World Journal of Emergency Medicine ›› 2014, Vol. 5 ›› Issue (4): 298-305.doi: 10.5847/wjem.j.issn.1920-8642.2014.04.010
• Original Articles • Previous Articles Next Articles
Jian Lu1,2, Yi Shen1, Hui-yin Qian2, Li-jun Liu2( ), Bao-chun Zhou2, Yan Xiao2, Jin-ning Mao2, Guo-yin An2, Ming-zhong Rui2, Tao Wang2, Chang-lai Zhu3
), Bao-chun Zhou2, Yan Xiao2, Jin-ning Mao2, Guo-yin An2, Ming-zhong Rui2, Tao Wang2, Chang-lai Zhu3
Received:2014-02-20
Accepted:2014-09-10
Online:2014-12-15
Published:2014-12-15
Contact:
Li-jun Liu
E-mail:lijunliusz@hotmail.com
Jian Lu, Yi Shen, Hui-yin Qian, Li-jun Liu, Bao-chun Zhou, Yan Xiao, Jin-ning Mao, Guo-yin An, Ming-zhong Rui, Tao Wang, Chang-lai Zhu. Effects of mild hypothermia on the ROS and expression of caspase-3 mRNA and LC3 of hippocampus nerve cells in rats after cardiopulmonary resuscitation[J]. World Journal of Emergency Medicine, 2014, 5(4): 298-305.
Table 1
Asphyxia time and data associated resuscitation in the CPR group (mean±SD)
| Groups | Survival number (n) | The time from asphyxiation to SBP≤25 mmHg (s) | The time of SBP ≤25 mmHg (s) | The time of resuscitation (s) | The time from induction to 32 °C of HT group (min) |
|---|---|---|---|---|---|
| NT-12 | 9 | 212±33 | 241±32 | 81±30 | — |
| NT-24 | 7 | 244±33 | 248±31 | 84±23 | — |
| HT-12 | 8 | 229±47 | 249±35 | 70±8 | 24.5±3.1 |
| HT-24 | 9 | 219±28 | 247±21 | 79±15 | 27.3±3.7 |
Table 2
Basic vital signs of the CPR group (mean±SD)
| Groups | T (center,°C) | HR (beats/min) | RR (beats/min) | MAP (mmHg) |
|---|---|---|---|---|
| NT (n=16) | ||||
| Baseline | 36.6±0.7 | 255±42 | 78±4 | 94±21 |
| PR-0.5 h | 36.5±0.5 | 232±58 | 78±1 | 66±9 |
| PR-4 h | 36.6±0.5 | 248±61 | 89±11 | 91±28 |
| HT (n=17) | ||||
| Baseline | 36.4±0.5 | 238±37 | 77±1 | 100±21 |
| PR-0.5 h | 32.4±0.6 | 260±62 | 77±1 | 78±15 |
| PR-4 h | 32.1±0.2 | 257±57 | 75±10 | 96±18 |
Table 3
Blood gas analysis of the CPR group before asphyxia, 0.5 and 4 hours after ROSC
| Groups | pH | PaO2 (mmHg) | PaCO2 (mmHg) | SaO2 (%) | Lac (mg/dL) |
|---|---|---|---|---|---|
| NT (n=16) | |||||
| Baseline | 7.36±0.06 | 91±29 | 42±6 | 94±8 | 2.2±0.9 |
| PR-0.5 h | 7.23±0.11 | 84±24 | 56±16 | 92±9 | 6.9±2.8 |
| PR-4 h | 7.29±0.07 | 87±27 | 49±10 | 90±9 | 3.4±1.8 |
| HT (n=17) | |||||
| Baseline | 7.39±0.03 | 85±9 | 41±6 | 96±2 | 2.1±0.9 |
| PR-0.5 h | 7.35±0.11 | 81±13 | 50±11 | 94±16 | 7.2±2.9 |
| PR-4 h | 7.33±0.08 | 71±10 | 44±6 | 92±4 | 2.3±1.1* |

Figure 5.
