External blood loss estimation using the MAR method
DOI:10.1016/j.ajem.2008.07.039
PMID:19931755
[Cited within: 1]

An element lacking in medical education is training to estimate blood volumes. Therefore, health care workers currently use visual estimation as their only means of determining blood volumes, which has shown to be highly inaccurate. This study proposes and tests a new method using one's fist to determine external blood loss.Increments of human whole blood were measured and used to compare fist size to surface area of blood present. A formula was created averaging blood per fist, hereafter known as the MAR Method. Two scenarios were staged using set quantities of blood (75 and 750 mL). Participants estimated blood volumes before and after being taught the MAR Method in a 1-minute session. Errors in estimation before and after using the MAR Method were compared.The MAR Method was created using a fist to cover a surface area of blood that equals 20 mL. A total of 74 participants had errors of 120% and 73% for visualization of the small and large pools, respectively. For the smaller volume, the average error from the mean decreased by 76% (P < .0001), and the interquartile range of errors decreased by 60%. For the larger volume, the average error from the mean reduced by 40% (P < .0001), and the interquartile range of errors reduced by 45%.Use of the MAR Method improves blood volume estimations. After less than 1 minute of instruction, participants were able to determine blood volumes with improved accuracy and precision.
STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration
DOI:10.1136/bmjopen-2016-012799 URL [Cited within: 1]
Variation in size of blood puddles on different surfaces
DOI:10.1097/MEJ.0000000000000092
PMID:24217851
[Cited within: 1]

It is known that visual estimation of blood loss is inaccurate independently from experience and qualification of rescuers or members of hospital staff. There is no information available about the size of a puddle of blood for a given amount of blood depending on the surface. This pilot study evaluated the size of blood puddles on various surfaces.Human blood was portioned in standardized amounts of fluid and poured on different surfaces: wooden and polyvinyl chloride (PVC) floors, flagging, carpet, asphalt, concrete, forest soil, mattress and towel. The resulting puddles of blood were documented by digital photos and their surface areas measured using a computer.The largest blood puddles were found on even surfaces such as PVC floors and concrete, and the smallest blood puddles were found on forest soil and carpet. When blood volume was 100 ml, the difference between the smallest and the largest blood puddle added up to a factor of 13.8 (77 cm forest soil, 1061 cm PVC). This factor was comparable in all other blood amounts on these two surfaces (13.7 with 250 ml, 13.0 with 500 ml, 13.5 with 1000 ml). A table with objects of daily life of comparable size (CD, letter, newspaper, etc.) was added for teaching purposes.The size of puddles of blood depended strongly on the type of surface. Up to 13 times larger blood puddles were found on hard and nonabsorbant surfaces (PVC, concrete) than on absorbant surfaces such as carpet or forest soil.
Observer accuracy and reproducibility of visual estimation of blood loss in obstetrics: how accurate and consistent are health-care professionals?
DOI:10.1007/s00404-009-1099-8 URL [Cited within: 2]
Estimating blood loss: can teaching significantly improve visual estimation?
PMID:15339775
[Cited within: 2]

Visually estimated blood loss has long been known to be imprecise, inaccurate, and often underestimated, which may lead to delayed diagnosis and treatment. Our purpose is to determine whether a brief didactic course can improve visually estimated blood loss and whether prior clinical experience influences estimation of blood loss.Reconstituted whole blood was obtained from the blood bank, and simulated scenarios with known measured blood loss were created using common surgical materials. Visually estimated blood loss was performed by medical personnel before and after a 20-minute didactic session. Percent errors of estimated blood loss were calculated and comparisons were made before and after the lecture. The effects of actual blood volume and clinical experience on estimation of blood loss were assessed.A total of 53 participants assessed 7 scenarios. There were significant reductions in error for all scenarios. Median percent error in estimated blood loss was not influenced by clinical experience, either before or after the didactic session. Blood loss tends to be overestimated at low volumes and underestimated at high volumes.Error in estimating blood loss is dependent on actual blood loss volume. Medical students and experienced faculty demonstrate similar errors, and both can be improved significantly with limited instruction. This educational process may assist clinicians in everyday practice to more accurately estimate blood loss and recognize patients at risk for hemorrhage-related complications.
Effect of on-site training on the accuracy of blood loss estimation in a simulated obstetrics environment
DOI:10.1002/ijgo.2017.137.issue-3 URL [Cited within: 1]
Increase accuracy of visual estimation of blood loss from education programme
Blood loss estimation in epistaxis scenarios
PMID:15807956
[Cited within: 1]

Thirty-two members of staff from the Ear, Nose and Throat Department at Warrington General Hospital were asked to estimate blood loss in commonly encountered epistaxis scenarios. Results showed that once the measured volume was above 100 ml, visual estimation became grossly inaccurate. Comparison of medical and non-medical staff showed under-estimation was more marked in the non-medical group. Comparison of doctors versus nurses showed no difference in estimation, and no difference was found between grades of staff.