World Journal of Emergency Medicine ›› 2024, Vol. 15 ›› Issue (6): 465-474.doi: 10.5847/wjem.j.1920-8642.2024.096
• Original Articles • Previous Articles Next Articles
Yaowen Liang1,2, Guoxiang Zou1, Dingchen Wang1,3, Weiyue Zeng1,3, Jiarui Zhang1,3, Xiaoran Huang1, Miao Lin4, Cong Mai3,5, Fei'er Song1, Yuelin Zhang1, Jinxiu Meng1, Hongliang Feng6( ), Yu Huang7(
), Yu Huang7( ), Xin Li1,2(
), Xin Li1,2( )
)
Received:2024-02-02
Accepted:2024-06-20
Online:2024-11-21
Published:2024-11-01
Contact:
Xin Li, Email: Yaowen Liang, Guoxiang Zou, Dingchen Wang, Weiyue Zeng, Jiarui Zhang, Xiaoran Huang, Miao Lin, Cong Mai, Fei'er Song, Yuelin Zhang, Jinxiu Meng, Hongliang Feng, Yu Huang, Xin Li. Association of alcohol consumption with aortic aneurysm and dissection risk: results from the UK Biobank cohort study[J]. World Journal of Emergency Medicine, 2024, 15(6): 465-474.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2024.096
Table 1.
Baseline characteristics stratified by alcohol consumption
| Characteristics | Overall (n=388,955) | Never-drinkers (n=19,999) | Former-drinkers (n=16,717) | Mild drinkers (n=157,188) | Moderate drinkers (n=106,554) | Moderate-heavy drinkers (n=47,627) | Heavy drinkers (n=40,870) | P-value |
|---|---|---|---|---|---|---|---|---|
| Age, years < 65 years ≥ 65 years | 57.1 ± 8.1 81.0 19.0 | 57.0 ± 8.6 75.8 24.2 | 57.18 ± 7.9 79.1 20.9 | 56.5 ± 8.1 80.8 19.2 | 56.5 ± 8.0 81.5 18.5 | 56.5 ± 7.9 82.3 17.7 | 56.5 ± 7.8 82.5 17.5 | <0.001 |
| Sex, % Female Male | 52.6 47.4 | 72.1 27.9 | 55.7 44.3 | 63.7 36.3 | 48.4 51.6 | 36.5 63.5 | 25.7 74.3 | <0.001 |
| Ethnicity, % Not white White | 5.2 94.8 | 29.5 70.5 | 8.1 91.9 | 5.3 94.7 | 2.5 97.5 | 2.0 98.0 | 1.8 98.2 | <0.001 |
