INTRODUCTION
Pericardiocentesis is a life-saving emergent procedure. Though performed rarely by emergency physicians, it is a skill they must know how to perform expertly when necessary. It is a critical skill taught and learned in all emergency medicine residency programs. Pericardial effusions can develop from medical causes (post-viral, related to cancer, infection, or post-surgical) or from traumatic injury to the heart. When a pericardial effusion impairs the filling of the heart, termed pericardial tamponade, hemodynamic instability ensues. This is an immediately life-threatening condition that must be treated with pericardiocentesis. Ideally performed in a controlled, surgical setting by an interventional cardiologist, this procedure is performed in the emergency department when the patient is rapidly decompensating and other resources are not available.
Traditionally performed using anatomical landmarks via a subxiphoid approach, the increasing and nearly ubiquitous use of point-of-care cardiac ultrasonography by emergency physicians has made ultrasound-guided pericardiocentesis in the emergency department a possibility. This procedure is best performed under ultrasound guidance, as the complication rate is much lower (0.5%-3.7%)[1,2,3,4] when compared to blind or electrocardiography-assisted pericardiocentesis (15%-20%).[5,6] Potential complications include right ventricular puncture, pneumothorax, gastric puncture, hepatic puncture, life-threatening hemorrhage, and resulting infection.
When using ultrasound guidance, the approach where the largest fluid collection visualized on ultrasound can be accessed closest to the skin surface is recommended. Ultrasound allows for a physician to utilize entry sites other than the subxiphoid area, such as a parasternal approach or an apical approach. To our knowledge, there is no clear consensus in the literature which approach is ideal. The expert- and consensus-based recommendations for needle placement and entry sites for pericardiocentesis vary. The Advanced Cardiac Life Support (ACLS) manual recommends a parasternal approach as the safest.[7] This approach is just lateral to the sternum on the anterior chest. The American College of Surgeons Advanced Trauma Life Support (ATLS) manual recommends a subxiphoid approach.[8] The most authoritative text on emergency medicine procedures recommends using the approach with which the clinician is most familiar, stating that the subxiphoid approach is the most common.[9] Tintinalli's Emergency Medicine: A Comprehensive Study Guide recommends a subxiphoid approach if the procedure must be performed blind.[10] A Mayo clinic study characterized all of the pericardiocenteses performed at their institution over a 21-year period; 1,127 pericardiocenteses were performed by cardiologists and of these, 208 were performed via subcostal or subxiphoid approach (18% of all total procedures) and 83 were performed parasternally (7% of all total procedures). The largest proportion from this study was performed from an apical position (n=714, 63%).[11] The apical position is not described or recommended in any of the emergency medicine literature, ACLS, or ATLS recommendations. In another study which retrospectively reviewed pericardiocentesis performed in the intensive care unit for patients with tamponade physiology, the subxiphoid approach was used 99% of the time (109 of 110 pericardiocentesis performed).[12] We have been unable to find any studies characterizing which approach is most frequently used in practice for emergency department pericardiocentesis, likely because this is such a rare emergency department procedure. Given the conflicting recommendations, our goal was to investigate the ideal entry site for point-of-care ultrasound-guided pericardiocentesis in the emergency department. The aim of this study is to identify the ideal approach for emergency-physician-performed ultrasound-guided pericardiocentesis as determined by ultrasound image quality, distance from surface to pericardial fluid, and likely obstructions or complications.
METHODS
Study design and study setting
This was a retrospective review of point-of-care cardiac ultrasound examinations performed in two urban academic emergency departments with a combined annual census of 120,000. Both emergency departments have an Accreditation Council for Graduate Medical Education (ACGME)-accredited emergency medicine residency and an active point-of-care ultrasound training program. The emergency medicine residents receive point-of-care ultrasound training and milestone assessment according to ACGME guidelines. Hospital-based credentialing in point-of-care ultrasound is available per American College of Emergency Physicians (ACEP) guidelines,[13] and quality assurance is performed for all examinations by emergency ultrasound fellowship-trained physicians. All point-of-care ultrasound examinations are archived in the web-based workflow solution database, Q-path (Telexy Healthcare, Port Coquitlam, Canada), which stores images and interpretation reports. An Institutional Review Board (IRB) approval was obtained for this study.
