INTRODUCTION
Sepsis is a severe critical care syndrome and a life-threatening condition with high morbidity and poor prognosis.[1,2] Acute respiratory distress syndrome (ARDS) is a type of acute diffuse, inflammatory lung injury caused by various factors inside and outside the lungs, leading increased pulmonary vascular permeability, increased lung weight, and loss of aerated lung tissue.[3] Many studies have reported that sepsis is one of the most common and lethal causes of ARDS,[4] and nearly 40% ARDS incidence results from sepsis.[5,6,7] ARDS, as a main cause of acute respiratory failure, is mainly characterized by increased pulmonary endothelial and epithelial permeability, diffuse alveolar injury, and severe pulmonary inflammation.[8] Proteinaceous fluid accumulation in the pulmonary interstitial area or alveoli reduces pulmonary compliance and volume for patients with ARDS.[9] Therefore, fluid management is crucial to ARDS. However, choices of fluid resuscitation strategies and fluid input volumes remain a thorny problem. Several relevant studies[10,11,12,13,14] have been conducted to explore this problem but showed contradictory results. Fluid resuscitation is also the mainstay of therapy for sepsis.[15] Restricted fluid resuscitation and negative fluid balance are shown to be beneficial to the prognosis of sepsis patients.[16,17,18] However, for ARDS patients secondary to sepsis, only a few studies have been conducted to illuminate the relationship between fluid resuscitation and prognosis. The study aimed to explore this problem.
METHODS
We conducted a single-center and retrospective study in Ruijin Hospital (2,100 beds) Affiliated to Shanghai Jiao Tong University School of Medicine in Shanghai, China. It was approved by the Ethics Committee of Ruijin Hospital (Reference number: 2017119). Because our study was retrospective, the patient’s consent was not necessary.
Inclusion criteria
Exclusion criteria
Patients were excluded if they: (1) participated in other studies; (2) had inadequate medical records; (3) had concomitant pulmonary diseases; (4) died; (5) were discharged within 24 hours; or (6) needed emergency operations after EICU admission.
Data collection
Baseline data included demographics, sepsis category, source of sepsis, the origin of patients, comorbidities, Acute Physiologic and Chronic Health Evaluation II (APACHE II) scores, and Sequential Organ Failure Assessment (SOFA) scores during the first 24 hours after EICU admission. We also collected data of tidal volumes, PaO2/FiO2, positive end-expiratory pressure (PEEP), duration of hospital and EICU stay as well as mechanical ventilation. The primary end point was in-hospital mortality, and the secondary end points were duration of hospital and EICU stay as well as mechanical ventilation.
Daily fluid input included oral, enteral, and intravenous fluids. Daily fluid output included urine volume, ultrafiltration, and fluid loss from drains and tubes. We didn’t consider insensible water loss. Daily net fluid balance for seven days was calculated by subtracting daily fluid output from daily fluid input.
We divided all patients into the ARDS group and the non-ARDS group. Furthermore, patients of the ARDS group were divided into survivors and non-survivors.
Statistical analysis
Continuous demographic and clinical variables were described as mean±standard deviation (SD) or median (interquartile range [IQR]), depending on the normality measured by the Kolmogorov-Smirnov method. Categorical variables were described as numbers and percentages. We used Student’s t-test or Mann-Whitney U-test to compare data of continuous variables, and Pearson’s Chi-square, continuity correction, Fisher’s exact, or likelihood ratio tests for categorical variables. Binary logistic regression analysis was applied to analyze the relationship between indicators with statistical significance (P<0.05) and mortality. If the two-sided P-value was <0.05, comparisons were considered significant. Analyses of data were performed using SPSS Version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
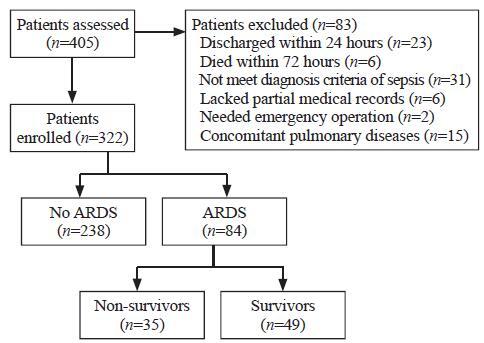
We assessed 405 patients in total, and 83 were excluded for various reasons which were listed in Figure 1. A total of 322 patients were enrolled finally, and 84 (26.1%) had ARDS within 72 hours after sepsis onset. Among patients with ARDS secondary to sepsis, 49 (58.3%) survived during the EICU stay (Figure 1).
Figure 1.
Figure 1.
Study flow chart.
First, we divided sepsis patients into the ARDS group and the non-ARDS group. Epidemiologic statistics compared between the two groups were counted as follows: men accounted for 60.6%, the median age was 62 (IQR 46-73) years, the mean body mass index (BMI) was 23.68±3.80 kg/m2, and patients with sepsis (59.6%) occupied a higher proportion (Table 1).
Table 1 Characteristics of sepsis patients with or without ARDS
| Parameters | Patients (n=322) | No ARDS (n=238) | ARDS (n=84) | P-value |
|---|---|---|---|---|
| Sex Male Female Age (years) BMI (kg/m2) Sepsis category Septic shock Sepsis Mortality Origin EICU Medical emergency ward Trauma surgery ward Other Comorbidities Hypertension Diabetes Arrhythmia CHD CKD Cerebral infarction Source of sepsis Gut Lung Urinary tract Abdomen Skin Blood Not found Other SOFA score APACHE II Creatinine (μmol/L) PaO2/FiO2 (mmHg) Duration of hospital stay (days) Duration of ICU stay (days) Duration of mechanical ventilation (days) | 195 (60.6) 127 (39.4) 62 (46-73) 23.68±3.80 192 (59.6) 130 (40.4) 72 (22.4) 219 (68.0) 67 (20.8) 9 (2.8) 27 (8.4) 138 (42.9) 78 (24.2) 19 (5.9) 26 (8.1) 5 (1.6) 12 (3.7) 35 (10.9) 181 (56.2) 18 (5.6) 48 (14.9) 9 (2.8) 8 (2.5) 13 (4.0) 10 (3.1) 6 (4-8) 11±5 167.4±217.3 231.9±94.8 21 (13-34) 14 (7-25) 0 (0-8) | 142 (59.7) 96 (40.3) 63 (43-73) 23.65±3.81 139 (58.4) 99 (41.6) 37 (15.5) 156 (65.5) 58 (24.4) 6 (2.5) 18 (7.6) 95 (39.9) 52 (21.8) 13 (5.5) 20 (8.4) 8 (3.4) 4 (1.7) 28 (11.8) 120 (50.4) 18 (7.6) 39 (16.3) 9 (3.8) 6 (2.5) 10 (4.2) 8 (3.4) 5 (3-7) 10±5 163.3±223.5 255.0±91.2 21 (14-33) 14 (7-24) 0 (0-0) | 53 (63.1) 31 (36.9) 62 (50-70) 23.71±3.83 53 (63.1) 31 (36.9) 35 (41.7) 63 (75.0) 9 (10.7) 3 (3.6) 9 (10.7) 43 (51.2) 26 (31.0) 6 (7.1) 6 (7.1) 4 (4.8) 1 (1.2) 7 (8.3) 61 (72.6) 0 (0) 9 (10.7) 0 (0) 2 (2.4) 3 (3.6) 2 (2.4) 8 (4-8) 14±5 178.8±198.7 166.4±71.0 23 (11-45) 15 (7-31) 11 (6-24) | 0.580 0.900 0.892 0.451 <0.001 0.110 0.008 0.907 0.370 0.322 0.094 0.574 0.715 0.804 1.000 0.385 <0.001 0.001 0.210 0.019 1.000 1.000 0.937 <0.001 <0.001 0.582 <0.001 0.737 0.227 <0.001 |
Values are given as number (%), median (25th-75th percentile), or mean±standard deviation (SD); BMI: body mass index; EICU: emergency intensive care unit; CHD: coronary heart disease; CKD: chronic kidney disease; SOFA: Sequential Organ Failure Assessment; APACHE II: Acute Physiology and Chronic Health Evaluation II.
Most patients were from EICU (68.0%) and medical emergency ward (20.8%). The most frequent comorbidities were hypertension (42.9%) and diabetes (24.2%). Lung (56.2%) and abdomen (14.9%) were the most common sources of sepsis (Table 1).
Sepsis patients had a lower PaO2/FiO2 ratio in the ARDS group than in the non-ARDS group (166.4±71.0 vs. 255.0±91.2, P<0.05). Besides, patients from the ARDS group had worse physical conditions, including higher illness severity scores and longer duration of mechanical ventilation (11 [6-24] days vs. 0 [0-0] days, P<0.05). Mortality rates were much higher in the ARDS group than in the non-ARDS group (41.7% vs. 15.5%, P<0.05). The duration of hospital and EICU stay didn’t show the statistical difference (Table 1).
Non-survivors indeed had higher SOFA scores and APACHE II scores, as well as shorter duration of hospital and EICU stay than survivors. However, we didn’t find significant differences among tidal volumes, PaO2/FiO2 ratio, and duration of mechanical ventilation between the two groups (Table 2).
Table 2 Characteristics of survivors and non-survivors
| Parameters | Survivors (n=49) | Non-survivors (n=35) | P-value |
|---|---|---|---|
| Sex Male Female Age (years) BMI (kg/m2) Sepsis category Septic shock Sepsis Origin EICU Medical emergency ward Trauma surgery ward Other Comorbidities Hypertension Diabetes Arrhythmia CHD CKD Cerebral infarction Source of sepsis Gut Lung Abdomen Other Not found SOFA score APACHE II score PEEP (cmH2O) Tidal volume (mL/kg) PaO2/FiO2 (mmHg) Creatinine (μmol/L) Duration of hospital stay (days) Duration of ICU stay (days) Duration of mechanical ventilation (days) | 32 (65.3) 17 (34.7) 64 (51-70) 24.30±3.50 29 (59.2) 20 (40.8) 33 (67.3) 7 (14.3) 3 (6.1) 6 (12.3) 29 (59.2) 15 (30.6) 4 (8.2) 6 (12.2) 4 (8.2) 1 (2.0) 5 (10.2) 37 (75.5) 4 (8.2) 1 (2.0) 2 (4.1) 7 (6-9) 13±5 6 (5-8) 8.6±2.1 175.1±71.5 148.2±161.3 32 (18-66) 19 (7-31) 12 (7-25) | 21 (60.0) 14 (40.0) 57 (44-70) 22.89±4.10 24 (68.6) 11 (31.4) 30 (85.7) 2 (5.7) 0 (0) 3 (8.6) 14 (40.0) 11 (31.4) 2 (5.7) 0 (0) 1 (2.9) 0 (0) 2 (5.7) 24 (68.6) 5 (14.3) 3 (8.6) 1 (2.9) 8 (7-11) 16±5 5 (5-8) 8.0±2.6 154.1±68.4 223.5±233.2 12 (7-25) 10 (7-18) 7 (6-18) | 0.619 0.427 0.097 0.379 0.055 0.371 0.069 0.858 0.083 0.936 1.000 0.009 0.585 0.297 0.739 0.482 0.592 0.386 1.000 0.022 0.023 0.233 0.312 0.186 0.089 <0.001 0.001 0.300 |
Values are given as number (%), median (25th-75th percentile), or mean±standard deviation (SD); BMI: body mass index; EICU: emergency intensive care unit; CHD: coronary heart disease; CKD: chronic kidney disease; SOFA: Sequential Organ Failure Assessment; APACHE II: Acute Physiology and Chronic Health Evaluation II; PEEP: positive end-expiratory pressure.
In the first 24 hours, mean fluid input volumes in the ARDS group were more than those in the non-ARDS group (50.1±22.1 mL/kg vs. 41.0±21.6 mL/kg, P<0.05). During the 7-day period, patients with ARDS had more mean daily fluid input volumes (46.3±20.8 mL/kg vs. 35.5±21.7 mL/kg, P<0.05) than those without ARDS, while mean daily output volumes between the two groups were similar (43.3±21.1 mL/kg vs. 40.7±21.3 mL/kg, P>0.05). Besides, we compared fluid input and output volumes between the two groups every day in seven days and found daily fluid input volumes were more in the ARDS group with significant differences while daily output volumes between the two groups didn’t show statistical differences except results on the 5th day.
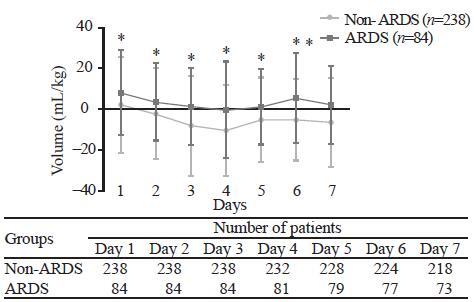
Patients with ARDS showed daily positive net fluid balance for seven days, while those without ARDS showed daily negative net fluid balance since the second day with statistically significant differences (P<0.05) (Figure 2). We compared net fluid balance every day for seven days between the ARDS group and the non-ARDS group and found all results had significant differences (P<0.05).
Figure 2.
Figure 2.
Mean fluid balance (mL/kg, mean±standard deviation) in sepsis patients with or without ARDS during seven continuous days after onset of sepsis. *Statistically significant difference at the P<0.05 level between two groups.
Our results showed that mean daily fluid input volumes were much lower in survivors than in non-survivors (43.2±16.7 mL/kg vs. 51.0±25.2 mL/kg, P<0.01) while output volumes were much higher in survivors (45.2±19.8 mL/kg vs. 40.2±22.7 mL/kg, P<0.05). We also compared daily fluid input and output for seven days between the two groups. Results of fluid input showed statistical differences only on the 4th and 6th day, and fluid output consequences didn’t show statistical differences except for the 7th day.
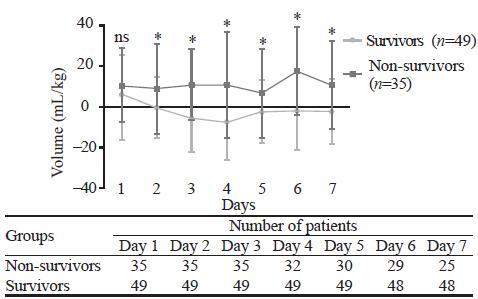
Survivors showed daily negative net fluid balance for seven days except for the first day, while non-survivors showed daily positive net fluid balance every day during the 7-day period with statistically significant differences (P<0.01) (Figure 3). We compared net fluid balance every day for seven days between survivors and non-survivors and found all results except the first day had statistically significant differences (P<0.05).
Figure 3.
Figure 3.
Mean fluid balance (mL/kg, mean±standard deviation) in survivors and non-survivors during seven continuous days in sepsis patients complicating with ARDS. *Statistically significant difference at the P<0.05 level between two groups. ns: not significant.
Finally, we used binary logistic regression analysis to measure which of the following indicators, including SOFA score, APACHE II score, and mean daily fluid balance, were independent prognostic factors. Results demonstrated that only mean fluid balance (P<0.01) was independently associated with the prognosis of sepsis patients with ARDS.
DISCUSSION
ARDS is a clinical syndrome characterized by refractory hypoxemia with high mortalities. A study conducted in 15 adult ICUs of Shanghai between 2001 and 2002 reported that ARDS incidence accounted for approximated 2% of all ICU admissions with a 90-day mortality rate of more than 70%.[21] The main treatment method of ARDS was etiology treatment, and fluid resuscitation was considered as an effective supportive treatment method of ARDS patients for increased capillary permeability and protein-rich fluid accumulation as the most important pathophysiological changes.[8] Many studies reported the relationship between fluid resuscitation and prognosis of ARDS, but results were contradictory. A large randomized study conducted by Wiedemann et al[10] compared a conservative and a liberal strategy of fluid management in 1,000 patients with acute lung injury, and concluded that patients from conservative fluid administration group had a shorter duration of mechanical ventilation and ICU stay while there was no significant difference in the primary outcome of the 60-day mortality. Another post-hoc analysis of a cohort of 313 children with ARDS revealed that positive fluid balance (in increments of 10 mL/[kg·day]) was associated with a significant increase in both mortality and prolonged duration of mechanical ventilation, independent of the presence of multiple organ system failure and the extent of oxygenation.[12] Rosenberg et al[13] assessed the fluid balance of 844 patients from 24 hospitals and 75 intensive care units and found that negative cumulative fluid balance at day 4 of acute lung injury was associated with significantly lower mortality. However, some investigators[11] found fluid resuscitation strategy might be a potential risk factor for long-term cognitive impairment. Sepsis, as the most frequent cause of ARDS, has a close relation with ARDS in critically ill patients. In 2002, an epidemiological study reported that sepsis was the most common cause of acute respiratory failure.[22] Another study conducted by the Korean Study Group on Respiratory Failure declared the incidence rate of sepsis-induced ARDS was 6.8% in Korea.[23] Fluid resuscitation is a lifesaving therapy for both sepsis and ARDS patients but only a few studies have been conducted to explore the relationship between fluid balance and prognosis of ARDS secondary to sepsis. Murphy et al[24] carried out a study containing 212 patients with septic shock complicated with ALI and found both early fluid management and late fluid management of septic shock complicated with ALI can influence patient outcomes. However, the term “acute lung injury (ALI)” was eliminated by the Berlin definition of ARDS in 2012.[20] Our study used the newest criteria of ARDS and mainly focused on ARDS patients secondary to sepsis. We included 322 patients, and ARDS patients accounted for 26.1%. In the group of sepsis complicated with ARDS, survivors had much lower input volumes and higher output volumes than non-survivors. Survivors showed daily negative net fluid balance since the second day, while non-survivors showed daily positive net fluid balance every day during the 7-day period with statistically significant differences except the first day. These results indicated that sufficient volume was necessary to resuscitate patients during the early time and excess fluid infusion should be avoided for fear of aggravation of pulmonary edema or injury of other organs. Negative fluid balance since the second day might be a prognostic factor for ARDS patients secondary to sepsis.
Besides fluid resuscitation, lung-protective ventilation was also an important strategy for ARDS patients, which could reduce mortality. Several clinical trials have demonstrated that lung-protective ventilation with low airway pressure and tidal volumes could prolong the survival time of patients with ARDS.[25,26,27] For patients with ARDS, the use of lower tidal volumes during ventilation was also an effective treatment that could reduce the release of inflammatory cytokines and detrimental lung stretch.[28,29,30] An early clinical trial reported the lower tidal volume was approximately 8.1 mL/kg compared with traditional tidal volume, which was approximately 12.2 mL/kg.[31] We didn’t find significant differences in tidal volumes between survivors and non-survivors because we employed low tidal volumes as a routine treatment for all ARDS patients. As for PEEP, there was a lack of an accurate method to define it. Some investigators thought higher PEEP values might improve the prognosis of ARDS patients.[32] We compared PEEP values between survivors and non-survivors and found no statistical difference. Acute kidney injury (AKI) was also reported to be an independent prognostic factor of patients with sepsis.[33,34] We wanted to clarify whether the positive fluid balance was due to AKI. Results showed that there was no statistical difference in creatinine on sepsis patients with or without ARDS (178.8±198.7 μmol/L vs. 163.3±223.5 μmol/L, P>0.05). We also compared the creatinine level between survivors and non-survivors of sepsis combined with ARDS. Although the creatinine level was higher in non-survivors than in survivors (223.5±233.2 μmol/L vs. 148.2±161.3 μmol/L), there was no statistical difference between the two groups (P>0.05). This indicated that positive fluid balance was not due to AKI and AKI was not an independent prognostic factor in our study.
Compared with sepsis patients without ARDS, the ARDS group did have higher SOFA and APACHE II scores, indicating a higher severity of the disease. However, we also knew that sepsis was a complex pathophysiological condition that might involve multiple organs. Due to the limited number of patients, we couldn’t make more detailed stratification to determine which factor had the most significant impact on prognosis. But our results showed that there was no difference in creatinine levels between the two groups, indicating AKI was not an important factor affecting the severity of the disease. However, the PaO2/FiO2 ratio was significantly lower, and the duration of mechanical ventilation was significantly longer in sepsis patients with ARDS, suggesting that the severity of ARDS might be an important factor affecting the severity of the entire disease, but not the only factor.
There were some limitations in our study. This was a monocentric and retrospective study, and enrolled patients were not enough. Besides, clinical data during the first several hours were not recorded which might be more important. And some clinical and laboratory parameters we omitted could influence our results in some degree.
CONCLUSIONS
We conclude that early negative fluid balance since the second day is independently associated with a better prognosis of ARDS patients secondary to sepsis. Early enough fluid resuscitation and late restricted fluid resuscitation might be beneficial to the prognosis of ARDS patients secondary to sepsis.
Funding: This work was supported by Shanghai Shenkang Hospital Development Center of China (SHDC12017116); Program for Outstanding Medical Academic, Shanghai Municipal Committee of Science and Technology (184119500900); Shanghai Municipal Commission of Health and Family Planning (2016ZB0206, ZHYY-ZXYJHZX-1-201702) and Shanghai Jiao Tong University School of Medicine (DLY201803) to Er-zhen Chen; Shanghai Municipal Commission of Health and Family Planning (201640089) to Zhi-tao Yang.
Ethical approval: The study was approved by the Ethics Committee of Ruijin Hospital (Reference number: 2017119).
Conflicts of interest: There are no competing interests involving this work.
Contributors: YMW wrote the first draft of this paper. All authors approved the final version.
Reference
Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit
DOI:10.1016/S2213-2600(14)70061-X
URL
PMID:24740011
[Cited within: 1]