Caspase-3 mRNA expression in nerve cells of the hippocampus in each group. The data of β-actin were normalized. The fold changes of caspase-3mRNA were calculated in the BC group, and the results are presented as the mean fold of the blank control±SD. *P<0.05 vs. the BC group; ﹟P<0.05 vs. the NT group. HT: mild hypothermia group; NT: normothermia group; BC: blank control group.

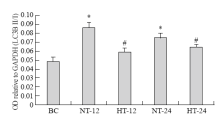
Figure 7.
LC3B-II/I expression in nerve cells of the hippocampus in each group. The data were normalized GAPDH. The fold changes of LC3B-II/I were calculated in the BC group, and the results were presented as the mean fold of the blank control ( mean±SD). *P<0.05 vs. the BC group; ﹟P<0.05 vs. the NT group. HT: mild hypothermia group; NT: normothermia group; BC: control group.


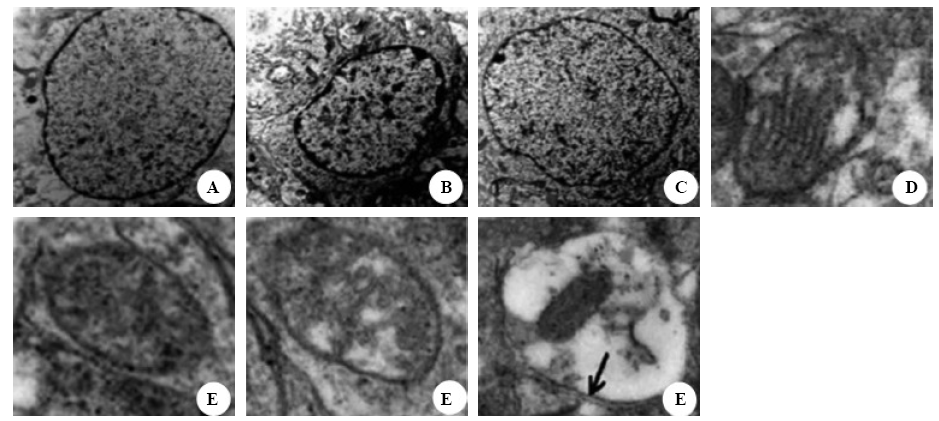
Figure 8.
Representative electron micrographs of nuclei (original magnification×8 000) and mitochondria (original magnification×40 000). Tissues were isolated from the rat hippocampus at 24 hours after ROSC. A: normal nuclei with intact nuclear membrane and a smooth chromatin in the blank control group. B: markedly damaged nuclei with chromatin margination and condensed nucleoplasm in the normothermia group. C: slightly damaged nuclei with basically normal nuclear membrane and a slightly damaged chromatin in the hypothermia group. D: normal mitochondria with intact membrane cristae and a smooth matrix in the blank control group. E: markedly damaged mitochondrion with disrupted cristae and a damaged matrix in the normothermia group. F: slightly damaged mitochondrion with basically normal cristae and a slightly damaged matrix in the hypothermia group. G: damaged mitochondria engulfed by autophagolysosome in the normothermia group (black arrow: double membrane structure of autophagosome).
| 1 |
Wang XP, Lin QM, Zhao S, Lin SR, Chen F. Therapeutic benefits of mild hypothermia in patients successfully resuscitated from cardiac arrest: A meta-analysis. World J Emerg Med 2013; 4:260-265.
doi: 10.5847/wjem.j.issn.1920-8642.2013.04.003 pmid: 25215129 |
| 2 |
Xiong W, Hoesch RE, Geocadin RG. Post-cardiac arrest encephalopathy. Semin Neurol 2011; 31:216-225.
doi: 10.1055/s-0031-1277991 pmid: 21590626 |
| 3 | Liu J, Huang L. The impact of mutual antagonism from AMPK and mTOR on the ischemic brain injury. Chin J Emerg Med 2012; 21:1398-1400. |
| 4 | Idris AH, Becker LB, Ornato JP, Hedges JR, Bircher NG, Chandra NC, et al. Utstein-style guidelines for uniformreporting of laboratory CPR research. Circulation 1996; 94:2324-2336. |
| 5 |
Geocadin RG, Ghodadra R, Kimura T, Lei H, Sherman DL, Hanley DF, et al. A novel quantitative EEG injury measure of global cerebral ischemia. Clin Neurophysiol 2000; 111:1779-87.
