Dear editor,
Traditional Chinese medicine (TCM) is popular in many countries, especially in the Chinese population.[1,2] In Hong Kong, it has been estimated that around 15% of the population consumed Chinese medicine products/herbs in the preceding month. Common reasons for consumption include regulating bodily functions, curing disease, and building up health.[3] In a survey conducted in a local emergency department (ED), 1.4% of ED patients reported TCM use within one week of attendance; among them, 7.6% exhibited TCM-related toxicity.[4] A population-based survey in Hong Kong revealed that 2.3% of over-the-counter TCM users reported at least one TCM-related adverse effect in the previous year, especially in those with a lower education level and less access to reliable information.[5]
While most TCM-related toxicities are mild,[4] the medical literature is not lacking in reports of severe adverse reactions after the consumption of certain Chinese herbs, such as Aconitum[6] and the Datura species.[7] According to the 2017 Annual Report published by the Hong Kong Poison Information Center, Chinese herbal medicine (CHM) and proprietary Chinese medicine (PCM) ranked number 5 and 15 in the most common poisons to which individuals are exposed, respectively.[8] In Hong Kong, TCM poisoning accounts for 0.2% of all acute adult medical admissions[9] and aconitine poisoning is the most common cause of TCM-related hospital admission.[10]
In spite of a lack of training in TCM, emergency physicians are often called upon to manage patients with acute toxicity related to TCM use in the ED. A lack of knowledge about TCM may lead to delayed recognition, misdiagnosis, and inappropriate management. While offering complete TCM training to all emergency physicians is not feasible or necessary, they may benefit from training that specifically targets TCM products/herbs with a higher propensity for serious adverse effects. Proper risk assessment of individual TCM products/herbs requires an understanding of the overall toxic profile of all TCM poisonings encountered in ED settings.
Thus far, most literature about TCM poisoning has either focused on individual products/herbs/ingredients[6] or on a particular toxidrome caused by TCM.[7] For this reason, a knowledge gap exists in regard to the overall trend and patterns of TCM toxicities in the ED. This information has a significant implication for the future training of emergency physicians since it highlights TCM ingredients with the highest risk and the greatest need for focused training.
Thus, we conducted a retrospective study in two EDs in Hong Kong to characterize the trend, clinical presentations, and health resource utilization of TCM poisoning, and to further identify predictors of a poor outcome.
METHODS
Study design and setting
We studied consecutive patients who presented to the Accident and Emergency Department (A&E) at Queen Mary Hospital (QMH) and Pamela Youde Nethersole Eastern Hospital (PYNEH) for TCM-related toxicity over an 11-year period between 1 January 2006 and 31 December 2016. We referenced the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines when reporting this study.[11]
The two study centers are major A&Es on Hong Kong Island, with an annual ED attendance of approximately 130,000 and 150,000, respectively. Each center has its own ED toxicology team, and each team is comprised of a group of emergency medicine specialists with post-graduate training in clinical toxicology. Patients with acute poisoning presenting to these two centers are either managed directly by the respective ED toxicology teams, or indirectly through internal consultation. Both centers run their own emergency medicine wards, which enables extended care to be provided to poisoned patients. Both are recognized training centers of clinical toxicology with regular monthly audits of poisoning management. When it is necessary, clinicians can consult the Hong Kong Poison Information Center for management advice. They can also send patient serum and urine specimens, herbal remnants, left-over herbs or other specimens to the Toxicology Reference Laboratory of the Hospital Authority (HA) for chemical analysis.
In QMH, data from all poisoned patients presenting to A&E have been prospectively collected and entered into an electronic clinical toxicology database by a designated nurse since 2005. Thus, it is possible to retrospectively identify eligible cases in QMH by reviewing the database. In PYNEH, diagnostic codes using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) by emergency physicians are mandatory for all A&E consultations. We searched the Clinical Data Analysis and Reporting System (CDARS) of HA (an electronic repository that stored diagnostic codes and electronic information of all A&E consultations) for potentially eligible cases using a broad set of diagnostic codes which emergency physicians may use in recording TCM poisoning in the ED (Table 1).
Table 1 Clinical presentations of TCM-related toxicities and comparison of patients with any CHM or PCM exposure, n (%)
| Variables | Total (n=123) | Involving any CHM (n=80) | Involving any PCM (n=45) | P-value |
|---|---|---|---|---|
| Acute toxicity | 96 (78.0) | 55 (69.6) | 41 (91.1) | 0.006a |
| Nature of poisoning | <0.001a | |||
| Accidental | 14 (11.4) | 1 (1.3) | 13 (28.9) | |
| Adverse drug reaction | 86 (69.9) | 78 (97.5) | 10 (22.2) | |
| Intentional | 23 (18.7) | 1 (1.3) | 22 (48.9) | |
| Major toxic herbal ingredients involved | ||||
| Aconitine | 18 (14.6) | 18 (22.5) | 0 (0) | 0.001a |
| Atropine/hyoscyamine/scopolamine | 3 (2.4) | 3 (3.8) | 0 (0) | NSb |
| Cardiac glycosides | 4 (3.3) | 2 (2.5) | 2 (4.4) | NSb |
| Psoralen/isopsoralen | 10 (8.1) | 9 (11.3) | 2 (4.4) | NSb |
| Sophora alkaloids | 9 (7.3) | 9 (11.3) | 0 (0) | 0.026b |
| Methyl salicylate | 16 (13.0) | 0 (0) | 16 (35.6) | <0.001a |
| Anthraquinones | 13 (10.6) | 12 (15.0) | 3 (6.7) | NSa |
| Co-ingestion of Western medicine | 14 (11.4) | 1 (1.3) | 13 (28.9) | <0.001a |
| Time from exposure to symptom onset | <0.001a | |||
| <1 hour | 13 (10.6) | 8 (10.0) | 5 (11.1) | |
| ≥1-4 hours | 45 (36.6) | 32 (40.0) | 13 (28.9) | |
| >4-24 hours | 13 (10.6) | 12 (15.0) | 1 (2.2) | |
| >24 hours | 11 (8.9) | 11 (13.8) | 0 (0) | |
| Not applicable (no symptom) | 8 (6.5) | 1 (1.3) | 7 (15.6) | |
| Unknown | 33 (26.8) | 16 (20.0) | 19 (42.2) | |
| Time from exposure to ED presentation | <0.001a | |||
| <1 hour | 6 (4.9) | 1 (1.3) | 5 (11.1) | |
| ≥1-4 hours | 44 (35.8) | 21 (26.3) | 23 (51.1) | |
| >4-24 hours | 32 (26.0) | 24 (30.0) | 8 (17.8) | |
| >24 hours | 28 (22.8) | 25 (31.3) | 3 (6.7) | |
| Unknown | 13 (10.6) | 9 (11.3) | 6 (13.3) | |
| Triage categories | <0.001a | |||
| 1 (critical) | 11 (8.9) | 4 (5.0) | 7 (15.6) | |
| 2 (emergent) | 12 (9.8) | 5 (6.3) | 7 (15.6) | |
| 3 (urgent) | 65 (52.8) | 37 (46.3) | 30 (66.7) | |
| 4 (semi-urgent) | 35 (28.5) | 34 (42.5) | 1 (2.2) | |
| 5 (non-urgent) | 0 (0) | 0 (0) | 0 (0) | |
| PSS, median (IQR) | 1.0 ( 1.0-2.0) | 2.0 (1.0-2.0) | 1.0 (1.0-2.0) | 0.002c |
| Treatments | ||||
| Gastric lavage | 2 (1.6) | 0 (0) | 2 (4.4) | NSb |
| Activated charcoal | 21 (17.0) | 3 (3.8) | 18 (40.0) | <0.001a |
| Antidote | 7 (5.7) | 2 (2.5) | 5 (11.1) | NSb |
| Electrical therapy | 4 (3.2) | 3 (3.8) | 1 (2.2) | NSb |
| Antiarrhythmic agent | 7 (5.7) | 7 (8.8) | 0 (0) | 0.049b |
| Inotropic support | 4 (3.2) | 4 (5.0) | 0 (0) | NSb |
| Intubation and mechanical ventilation | 7 (5.7) | 3 (3.8) | 4 (8.9) | NSb |
| Renal replacement therapy | 4 (3.3) | 1 (1.3) | 3 (6.7) | NSb |
| Observation ward/emergency medicine ward admission | 59 (48.0) | 39 (48.8) | 20 (44.4) | NSa |
| General ward admission | 36 (29.3) | 23 (28.7) | 15 (33.3) | NSa |
| ICU admission | 15 (12.2) | 8 (10.0) | 7 (15.6) | NSa |
| Median ED length of stay, hours | 1.8 (1.0-2.6) | 2.0 (1.2-3.1) | 1.2 (0.7-2.5) | 0.004 |
| Median length of hospitalization, hours, median (IQR) | 26.7 (16.9-76.2) | 33.1 (17.6-90.9) | 23.2 (14.4-71.3 ) | NS |
| Median length of ICU stay, hours, median (IQR) | 30.8 (19.1-73.3) | 32.8 (19.4-81.4) | 30.4 (10.0-73.3) | NS |
| Episode death | 1 (0.8) | 0 (0) | 1 (2.2) | NSb |
| Poor outcome | 16 (13.0) | 8 (10.0) | 8 (17.8) | NSa |
TCM: traditional Chinese medicine; CHM: Chinese herbal medicine; PCM: proprietary Chinese medicine; ED: emergency department; PSS: Poison Severity Score; IQR: interquartile range; ICU: intensive care unit; NS: not significant; a: Chi-square test; b: Fisher’s exact test; c: Mann-Whitney U test.
Selection of subjects
We recruited patients with a diagnosis of TCM-related poisoning within the study period. We excluded patients with: (1) exposure to a product not fulfilling the definition of TCM in Hong Kong (see below); (2) missing information about the TCM ingredients; (3) exposure to a normal dose with no clinical effects; (4) clinical symptoms not explained by the TCM consumed; (5) allergic reaction to TCM product/herbs; and (6) adverse reactions due to drug interaction with Western medicine, which was not the focus of our study.
Definitions
Chinese herbs are widely used as food ingredients, health supplements, and medicine. Indeed, several plant species are used not only in TCM, but also in traditional or proprietary remedies in other Asian countries. As such, there is a need to clearly define TCM to minimize misclassification of exposure.
We referenced the Chinese Medicine Ordinance (Cap. 549) in Hong Kong, which provided clear definitions for local regulation of TCM use. In this study, we defined TCM as: (1) any materials of herbal, animal, or mineral origin prescribed by a registered Chinese medicine practitioner or a listed Chinese medicine practitioner; or (2) any materials of herbal, animal, or mineral origin self-prescribed or purchased over-the-counter that were customarily used by the Chinese and registered in Hong Kong. We also included TCM that was listed in the Pharmacopoeia of the People’s Republic of China.[12]
We further classified TCM into CHM and PCM, according to the Chinese Medicine Ordinance (Cap. 549). In this study, CHM refers to the Chinese herbal medicines specified in Schedule 1 and Schedule 2 of the Ordinance (https://www.elegislation.gov.hk/hk/cap549) and PCM refers to any proprietary product composed solely of any CHM or any materials of herbal, animal or mineral origin customarily used by the Chinese that is formulated in a finished dose form (such as pills or medicinal oils) and is delivered with a curative or health claim.[13]
We further defined acute toxicity as the adverse effects of a substance resulting either from a single exposure or from multiple exposures in less than 24 hours and the adverse effects should occur within 14 days of TCM consumption.[14]
Outcome
A poor outcome was defined as a composite of death, ICU admission, electrical therapy, antiarrhythmic agents, inotropic support, intubation and mechanical ventilation, renal replacement therapy, or extracorporeal membrane oxygenation (ECMO) during the index hospitalization.
Data collection
Medical records of all eligible cases were reviewed, and data were extracted by an investigator trained in clinical toxicology. Demographic data, TCM product/herbs used, clinical presentation, reasons of exposure, laboratory findings (including analytical findings in the Toxicology Reference Laboratory), consultation records from Hong Kong Poison Information Center, health resource utilization, and clinical outcomes were recorded using a standardized data collection form. We evaluated the whole clinical course of each case (from ED presentation to ED discharge/hospital discharge/death) and graded the severity of TCM toxicity using the Poison Severity Score (PSS) as: 0=none, 1=minor, 2=moderate, 3=severe, and 4=fatal poisoning, based on the most severe clinical features (including both subjective symptoms and objective signs). The PSS has been validated for a wide variety of poisoning.[15]
Data analysis
We calculated the ED incidence of TCM-related visits per 100,000 attendances over the study period and evaluated the trend using Poisson regression with the logarithm of total ED attendance as the offset term. We then characterized the clinical presentations and health resource utilization of TCM toxicity using descriptive statistics. Missing values were not inputted. We excluded cases with missing information on the herbal ingredients from data analysis, since their eligibility for inclusion could not be ascertained.
We stratified the data and compared the pattern of clinical toxicities of CHM and PCM exposure. Two patients consumed both CHM and TCM in our study. Therefore, we performed a sensitivity analysis by excluding them in the comparison to determine whether the findings remained robust. We studied the differences in proportions between groups using the Pearson’s Chi-square test (or the Fisher’s exact test where appropriate). We compared the mean values of the variables of interest across different groups using the Student’s t-test. For variables that did not follow a normal distribution, we calculated the median and interquartile range (IQR) and used the Mann-Whitney U test for analysis.
We then performed univariate analysis to identify factors associated with a poor outcome. Factors that were significantly associated with a poor outcome (P<0.05) in univariate analysis were entered into a multivariable backward logistic regression model to control for the confounding factors and to identify independent predictors. The SPSS for Window version 25.0 was used for data analysis. A two-tailed P-value <0.05 was considered statistically significant.
RESULTS
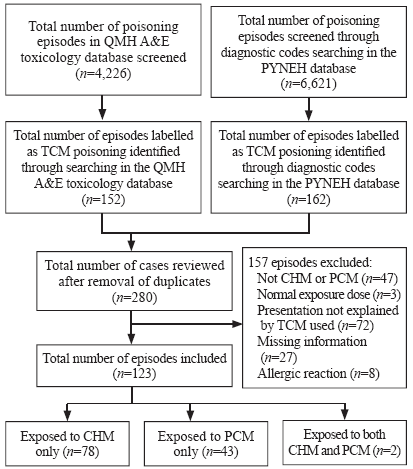
We identified 314 episodes (152 in QMH and 162 in PYNEH) and reviewed 280 episodes after removal of duplicates. We excluded 157 episodes based on the pre-defined criteria. Among the 123 episodes included, 78 involved CHM, 43 involved PCM, and 2 involved both (Figure 1). The mean annual incidences of TCM, CHM, and PCM poisoning were 4.19, 2.65, and 1.47 per 100,000 ED attendances, respectively. Over the study period, the incidence of CHM toxicities increased significantly, though the rise was modest (odds ratio [OR] 1.09, P=0.027, 95% confidence interval [CI] 1.01-1.18), while PCM toxicities (OR 0.96, P=0.399, 95% CI 0.88-1.05) and the overall trend remained static (OR 1.05, P=0.178, 95% CI 0.98-1.12).
Figure 1.
Figure 1.
Flow diagram of subject recruitment.
QMH: Queen Mary Hospital; PYNEH: Pamela Youde Nethersole Eastern Hospital; TCM: traditional Chinese medicine; CHM: Chinese herbal medicine; PCM: proprietary Chinese medicine.
The 123 studied episodes involved 122 patients (one patient presented with aconite poisoning twice over six months). Two clusters of poisoning were identified: one cluster involved three members of a family who suffered from neurotoxicity after consumption of Cassytha filiformis picked from the wild that was contaminated by Gelsemium elegans; the other involved seven members of a family who suffered gastrointestinal toxicity, two of whom suffered from liver derangement after consuming the root of Sauropus spatulifolius (Longliye).
The mean age of the patients was 49.4 years (range 1-95 years), and the female-to-male ratio was 1.8:1 (78 women and 44 men). Adverse reaction to TCM accounted for more than half of the studied episodes, and exposure was confirmed with laboratory analysis of patient/herbal specimen in 44 episodes (35.8%). Overall, the median PSS was 1.0 (IQR 1.0-2.0). The patterns of consumption, clinical presentations, severity of toxicities, treatments, and outcomes are summarized in Table 1.
The clinical presentations of CHM and PCM toxicities differed significantly in many aspects (Table 1). While the majority of CHM toxicities were adverse drug reactions, almost half of PCM poisonings were intentional. Toxic herbal ingredients, such as aconitine and Sophora alkaloids, were only seen in CHM poisoning. Salicylate poisoning was only seen in patients who ingested PCM that contained methyl salicylate. Patients with PCM toxicities tended to present earlier after exposure, have co-ingestion of Western medications, receive more urgent triage ranking and activated charcoal treatment. On the other hand, patients with CHM toxicities had a higher median PSS, a longer ED stay, and a higher chance of being given antiarrhythmic agents.
The toxic profiles of the seven toxic herbs, including their median PSS, organ system where the most symptomatology occurred, common clinical presentations (in descending order of frequency), and interventions given, are presented in Table 2.
Table 2 The Poison Severity Score (PSS) and distribution of most severe symptomatology in different organ systems of ten selected toxic herbal ingredients
| Herbal ingredients involved | Median PSS (IQR) | Organ system where the most severe symptomatology occurred | Commonest clinical features (n, %) | Intervention provided (n, %) |
|---|---|---|---|---|