BACKGROUND: Global epidemiological data regarding outcomes for patients in intensive care units (ICUs) are scarce, but are important in understanding the worldwide burden of critical illness. We, therefore, did an international audit of ICU patients worldwide and assessed variations between hospitals and countries in terms of ICU mortality. METHODS: 730 participating centres in 84 countries prospectively collected data on all adult (>16 years) patients admitted to their ICU between May 8 and May 18, 2012, except those admitted for fewer than 24 h for routine postoperative monitoring. Participation was voluntary. Data were collected daily for a maximum of 28 days in the ICU and patients were followed up for outcome data until death or hospital discharge. In-hospital death was analysed using multilevel logistic regression with three levels: patient, hospital, and country. FINDINGS: 10,069 patients were included from ICUs in Europe (5445 patients; 54.1%), Asia (1928; 19.2%), the Americas (1723; 17.1%), Oceania (439; 4.4%), the Middle East (393; 3.9%), and Africa (141; 1.4%). Overall, 2973 patients (29.5%) had sepsis on admission or during the ICU stay. ICU mortality rates were 16.2% (95% CI 15.5-16.9) across the whole population and 25.8% (24.2-27.4) in patients with sepsis. Hospital mortality rates were 22.4% (21.6-23.2) in the whole population and 35.3% (33.5-37.1) in patients with sepsis. Using a multilevel analysis, the unconditional model suggested significant between-country variations (var=0.19, p=0.002) and between-hospital variations (var=0.43, p<0.0001) in the individual risk of in-hospital death. There was a stepwise increase in the adjusted risk of in-hospital death according to decrease in global national income. INTERPRETATION: This large database highlights that sepsis remains a major health problem worldwide, associated with high mortality rates in all countries. Our findings also show a significant association between the risk of death and the global national income and suggest that ICU organisation has an important effect on risk of death. FUNDING: None.
Sepsis: a roadmap for future research
DOI:10.1016/S1473-3099(15)70112-X
URL
PMID:25932591
[Cited within: 1]