Study protocol
Eligible point-of-care cardiac ultrasound examinations were identified through search of the emergency department ultrasound image archival system (Q-path, Telexy Healthcare, Port Coquitlam, Canada) during the study period. Emergency medicine residents and attending physicians with varied point-of-care ultrasound experience performed cardiac ultrasound examinations as part of routine patient evaluation after initial clinical assessment. The examinations were performed with a Z.One Ultra (Zonare Medical Systems, Mountain View, CA, USA) or a SonixTouch (Ultrasonix Medical Corporation, Richmond, British Columbia, Canada) system with a low-frequency broadband phased array transducer. Emergency physicians with varying ultrasound examination skills performed the studies, ranging from first-year residents to attending physicians.
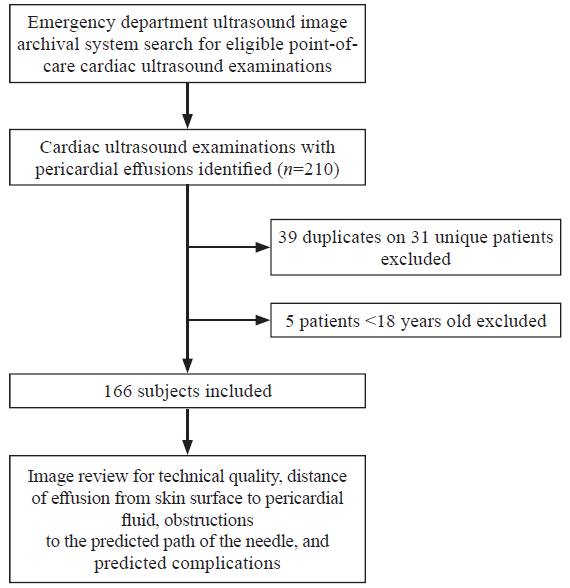
All point-of-care ultrasound studies performed in the emergency departments over the study period were reviewed for the presence of cardiac images. Patients were included in the study if they received a point-of-care cardiac ultrasound examination, were over 18 years old, or were found to have a pericardial effusion (Figure 1). All images were reviewed by an emergency ultrasound fellowship-trained physician for technical quality, distance of effusion from skin surface to pericardial fluid, obstructions to the predicted path of the needle, and predicted complications. The technical quality of the images was rated on a grading scale from 1-5 using the proposed ACEP suggested quality assurance grading scale.[14] The distance from skin surface to pericardial fluid was measured from saved images using manual measurements and the recorded sonographic scale. The size of the pericardial effusion was recorded and definitions were standardized based on the criteria proposed by Armstrong.[15] Obstructions to the predicted path of the needle or predicted complications were recorded. These included obstruction by another organ such as the lung, stomach, or liver, poor image quality or prohibitive depth. The investigators used their professional judgement as to whether obstructions, prohibitive depth, or predicted complications existed.
Figure 1.
Figure 1.
Flow chart.
Outcome measures
The primary outcomes were predicted complication rates for pericardiocentesis for different cardiac views and the mean skin-to-pericardial fluid distance. The secondary outcomes included image quality ratings for different cardiac views.
Data analysis
Descriptive statistics are presented along with 95% confidence intervals (95% CI). Proportions were compared using Fisher's exact test, means were compared using the Student's t-test, and medians were compared using the Mann-Whitney U-test. All analyses were conducted in STATA 15 (College Station, Texas).
RESULTS
A total of 166 pericardial effusions were identified. Subxiphoid, parasternal, and apical views were each obtained for 84.3% (95% CI 77.9%-89.5%), 73.5% (95% CI 66.1%-80.0%), and 60.2% (95% CI 52.4%-67.7%) of examinations, respectively. The presence of a pericardial fluid collection was visualized in each view as follows: 88.6% (95% CI 82.1%-93.3%) of subxiphoid views, 81.1% (95% CI 73.0%-87.7%) of parasternal views, and 72.0% (95% CI 62.1%-80.5%) of apical views (P=0.005). Image quality ratings were similar for the three views, with a median and interquartile range (IQR) rating of 3 (3-4) for the subxiphoid views, 4 (3-5) for the parasternal views, and 4 (3-4) for the apical views. The mean skin-to-pericardial fluid distance was significantly greater for the subxiphoid views compared to both the parasternal and apical views (Table 1). Each view was evaluated for the potential complications. The subxiphoid view had the highest predicted complication rate at 79.7% (95% CI 71.5%-86.4%) and was significantly greater than the apical (31.9%; 95% CI 21.4%-44.0%, P<0.001) and parasternal (20.2%; 95% CI 12.8%-29.5%, P<0.001) views. The most frequently predicted complication for the three views was the liver puncture in the subxiphoid views (83.7%; 95% CI 74.8%-90.4%), poor image quality precluding safe procedure in the parasternal view (30.0%; 95% CI 11.9%-54.3%), and inability to access the fluid collection in the apical view (26%; 95% CI 10.2%-48.4%). The specific frequencies of predicted complications for the subxiphoid view are summarized in Table 2.