| Townsend deprivation index | -1.4 ± 3.0 | -0.3 ± 3.4 | -0.1 ± 3.5 | -1.5 ± 2.9 | -1.7 ± 2.9 | -1.6 ± 2.9 | -1.3 ± 3.0 | <0.001 |
| Education level, % No qualification Any other qualification College degree or above | 15.8 49.8 34.4 | 26.9 46.5 26.6 | 26.9 46.9 26.2 | 15.8 50.8 33.4 | 13.9 49.3 36.8 | 13.0 49.6 37.4 | 14.2 50.6 35.1 | <0.001 |
| Smoking status, % Never smokers Former/current smokers | 54.4 45.6 | 81.9 18.1 | 44.6 55.4 | 62.1 37.9 | 51.5 48.5 | 42.0 58.0 | 34.3 65.7 | <0.001 |
| Regular physical activity, % No Yes | 33.3 66.7 | 44.6 55.4 | 30.6 69.4 | 33.8 66.2 | 30.8 69.2 | 30.1 69.9 | 31.8 68.2 | <0.001 |
| Systolic blood pressure, mmHg | 139.8 ± 19.6 | 139.2 ± 20.4 | 137.7 ± 19.9 | 138.5 ± 19.7 | 139.8 ± 19.3 | 141.9 ± 19.1 | 144.6 ± 19.2 | <0.001 |
| Diastolic blood pressure, mmHg | 82.2 ± 10.6 | 81.3 ± 10.8 | 80.7 ± 10.8 | 81.3 ± 10.6 | 82.3 ± 10.5 | 83.7 ± 10.6 | 85.4 ± 10.5 | <0.001 |
| Body mass index, kg/m2 < 25 kg/m2, % ≥ 25 to <30 kg/m2, % ≥ 30 kg/m2, % | 27.2 ± 4.6 34.1 43.2 22.7 | 28.1 ± 5.6 31.1 38.3 30.6 | 28.2 ± 5.7 30.6 37.9 31.5 | 27.1 ± 4.7 36.6 41.0 22.4 | 26.9 ± 4.3 35.5 44.6 19.9 | 27.2 ± 4.2 31.2 47.0 21.8 | 27.7 ± 4.2 26.2 48.8 25.0 | <0.001 |
| Cholesterol-lowering medication use, % No Yes | 90.1 9.9 | 87.5 12.5 | 88.4 11.6 | 90.3 9.7 | 90.9 9.1 | 90.3 9.7 | 89.2 10.8 | <0.001 |
| Baseline CVD, % No Yes | 94.5 5.5 | 92.3 7.7 | 89.3 10.7 | 95.2 4.8 | 94.9 5.1 | 94.6 5.4 | 94.0 6.0 | <0.001 |
| Baseline diabetes, % No Yes | 95.2 4.8 | 89.8 10.2 | 89.4 10.6 | 95.4 4.6 | 96.2 3.8 | 96.1 3.9 | 95.6 4.4 | <0.001 |
Table 2.
Associations of weekly alcohol consumption with hazard of aortic aneurysm and dissection (AAD)