Sepsis is a common and lethal syndrome: although outcomes have improved, mortality remains high. No specific anti-sepsis treatments exist; as such, management of patients relies mainly on early recognition allowing correct therapeutic measures to be started rapidly, including administration of appropriate antibiotics, source control measures when necessary, and resuscitation with intravenous fluids and vasoactive drugs when needed. Although substantial developments have been made in the understanding of the basic pathogenesis of sepsis and the complex interplay of host, pathogen, and environment that affect the incidence and course of the disease, sepsis has stubbornly resisted all efforts to successfully develop and then deploy new and improved treatments. Existing models of clinical research seem increasingly unlikely to produce new therapies that will result in a step change in clinical outcomes. In this Commission, we set out our understanding of the clinical epidemiology and management of sepsis and then ask how the present approaches might be challenged to develop a new roadmap for future research.
Definition and epidemiology of acute respiratory distress syndrome
DOI:10.21037/atm.2017.06.62
URL
PMID:28828357
[Cited within: 1]

Fifty years ago, Ashbaugh and colleagues defined for the first time the acute respiratory distress syndrome (ARDS), one among the most challenging clinical condition of the critical care medicine. The scientific community worked over the years to generate a unified definition of ARDS, which saw its revisited version in the Berlin definition, in 2014. Epidemiologic information about ARDS is limited in the era of the new Berlin definition, and wide differences are reported among countries all over the world. Despite decades of study in the field of lung injury, ARDS is still so far under-recognized, with 2 out of 5 cases missed by clinicians. Furthermore, although advances of ventilator strategies in the management of ARDS associated with outcome improvements-such as protective mechanical ventilation, lower driving pressure, higher PEEP levels and prone positioning-ARDS appears to be undertreated and mortality remains elevated up to 40%. In this review, we cover the history that led to the current worldwide accepted Berlin definition of ARDS and we summarize the recent data regarding ARDS epidemiology.
Screening of ARDS patients using standardized ventilator settings: influence on enrollment in a clinical trial
DOI:10.1007/s00134-004-2163-2
URL
PMID:14991096
[Cited within: 1]

OBJECTIVES: The American-European consensus conference (AECC) definition for acute respiratory distress syndrome (ARDS) requires a PaO(2)/F(I)O(2)< or =200 mmHg, regardless of ventilator settings. We report the results of using standardized ventilator settings to screen and enroll ARDS patients in a clinical trial of high-frequency oscillatory ventilation (HFOV), including the impact on study enrollment, and potential effects on study outcome. DESIGN: Prospective cohort study. SETTING: Intensive care units in two teaching hospitals. PARTICIPANTS. A consecutive sample of 41 patients with early ARDS by AECC criteria (baseline PaO(2)/F(I)O(2)< or =200) who met all other inclusion/exclusion criteria for the HFOV trial. INTERVENTIONS: Patients were placed on standardized ventilator settings (tidal volume 7-8 ml/kg, PEEP 10 cmH(2)O, F(I)O(2) 1.0), and the PaO(2)/F(I)O(2) was reassessed after 30 min. RESULTS: Seventeen patients (41.5%) had PaO(2)/F(I)O(2) ratios that remained < or =200 mmHg [Persistent ARDS; PaO(2)/F(I)O(2)=94+/-36 (mean+/-SD)] and went on to inclusion in the HFOV study; however, in 24 patients (58.5%) the PaO(2)/F(I)O(2) was >200 mmHg [Transient ARDS; PaO(2)/F(I)O(2)=310+/-74] and these patients were ineligible for the HFOV study. The ICU mortality was significantly greater (52.9 vs 12.5%; p=0.01) in the Persistent ARDS patients. CONCLUSIONS: The use of these standardized ventilatory significantly impacted the PaO(2)/F(I)O(2) ratio and therefore the ARDS prevalence and trial enrollment. These results have effects on the evaluation of the current ARDS literature and conduct of clinical trials in ARDS and hence consideration should be given to the use of standardized ventilatory settings in future ARDS trials.
Acute lung injury and acute respiratory distress syndrome in sepsis and septic shock
DOI:10.1016/s0749-0704(05)70111-1
URL
PMID:10768083
[Cited within: 1]