doi: 10.1016/s1388-2457(00)00379-5 pmid: 11018492 |
| 6 |
Murphy MP. How mitochondria produce reactive oxygen species. Biochem J 2009; 417:1-13.
pmid: 19061483 |
| 7 | Marchi S, Giorgi C, Suski JM, Agnoletto C, Bononi A, Bonora M, et al. Mitochondria-ros crosstalk in the control of cell death and aging. J Signal Transduct 2012; 329635. |
| 8 |
Liu X, Wang M, Chen H, Guo Y, Ma F, Shi F, et al. Hypothermia protects the brain from transient global ischemia/reperfusion by attenuating endoplasmic reticulum response-induced apoptosis through CHOP. PLoS One 2013; 8:e53431
doi: 10.1371/journal.pone.0053431 pmid: 23301071 |
| 9 |
Wu X, Mao H, Liu J, Xu J, Cao J, Gu X, et al. Dynamic change of SGK expression and its role in neuron apoptosis after traumatic brain injury. Int J Clin Exp Pathol 2013; 6:1282-1293.
pmid: 23826409 |
| 10 | Zgavc T, Ceulemans AG, Hachimi-Idrissi S, Kooijman R, Sarre S, Michotte Y. The neuroprotective effect of post ischemic brief mild hypothermic treatment correlates with apoptosis, but not with gliosis in endothelin-1 treated rats. BMC Neurosci 2012; 13:105. |
| 11 |
Adhami F, Liao G, Morozov YM, Schloemer A, Schmithorst VJ, Lorenz JN, et al. Cerebral ischemia-hypoxia induces intravascular coagulation and autophagy. Am J Pathol 2006; 169:566-583.
doi: 10.2353/ajpath.2006.051066 pmid: 16877357 |
| 12 |
Jaeger PA, Wyss-Coray T. All-you-can-eat: autophagy in neurodegeneration and neuroprotection. Mol Neurodegener 2009; 4:16.
pmid: 19348680 |
| 13 |
Adhami F, Liao G, Morozov YM, Schloemer A, Schmithorst VJ, Lorenz JN, et al. Cerebral ischemia-hypoxia induces intravascular coagulation and autophagy. Am J Pathol 2006; 169:566-583.
doi: 10.2353/ajpath.2006.051066 pmid: 16877357 |
| 14 |
Weidberg H, Shvets E, Shpilka T, Shimron F, Shinder V, Elazar Z. LC3 and GATE-16/GABARAP subfamilies are both essential yet act differently in autophagosome biogenesis. EMBO J 2010; 29:1792-1802.
pmid: 20418806 |
| 15 |
Bendix I, Schulze C, Haefen Cv, Gellhaus A, Endesfelder S, Heumann R, et al. Erythropoietin modulates autophagy signaling in the developing rat brain in an in vivo model of oxygen-toxicity. Int J Mol Sci 2012; 13:12939-12951.
doi: 10.3390/ijms131012939 pmid: 23202931 |
| 16 |
Klionsky DJ, Abdalla FC, Abeliovich H, Abraham RT, Acevedo-Arozena A, Adeli K, et al. Guidelines for the use and interpretation of assays for monitoring autophagy in higher eukaryotes. Autophagy 2008; 4:151-175.