| Aconitine | 2.0 (1.8-3.0) | Cardiovascular system | Limb numbness (13, 72.2), perioral numbness (12, 66.7), dizziness (12, 66.7), ventricular ectopics (7, 38.9), ventricular tachycardia (6, 33.3), vomiting (6, 33.3) | IV fluid (12, 66.7), administration of amiodarone (7, 38.9), administration of magnesium (4, 22.2), use of inotrope (4, 22.2), intubation (3, 16.7), synchronized cardioversion (3, 16.7), defibrillation (2, 11.1), activated charcoal (2, 11.1), CPR (1, 5.6) |
| Atropine/hyoscyamine/ scopolamine | 1.0 (1.0-1.5) | Nervous system | Anticholinergic toxidrome (3, 100), dizziness (3, 100) | IV fluid (1, 33.3) |
| Cardiac glycosides | 1.0 (1.0-2.5) | Cardiovascular system | Vomiting (3, 75.0), abdominal pain (2, 50.0), dizziness (2, 50.0), sinus bradycardia (1, 25.0) | IV fluid (1, 25.0), activated charcoal (1, 25.0), administration of DigiFab (1, 25.0) |
| Psoralen/isopsoralen | 2.0 (2.0-2.5) | Liver/kidney | Tea-colour urine (8, 88.9), malaise (8, 88.9), jaundice (4, 44.4), peak ALT > 1,000 IU/L (4, 44.4), renal impairment (1, 11.1) | IV fluid (1, 11.1), haemodialysis (1, 11.1) |
| Sophora alkaloids | 1.0 (1.0-1.0) | Nervous system | Dizziness (8, 88.9), vomiting (5, 55.6), palpitation (4, 44.4), limb weakness (3, 33.3), diarrhoea (3, 33.3) | IV fluid (3, 33.3) |
| Methyl salicylate | 1.0 (0.3-3.0) | Nervous system | Dizziness (5, 31.3), vomiting (5, 31.3), abdominal pain (5, 31.3), decrease in sensorium (4, 25.0), metabolic acidosis (2, 12.5), hypokalaemia (2, 12.5) | IV fluid (14, 87.5), activated charcoal (12, 75.0), urine alkalinization (5, 31.3), intubation (4, 25.0), haemodialysis (3, 18.8), gastric lavage (2, 12.5), defibrillation (1, 6.3), CPR (1, 6.3) |
| Anthraquinones | 2.0 (1.5-2.5) | Liver/kidney | Tea-colour urine (9, 69.2), peak ALT > 1,000 IU/L (8, 61.5), jaundice (7, 53.8), malaise (6, 46.2), poor oral intake (5, 38.5) | IV fluid (1, 7.7) |
ALT: alanine transaminase; IV: intravenous; CPR: cardiopulmonary resuscitation; unless otherwise stated, the rest of the patients were observed without any specific intervention.
Cardiac toxicities were the most severe in patients exposed to aconitine alkaloids and cardiac glycosides. The majority of patients with aconite poisoning (16/18) developed more than one arrhythmia during their clinical course, among whom only one had a history of heart disease. In our cohort, exposure to aconitine alkaloids accounted for the majority of those who received electric therapy. Administration of antiarrhythmic agents and inotrope was related to aconite poisoning. One patient with aconite poisoning developed cardiac arrest longer than one hour and survived after prolonged resuscitation without the use of ECMO.
Neurological toxicities were the most severe in patients who had been exposed to atropine/hyoscyamine/scopolamine, Sophora alkaloids, and methyl salicylate. Five patients with methyl salicylate poisoning complained of dizziness, while four experienced a decrease in sensorium, warranting intubation, and mechanical ventilation. Metabolic acidosis occurred in two patients, and three were given haemodialysis. One patient with advanced malignancies, who deliberately drank medicine oil that contained methyl salicylate, died.
Exposure to psoralen/isopsoralen (Fructus Psoraleae [Buguzhi]), anthraquinones (Polygoni multiflori [Heshouwu] and Rhizoma rhei [Dahuang]), and a number of other herbs, including Folium artemisiae argyi (Aiye), Fructus xanthii (Cang’erzi), Radix bupleuri (Chaihu), Radix scutellariae (Huangqin), Rhizoma dioscoreae bulbiferae (Huangyaozi), Rhizoma pinella (Banxia), Sauropus spatulifolius (Longliye) was associated with elevated liver transaminases and deranged liver function, but none required liver transplantation.
Univariate analysis revealed that a higher triage category (category 1 or 2), exposure to aconitine, exposure to methyl salicylate, earlier ED presentation after exposure, a lower triage Glasgow Coma Scale and a lower triage systolic blood pressure were significantly associated with a poor outcome. When all six factors were entered into the multivariable backward logistic regression model, only high triage category (OR 7.33, 95% CI 1.32-40.61, P=0.023), exposure to aconitine (OR 27.42, 95% CI 2.55-295.31, P=0.006), and exposure to methyl salicylate (OR 24.17, 95% CI 2.09-279.69, P=0.011) remained independent predictors of a poor outcome (Table 3).
Table 3 Predictors for poor outcomes in TCM poisoning in the ED
| Variables | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Exposure to aconitine | 6.79 (2.11-21.83)* | 27.42 (2.55-295.31)* |
| Exposure to methyl salicylate | 8.47 (2.55-28.14)** | 24.17 (2.09-279.69)* |
| High triage category (category 1 or 2) | 12.10 (3.75-38.69)** | 7.33 (1.32-40.61)* |
| Triage systolic BP | 0.96 (0.94-0.99)* | |
| Triage Glasgow Coma Scale | 0.71 (0.41-1.23) | |
| Time from exposure to ED presentation <1 hour | Ref | |
| Time from exposure to ED presentation ≥1-4 hours | 0.59 (0.09-3.70) | |
| Time from exposure to ED presentation >4-24 hours | 0.13 (0.01-1.23) | |
| Time from exposure to ED presentation >24 hours | 0.07 (0.01-1.02) |
TCM: traditional Chinese medicine; ED: emergency department; BP: blood pressure; CI: confidence interval; OR: odds ratio; *P<0.05; **P<0.01.
DISCUSSION
In this study, we characterized the overall pattern of TCM toxicity presenting to the ED using inclusion and exclusion criteria that were based on regulatory standards, clear definitions of TCM and its various forms, and validated PSS. We believe this approach provides a better understanding of the overall impact of TCM poisoning in the ED and the relative contribution of different toxic herbal ingredients, highlighting key areas of focus for emergency physicians and clinical toxicologists without training in TCM.
In the literature, there is a paucity of published data on the ED incidence of TCM toxicities. Our study found that, in high-volume Asian EDs serving a predominantly Chinese society where TCM use is common, the ED incidence of TCM toxicities has remained low throughout the past decade. Although the trend of CHM toxicities appears to be rising slightly, the overall number of TCM toxicities, as well as that of PCM toxicities, has remained low and static. The reported incidence in the current study was lower compared with a previous local study (102.4 per 100,000 ED attendance),[4] but this can be explained by the different study methodology, use of more stringent recruitment criteria, and the exclusion of allergic reactions in the current study.
Despite the low incidence, our study demonstrated that 13% of TCM poisoning cases in the ED had a poor outcome. The rarity of occurrence has led to a lack of experience in clinicians in recognizing and managing TCM poisoning. When the clinician’s native language is not Chinese, additional problems in interpreting the CHM formula and recognizing the toxic herbal ingredients will appear. Our experience indicates that the ED toxicology team model, with around-the-clock access to poison center consultation and laboratory support, helps accumulate experience in the team. As in other poisonings, the ED toxicology team can also help reduce unnecessary hospital admission and shorten patients’ length of stay without jeopardizing the quality of patient care.[16,17] Our findings reveal that almost half of TCM poisoning cases can be managed by emergency physicians in the observation ward or emergency short-stay ward with supportive care. Indeed, less than one third of patients require hospital admission.
CHM and PCM toxicities differ in several ways in regard to presentation. The majority of CHM toxicities presented as adverse drug reactions, while almost half of PCM overdoses were intentional. Certain formulation of PCM, often in the form of medicinal oil and oral capsules/tablets, enables ingestion of a large amount in deliberate self-harm. Patients with PCM toxicities are often assigned a higher triage rating and administered activated charcoal, which could be explained by their earlier presentation and a higher rate of co-ingestion of Western medicine. However, emergency physicians should be aware that CHM is no less harmful than PCM. In our study, the median PSS of CHM toxicities was significantly higher than that of PCM poisoning, and the ED length of stay was also longer.
Our study found that a higher triage category (category 1 or 2), exposure to aconitine, and exposure to methyl salicylate are significant predictors of poor outcomes in TCM poisoning. This finding has two implications. First, the 5-level triage system currently in use in Hong Kong, which is based on the triage nurse’s assessment of the severity of patient’s presenting condition and the stability of vital signs,[18] can identify high-risk TCM-poisoned patients for whom early intensive treatment is necessary. Second, while the management of salicylate poisoning is generally covered in most medical undergraduate curricula, it is necessary to include aconitine poisoning in formal emergency medicine and clinical toxicology training.
Aconitine and related alkaloids are potent cardiotoxins and neurotoxins found in TCM “Chuanwu” (the root tuber of Aconitum carmichaeli), “Caowu” (the root tuber of Aconitum kusnezoffii) and “Fuzi” (the lateral root tuber of Aconitum carmichaeli), which are used to treat rheumatism, arthritis, fractures, bruises, and pains.[6] Aconitine and mesaconitine bind to the receptor site 2 of the voltage-sensitive Na+ channel at its open state, causing persistent activation of these channels in excitable tissues. They can trigger life-threatening arrhythmia through delayed after-depolarization and early after-depolarization.[19] Although regulations on prescription and publicity measures have reduced the incidence of aconite poisoning in the last decade,[20] our study shows that aconite poisoning remains a recurring problem in the ED. The combination of cardiovascular, neurological, and gastrointestinal toxicities observed in our study was consistent with that reported in the literature,[21,22] signifying that recognition of the presentation pattern may play a role in the early clinical diagnosis of aconite poisoning. Our observation further indicates that almost all emergency physicians followed the Advanced Cardiac Life Support pathway, including the use of amiodarone, magnesium, lignocaine, and electrical therapy, in managing ventricular dysrhythmias arising from aconite poisoning, although with mixed success. These findings are consistent with those reported in a systematic review of the management of ventricular dysrhythmia in aconite poisoning.[23] Flecainide, charcoal hemoperfusion, and cardiopulmonary bypass were not used in our case series, and therefore we cannot comment on their effectiveness. Based on our data, we support the use of a time-buying strategy, including supportive treatment and prolonged cardiopulmonary resuscitation (in case of cardiac arrest), to allow the body to excrete the toxic alkaloids.
Consistent with a previous study on PCM, we found that most PCM toxicities were mild or moderate, except for those that involve methyl salicylate.[24] Methyl salicylate is a major ingredient in numerous over-the-counter PCM in the form of medicinal oil, ointments, lotions or liniments, which are widely used to relieve musculoskeletal aches and pains.[25,26] Accidental or deliberate ingestion of methyl salicylate can result in rapid salicylate poisoning, because of its high concentration in PCM, liquid formulation, and lipid solubility. The latter increases its penetration across the blood-brain barrier and causes central nervous system toxicity. The presence of other toxic ingredients, such as camphor and turpentine, may contribute to neurological toxicities.[27,28] Our study also found that neurological toxicities were a predominant toxic feature after exposure to methyl salicylate: four patients required endotracheal intubation for airway protection. The high occurrence of vomiting (around 1/3 in our study) and decreased sensorium (1/4 in our study) call for proper airway protection when gastrointestinal decontamination is indicated.
Although not associated with a poor outcome, as defined in our study, we found that exposure to certain herbal ingredients was associated with hepatotoxicity. Herb-induced hepatotoxicity has been well reported after consumption of psoralen/isopsoralen (Fructus psoraleae [Buguzhi]), anthraquinones (Polygoni multiflori (Heshouwu) and Rhizoma rhei (Dahuang), Folium artemisiae argyi (Aiye), Fructus xanthii (Cang’erzi), Radix bupleuri (Chaihu), Radix scutellariae (Huangqin), Rhizoma dioscoreae bulbiferae (Huangyaozi), and Rhizoma pinella (Banxia) in the literature.[29,30,31] In our study, we also identified two cases of hepatotoxicity induced by Sauropus Spatulifolius (Longliye), which was not reported previously within the literature.[32] In general, patients who are exposed to these herbs often exhibit elevated liver transaminase and features of deranged liver function. It is often only after the exclusion of other plausible causes that a diagnosis of herb-induced hepatotoxicity is made. Emergency physicians should actively check for exposure to hepatotoxic herbs when managing patients with unexplained deranged liver function in the ED.
Limitations
There are several limitations to this study. First, its retrospective design might lead to information bias. We sought to minimize the misclassification of cases by screening the whole QMH toxicology database for potential cases and using a broad strategy for the diagnostic code search in PYNEH. Second, the current study relied on clinical diagnoses made by the attending clinicians and critical retrospective chart reviews by the investigators. We did not involve Chinese medicine practitioners when evaluating causality. On the one hand, we might have under-reported the incidence of TCM toxicities in the ED, because of the stringent criteria and definitions used in the case selection, the lack of information in some cases, and the occurrence of misdiagnosis by attending clinicians. On the other hand, we might have over-reported the incidence, because causality was not critically reviewed by a Chinese medicine practitioner. However, we believe that this limitation reflects the real clinical situation, where the timely consultation of a Chinese medicine practitioner is not an option in most EDs. Moreover, stringent case selection criteria and definitions are important to avoid overstating the toxic effects of TCM, especially when not every case has been analytically confirmed. Third, we were not able to explore the reason behind TCM toxicity in many cases due to incomplete documentation. We could not evaluate the impact of prescription or dispensary error, contamination, impurities, adulteration, and substitution, which are not uncommon in TCM poisoning. Thus, further studies should examine the relative contribution of these factors in instances of TCM poisoning encountered in the ED. Finally, the data of this study were obtained from two EDs in Hong Kong only. The results might not be generalizable to other EDs where the population has a different prevalence and pattern of TCM use.
CONCLUSIONS
Although TCM poisoning is a rare occurrence in the ED, a significant portion of patients develop a poor outcome. Emergency physicians should be aware of the differences between CHM and PCM poisoning and should not underestimate the consequences of an adverse drug reaction to CHM. Training that focuses on managing aconite poisoning and methyl salicylate poisoning should be offered to all emergency physicians practising in regions where TCM use is popular.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Tony Wing Lai Mak from the Hospital Authority Toxicology Reference Laboratory, as well as Dr. Man Li Tse and Mr. Tin Yat Chow from the Hong Kong Poison Information Center for reviewing the laboratory and poison center consultation records to help in the creation of this manuscript.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval: The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW 16-1003) and the Research Ethics Committee of the Hospital Authority Hong Kong East Cluster (HKEC-2016-112).
Conflicts of interests: The authors have no conflicts of interest to declare.
Contributors: RPKL conceived and designed the study and developed the method. JKSL and MSHT provided study supervision. RPKL and WLY retrieved medical records, performed chart review, and collected data. RPKL and EHYL analyzed and interpreted the data. RPKL, WLY, JKSL and MSHT reviewed the literature. RPKL drafted the article. All authors contributed substantially to its revision and provided final approval. PRKL took the responsibility for the paper as a whole.
Reference
Use frequency of traditional Chinese medicine in
Complementary and alternative medicine use in multiracial
DOI:10.1016/j.ctim.2004.11.002
URL
PMID:15907674
[Cited within: 1]