Sepsis remains the leading cause of ARDS, and ARDS is still an often fatal condition. With our expanding knowledge of the pathobiologic mechanisms and the relationship between these two entities, early recognition, treatment, and prevention of sepsis may prevent or hasten recovery from ARDS. Understanding the biologic markers involved in the complex inflammatory response of sepsis and acute lung injury offers the possibility of future investigations to target treatment based on these mediators.
Risk factors for the development of acute lung injury in patients with septic shock: an observational cohort study
URL PMID:18434908 [Cited within: 1]
Causes and timing of death in patients with ARDS
DOI:10.1378/chest.128.2.525
URL
PMID:16100134
[Cited within: 1]

BACKGROUND: Since the early 1980s, case fatality of patients with ARDS has decreased, and explanations are unclear. DESIGN AND METHODS: Using identical definitions of ARDS and organ failure, we analyzed consecutive cohorts of patients meeting syndrome criteria at our institution in 1982 (n = 46), 1990 (n = 112), 1994 (n = 99), and 1998 (n = 205) to determine causes and timing of death. RESULTS: Overall case fatality has decreased from 68% in 1981-1982 to a low of 29% in 1996, plateauing since the mid-1990s (p = 0.001 for trend). Sepsis syndrome with multiple organ failure remains the most common cause of death (30 to 50%), while respiratory failure causes a small percentage (13 to 19%) of deaths. The distribution of causes of death has not changed over time. There was no change in the timing of death during the study periods: 26 to 44% of deaths occurred early (< 72 h after ARDS onset), and 56 to 74% occurred late (> 72 h after ARDS onset). However, the increased survival over the past 2 decades is entirely accounted for by patients who present with trauma and other risk factors for their ARDS, while survival for those patients whose risk factor is sepsis has not changed. Additionally, withdrawal of life support in these patients is now occurring at our institution significantly more frequently than in the past, and median time until death has decreased in patients who have support withdrawn. CONCLUSIONS: While these results do not explain the overall case fatality decline in ARDS, they do indicate that sepsis syndrome remains the leading cause of death and suggest that future therapies to improve survival be targeted at reducing the complications of sepsis.
Acute respiratory distress syndrome
DOI:10.1056/NEJMra1608077 URL PMID:28792873 [Cited within: 2]
The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination
DOI:10.1164/ajrccm.149.3.7509706
URL
PMID:7509706
[Cited within: 1]

The acute respiratory distress syndrome (ARDS), a process of nonhydrostatic pulmonary edema and hypoxemia associated with a variety of etiologies, carries a high morbidity, mortality (10 to 90%), and financial cost. The reported annual incidence in the United States is 150,000 cases, but this figure has been challenged, and it may be different in Europe. Part of the reason for these uncertainties are the heterogeneity of diseases underlying ARDS and the lack of uniform definitions for ARDS. Thus, those who wish to know the true incidence and outcome of this clinical syndrome are stymied. The American-European Consensus Committee on ARDS was formed to focus on these issues and on the pathophysiologic mechanisms of the process. It was felt that international coordination between North America and Europe in clinical studies of ARDS was becoming increasingly important in order to address the recent plethora of potential therapeutic agents for the prevention and treatment of ARDS.
Comparison of two fluid-management strategies in acute lung injury
DOI:10.1056/NEJMoa062200
URL
PMID:16714767
[Cited within: 2]

BACKGROUND: Optimal fluid management in patients with acute lung injury is unknown. Diuresis or fluid restriction may improve lung function but could jeopardize extrapulmonary-organ perfusion. METHODS: In a randomized study, we compared a conservative and a liberal strategy of fluid management using explicit protocols applied for seven days in 1000 patients with acute lung injury. The primary end point was death at 60 days. Secondary end points included the number of ventilator-free days and organ-failure-free days and measures of lung physiology. RESULTS: The rate of death at 60 days was 25.5 percent in the conservative-strategy group and 28.4 percent in the liberal-strategy group (P=0.30; 95 percent confidence interval for the difference, -2.6 to 8.4 percent). The mean (+/-SE) cumulative fluid balance during the first seven days was -136+/-491 ml in the conservative-strategy group and 6992+/-502 ml in the liberal-strategy group (P<0.001). As compared with the liberal strategy, the conservative strategy improved the oxygenation index ([mean airway pressure x the ratio of the fraction of inspired oxygen to the partial pressure of arterial oxygen]x100) and the lung injury score and increased the number of ventilator-free days (14.6+/-0.5 vs. 12.1+/-0.5, P<0.001) and days not spent in the intensive care unit (13.4+/-0.4 vs. 11.2+/-0.4, P<0.001) during the first 28 days but did not increase the incidence or prevalence of shock during the study or the use of dialysis during the first 60 days (10 percent vs. 14 percent, P=0.06). CONCLUSIONS: Although there was no significant difference in the primary outcome of 60-day mortality, the conservative strategy of fluid management improved lung function and shortened the duration of mechanical ventilation and intensive care without increasing nonpulmonary-organ failures. These results support the use of a conservative strategy of fluid management in patients with acute lung injury. (ClinicalTrials.gov number, NCT00281268 [ClinicalTrials.gov].).
The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury
DOI:10.1164/rccm.201111-2025OC
URL
PMID:22492988
[Cited within: 2]

RATIONALE: Cognitive and psychiatric morbidity is common and potentially modifiable after acute lung injury (ALI). However, practical measures of neuropsychological function for use in multicenter trials are lacking. OBJECTIVES: To determine whether a validated telephone-based neuropsychological test battery is feasible in a multicenter trial. To determine the frequency and risk factors for long-term neuropsychological impairment. METHODS: As an adjunct study to the Acute Respiratory Distress Syndrome Clinical Trials Network Fluid and Catheter Treatment Trial, we assessed neuropsychological function at 2 and 12 months post-hospital discharge. MEASUREMENTS AND MAIN RESULTS: Of 406 eligible survivors, we approached 261 to participate and 213 consented. We tested 122 subjects at least once, including 102 subjects at 12 months. Memory, verbal fluency, and executive function were impaired in 13% (12 of 92), 16% (15 of 96), and 49% (37 of 76) of long-term survivors. Long-term cognitive impairment was present in 41 of the 75 (55%) survivors who completed cognitive testing. Depression, post-traumatic stress disorder, or anxiety was present in 36% (37 of 102), 39% (40 of 102), and 62% (63 of 102) of long-term survivors. Enrollment in a conservative fluid-management strategy (P = 0.005) was associated with cognitive impairment and lower partial pressure of arterial oxygen during the trial was associated with cognitive (P = 0.02) and psychiatric impairment (P = 0.02). CONCLUSIONS: Neuropsychological function can be assessed by telephone in a multicenter trial. Long-term neuropsychological impairment is common in survivors of ALI. Hypoxemia is a risk factor for long-term neuropsychological impairment. Fluid management strategy is a potential risk factor for long-term cognitive impairment; however, given the select population studied and an unclear mechanism, this finding requires confirmation.
Positive fluid balance is associated with higher mortality and prolonged mechanical ventilation in pediatric patients with acute lung injury
DOI:10.1155/2011/854142
URL
PMID:21687578
[Cited within: 2]

Introduction. We analyzed a database of 320 pediatric patients with acute lung injury (ALI), to test the hypothesis that positive fluid balance is associated with worse clinical outcomes in children with ALI. Methods. This is a post-hoc analysis of previously collected data. Cumulative fluid balance was analyzed in ml per kilogram per day for the first 72 hours after ALI while in the PICU. The primary outcome was mortality; the secondary outcome was ventilator-free days. Results. Positive fluid balance (in increments of 10 mL/kg/24 h) was associated with a significant increase in both mortality and prolonged duration of mechanical ventilation, independent of the presence of multiple organ system failure and the extent of oxygenation defect. These relationships remained unchanged when the subgroup of patients with septic shock (n = 39) were excluded. Conclusions. Persistently positive fluid balance may be deleterious to pediatric patients with ALI. A confirmatory, prospective randomized controlled trial of fluid management in pediatric patients with ALI is warranted.
Review of a large clinical series: association of cumulative fluid balance on outcome in acute lung injury: a retrospective review of the ARDSnet tidal volume study cohort
DOI:10.1177/0885066608329850
URL
PMID:19103612
[Cited within: 2]