| Alcohol consumption | AAD events/N | Person-year | Model 1 HR (95%CI) | Model 2 HR (95%CI) |
|---|---|---|---|---|
| Never-drinkers | 106/19,999 | 246,484 | ref | ref |
| Former-drinkers | 178/16,717 | 201,296 | 1.257 (0.986-1.603) | 1.155 (0.904-1.475) |
| Mild drinkers | 981/157,188 | 1,932,136 | 0.904 (0.739-1.106) | 0.922 (0.751-1.132) |
| Moderate drinkers | 764/106,554 | 1,328,554 | 0.777 (0.632-0.954)* | 0.797 (0.646-0.984)* |
| Moderate-heavy drinkers | 405/47,627 | 592,064 | 0.773 (0.621-0.961)* | 0.794 (0.635-0.992)* |
| Heavy drinkers | 461/40,870 | 503,742 | 0.886 (0.713-1.100) | 0.891 (0.713-1.112) |
| P for trend | 0.018 | 0.041 |
Figure 2.
Associations of alcohol consumption with hazard of aortic aneurysm and dissection (AAD) stratified by age and sex. HR were adjusted for age, sex, smoking status, ethnicity, Townsend deprivation index, education level, physical activity, systolic blood pressure, diastolic blood pressure, body mass index, cholesterol-lowering medication use, baseline diabetes, and baseline cardiovascular disease. HR: hazard ratio; CI: confidence interval; ref: reference.
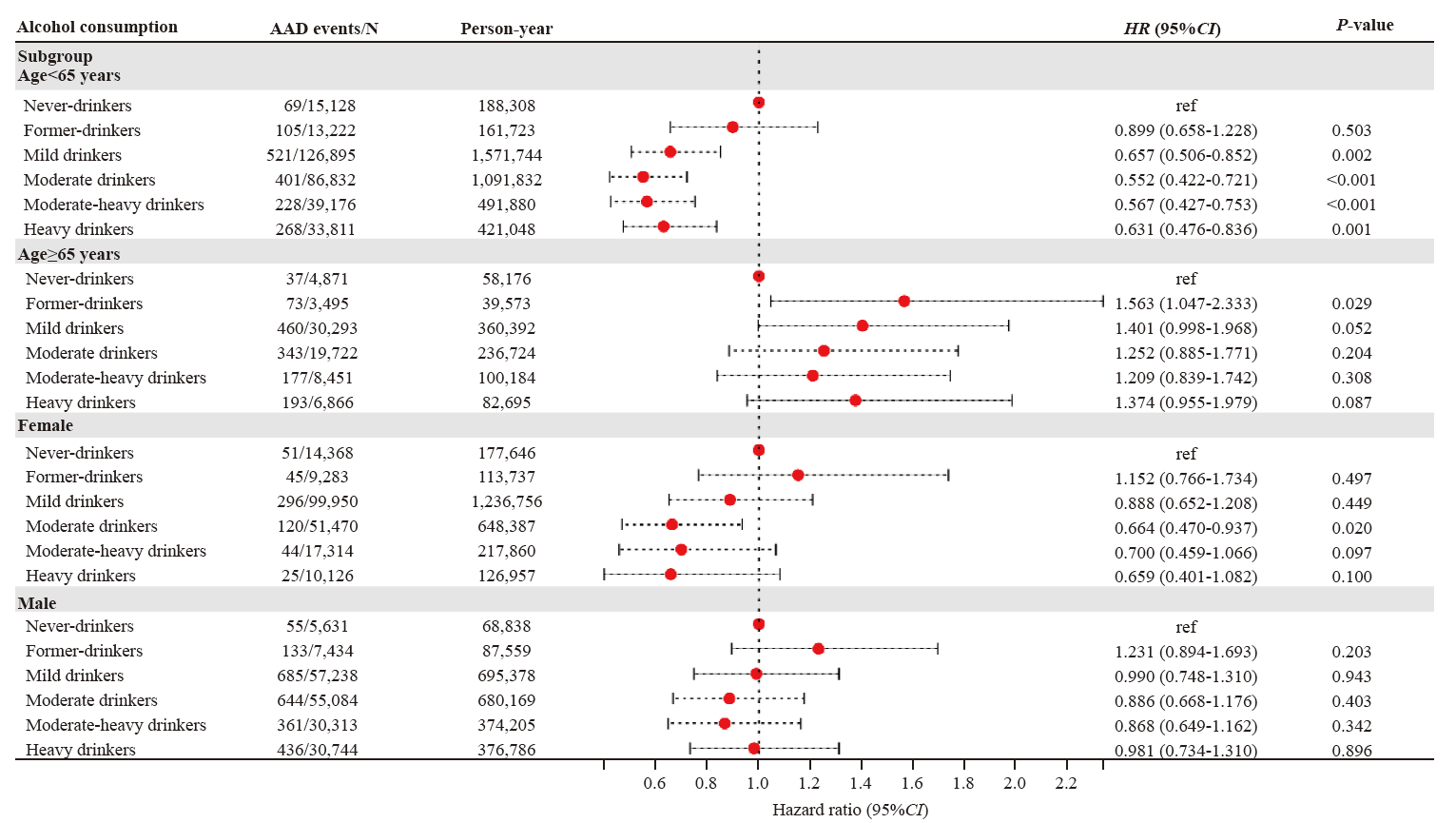

Figure 3.
Dose-response hazard ratio of aortic aneurysm and dissection by alcohol consumption (g/week). Data were fitted with the use of a Cox proportional hazards model with restricted cubic splines with 3 knots (10th, 50th, 90th). Estimates were adjusted for the same variables as in model 2 in Table 2. Shaded areas represent 95% confidence intervals. A: for all participants; B: for current drinkers; C: for participants < 65 years; D: for participants ≥65 years; E: for females; F: for males.

Table 3.