OBJECTIVE: To determine the prevalence of complementary and alternative medicine (CAM) use in Singapore, the factors influencing CAM use, and the attitudes, beliefs and perceptions of the general population towards CAM. DESIGN: An interviewer-administered questionnaire survey in a housing estate with demographic and socioeconomic characteristics closely matching that of Singapore. RESULTS: 76% (95% C.I. 73.9-77.9%) used CAM over a 12-month period. Females were 2.1 times (95% C.I. 1.3-3.4) more likely than males to use CAM. Chinese (84%) were the most frequent users, followed by Malays (69%) and Indians (69%), with adjusted odds ratios of 0.4 (95% C.I. 0.2-0.7) for Malays and 0.4 (95% C.I. 0.2-0.8) for Indians. Traditional Chinese Medicine (88%) was the most widely used form of CAM, followed by Traditional Malay (Jamu) Medicine (8%) and Traditional Indian (Ayuverdic) Medicine (3%). Similar to western studies, CAM was more likely to be used for maintenance of health than for treatment of illness. Different from western studies, CAM use was not independently associated with household income, marital status, age and education. Seventy-four percent did not discuss their use of CAM with their western-trained doctors. CONCLUSIONS: The high prevalence of CAM use in multi-racial Singapore suggests the same may be true in other Asian countries. Western-trained doctors need to understand CAM better and communicate more with their patients regarding CAM use. The lack of a scientific evidence base for most forms of CAM notwithstanding, its ubiquitous use worldwide is something that governments and the medical profession cannot afford to ignore.
Thematic Household Survey Report No. 3. Hong Kong; Census and Statistics Department
Traditional Chinese medicine use among emergency patients in Hong Kong. Hong Kong
[J]
Acute adverse events from over-the-counter Chinese herbal medicines: a population-based survey of
DOI:10.1186/1472-6882-13-336
URL
PMID:24279604
[Cited within: 1]