OBJECTIVE: To evaluate the independent influence of fluid balance on outcomes for patients with acute lung injury. DESIGN: Secondary analysis of a prospective cohort study conducted between March 1996 and March 1999. SETTING: The study involved 10 academic clinical centers (with 24 hospitals and 75 Intensive Care Units). PATIENTS: All patients for whom fluid balance data existed (844) from the 902 patients enrolled in the National Heart Lung Blood Institute's ARDS Network ventilator-tidal volume trial. INTERVENTIONS: The study had no interventions. MEASUREMENTS/RESULTS: On the first day of study enrollment, 683 patients were, on average, more than 3.5 L in positive fluid balance compared to 161 patients in negative fluid balance (P < .001). Cumulative negative fluid balance on day 4 of the study was associated with an independently lower hospital mortality (OR, 0.50; 95% CI, 0.28-0.89; P < .001) more ventilator and intensive care unit-free days. CONCLUSIONS: Negative cumulative fluid balance at day 4 of acute lung injury is associated with significantly lower mortality, independent of other measures of severity of illness.
A simple clinical predictive index for objective estimates of mortality in acute lung injury
DOI:10.1097/CCM.0b013e3181a009b4
URL
PMID:19384214
[Cited within: 1]

OBJECTIVE: We sought to develop a simple point score that would accurately capture the risk of hospital death for patients with acute lung injury (ALI). DESIGN: This is a secondary analysis of data from two randomized trials. Baseline clinical variables collected within 24 hours of enrollment were modeled as predictors of hospital mortality using logistic regression and bootstrap resampling to arrive at a parsimonious model. We constructed a point score based on regression coefficients. SETTING: Medical centers participating in the Acute Respiratory Distress Syndrome Clinical Trials Network (ARDSnet). PATIENTS: Model development: 414 patients with nontraumatic ALI participating in the low tidal volume arm of the ARDSnet Acute Respiratory Management in ARDS study. Model validation: 459 patients participating in the ARDSnet Assessment of Low tidal Volume and elevated End-expiratory volume to Obviate Lung Injury study. Model Validation: 459 patients participating in the ARDSnet Assessment of Low tidal Volume and elevated End-expiratory volume to Obviate Lung Injury trial. INTERVENTIONS: None. MEASUREMENTS AND MAIN RESULTS: Variables comprising the prognostic model were hematocrit <26% (1 point), bilirubin >or=2 mg/dL (1 point), fluid balance >2.5 L positive (1 point), and age (1 point for age 40-64 years, 2 points for age >or=65 years). Predicted mortality (95% confidence interval) for 0, 1, 2, 3, and 4+ point totals was 8% (5% to 14%), 17% (12% to 23%), 31% (26% to 37%), 51% (43% to 58%), and 70% (58% to 80%), respectively. There was an excellent agreement between predicted and observed mortality in the validation cohort. Observed mortality for 0, 1, 2, 3, and 4+ point totals in the validation cohort was 12%, 16%, 28%, 47%, and 67%, respectively. Compared with the Acute Physiology Assessment and Chronic Health Evaluation III score, areas under the receiver operating characteristic curve for the point score were greater in the development cohort (0.72 vs. 0.67, p = 0.09) and lower in the validation cohort (0.68 vs. 0.75, p = 0.03). CONCLUSIONS: Mortality in patients with ALI can be predicted using an index of four readily available clinical variables with good calibration. This index may help inform prognostic discussions, but validation in nonclinical trial populations is necessary before widespread use.
Severe sepsis and septic shock
DOI:10.1056/NEJMra1208623 URL PMID:23984731 [Cited within: 1]
Conservative fluid management or deresuscitation for patients with sepsis or acute respiratory distress syndrome following the resuscitation phase of critical illness: a systematic review and meta-analysis
DOI:10.1007/s00134-016-4573-3
URL
PMID:27734109
[Cited within: 1]

BACKGROUND: It is unknown whether a conservative approach to fluid administration or deresuscitation (active removal of fluid using diuretics or renal replacement therapy) is beneficial following haemodynamic stabilisation of critically ill patients. PURPOSE: To evaluate the efficacy and safety of conservative or deresuscitative fluid strategies in adults and children with acute respiratory distress syndrome (ARDS), sepsis or systemic inflammatory response syndrome (SIRS) in the post-resuscitation phase of critical illness. METHODS: We searched Medline, EMBASE and the Cochrane central register of controlled trials from 1980 to June 2016, and manually reviewed relevant conference proceedings from 2009 to the present. Two reviewers independently assessed search results for inclusion and undertook data extraction and quality appraisal. We included randomised trials comparing fluid regimens with differing fluid balances between groups, and observational studies investigating the relationship between fluid balance and clinical outcomes. RESULTS: Forty-nine studies met the inclusion criteria. Marked clinical heterogeneity was evident. In a meta-analysis of 11 randomised trials (2051 patients) using a random-effects model, we found no significant difference in mortality with conservative or deresuscitative strategies compared with a liberal strategy or usual care [pooled risk ratio (RR) 0.92, 95 % confidence interval (CI) 0.82-1.02, I (2) = 0 %]. A conservative or deresuscitative strategy resulted in increased ventilator-free days (mean difference 1.82 days, 95 % CI 0.53-3.10, I (2) = 9 %) and reduced length of ICU stay (mean difference -1.88 days, 95 % CI -0.12 to -3.64, I (2) = 75 %) compared with a liberal strategy or standard care. CONCLUSIONS: In adults and children with ARDS, sepsis or SIRS, a conservative or deresuscitative fluid strategy results in an increased number of ventilator-free days and a decreased length of ICU stay compared with a liberal strategy or standard care. The effect on mortality remains uncertain. Large randomised trials are needed to determine optimal fluid strategies in critical illness.
Fluid balance in sepsis and septic shock as a determining factor of mortality
DOI:10.1016/j.ajem.2014.11.016
URL
PMID:25483379
[Cited within: 1]

OBJECTIVE: The objective was to assess whether fluid balance had a determinant impact on mortality rate in a cohort of critically ill patients with severe sepsis or septic shock. DESIGN: A prospective and observational study was carried out on an inception cohort. SETTING: The setting was an intensive care unit of a university hospital. PATIENTS: Patients admitted consecutively in the intensive care unit who were diagnosed with severe sepsis or septic shock were included. INTERVENTIONS: Demographic, laboratory, and clinical data were registered, as well as time of septic shock onset, illness severity (Simplified Acute Physiology Score II, Sepsis-related Organ Failure Assessment), and comorbidities. Daily and accumulated fluid balance was registered at 24, 48, 72, and 96 hours. Survival curves representing 28-day mortality were built according to the Kaplan-Meier method. RESULTS: A total of 42 patients were included in the analysis: men, 64.3%; mean age, 61.8+/-15.9 years. Septic shock was predominant in 69% of the cases. Positive blood cultures were obtained in 17 patients (40.5%). No age, sex, Sepsis-related Organ Failure Assessment, creatinine, lactate, venous saturation of O2, and troponin differences were observed upon admission between survivors and nonsurvivors. However, higher Simplified Acute Physiology Score II was observed in nonsurvivors, P=.016. Nonsurvivors also showed higher accumulated positive fluid balance at 48, 72, and 96 hours with statistically significant differences. Besides, significant differences (P=.02) were observed in the survival curve with the risk of mortality at 72 hours between patients with greater than 2.5 L and less than 2.5 L of accumulated fluid balance. CONCLUSIONS: Fluid administration at the onset of severe sepsis or septic shock is the first line of hemodynamic treatment. However, the accumulated positive fluid balance in the first 48, 72, and 96 hours is associated with higher mortality in these critically ill patients.
Negative fluid balance predicts survival in patients with septic shock: a retrospective pilot study
DOI:10.1378/chest.117.6.1749
URL
PMID:10858412
[Cited within: 1]