Table 1 Mean skin-to-pericardial fluid distance for each of the echocardiographic views
| Echocardiographic view | Mean skin-to-pericardial fluid distance, cm |
|---|---|
| Subxiphoid | 5.6 (95% CI 5.2-6.0) |
| Parasternal | 2.7 (95% CI 2.5-2.8) |
| Apical | 2.5 (95% CI 2.3-2.7) |
Table 2 Frequency of specific predicted complications for the subxiphoid view
| Predicted complication | Frequency | Percent |
|---|---|---|
| Liver in needle path | 82 | 49% |
| Prohibitive depth | 21 | 13% |
| Poor image quality | 20 | 12% |
| Movement (cardiac or respiratory) | 7 | 4% |
| Other | 8 | 5% |
DISCUSSION
Our study is relevant in a variety of settings where pericardiocentesis is performed, such as in the emergency department, intensive care unit, and other acute care environments. Pericardial effusions are increasingly detected on point-of-care cardiac ultrasounds, and they can be caused by trauma, malignancy, autoimmune disease, renal disease, and infection, or be idiopathic. Emergent pericardiocentesis is often indicated in the setting of cardiac arrest and in patients with hemodynamic compromise. Because it is a procedure that is uncommonly performed, operator confidence when performing this procedure based on landmarks only may be limited. The success of a pericardiocentesis is dependent on the size of the effusion and distance from the skin to pericardial fluid. It is recommended to choose the needle insertion site based on the location at which the effusion lies closest to the skin to avoid vital structures. Point-of-care ultrasound allows the operator to visualize the real-time needle throughout the entire procedure. In general, continuous observation of the advancing needle tip is challenging in the subxiphoid compared to the parasternal approach. The apical technique may be preferred over the subxiphoid but still proves much more difficult than utilizing the parasternal window in many patients.
Our study results show that the approach with the highest complication rate is the subxiphoid approach. This result is not unexpected given that the needle may traverse vital structures such as the lung, liver, internal thoracic artery, left anterior descending artery, colon, and stomach.[16] This is also the longest distance from skin to pericardial space. In Petri et al's simulated study of 150 blind pericardiocentesis, the complication rate ranged from 5% to 31% with different puncture techniques and authors recommended to perform pericardiocentesis with image guidance whenever it is possible.[16] Ultrasound-guidance is especially important when the pericardial effusion is posterior in location and the usual approach from the subxiphoid position would not reach the pericardial space.
Osman et al[17] evaluated a novel in-plane parasternal medial-to-lateral approach for pericardiocentesis with a high-frequency probe in patients with cardiac tamponade and reported a 100% success rate without complications. The advantages of this medial-to-lateral approach include better visualization of needle trajectory and adjacent anatomical structures (lungs and thoracic vasculature) with a high-frequency probe which can reduce complications and shorten procedural time. This differs from the traditional technique (subxiphoid and apical) using a low-frequency probe where real-time visualization of the entire needle trajectory might be challenging and can potentially result in puncture of adjacent vital organs. The potential complications include pneumothorax with an apical approach, and increased risk of injury to the liver, heart, and inferior vena cava with subxiphoid approach. Several other observational studies demonstrated that the parasternal approach was superior to the traditional subxiphoid approach.[18,19,20,21] In our study, the parasternal approach had the lowest predicted complication rate with a shorter mean skin-to-pericardial fluid distance compared to the subxiphoid approach. Our study suggests that the parasternal approach is superior to the subxiphoid approach even under ultrasound guidance. We recommend choosing a parasternal approach whenever possible, since it provides the safest, superficial, and direct path to the pericardial space. However, we acknowledge that other factors may determine the site of pericardiocentesis with complete disregard to the ideal site based on imaging. If a patient is in cardiac arrest, this precludes a parasternal approach entirely due to cardiopulmonary resuscitation. In these situations, a subxiphoid approach is wholly preferred. Patients with chronic obstructive pulmonary disease with hyperinflated lungs are unlikely to have preferable parasternal or apical views, and a subxiphoid approach may be preferred in these situations.