BACKGROUND: Although over-the-counter traditional Chinese herbal medicine (COTC) is commonly used to treat everyday illness in many parts of the world, no population-based study has been done to examine the prevalence and factors associated with COTC-related adverse events. METHODS: A cross-sectional telephone survey was conducted among Hong Kong Chinese adults in 2011 (n = 1100) with informed verbal consent. Stepwise logistic regression of demographic, attitudinal and behavioral variables was used to determine factors associated with past-year adverse events. RESULTS: Of study respondents, 71.7% (789/1100) reported past-year COTC use and 2.3% (25/1100) reported at least one COTC-related adverse event in the past year. Of the 27 adverse events cases reported among COTC users, the most common were allergic reactions (n = 11) dizziness (n = 5), and gastro-intestinal problems (n = 4). Pills/capsules were the dosage form that caused the highest proportion of adverse events (n = 10), followed by plasters (n = 7), creams/ointments (n = 5), and ingestible powders (n = 2).Although COTC users reporting adverse events were more likely to report greater practices to avoid adverse events (OR = 6.47; 95% CI: 1.38-30.3); they were also more likely to possess lower education levels (OR = 9.64, 95% CI: 2.20-42.3) and to have received COTC information from non-reliable, mass-media information sources such as magazines (OR = 3.32; 95% CI: 1.01-8.50) or television (OR = 2.93; 95% CI: 1.03-10.7). Package labels were also felt to be unclear by 42.9% of COTC users. A large proportion of COTC users demonstrated low levels of COTC-related knowledge, while the main impediment to greater information-seeking was the belief that reliable COTC information is not obtainable from Western health professionals. CONCLUSIONS: Despite global movements toward more stringent complementary medicine regulation, the limited accessibility of reliable information and widespread misperceptions among consumers present major challenges for the safe use of complementary medicine.
Aconite poisoning
DOI:10.1080/15563650902904407 URL [Cited within: 3]
Hong Kong poison information centre: annual report 2017. Hong Kong
[J]
Hospital admissions due to adverse reactions to Chinese herbal medicines.
[J]
Poisoning by Chinese herbal medicines in Hong Kong: a hospital-based study
URL
PMID:7900276
[Cited within: 1]