OBJECTIVE: We hypothesized that patients with septic shock who achieve negative fluid balance (< or =-500 mL) on any day in the first 3 days of management are more likely to survive than those who do not. DESIGN: Retrospective chart review. PATIENTS: Thirty-six patients admitted with the diagnosis of septic shock. SETTING: Twelve-bed medical ICU of a 300-bed community teaching hospital. METHODS: Medical records of 36 patients admitted to our medical ICU over a 21-month period were examined. Patients with septic shock who required dialysis prior to hospitalization were not included. A number of demographic and physiologic variables were extracted from the medical records. Admission APACHE (acute physiology and chronic health evaluation) II and daily sequential organ failure assessment (SOFA) scores were computed from the extracted data. Variables were compared between survivors and nonsurvivors and in patients who did vs those who did not achieve negative (< or = 500 mL) fluid balance in > or = 1 day of the first 3 days of management. Survival risk ratios (RRs) were used as the measure of association between negative fluid balance and survival. RRs were adjusted for age, APACHE II scores, SOFA scores on the first and third days, and the need for mechanical ventilation, by stratified analyses. RESULTS: Patients ranged in age from 16 to 85 years with a mean (+/- SE) age of 67.4 +/- 3.3 years. The mean admission APACHE II score was 25.4 +/- 1.4, and the day 1 SOFA score was 9.0 +/- 0.8. Twenty patients did not survive; nonsurvivors had higher mean APACHE II scores than survivors (29.8 vs 20.4, respectively) and higher first day SOFA scores than survivors (10.8 vs 6.9, respectively), and they were more likely to require vasopressors and mechanical ventilation compared to patients who survived. Whereas all 11 patients who achieved a negative balance of > 500 mL on > or = 1 of the first 3 days of treatment survived, only 5 of 25 patient who failed to achieve a negative fluid balance of > 500 mL by the third day of treatment survived (RR, 5.0; 95% CI, 2.3 to 10.9; p = 0.00001). At least 1 day of net negative fluid balance in the first 3 days of treatment strongly predicted survival across the strata of age, APACHE II scores, first- and third-day SOFA scores, the need for mechanical ventilation, and creatinine levels measured at admission. CONCLUSION: These results suggest that at least 1 day of negative fluid balance (< or = -500 mL) achieved by the third day of treatment may be a good independent predictor of survival in patients with septic shock. These findings suggest the hypothesis
The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
DOI:10.1001/jama.2016.0287
URL
PMID:26903338
[Cited within: 1]

IMPORTANCE: Definitions of sepsis and septic shock were last revised in 2001. Considerable advances have since been made into the pathobiology (changes in organ function, morphology, cell biology, biochemistry, immunology, and circulation), management, and epidemiology of sepsis, suggesting the need for reexamination. OBJECTIVE: To evaluate and, as needed, update definitions for sepsis and septic shock. PROCESS: A task force (n = 19) with expertise in sepsis pathobiology, clinical trials, and epidemiology was convened by the Society of Critical Care Medicine and the European Society of Intensive Care Medicine. Definitions and clinical criteria were generated through meetings, Delphi processes, analysis of electronic health record databases, and voting, followed by circulation to international professional societies, requesting peer review and endorsement (by 31 societies listed in the Acknowledgment). KEY FINDINGS FROM EVIDENCE SYNTHESIS: Limitations of previous definitions included an excessive focus on inflammation, the misleading model that sepsis follows a continuum through severe sepsis to shock, and inadequate specificity and sensitivity of the systemic inflammatory response syndrome (SIRS) criteria. Multiple definitions and terminologies are currently in use for sepsis, septic shock, and organ dysfunction, leading to discrepancies in reported incidence and observed mortality. The task force concluded the term severe sepsis was redundant. RECOMMENDATIONS: Sepsis should be defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. For clinical operationalization, organ dysfunction can be represented by an increase in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score of 2 points or more, which is associated with an in-hospital mortality greater than 10%. Septic shock should be defined as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by a vasopressor requirement to maintain a mean arterial pressure of 65 mm Hg or greater and serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia. This combination is associated with hospital mortality rates greater than 40%. In out-of-hospital, emergency department, or general hospital ward settings, adult patients with suspected infection can be rapidly identified as being more likely to have poor outcomes typical of sepsis if they have at least 2 of the following clinical criteria that together constitute a new bedside clinical score termed quickSOFA (qSOFA): respiratory rate of 22/min or greater, altered mentation, or systolic blood pressure of 100 mm Hg or less. CONCLUSIONS AND RELEVANCE: These updated definitions and clinical criteria should replace previous definitions, offer greater consistency for epidemiologic studies and clinical trials, and facilitate earlier recognition and more timely management of patients with sepsis or at risk of developing sepsis.
Acute respiratory distress syndrome: the Berlin Definition
DOI:10.1001/jama.2012.5669
URL
PMID:22797452
[Cited within: 2]

The acute respiratory distress syndrome (ARDS) was defined in 1994 by the American-European Consensus Conference (AECC); since then, issues regarding the reliability and validity of this definition have emerged. Using a consensus process, a panel of experts convened in 2011 (an initiative of the European Society of Intensive Care Medicine endorsed by the American Thoracic Society and the Society of Critical Care Medicine) developed the Berlin Definition, focusing on feasibility, reliability, validity, and objective evaluation of its performance. A draft definition proposed 3 mutually exclusive categories of ARDS based on degree of hypoxemia: mild (200 mm Hg < PaO2/FIO2 /=10 cm H2O), and corrected expired volume per minute (>/=10 L/min). The draft Berlin Definition was empirically evaluated using patient-level meta-analysis of 4188 patients with ARDS from 4 multicenter clinical data sets and 269 patients with ARDS from 3 single-center data sets containing physiologic information. The 4 ancillary variables did not contribute to the predictive validity of severe ARDS for mortality and were removed from the definition. Using the Berlin Definition, stages of mild, moderate, and severe ARDS were associated with increased mortality (27%; 95% CI, 24%-30%; 32%; 95% CI, 29%-34%; and 45%; 95% CI, 42%-48%, respectively; P < .001) and increased median duration of mechanical ventilation in survivors (5 days; interquartile [IQR], 2-11; 7 days; IQR, 4-14; and 9 days; IQR, 5-17, respectively; P < .001). Compared with the AECC definition, the final Berlin Definition had better predictive validity for mortality, with an area under the receiver operating curve of 0.577 (95% CI, 0.561-0.593) vs 0.536 (95% CI, 0.520-0.553; P < .001). This updated and revised Berlin Definition for ARDS addresses a number of the limitations of the AECC definition. The approach of combining consensus discussions with empirical evaluation may serve as a model to create more accurate, evidence-based, critical illness syndrome definitions and to better inform clinical care, research, and health services planning.
A 12-month clinical survey of incidence and outcome of acute respiratory distress syndrome in Shanghai intensive care units
DOI:10.1007/s00134-004-2479-y
URL
PMID:15650866
[Cited within: 1]

OBJECTIVE: To investigate incidence, causes, and outcome of acute respiratory distress syndrome (ARDS) in adult patients admitted to intensive care units (ICU) in Shanghai. DESIGN: A prospective 12-month survey during 2001-2002 of the predispositions, clinical management strategies, complications, and 90-day survival rates of patients with ARDS. PATIENTS AND SETTING: Fifteen ICU in 12 university hospitals in Shanghai. All ICU admissions >/=15 years of age in the 12-month period were assessed. Patients fulfilling diagnostic criteria of ARDS, as defined by the American-European Consensus Conference, and having a continuous treatment period >/=24 h, were recruited. MEASUREMENTS AND RESULTS: Of 5320 adult patients admitted to ICUs, there were 108 (2%) with ARDS. At inclusion, ARDS patients had a mean PaO(2)/FiO(2) value of 111.3+/-40.3 mmHg and a mean acute physiology and chronic health evaluation score (APACHE II) of 17.3+/-8.0; 33 patients had a lung injury score >2.5. Forty-one and 67 patients had ARDS associated with diseases of pulmonary and extrapulmonary origin, respectively. The most common predisposing factors for ARDS were pneumonia (34.3%) and nonpulmonary sepsis (30.6%). The overall ICU mortality was 10.3%. In-hospital and 90-day mortalities of ARDS patients were 68.5 and 70.4%, respectively, and accounted for 13.5% of the overall ICU mortality. For ARDS patients, multiple organ dysfunction syndrome was a major risk factor associated with death (59.5%). CONCLUSION: The high morbidity and mortality of ARDS in the ICUs in Shanghai require reassessment of respiratory and intensive care management and implementation of effective therapeutic interventions.
Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study
DOI:10.1001/jama.287.3.345
URL
PMID:11790214
[Cited within: 1]

CONTEXT: The outcome of patients receiving mechanical ventilation for particular indications has been studied, but the outcome in a large number of unselected, heterogeneous patients has not been reported. OBJECTIVE: To determine the survival of patients receiving mechanical ventilation and the relative importance of factors influencing survival. DESIGN, SETTING, AND SUBJECTS: Prospective cohort of consecutive adult patients admitted to 361 intensive care units who received mechanical ventilation for more than 12 hours between March 1, 1998, and March 31, 1998. Data were collected on each patient at initiation of mechanical ventilation and daily throughout the course of mechanical ventilation for up to 28 days. MAIN OUTCOME MEASURE: All-cause mortality during intensive care unit stay. RESULTS: Of the 15 757 patients admitted, a total of 5183 (33%) received mechanical ventilation for a mean (SD) duration of 5.9 (7.2) days. The mean (SD) length of stay in the intensive care unit was 11.2 (13.7) days. Overall mortality rate in the intensive care unit was 30.7% (1590 patients) for the entire population, 52% (120) in patients who received ventilation because of acute respiratory distress syndrome, and 22% (115) in patients who received ventilation for an exacerbation of chronic obstructive pulmonary disease. Survival of unselected patients receiving mechanical ventilation for more than 12 hours was 69%. The main conditions independently associated with increased mortality were (1) factors present at the start of mechanical ventilation (odds ratio [OR], 2.98; 95% confidence interval [CI], 2.44-3.63; P<.001 for coma), (2) factors related to patient management (OR, 3.67; 95% CI, 2.02-6.66; P<.001 for plateau airway pressure >35 cm H(2)O), and (3) developments occurring over the course of mechanical ventilation (OR, 8.71; 95% CI, 5.44-13.94; P<.001 for ratio of PaO(2) to fraction of inspired oxygen <100). CONCLUSION: Survival among mechanically ventilated patients depends not only on the factors present at the start of mechanical ventilation, but also on the development of complications and patient management in the intensive care unit.
Sepsis and acute respiratory distress syndrome: recent update
DOI:10.4046/trd.2016.79.2.53 URL [Cited within: 1]
The importance of fluid management in acute lung injury secondary to septic shock
DOI:10.1378/chest.08-2706
URL
PMID:19318675
[Cited within: 1]