Probe choice for emergent pericardiocentesis can differ based on the chosen approach and patient characteristics. A linear array probe may be chosen for effusion that is directly opposed to the chest wall and can be fully imaged within a few centimeters of depth. This may be ideal for a parasternal approach or an apical approach if the effusion is amenable to superficial imaging. A linear array probe allows for improved spatial resolution with fewer artifacts. Additionally, in-plane needle guidance with a linear array probe is a skill that many emergency physicians utilize on a regular basis, making this rare procedure more familiar to other common procedures (i.e., ultrasound-guided regional anesthesia and peripheral and central vascular access). Utilizing the same in-plane needle guidance technique with a phased or a curvilinear array probe does not provide the level of detail with needle guidance and is more prone to confounding artifacts. The limitation of depth with the linear probe precludes its use when the pericardial effusion is deep or if all relevant structures (i.e., the heart) cannot be imaged within the field. In these scenarios, a phased array or curvilinear probe is ideal, despite the anticipated difficulties with needle guidance.
Limitations
Our study has several limitations, including its retrospective study design and also a small number of pericardial effusions, which can limit the conclusions that can be reached. Another major limitation of this study is the selection bias from the convenience sample design, since emergency department patients received point-of-care cardiac ultrasound examination only when credentialed attending physicians were on duty. The image reviewers were not blinded to the study hypothesis. Not all three views (subxiphoid, parasternal, and apical) were obtained in every point-of-care cardiac ultrasound examination. This is likely because the studies were performed by residents and attending physicians with varied ultrasound experience which reflects the real-world clinical setting. We did not review medical records to determine the clinical significance of pericardial effusion and if they underwent pericardiocentesis; therefore, the final outcomes (arrhythmia, cardiac arrest, mortality, etc.) including actual complication rates of pericardiocentesis are unknown.
CONCLUSIONS
Our results suggest that complication rates with pericardiocentesis will be lower via the parasternal or apical approach compared to the subxiphoid approach. The distance from skin to fluid collection is the least in both of these views. However, additional factors may determine the best approach for pericardiocentesis regardless of the ideal site found on ultrasound, and a patient-specific or individualized approach should be considered when using ultrasound guidance.
Funding: None
Ethical approval: An IRB approval was obtained for this study.
Conflicts of interest: Authors have no financial or other conflicts of interest related to this submission.
Contributors: LS proposed and wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts.
Reference
Complications of percutaneous pericardiocentesis under fluoroscopic guidance
PMID:1633040
[Cited within: 1]

Complications in 352 cases of fluoroscopy-guided percutaneous pericardiocentesis accomplished through an indwelling catheter were reviewed following surgery and non-surgery. Thirteen major complications were found, namely 3 cardiac perforations, 2 cardiac arrhythmias, 4 cases of arterial bleeding, 2 cases of pneumothorax in children, one infection, and one major vagal reaction. No significant difference in complications was found between pericardiocenteses for pericardial effusions after cardiac surgery (n = 208) and those for effusions of non-surgical (n = 144) origin. Fluoroscopy-guided pericardiocentesis by the subxiphoid approach with placement of an indwelling catheter is a safe method for achieving pericardial drainage in both surgical and non-surgical effusions. Accidental cardiac perforation with a fine needle is a minor complication as long as the needle is directed towards the anterior diaphragmatic border of the right ventricle and drainage is achieved with a reliable indwelling catheter.