The harmful effects of some Chinese herbal medicines (CHM) have become a cause for concern among the medical profession and the general public in Hong Kong. From 1989 to 1993, at least 33 patients were treated in the Prince of Wales Hospital because of severe poisoning by CHM. Of these, 20 presented with clinical features typical of aconitine poisoning following the ingestion of
The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies
DOI:10.7326/0003-4819-147-8-200710160-00010
URL
PMID:17938396
[Cited within: 1]

Much biomedical research is observational. The reporting of such research is often inadequate, which hampers the assessment of its strengths and weaknesses and of a study's generalizability. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Initiative developed recommendations on what should be included in an accurate and complete report of an observational study. We defined the scope of the recommendations to cover 3 main study designs: cohort, case-control, and cross-sectional studies. We convened a 2-day workshop in September 2004, with methodologists, researchers, and journal editors, to draft a checklist of items. This list was subsequently revised during several meetings of the coordinating group and in e-mail discussions with the larger group of STROBE contributors, taking into account empirical evidence and methodological considerations. The workshop and the subsequent iterative process of consultation and revision resulted in a checklist of 22 items (the STROBE Statement) that relate to the title, abstract, introduction, methods, results, and discussion sections of articles. Eighteen items are common to all 3 study designs and 4 are specific for cohort, case-control, or cross-sectional studies. A detailed Explanation and Elaboration document is published separately and is freely available at http://www.annals.org and on the Web sites of PLoS Medicine and Epidemiology. We hope that the STROBE Statement will contribute to improving the quality of reporting of observational studies.
DOI:10.3390/medicines4010002
URL
PMID:28930219
[Cited within: 1]