doi: 10.4161/auto.5338 pmid: 18188003 |
| [1] | Alexei Birkun, Fatima Trunkwala, Adhish Gautam, Miriam Okoroanyanwu, Adesokan Oyewumi. Availability of basic life support courses for the general populations in India, Nigeria and the United Kingdom: An internet-based analysis [J]. World Journal of Emergency Medicine, 2020, 11(3): 133-139. |
| [2] | Jung Wan Kim, Jin Woong Lee, Seung Ryu, Jung Soo Park, InSool Yoo, Yong Chul Cho, Hong Joon Ahn. Changes in peak inspiratory flow rate and peak airway pressure with endotracheal tube size during chest compression [J]. World Journal of Emergency Medicine, 2020, 11(2): 97-101. |
| [3] | Ye-cheng Liu, Yan-meng Qi, Hui Zhang, Joseph Walline, Hua-dong Zhu. A survey of ventilation strategies during cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2019, 10(4): 222-227. |
| [4] | Israel Olatunji Gabriel, Joel O. Aluko. Theoretical knowledge and psychomotor skill acquisition of basic life support training programme among secondary school students [J]. World Journal of Emergency Medicine, 2019, 10(2): 81-87. |
| [5] | Alexei Birkun, Yekaterina Kosova. Social attitude and willingness to attend cardiopulmonary resuscitation training and perform resuscitation in the Crimea [J]. World Journal of Emergency Medicine, 2018, 9(4): 237-248. |
| [6] | Alexei Birkun, Maksim Glotov, Herman Franklin Ndjamen, Esther Alaiye, Temidara Adeleke, Sergey Samarin. Pre-recorded instructional audio vs. dispatchers’ conversational assistance in telephone cardiopulmonary resuscitation: A randomized controlled simulation study [J]. World Journal of Emergency Medicine, 2018, 9(3): 165-171. |
| [7] | Alexei Birkun, Maksim Glotov. Education in cardiopulmonary resuscitation in Russia: A systematic review of the available evidence [J]. World Journal of Emergency Medicine, 2017, 8(4): 245-252. |
| [8] | Ling Zhou, Hui Li, Hong-yan Wei, Chun-lin Hu, Xiao-li Jing, Hong Zhan, Xiao-xing Liao, Xin Li. Study on the development and usage of a cardiopulmonary resuscitation time point recorder [J]. World Journal of Emergency Medicine, 2017, 8(3): 195-199. |
| [9] | Chennappa Kalvatala Krishna, Hakim Irfan Showkat, Meenakshi Taktani, Vikram Khatri. Out of hospital cardiac arrest resuscitation outcome in North India — CARO study [J]. World Journal of Emergency Medicine, 2017, 8(3): 200-205. |
| [10] | Vinej Somaraj, Rekha P Shenoy, Ganesh Shenoy Panchmal, Praveen S Jodalli, Laxminarayan Sonde, Ravichandra Karkal. Knowledge, attitude and anxiety pertaining to basic life support and medical emergencies among dental interns in Mangalore City, India [J]. World Journal of Emergency Medicine, 2017, 8(2): 131-135. |
| [11] | Ji Ung Na, Sang Kuk Han, Pil Cho Choi, Dong Hyuk Shin. Effect of metronome rates on the quality of bag-mask ventilation during metronome-guided 30:2 cardiopulmonary resuscitation: A randomized simulation study [J]. World Journal of Emergency Medicine, 2017, 8(2): 136-140. |
| [12] | Gan-nan Wang, Xu-feng Chen, Li Qiao, Yong Mei, Jin-ru Lv, Xi-hua Huang, Bin Shen, Jin-song Zhang. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A meta-analysis of 2 260 patients with cardiac arrest [J]. World Journal of Emergency Medicine, 2017, 8(1): 5-11. |
| [13] | Marion Leary, David G. Buckler, Daniel J. Ikeda, Daiane A. Saraiva, Robert A. Berg, Vinay M. Nadkarni, Audrey L. Blewer, Benjamin S. Abella. The association of layperson characteristics with the quality of simulated cardiopulmonary resuscitation performance [J]. World Journal of Emergency Medicine, 2017, 8(1): 12-18. |
| [14] | Sarah A. Alkandari, Lolwa Alyahya, Mohammed Abdulwahab. Cardiopulmonary resuscitation knowledge and attitude among general dentists in Kuwait [J]. World Journal of Emergency Medicine, 2017, 8(1): 19-24. |
| [15] | Mario Kobras, Sascha Langewand, Christina Murr, Christiane Neu, Jeannette Schmid. Short lessons in basic life support improve self-assurance in performing cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2016, 7(4): 255-262. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 644
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 259
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