Associations of GSCAN of alcohol consumption with hazard of aortic aneurysm and dissection
| GRS of alcohol consumption | AAD events/N | Person-year | Model 2 HR (95%CI) |
|---|---|---|---|
| Low GRS | 996/129,538 | 1,597,650 | ref |
| Intermediate GRS | 911/129,925 | 1,604,955 | 0.883 (0.807-0.966)** |
| High GRS | 988/129,492 | 1,620,818 | 0.952 (0.871-1.040) |
| P for trend | 0.281 |
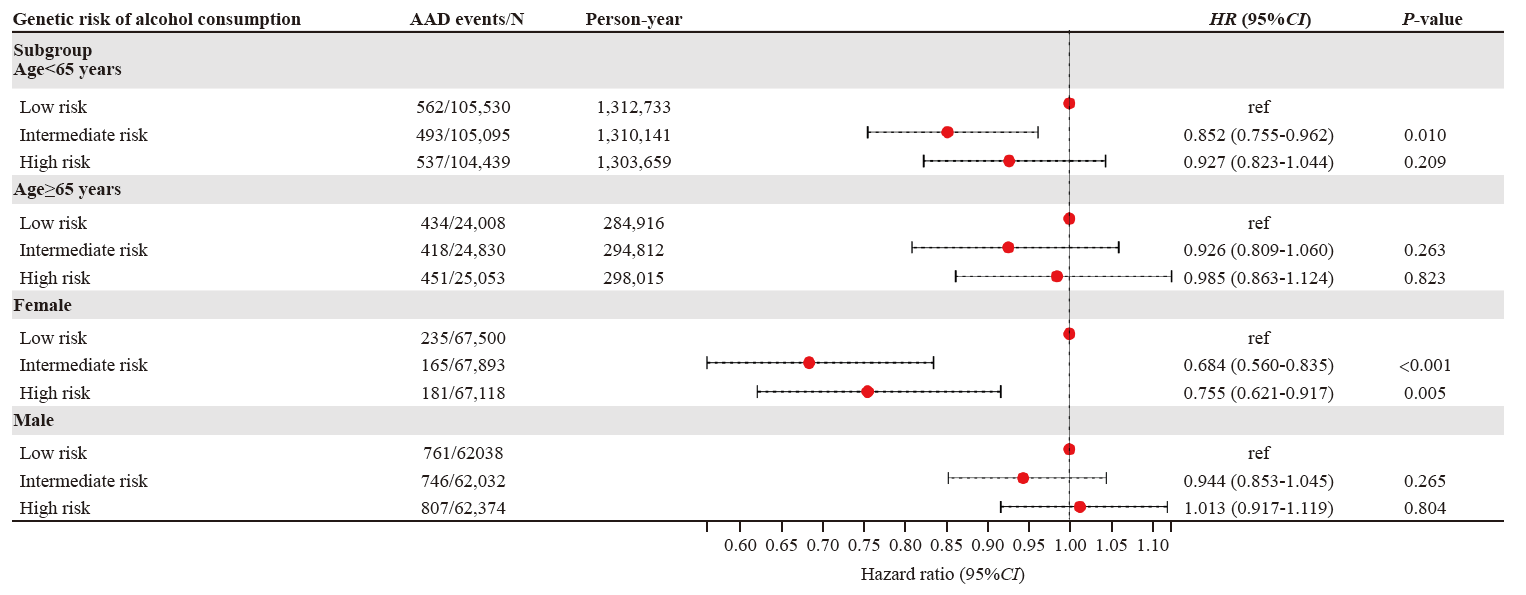
Figure 4.
Associations of genetic risk score (GRS) with hazard of aortic aneurysm and dissection (AAD) stratified by age and sex. HR were adjusted for age, sex, smoking status, ethnicity, Townsend deprivation index, education level, physical activity, systolic blood pressure, diastolic blood pressure, body mass index, cholesterol-lowering medication use, baseline diabetes, and baseline cardiovascular disease. HR: hazard ratio; CI: confidence interval; ref: reference.
| [1] | Gao J, Cao H, Hu G, Wu Y, Xu Y, Cui H, et al. The mechanism and therapy of aortic aneurysms. Signal Transduct Target Ther. 2023; 8(1):55. |
| [2] |
Bossone E, Eagle KA. Epidemiology and management of aortic disease: aortic aneurysms and acute aortic syndromes. Nat Rev Cardiol. 2021; 18(5): 331-48.
doi: 10.1038/s41569-020-00472-6 pmid: 33353985 |
| [3] | Gouveia E Melo R, Silva Duarte G, Lopes A, Alves M, Caldeira D, Fernandes E Fernandes R, et al. Incidence and prevalence of thoracic aortic aneurysms: a systematic review and meta-analysis of population-based studies. Semin Thorac Cardiovasc Surg. 2022; 34(1): 1-16. |
| [4] | McFarlane MJ. The epidemiologic necropsy for abdominal aortic aneurysm. JAMA. 1991; 265(16): 2085-8. |
| [5] |
Sakalihasan N, Limet R, Defawe OD. Abdominal aortic aneurysm. Lancet. 2005; 365(9470): 1577-89.