Background: The purpose of this discussion is to explore the theory, evidence base, and practice of Qigong for individuals with cancer. Questions addressed are: What is qigong? How does it work? What evidence exists supporting its practice in integrative oncology? What barriers to wide-spread programming access exist? Methods: Sources for this discussion include a review of scholarly texts, the Internet, PubMed, field observations, and expert opinion. Results: Qigong is a gentle, mind/body exercise integral within Chinese medicine. Theoretical foundations include Chinese medicine energy theory, psychoneuroimmunology, the relaxation response, the meditation effect, and epigenetics. Research supports positive effects on quality of life (QOL), fatigue, immune function and cortisol levels, and cognition for individuals with cancer. There is indirect, scientific evidence suggesting that qigong practice may positively influence cancer prevention and survival. No one Qigong exercise regimen has been established as superior. Effective protocols do have common elements: slow mindful exercise, easy to learn, breath regulation, meditation, emphasis on relaxation, and energy cultivation including mental intent and self-massage. Conclusions: Regular practice of Qigong exercise therapy has the potential to improve cancer-related QOL and is indirectly linked to cancer prevention and survival. Wide-spread access to quality Qigong in cancer care programming may be challenged by the availability of existing programming and work force capacity.
Compendium of chemical terminology: IUPAC recommendations 2 nd ed
DOI:10.1126/science.248.4960.1242 URL PMID:17809910 [Cited within: 1]
Poisoning severity score. Grading of acute poisoning
DOI:10.3109/15563659809028940 URL [Cited within: 1]
The impact of an emergency department toxicology team in the management of acute intoxication. Hong Kong
[J]
Toxicology training unit in emergency department reduces admission to other specialties and hospital length of stay. Hong Kong
[J]
Validation of the Hong Kong accident and emergency triage guidelines
DOI:10.12809/hkmj133900
URL
[Cited within: 1]