Pericardiocentesis: differential aspects of a common procedure
DOI:10.1007/s001340051206 URL [Cited within: 1]
Clinical and echocardiographic characteristics of significant pericardial effusions following cardiothoracic surgery and outcomes of echo-guided pericardiocentesis for management: Mayo Clinic experience, 1979-1998
PMID:10453858
[Cited within: 1]

This study assessed the clinical features, timing of presentation, and echocardiographic characteristics associated with clinically significant pericardial effusions after cardiothoracic surgery. The outcomes of echocardiographically (echo-) guided pericardiocentesis for the management of these effusions were evaluated.From the prospective Mayo Clinic Registry of Echo-guided Pericardiocentesis (February 1979 to June 1998), 245 procedures performed for clinically significant postoperative effusions were identified. Clinical features, effusion causes, echocardiographic findings, and management outcomes were studied and analyzed. Cross-referencing the registry with the Mayo Clinic surgical database provided an estimate of the incidence of significant postoperative effusions and the number of cases in which primary surgical management was chosen instead of pericardiocentesis.Use of anticoagulant therapy was considered a significant contributing factor in 86% and 65% of early effusions (< or =7 days after surgery) and late effusions (>7 days after surgery), respectively. Postpericardiotomy syndrome was an important factor in the development of late effusions (34%). Common presenting symptoms included malaise (90%), dyspnea (65%), and chest pain (33%). Tachycardia, fever, elevated jugular venous pressure, hypotension, and pulsus paradoxus were found in 53%, 40%, 39%, 27%, and 17% of cases, respectively. Transthoracic echocardiography permitted rapid diagnosis and hemodynamic assessment of all effusions except for three cases that required transesophageal echocardiography for confirmation. Echo-guided pericardiocentesis was successful in 97% of all cases and in 96% of all loculated effusions. Major complications (2%), including chamber lacerations (n = 2) and pneumothoraces (n = 3), were successfully treated by surgical repair and chest tube reexpansion, respectively. Median follow-up duration for the study population was 3.8 years (range, 190 days to 16.4 years). The use of extended catheter drainage was associated with reduction in recurrence for early and late postoperative effusions by 46% and 50%, respectively.The symptoms and physical findings of clinically significant postoperative pericardial effusions are frequently nonspecific and may be inadequate for a decision regarding intervention. Echocardiography can quickly confirm the presence of an effusion, and pericardiocentesis under echocardiographic guidance is safe and effective. The use of a pericardial catheter for extended drainage is associated with lower recurrence rates, and the majority of patients so treated do not require further intervention.
Pericardiocentesis adverse event risk factors: a nationwide population-based cohort study
DOI:10.1159/000368796 URL [Cited within: 1]
The risk of pericardiocentesis
PMID:495505
[Cited within: 1]

The risk and potential risk factors of pericardiocentesis were assessed by a review of a series of 52 pericardiocenteses comprising all those performed in the cardiac catheterization laboratory of one institution from 1971 to 1978. On the basis of the operative results, the patients were separated into two groups for comparison; Group I comprised all patients with a successful uncomplicated (35) pericardiocentesis and Group II all those with a nonproductive (16), nontherapeutic (1) or complicated (8) pericardiocentesis. Complications consisted of one death, one cardiac arrest, one aspiration of a subdiaphragmatic abscess and five ventricular punctures without adverse sequelae. Among the patients who had a nonproductive pericardiocentesis, the condition of 11 had probably been misdiagnosed but at least 4 had a false negative pericardiocentesis. Comparison of the two groups showed no significant difference in the incidence of cardiac tamponade or in the clinical presentation based on historical, physical, electrocardiographic, roentgenographic or echocardiographic findings of pericardial disease. Pericardiocentesis was usually successful when performed for suspected malignant pericardial effusion but often unsuccessful when performed for suspected hemopericardium. Anatomically, all patients in Group II had either minimal or loculated posterior pericardial effusion. It is concluded that pericardiocentesis can be performed at a low risk that can be further minimized by consideration of the disease process and the anatomic location of the pericardial fluid.
The electrocardiogram as a safeguard in pericardiocentesis
Advanced cardiovascular life support: provider manual
ATLS: advanced trauma life support for doctors (8th ed.)