doi: 10.1016/S0140-6736(05)66459-8 pmid: 15866312 |
| [6] |
Sampson UK, Norman PE, Fowkes FG, Aboyans V, Yanna Song, Harrell FE Jr, et al. Global and regional burden of aortic dissection and aneurysms: mortality trends in 21 world regions, 1990 to 2010. Glob Heart. 2014; 9(1): 171-80.e10.
doi: 10.1016/j.gheart.2013.12.010 pmid: 25432126 |
| [7] |
Svensjö S, Björck M, Gürtelschmid M, Djavani Gidlund K, Hellberg A, Wanhainen A. Low prevalence of abdominal aortic aneurysm among 65-year-old Swedish men indicates a change in the epidemiology of the disease. Circulation. 2011; 124(10): 1118-23.
doi: 10.1161/CIRCULATIONAHA.111.030379 pmid: 21844079 |
| [8] | Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, et al. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ Clin Res Ed. 2017;356: j909. |
| [9] | Ding CY, O’Neill D, Bell S, Stamatakis E, Britton A. Association of alcohol consumption with morbidity and mortality in patients with cardiovascular disease: original data and meta-analysis of 48, 423 men and women. BMC Med. 2021; 19(1): 167. |
| [10] | Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342: d671. |
| [11] |
Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet. 2019; 393(10183): 1831-42.
doi: S0140-6736(18)31772-0 pmid: 30955975 |
| [12] | Wong DR, Willett WC, Rimm EB. Smoking, hypertension, alcohol consumption, and risk of abdominal aortic aneurysm in men.Am J Epidemiol. 2007; 165(7): 838-45. |
| [13] |
Stackelberg O, Björck M, Larsson SC, Orsini N, Wolk A. Alcohol consumption, specific alcoholic beverages, and abdominal aortic aneurysm. Circulation. 2014; 130(8): 646-52.
doi: 10.1161/CIRCULATIONAHA.113.008279 pmid: 24965567 |
| [14] |
Spencer SM, Trower AJ, Jia X, Scott DJA, Greenwood DC. Meta-analysis of the association between alcohol consumption and abdominal aortic aneurysm. Br J Surg. 2017; 104(13): 1756-64.
doi: 10.1002/bjs.10674 pmid: 28880391 |
| [15] | Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015; 12(3): e1001779. |
| [16] |
Mindell J, Biddulph JP, Hirani V, Stamatakis E, Craig R, Nunn S, et al. Cohort profile: the health survey for England. Int J Epidemiol. 2012; 41(6): 1585-93.
doi: 10.1093/ije/dyr199 pmid: 22253315 |
| [17] |
Gray L, Batty GD, Craig P, Stewart C, Whyte B, Finlayson A, et al. Cohort profile: the Scottish health surveys cohort: linkage of study participants to routinely collected records for mortality, hospital discharge, cancer and offspring birth characteristics in three nationwide studies. Int J Epidemiol. 2010; 39(2): 345-50.
doi: 10.1093/ije/dyp155 pmid: 19349480 |
| [18] | Knott CS, Coombs N, Stamatakis E, Biddulph JP. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ. 2015;350: h384. |
| [19] |
Liu MZ, Jiang Y, Wedow R, Li Y, Brazel DM, Chen F, et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat Genet. 2019; 51(2): 237-44.
doi: 10.1038/s41588-018-0307-5 pmid: 30643251 |
| [20] | Lloyd-Jones DM, Hong YL, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010; 121(4): 586-613. |
| [21] | Kuitunen I, Ponkilainen VT, Uimonen MM, Eskelinen A, Reito A. Testing the proportional hazards assumption in cox regression and dealing with possible non-proportionality in total joint arthroplasty research: methodological perspectives and review. BMC Musculoskelet Disord. 2021; 22(1): 489. |
| [22] | GBD 2020 Alcohol Collaborators. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the Global Burden of Disease Study 2020. Lancet. 2022; 400(10347): 185-235. |
| [23] | Castaldo L, Narváez A, Izzo L, Graziani G, Gaspari A, Minno GD, et al. Red wine consumption and cardiovascular health. Molecules. 2019; 24(19): 3626. |
| [24] |
Goldberg IJ, Mosca L, Piano MR, Fisher EA. AHA Science Advisory. Wine and your heart: a science advisory for healthcare professionals from the Nutrition Committee, Council on Epidemiology and Prevention, and Council on Cardiovascular Nursing of the American Heart Association. Stroke. 2001; 32(2): 591-4.