Objective To validate the Hong Kong Accident and Emergency Triage guidelines.
Design Retrospective chart review.
Setting The Accident and Emergency Department of a tertiary hospital in Hong Kong.
Participants Patients who attended the Accident and Emergency Department on one day in February 2012.
Main outcome measures The inter-rater reliability in two pairs of nurses grouped according to experience and validity as compared with an expert panel.
Results Of the 100 patients recruited and triaged into levels 1 to 5, the weighted kappa coefficient (inter-rater reliability) for the two pairs of nurses was 0.699 and 0.717, respectively. The weighted kappa coefficient for validity was 0.766. When only patients in triage levels 3 and 4 were included, the weighted kappa coefficient for reliability dropped to 0.632 and 0.585, respectively. The weighted kappa coefficient for validity also decreased to 0.558.
Conclusions The overall inter-rater reliability and validity of the Guidelines appeared acceptable. Further revision of the Guidelines on triaging patients to levels 3 or 4 is probably necessary.
Aconitine poisoning due to Chinese herbal medicines: a review
URL
PMID:7839574
[Cited within: 1]

Both
Incidence of herb-induced aconitine poisoning in Hong Kong: impact of publicity measures to promote awareness among the herbalists and the public
DOI:10.2165/00002018-200225110-00006
URL
PMID:12222992
[Cited within: 1]

BACKGROUND: In Hong Kong 'chuanwu' (the main root of Aconitum carmichaeli) and 'caowu' (the root of Aconitum kusnezoffii) are used by herbalists to treat patients with various musculoskeletal disorders. These aconite roots contain aconitine, mesaconitine and hypaconitine, which are neurotoxins and cardiotoxins. During 1989 to 1991, 31 patients were treated in public hospitals because of poisoning by aconite roots and there were two deaths from ventricular arrhythmias. In late 1991, healthcare officials together with cardiologists held a press conference to warn the public, healthcare professionals and herbalists of the potential toxicity of aconite roots. The risk of ventricular arrhythmias and the need for urgent medical attention were highlighted. An information leaflet was also sent to hospital doctors. Since 1992, the topic was covered periodically in the local newspapers, medical journals and continuing medical education programmes. OBJECTIVE: The objective of this study was to assess the impact of these publicity measures on the incidence of herb-induced aconitine poisoning in the New Territories East, based on the number of admissions to the Prince of Wales Hospital. METHODS: During 1989 to 1993 and 1996 to 1998, all patients admitted to our medical wards because of herb-induced aconitine poisoning were identified by on-going surveillance of medical patients, searching our computerised medical record system and reviewing reports received by the 24-hour Drug and Poisons Information Bureau. RESULTS: The number of hospitalisations due to aconitine poisoning markedly decreased from four to six per year in 1989 to 1991 to one to two per year in 1992 to 1993. The annual incidence of aconitine poisoning showed a marked decrease from 0.49 to 0.69 [overall 0.60, 95% confidence intervals (CI) 0.34 to 0.99] to 0.10 to 0.22 (overall 0.16, 95% CI 0.03 to 0.46) per 100,000 population (p = 0.024). During 1996 to 1998, herb-induced aconitine poisoning remained uncommon, with zero to two hospital admissions per year or an annual incidence of zero to 0.33 (overall 0.17, 95% CI 0.05 to 0.43) per 100,000 population (p = 0.016). DISCUSSION: It is possible that the herbalists could have used smaller doses of 'chuanwu' and 'caowu' than before. Patients could be more compliant with the instructions on how to prepare the herbal decoction at home. However, our experience suggested that publicity measures to promote awareness, among the herbalists and the public, may reduce the incidence of poisoning due to toxic herbs such as aconite roots.
Cardiotoxicity after accidental herb-induced aconite poisoning
DOI:10.1016/0140-6736(92)92951-b
URL
PMID:1359321
[Cited within: 1]

Aconitine and its related alkaloids are known cardiotoxins with no therapeutic role in modern western medicine. The rootstocks of Aconitum plants, which contain aconite alkaloids, have been common components of Chinese herbal recipes. We have documented life-threatening intoxication in 17 Chinese subjects after accidental herb-induced aconite poisoning. All patients developed symptoms of aconite toxicity within 2 h of herb ingestion. Most developed tachyarrhythmias, including ventricular tachycardia and fibrillation from which 2 patients died. Toxicological evaluation revealed that aconites from the Aconitum rootstocks were the only plausible casual factor for intoxication. These cases point to the need for strict surveillance of herbal substances with low safety margins.
Clinical features and management of herb-induced aconitine poisoning
DOI:10.1016/j.annemergmed.2003.10.046
URL
PMID:15111916
[Cited within: 1]

STUDY OBJECTIVE: We define the potential sources, clinical manifestations, and treatment of aconitine poisoning. METHODS: The database of the National Poison Center in Taiwan was retrospectively searched for the diagnosis of aconitine poisoning for 1990 to 1999. The reasons for taking the aconite roots, the clinical features, management, and possible predisposing factors were noted. RESULTS: A total of 17 cases occurred and consisted of 9 men and 8 women aged 30 to 70 years. Thirteen patients ingested aconite roots as treatment for rheumatism and wounds. Two patients volunteered to test the effects of aconite roots in a drug study. Two patients accidentally ingested the aconite roots. After a latent period of 10 to 90 minutes, patients developed a combination of neurologic (n=17), cardiovascular (n=14), gastrointestinal (n=9), and other (n=5) features typical of aconitine poisoning. Four patients developed ventricular tachycardia. All patients received supportive treatment. Patients with ventricular tachycardia were also treated with charcoal hemoperfusion. All patients made a complete recovery. CONCLUSION: Life-threatening ventricular tachycardia can occur after the consumption of aconite roots. The risk is higher with inadequately processed aconite roots, large doses, or tincture preparations. With increasing popularity of herbal medicines, herb-induced aconitine poisoning may also be seen in Western countries.
The management of ventricular dysrhythmia in aconite poisoning
DOI:10.1080/15563650.2017.1291944 URL [Cited within: 1]
Poisoning due to Chinese proprietary medicines
DOI:10.1177/096032719501400508
URL
PMID:7612306
[Cited within: 1]