BACKGROUND: Recent studies have suggested that early goal-directed resuscitation of patients with septic shock and conservative fluid management of patients with acute lung injury (ALI) can improve outcomes. Because these may be seen as potentially conflicting practices, we set out to determine the influence of fluid management on the outcomes of patients with septic shock complicated by ALI. METHODS: A retrospective analysis was performed at Barnes-Jewish Hospital (St. Louis, MO) and in the medical ICU of Mayo Medical Center (Rochester, MN). Patients hospitalized with septic shock were enrolled into the study if they met the American-European Consensus definition of ALI within 72 h of septic shock onset. Adequate initial fluid resuscitation (AIFR) was defined as the administration of an initial fluid bolus of >or= 20 mL/kg prior to and achievement of a central venous pressure of >or= 8 mm Hg within 6 h after the onset of therapy with vasopressors. Conservative late fluid management (CLFM) was defined as even-to-negative fluid balance measured on at least 2 consecutive days during the first 7 days after septic shock onset. RESULTS: The study cohort was made up of 212 patients with ALI complicating septic shock. Hospital mortality was statistically lowest for those achieving both AIFR and CLFM and higher for those achieving only CLFM, those achieving only AIFR, and those achieving neither (17 of 93 patients [18.3%] vs 13 of 31 patients [41.9%] vs 30 of 53 patients [56.6%] vs 27 of 35 [77.1%], respectively; p < 0.001). CONCLUSIONS: Both early and late fluid management of septic shock complicated by ALI can influence patient outcomes.
Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome
DOI:10.1056/NEJM199802053380602
URL
PMID:9449727
[Cited within: 1]

BACKGROUND: In patients with the acute respiratory distress syndrome, massive alveolar collapse and cyclic lung reopening and overdistention during mechanical ventilation may perpetuate alveolar injury. We determined whether a ventilatory strategy designed to minimize such lung injuries could reduce not only pulmonary complications but also mortality at 28 days in patients with the acute respiratory distress syndrome. METHODS: We randomly assigned 53 patients with early acute respiratory distress syndrome (including 28 described previously), all of whom were receiving identical hemodynamic and general support, to conventional or protective mechanical ventilation. Conventional ventilation was based on the strategy of maintaining the lowest positive end-expiratory pressure (PEEP) for acceptable oxygenation, with a tidal volume of 12 ml per kilogram of body weight and normal arterial carbon dioxide levels (35 to 38 mm Hg). Protective ventilation involved end-expiratory pressures above the lower inflection point on the static pressure-volume curve, a tidal volume of less than 6 ml per kilogram, driving pressures of less than 20 cm of water above the PEEP value, permissive hypercapnia, and preferential use of pressure-limited ventilatory modes. RESULTS: After 28 days, 11 of 29 patients (38 percent) in the protective-ventilation group had died, as compared with 17 of 24 (71 percent) in the conventional-ventilation group (P<0.001). The rates of weaning from mechanical ventilation were 66 percent in the protective-ventilation group and 29 percent in the conventional-ventilation group (P=0.005): the rates of clinical barotrauma were 7 percent and 42 percent, respectively (P=0.02), despite the use of higher PEEP and mean airway pressures in the protective-ventilation group. The difference in survival to hospital discharge was not significant; 13 of 29 patients (45 percent) in the protective-ventilation group died in the hospital, as compared with 17 of 24 in the conventional-ventilation group (71 percent, P=0.37). CONCLUSIONS: As compared with conventional ventilation, the protective strategy was associated with improved survival at 28 days, a higher rate of weaning from mechanical ventilation, and a lower rate of barotrauma in patients with the acute respiratory distress syndrome. Protective ventilation was not associated with a higher rate of survival to hospital discharge.
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome
DOI:10.1056/NEJM200005043421801
URL
PMID:10793162
[Cited within: 1]

BACKGROUND: Traditional approaches to mechanical ventilation use tidal volumes of 10 to 15 ml per kilogram of body weight and may cause stretch-induced lung injury in patients with acute lung injury and the acute respiratory distress syndrome. We therefore conducted a trial to determine whether ventilation with lower tidal volumes would improve the clinical outcomes in these patients. METHODS: Patients with acute lung injury and the acute respiratory distress syndrome were enrolled in a multicenter, randomized trial. The trial compared traditional ventilation treatment, which involved an initial tidal volume of 12 ml per kilogram of predicted body weight and an airway pressure measured after a 0.5-second pause at the end of inspiration (plateau pressure) of 50 cm of water or less, with ventilation with a lower tidal volume, which involved an initial tidal volume of 6 ml per kilogram of predicted body weight and a plateau pressure of 30 cm of water or less. The primary outcomes were death before a patient was discharged home and was breathing without assistance and the number of days without ventilator use from day 1 to day 28. RESULTS: The trial was stopped after the enrollment of 861 patients because mortality was lower in the group treated with lower tidal volumes than in the group treated with traditional tidal volumes (31.0 percent vs. 39.8 percent, P=0.007), and the number of days without ventilator use during the first 28 days after randomization was greater in this group (mean [+/-SD], 12+/-11 vs. 10+/-11; P=0.007). The mean tidal volumes on days 1 to 3 were 6.2+/-0.8 and 11.8+/-0.8 ml per kilogram of predicted body weight (P<0.001), respectively, and the mean plateau pressures were 25+/-6 and 33+/-8 cm of water (P<0.001), respectively. CONCLUSIONS: In patients with acute lung injury and the acute respiratory distress syndrome, mechanical ventilation with a lower tidal volume than is traditionally used results in decreased mortality and increases the number of days without ventilator use.
A high positive end-expiratory pressure, low tidal volume ventilatory strategy improves outcome in persistent acute respiratory distress syndrome: a randomized, controlled trial
DOI:10.1097/01.CCM.0000215598.84885.01
URL
PMID:16557151
[Cited within: 1]

OBJECTIVE: It has been shown in a two-center study that high positive end-expiratory pressure (PEEP) and low tidal volume (LTV) improved outcome in ARDS. However, that study involved patients with underlying diseases unique to the study area, was conducted at only two centers, and enrolled a small number of patients. We similarly hypothesized that a ventilatory strategy based on PEEP above the lower inflection point of the pressure volume curve of the respiratory system (Pflex) set on day 1 with a low tidal volume would result in improved outcome in patients with severe and persistent acute respiratory distress syndrome (ARDS). DESIGN: Randomized, controlled clinical trial. SETTING: Network of eight Spanish multidisciplinary intensive care units (ICUs) under the acronym of ARIES (Acute Respiratory Insufficiency: Espana Study). PATIENTS: All consecutive patients admitted into participating Spanish ICUs from March 1999 to March 2001 with a diagnosis of ARDS were considered for the study. If 24 hrs after meeting ARDS criteria, the Pao2/Fio2 remained < or =200 mm Hg on standard ventilator settings, patients were randomized into two groups: control and Pflex/LTV. INTERVENTIONS: In the control group, tidal volume was 9-11 mL/kg of predicted body weight (PBW) and PEEP > or =5 cm H2O. In the Pflex/LTV group, tidal volume was 5-8 mL/kg PBW and PEEP was set on day 1 at Pflex + 2 cm H2O. In both groups, Fio2 was set to maintain arterial oxygen saturation >90% and Pao2 70-100 mm Hg, and respiratory rate was adjusted to maintain Paco2 between 35 and 50 mm Hg. MEASUREMENTS AND MAIN RESULTS: The study was stopped early based on an efficacy stopping rule as described in the methods. Of 103 patients who were enrolled (50 control and 53 Pflex), eight patients (five in control, three in Pflex) were excluded from the final evaluation because the random group assignment was not performed in one center according to protocol. Main outcome measures were ICU and hospital mortality, ventilator-free days, and nonpulmonary organ dysfunction. ICU mortality (24 of 45 [53.3%] vs. 16 of 50 [32%], p = .040), hospital mortality (25 of 45 [55.5%] vs. 17 of 50 [34%], p = .041), and ventilator-free days at day 28 (6.02 +/- 7.95 in control and 10.90 +/- 9.45 in Pflex/LTV, p = .008) all favored Pflex/LTV. The mean difference in the number of additional organ failures postrandomization was higher in the control group (p < .001). CONCLUSIONS: A mechanical ventilation strategy with a PEEP level set on day 1 above Pflex and a low tidal volume compared with a strategy with a higher tidal volume and relatively low PEEP has a beneficial impact on outcome in patients with severe and persistent ARDS.
Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study
DOI:10.1097/00003246-199422100-00011
URL
PMID:7924367
[Cited within: 1]