pmid: 11157206 |
| [25] | GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018; 392(10152):1015-35. |
| [26] | Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342: d636. |
| [27] | Rimm EB, Williams P, Fosher K, Criqui M, Stampfer MJ. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. BMJ. 1999; 319(7224): 1523-8. |
| [28] |
Tao WY, Hong YM, He HW, Han Q, Mao MM, Hu B, et al. MicroRNA-199a-5p aggravates angiotensin II-induced vascular smooth muscle cell senescence by targeting Sirtuin-1 in abdominal aortic aneurysm. J Cell Mol Med. 2021; 25(13): 6056-69.
doi: 10.1111/jcmm.16485 pmid: 34132029 |
| [29] |
Björck M, Wanhainen A. Pathophysiology of AAA: heredity vs environment. Prog Cardiovasc Dis. 2013; 56(1): 2-6.
doi: 10.1016/j.pcad.2013.05.003 pmid: 23993232 |
| [30] |
Shah PK. Inflammation, metalloproteinases, and increased proteolysis. Circulation. 1997; 96(7): 2115-7.
pmid: 9337176 |
| [31] | Adorni MP, Palumbo M, Marchi C, Zimetti F, Ossoli A, Turri M, et al. HDL metabolism and functions impacting on cell cholesterol homeostasis are specifically altered in patients with abdominal aortic aneurysm. Front Immunol. 2022;13: 935241. |
| [32] |
Mezue K, Osborne MT, Abohashem S, Zureigat H, Gharios C, Grewal SS, et al. Reduced stress-related neural network activity mediates the effect of alcohol on cardiovascular risk. J Am Coll Cardiol. 2023; 81(24):2315-25.
doi: 10.1016/j.jacc.2023.04.015 pmid: 37316112 |
| [33] |
Batelaan NM, Seldenrijk A, Bot M, van Balkom AJLM, Penninx BWJH. Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. Br J Psychiatry. 2016; 208(3): 223-31.
doi: 10.1192/bjp.bp.114.156554 pmid: 26932485 |
| [34] | Nakada S, Ho FK, Celis-Morales C, Jackson CA, Pell JP. Individual and joint associations of anxiety disorder and depression with cardiovascular disease: a UK Biobank prospective cohort study. Eur Psychiatry. 2023; 66(1): e54. |
| [35] | Im PK, Wright N, Yang L, Chan KH, Chen YP, Guo Y, et al. Alcohol consumption and risks of more than 200 diseases in Chinese men. Nat Med. 2023; 29(6): 1476-86. |
| [36] |
Smyth A, Teo KK, Rangarajan S, O’Donnell M, Zhang X; PURE Investigators, et al. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: a prospective cohort study. Lancet. 2015; 386(10007):1945-54.
doi: 10.1016/S0140-6736(15)00235-4 pmid: 26386538 |
| [37] | Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S; Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018; 391(10129):1513-23. |
| [38] |
Park S, Yon H, Ban CY, Shin H, Eum S, Lee SW, et al. National trends in alcohol and substance use among adolescents from 2005 to 2021: a Korean serial cross-sectional study of one million adolescents. World J Pediatr. 2023; 19(11):1071-81.
doi: 10.1007/s12519-023-00715-9 pmid: 36977821 |
| [39] |
Di Castelnuovo A, Bonaccio M, Costanzo S, McElduff P, Linneberg A, Salomaa V, et al. Drinking alcohol in moderation is associated with lower rate of all-cause mortality in individuals with higher rather than lower educational level: findings from the MORGAM project. Eur J Epidemiol. 2023; 38(8): 869-81.
doi: 10.1007/s10654-023-01022-3 pmid: 37386255 |
| [1] | Qian Lu, Shi-jiao Yan, Huan-jun Chen, Xiong-fei Pan, Yi-xiang Ye, Xing-yue Song, Ri-xing Wang, Chuan-zhu Lyu. The relationship between physical activity in early pregnancy and hypertensive disorders of pregnancy: a cohort study in Chinese women [J]. World Journal of Emergency Medicine, 2023, 14(3): 204-208. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