1. To determine the toxic potentials of those Chinese proprietary medicines (CPM) which are commonly used for self-poisoning by adults in Hong Kong, all patients admitted to four of the eight general medical wards at the Prince of Wales Hospital between January 1988 and December 1993 were retrospectively studied. 2. There were 54 women and 17 men with their age ranging from 15 to 86 years. Twenty-three subjects (32%) also took alcohol, chemicals or drugs. Of the 51 subjects (72%) who had taken topical medicaments, 22 had no symptoms while 28 had minor features of gastrointestinal irritation (n = 26), mild (n = 2) or severe (n = 1) salicylate poisoning. Of the 17 subjects (24%) who had taken CPM tablets/capsules, nine had mild symptoms including nausea/vomiting and drowsiness. The three remaining patients (4%) who had ingested liquid CPM preparations were asymptomatic. Elevated plasma salicylate or paracetamol concentrations (> 0.1 mmol l-1) were found in some patients who had taken topical medicaments and CPM tablets/capsules, respectively. All the 71 patients completely recovered. 3. Most of the CPM used for self-poisoning in Hong Kong were of low to moderate toxicity except for those containing wintergreen oil (methyl salicylate).
Potential dangers from topical preparations containing methyl salicylate
DOI:10.1177/096032719601500905
URL
PMID:8880210
[Cited within: 1]

Methyl salicylate (oil of wintergreen) is widely available in many over-the-counter liniments, ointments, lotions or medicated oils for the relief of musculoskeletal aches and pains. Ingestion of methyl salicylate poses the threat of severe, rapid-onset salicylate poisoning because of its liquid, concentrated form and lipid solubility. Excessive usage of these preparations in patients receiving warfarin may result in adverse interactions and bleedings. Methyl salicylate in topical analgesic preparations may cause irritant or allergic contact dermatitis and anaphylactic reactions. Physicians should fully appreciate the potential dangers from topical preparations containing methyl salicylate.
The risk of severe salicylate poisoning following the ingestion of topical medicaments or aspirin
DOI:10.1136/pgmj.72.844.109
URL
PMID:8871462
[Cited within: 1]

Apart from isolated reports of severe salicylate poisoning after ingesting an unusually large amount of a medicinal oil, there are no published data on the threat arising from attempted suicide with topical medicaments containing methyl salicylate or wintergreen oil compared with aspirin tablets. In this retrospective study, the admission plasma salicylate concentrations and clinical presentations were compared in 80 subjects who had taken aspirin tablets (n = 42) or topical medicaments (n = 38). The proportions of subjects being symptomatic were similar in the two groups. Although the admission plasma salicylate concentrations were generally higher in subjects who had ingested aspirin tablets, the two highest readings (4.3 and 3.5 mmol/1) belonged to two of the subjects who had taken topical medicaments. Because of its liquid, concentrated form and lipid solubility, methyl salicylate poses the threat of severe, rapid-onset salicylate poisoning. The toxic potential of topical medicaments containing methyl salicylate or wintergreen oil should be fully appreciated by both physicians and the general public.
Small doses, big problems: a selected review of highly toxic common medications
URL
PMID:8247936
[Cited within: 1]

Many commonly used medications have serious toxicity in children when ingested in small doses. The toxicologic characteristics of methyl salicylate, camphor, topical imidazolines, benzocaine, and diphenoxylate-atropine are striking examples. All of these medications except Lomotil are over-the-counter and therefore, are often perceived as minimally harmful when ingested. For all of these substances, however, doses as little as 1/4 teaspoon or 1/2 tablet can have serious or fatal consequences. Thus, referral to an emergency department is prudent for ingestions involving these products. Options for initial gastrointestinal (GI) decontamination are variable, depending on the estimated amount and time of the ingestion. Induction of emesis is contraindicated for significant camphor, topical imidazoline, and Lomotil ingestions. Activated charcoal should be administered in all cases. Finally, the emergency physician must recognize the potential seriousness of these ingestions, as well as their clinical presentations to provide expeditious evaluation and treatment.
Acute intoxication and recovery following massive turpentine ingestion: clinical and toxicological data
URL
PMID:9167245
[Cited within: 1]

Reports of acute turpentine intoxication, particularly containing toxicological data, are poorly verified in the literature. This report regards the intentional massive ingestion of turpentine solution in an elderly woman who developed mainly central nervous system manifestations, then had an impressive and quick total recovery although the initial prognosis was very bad. Blood and urine levels of turpentine were monitored using gas chromatography and at the early toxicogenic stage were 28 micrograms/mL and 15 micrograms/mL respectively. Gastric fluid analysis on admission to the hospital revealed the presence of approximately 200 mL turpentine in the intestine. A review of earlier reports is given.
Traditional Chinese Medicine and herbal hepatotoxicity: a tabular compilation of reported cases
URL
PMID:25536637
[Cited within: 1]

Traditional Chinese Medicine (TCM) with its focus on herbal use became popular worldwide. Treatment was perceived as safe, with neglect of rare adverse reactions including liver injury. To compile worldwide cases of liver injury by herbal TCM, we undertook a selective literature search in the PubMed database and searched for the items Traditional Chinese Medicine, TCM, Traditional Asian Medicine, and Traditional Oriental Medicine, also combined with the terms herbal hepatotoxicity or herb induced liver injury. The search focused primarily on English-language case reports, case series, and clinical reviews. We identified reported hepatotoxicity cases in 77 relevant publications with 57 different herbs and herbal mixtures of TCM, which were further analyzed for causality by the Council for International Organizations of Medical Sciences (CIOMS) scale, positive reexposure test results, or both. Causality was established for 28/57 different herbs or herbal mixtures, Bai Xian Pi, Bo He, Ci Wu Jia, Chuan Lian Zi, Da Huang, Gan Cao, Ge Gen, Ho Shou Wu, Huang Qin, Hwang Geun Cho, Ji Gu Cao, Ji Xue Cao, Jin Bu Huan, Jue Ming Zi, Jiguja, Kudzu, Ling Yang Qing Fei Keli, Lu Cha, Rhen Shen, Ma Huang, Shou Wu Pian, Shan Chi, Shen Min, Syo Saiko To, Xiao Chai Hu Tang, Yin Chen Hao, Zexie, and Zhen Chu Cao. In conclusion, this compilation of liver injury cases establishes causality for 28/57 different TCM herbs and herbal mixtures, aiding diagnosis for physicians who care for patients with liver disease possibly related to herbal TCM.
Epidemiology of drug-induced liver injury in China: a systematic analysis of the Chinese literature including 21,789 patients. Eur
[J]
Drug-induced liver injury associated with complementary and alternative medicine: a review of adverse event reports in an Asian community from 2009 to 2014
DOI:10.1186/s12906-016-1168-z URL [Cited within: 1]
Dragon’s tongue (Sauropus spatulifolius)-induced liver injury - a report of two cases. In: North American Congress of Clinical Toxicology (NACCT) Abstracts 2017