Pericardiocentesis
Thoracic trauma
Consecutive 1127 therapeutic echocardiography-guided pericardiocentesis: clinical profile, practice patterns and outcomes spanning 21 years
DOI:10.1016/S0025-6196(11)62211-8 URL [Cited within: 1]
Subxyphoid pericardiocentesis guided by contrast two-dimensional echocardiography in cardiac tamponade: experience of 110 consecutive patients
PMID:12086218
[Cited within: 1]

We evaluated echo-guided pericardiocentesis with contrast study in cardiac tamponade management.From 1982 to 1998 we performed pericardiocentesis in 110 patients (56 +/- 14 years old). Subxiphoid approach was used in 109. Cardiac tamponade was idiopathic (n = 16), secondary to malignant disease (n = 50) and miscellaneous disorders (n = 44).Pericardial fluid was bloody (n=75), serous (n = 29) or turbid (n = 6). Mean volume of fluid removed was 585 +/- 370 ml. When prolonged drainage (60 +/- 26 h) was used (n = 41), total effusion volume was 850 +/- 340 ml. Eleven deaths were observed during the early period following pericardiocentesis. No relation with procedure was demonstrated by autopsy in 10, and death always occurred in critically-ill patients (five malignant diseases, five cardiac ruptures and one septic shock). Other complications were: right ventricular puncture (n = 11) with deleterious effect in one, vasovagal hypotension (n = 6) and paroxysmal arrhythmia (n = 6). Surgical drainage was mandatory in 19 patients. It had to be done as an emergency (within 6 h), because of failure of the procedure in four patients. In 14 patients without prolonged drainage a delayed surgical evacuation was indicated, because of persistent (n = 3) or recurrent (n = 11) cardiac tamponade. Only one surgical procedure was required after prolonged drainage.Echo-guided pericardiocentesis with contrast study is an effective technique which reduces the risk of cardiac tamponade management. It should be considered in patients with critical haemodynamic condition or advanced malignancy, and in patients with poor short-term prognosis.
Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine
DOI:10.1016/j.annemergmed.2016.08.457 URL [Cited within: 1]
Feigenbaum’s echocardiography (7th ed.)
“Blind” pericardiocentesis: a comparison of different puncture directions
DOI:10.1002/ccd.v92.5 URL [Cited within: 2]
Ultrasound-guided pericardiocentesis: a novel parasternal approach
DOI:10.1097/MEJ.0000000000000471
PMID:28509710
[Cited within: 1]

The aim of this study was to evaluate a novel pericardiocentesis technique using an in-plane parasternal medial-to-lateral approach with the use of a high-frequency probe in patients with cardiac tamponade.Echocardiography is pivotal in the diagnosis of pericardial effusion and tamponade physiology. Ultrasound guidance for pericardiocentesis is currently considered the standard of care. Several approaches have been described recently, which differ mainly on the site of puncture (subxiphoid, apical, or parasternal). Although they share the use of low-frequency probes, there is absence of complete control of needle trajectory and real-time needle visualization. An in-plane and real-time technique has only been described anecdotally.A retrospective analysis of 11 patients (63% men, mean age: 37.7±21.2 years) presenting with cardiac tamponade admitted to the tertiary-care emergency department and treated with parasternal medial-to-lateral in-plane pericardiocentesis was carried out. The underlying causes of cardiac tamponade were different among the population. All the pericardiocentesis were successfully performed in the emergency department, without complications, relieving the hemodynamic instability. The mean time taken to perform the eight-step procedure was 309±76.4 s, with no procedure-related complications.The parasternal medial-to-lateral in-plane pericardiocentesis is a new technique theoretically free of complications and it enables real-time monitoring of needle trajectory. For the first time, a pericardiocentesis approach with a medial-to-lateral needle trajectory and real-time, in-plane, needle visualization was performed in a tamponade patient population.
New two dimensional ehocardiographically directed pericardiocentesis in cardiac tamponade
PMID:2364716
[Cited within: 1]

Seventeen patients with cardiac tamponade were treated by pericardiocentesis guided by two-dimensional (2-D) echocardiography and a needle guide. The needle guide used in the present study was designed so that the needle path lies within the center of the scan thickness. Before actual puncture, the mask method was performed in a water bath so that the needle progress avoided injury. The needle progress was monitored continuously in real time on the display throughout the procedure. Immediate relief from acute cardiac tamponade was obtained in all except one patient, who was treated by pericardiotomy because of insufficient drainage. In two patients, second drainage was performed because of reaccumulation of the pericardial effusion. There were no major complications. Nine patients recovered and the other patients died of underlying disease. Accurate and efficient visualization of the needle might allow a safer procedure. We conclude that pericardiocentesis guided by 2-D echocardiography using a needle guide may be a safe and easily applied technique for the management of pericardial effusion.
Clinical and echocardiographic characteristics of pericardial effusion in patients who underwent echocardiographically guided pericardiocentesis: Yonsei Cardiovascular Center experience, 1993-2003
DOI:10.3349/ymj.2004.45.3.462 URL [Cited within: 1]
Novel, long-axis in-plane ultrasound-guided pericardiocentesis for postoperative pericardial effusion drainage
DOI:10.1007/s00246-016-1438-z URL [Cited within: 1]
A contemporary look at pericardiocentesis
DOI:10.1016/j.tcm.2018.10.016 URL [Cited within: 1]