OBJECTIVES: To evaluate the outcome in patients with severe adult respiratory distress syndrome (ARDS) managed with limitation of peak inspiratory pressure to 30 to 40 cm H2O, low tidal volumes (4 to 7 mL/kg), spontaneous breathing using synchronized intermittent mandatory ventilation from the start of ventilation, and permissive hypercapnia without the use of bicarbonate to buffer acidosis. Also, to compare hospital mortality rate with that predicted by the Acute Physiology and Chronic Health Evaluation (APACHE) II scoring system and the
Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome
DOI:10.1007/BF01735174
URL
PMID:2246418
[Cited within: 1]

Many animal studies have shown that high peak inspiratory pressures (PIP) during mechanical ventilation can induce acute lung injury with hyaline membranes. Since 1984 we have limited PIP in patients with ARDS by reducing tidal volume, allowing spontaneous breathing with SIMV and disregarding hypercapnia. Since 1987 50 patients with severe ARDS with a
Mechanical ventilation
DOI:10.1378/chest.104.6.1833 URL PMID:8252973 [Cited within: 1]
Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome
DOI:10.1056/NEJM199802053380603
URL
PMID:9449728
[Cited within: 1]

BACKGROUND: A strategy of mechanical ventilation that limits airway pressure and tidal volume while permitting hypercapnia has been recommended for patients with the acute respiratory distress syndrome. The goal is to reduce lung injury due to overdistention. However, the efficacy of this approach has not been established. METHODS: Within 24 hours of intubation, patients at high risk for the acute respiratory distress syndrome were randomly assigned to either pressure- and volume-limited ventilation (limited-ventilation group), with the peak inspiratory pressure maintained at 30 cm of water or less and the tidal volume at 8 ml per kilogram of body weight or less, or to conventional ventilation (control group), with the peak inspiratory pressure allowed to rise as high as 50 cm of water and the tidal volume at 10 to 15 ml per kilogram. All other ventilatory variables were similar in the two groups. RESULTS: A total of 120 patients with similar clinical features underwent randomization (60 in each group). The patients in the limited-ventilation and control groups were exposed to different mean (+/-SD) tidal volumes (7.2+/-0.8 vs. 10.8+/-1.0 ml per kilogram, respectively; P<0.001) and peak inspiratory pressures (23.6+/-5.8 vs. 34.0+/-11.0 cm of water, P<0.001). Mortality was 50 percent in the limited-ventilation group and 47 percent in the control group (relative risk, 1.07; 95 percent confidence interval, 0.72 to 1.57; P=0.72). In the limited-ventilation group, permissive hypercapnia (arterial carbon dioxide tension, >50 mm Hg) was more common (52 percent vs. 28 percent, P=0.009), more marked (54.4+/-18.8 vs. 45.7+/-9.8 mm Hg, P=0.002), and more prolonged (146+/-265 vs. 25+/-22 hours, P=0.017) than in the control group. The incidence of barotrauma, the highest multiple-organ-dysfunction score, and the number of episodes of organ failure were similar in the two groups; however, the numbers of patients who required paralytic agents (23 vs. 13, P=0.05) and dialysis for renal failure (13 vs. 5, P= 0.04) were greater in the limited-ventilation group than in the control group. CONCLUSIONS: In patients at high risk for the acute respiratory distress syndrome, a strategy of mechanical ventilation that limits peak inspiratory pressure and tidal volume does not appear to reduce mortality and may increase morbidity.
Higher vs. lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis
DOI:10.1001/jama.2010.218
URL
PMID:20197533
[Cited within: 1]

CONTEXT: Trials comparing higher vs lower levels of positive end-expiratory pressure (PEEP) in adults with acute lung injury or acute respiratory distress syndrome (ARDS) have been underpowered to detect small but potentially important effects on mortality or to explore subgroup differences. OBJECTIVES: To evaluate the association of higher vs lower PEEP with patient-important outcomes in adults with acute lung injury or ARDS who are receiving ventilation with low tidal volumes and to investigate whether these associations differ across prespecified subgroups. DATA SOURCES: Search of MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials (1996-January 2010) plus a hand search of conference proceedings (2004-January 2010). STUDY SELECTION: Two reviewers independently screened articles to identify studies randomly assigning adults with acute lung injury or ARDS to treatment with higher vs lower PEEP (with low tidal volume ventilation) and also reporting mortality. DATA EXTRACTION: Data from 2299 individual patients in 3 trials were analyzed using uniform outcome definitions. Prespecified effect modifiers were tested using multivariable hierarchical regression, adjusting for important prognostic factors and clustering effects. RESULTS: There were 374 hospital deaths in 1136 patients (32.9%) assigned to treatment with higher PEEP and 409 hospital deaths in 1163 patients (35.2%) assigned to lower PEEP (adjusted relative risk [RR], 0.94; 95% confidence interval [CI], 0.86-1.04; P = .25). Treatment effects varied with the presence or absence of ARDS, defined by a value of 200 mm Hg or less for the ratio of partial pressure of oxygen to fraction of inspired oxygen concentration (P = .02 for interaction). In patients with ARDS (n = 1892), there were 324 hospital deaths (34.1%) in the higher PEEP group and 368 (39.1%) in the lower PEEP group (adjusted RR, 0.90; 95% CI, 0.81-1.00; P = .049); in patients without ARDS (n = 404), there were 50 hospital deaths (27.2%) in the higher PEEP group and 44 (19.4%) in the lower PEEP group (adjusted RR, 1.37; 95% CI, 0.98-1.92; P = .07). Rates of pneumothorax and vasopressor use were similar. CONCLUSIONS: Treatment with higher vs lower levels of PEEP was not associated with improved hospital survival. However, higher levels were associated with improved survival among the subgroup of patients with ARDS.
Early acute kidney injury and sepsis: a multicentre evaluation
DOI:10.1186/cc6863
URL
PMID:18402655
[Cited within: 1]

INTRODUCTION: We conducted a study to evaluate the incidence, risk factors and outcomes associated with early acute kidney injury (AKI) in sepsis. METHODS: The study was a retrospective interrogation of prospectively collected data from the Australian New Zealand Intensive Care Society Adult Patient Database. Data were collected from 57 intensive care units (ICUs) across Australia. In total, 120,123 patients admitted to ICU for more than 24 hours from 1 January 2000 to 31 December 2005 were included in the analysis. The main outcome measures were clinical and laboratory data and outcomes. RESULTS: Of 120,123 patients admitted, 33,375 had a sepsis-related diagnosis (27.8%). Among septic patients, 14,039 (42.1%) had concomitant AKI (septic AKI). Sepsis accounted for 32.4% of all patients with AKI. For septic AKI stratified by RIFLE (risk of renal failure, injury to the kidney, failure of kidney function, loss of kidney function and end-stage kidney disease) category, 38.5% of patients belonged to the risk category, 38.8% to the injury category and 22.7% to the failure category. Septic AKI patients had greater acuity of illness (P < 0.0001), lower blood pressure (P < 0.0001), higher heart rates (P < 0.0001), worse pulmonary function measures by arterial oxygen tension/fraction of inspired oxygen ratio (P < 0.0001), greater acidaemia (P < 0.0001) and higher white cell counts (P < 0.0001) compared with patients with nonseptic AKI. Septic AKI was also associated with greater severity of AKI (RIFLE category injury or failure) compared with nonseptic AKI. Septic AKI was associated with a significantly higher crude and co-variate adjusted mortality in the ICU (19.8% versus 13.4%; odds ratio 1.60, 95% confidence interval 1.5 to 1.7; P < 0.001) and in hospital (29.7% versus 21.6%; odds ratio 1.53, 95% confidence interval 1.46 to 1.60; P < 0.001) compared with nonseptic AKI. Septic AKI was associated with higher ICU and hospital mortality across all strata of RIFLE categories. Septic AKI patients had longer durations of stay in both ICU and hospital across all strata of RIFLE categories. CONCLUSION: Septic AKI is common during the first 24 hours after ICU admission. Patients with septic AKI are generally sicker, with a higher burden of illness, and have greater abnormalities in acute physiology compared with patients with nonseptic AKI. Moreover, septic AKI is independently associated with higher odds of death and longer duration of hospitalization.
Sepsis-associated AKI
DOI:10.2215/CJN.07310717 URL PMID:29070523 [Cited within: 1]