World Journal of Emergency Medicine ›› 2025, Vol. 16 ›› Issue (2): 153-160.doi: 10.5847/wjem.j.1920-8642.2025.037
• Original Articles • Previous Articles Next Articles
Yi Zhu1,2, Lina Mao1,2, Zhongman Zhang1,2, Sae Rom Lee1,2, Tianshi Li1,2, Hao Zhou1,2, Yanbin Dong1,2, Di An1,2, Wei Li1,2( ), Xufeng Chen1,2(
), Xufeng Chen1,2( )
)
Received:2024-05-29
Accepted:2024-10-04
Online:2025-03-19
Published:2025-03-01
Contact:
Xufeng Chen, Email: Yi Zhu, Lina Mao, Zhongman Zhang, Sae Rom Lee, Tianshi Li, Hao Zhou, Yanbin Dong, Di An, Wei Li, Xufeng Chen. A predictive model for intracranial hemorrhage in adult patients receiving extracorporeal membrane oxygenation[J]. World Journal of Emergency Medicine, 2025, 16(2): 153-160.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2025.037
Table 1.
Baseline demographics and clinical characteristics of adult patients receiving ECMO
| Variables | All patients (n=227) | ICH group (n=22) | Non-ICH group (n=205) | P-value |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 48 (33, 60) | 44 (28, 55) | 49 (34, 61) | 0.088 |
| Male gender | 153 (67.4) | 14 (63.6) | 139 (67.8) | 0.657 |
| Body mass index, kg/m2 | 24.0 ± 3.2 | 24.1 ± 3.5 | 24.0 ± 3.2 | 0.825 |
| Comorbidity | ||||
| Hypertension | 68 (30.0) | 6 (27.3) | 62 (30.2) | 0.772 |
| Diabetes mellitus | 39 (17.2) | 3 (13.6) | 36 (17.6) | 0.774 |
| Coronary heart disease | 33 (14.5) | 1 (4.5) | 32 (15.6) | 0.214 |
| Stroke | 18 (7.9) | 4 (18.2) | 14 (6.8) | 0.081 |
| Chronic renal disease | 6 (2.6) | 1 (4.5) | 5 (2.4) | 0.461 |
| Chronic hepatic disease | 6 (2.6) | 0 (0.0) | 6 (2.9) | 1.000 |
| ECMO mode | 0.482 | |||
| Veno-venous | 48 (21.1) | 4 (18.2) | 44 (21.5) | |
| Veno-arterial | 72 (31.7) | 5 (22.7) | 67 (32.7) | |
| ECPR | 107 (47.1) | 13 (59.1) | 94 (45.9) | |
| Recent bleeding history | 41 (18.1) | 6 (27.3) | 35 (17.1) | 0.247 |
| Anti-platelet therapy | 14 (6.2) | 1 (4.5) | 13 (6.3) | 1.000 |
| Anti-coagulant therapy | 8 (3.5) | 1 (4.5) | 7 (3.4) | 0.564 |
| Pre-ECMO cardiac arrest | 109 (48.0) | 14 (63.6) | 95 (46.3) | 0.123 |
| MAP pre-ECMO, mmHg | 58 (37, 80) | 44 (34, 68) | 60 (38, 81) | 0.080 |
| Lab findings pre-ECMO | ||||
| Hematocrit | 0.340 ± 0.767 | 0.330 ± 0.817 | 0.341 ± 0.763 | 0.503 |
| Platelet count, ×109/L | 160 (104, 219) | 127 (56, 194) | 166 (107, 220) | 0.126 |
| Creatinine, μmol/L | 107.0 (73.1, 150.7) | 134.1 (75.4, 156.2) | 106.4 (70.7, 150.7) | 0.263 |
| Fibrinogen, g/L | 2.29 (1.41, 3.58) | 1.57 (0.47, 2.44) | 2.35 (1.53, 3.66) | 0.003 |
| INR | 1.45 (1.23, 2.04) | 1.93 (1.40, 2.82) | 1.43 (1.22, 1.93) | 0.005 |
| GWR | 1.31 (1.26, 1.35) | 1.23 (1.17, 1.29) | 1.32 (1.27, 1.35) | <0.001 |
Table 2.
Clinical characteristics during ECMO support of adult patients receiving ECMO
| Variables | All patients (n=227) | ICH group (n=22) | Non-ICH group (n=205) | P-value |
|---|---|---|---|---|
| Lab findings during ECMOa | ||||
| Minimum HCT | 0.256 ± 0.534 | 0.242 ± 0.522 | 0.257 ± 0.534 | 0.201 |
| Minimum platelet count, ×109/L | 61 (41, 93) | 43 (18, 65) | 62 (43, 94) | 0.001 |
| Peak creatinine, μmol/L | 113.7 (75.6, 154.6) | 130.9 (81.6, 171.2) | 112.2 (73.0, 153.3) | 0.290 |
| Minimum fibrinogen, g/L | 1.75 (1.16, 2.55) | 1.71 (0.73, 2.46) | 1.75 (1.20, 2.57) | 0.285 |
| Peak INR | 1.58 (1.33, 2.18) | 1.49 (1.20, 2.90) | 1.58 (1.34, 2.13) | 0.650 |
| Transfused blood products a | ||||
| RBC, mL/(kg·d) | 2.35 (0.46, 4.98) | 1.98 (1.02, 4.36) | 2.34 (0, 5.20) | 0.968 |
| Platelet, mL/(kg·d) | 0.29 (0, 1.64) | 1.34 (0.22, 3.06) | 0 (0, 1.54) | 0.006 |
| FFP, mL/(kg·d) | 0 (0, 1.43) | 1.13 (0, 4.40) | 0 (0, 1.05) | 0.004 |
| Extracranial bleeding a | 81 (35.7) | 11 (50.0) | 70 (34.1) | 0.140 |
| Hepatic failurea | 34 (15.0) | 6 (27.2) | 28 (13.7) | 0.112 |
| Duration of MV, days | 7 (3, 12) | 7 (4, 9) | 7 (2, 12) | 0.930 |
| Duration of CRRT, days | 3 (0, 9) | 4 (1, 7) | 3 (0, 9) | 0.523 |
| 28-day mortality | 115 (50.7) | 18 (81.8) | 97 (47.3) | 0.001 |
| In-hospital mortality | 118 (52.0) | 20 (90.9) | 98 (47.8) | 0.001 |
Table 3.
Predictive performance of clinical characteristics for ICH in adults receiving ECMO
| Variables | AUC | 95%CI | Optimal cut-off value | Youden index | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | P-value |
|---|---|---|---|---|---|---|---|---|---|
| Age | 0.611 | 0.496-0.726 | 49 | 0.199 | 51.7 | 68.2 | 13.2 | 93.8 | 0.088 |
| MAP pre-ECMO | 0.614 | 0.489-0.738 | 48 | 0.230 | 63.9 | 59.1 | 14.9 | 93.6 | 0.080 |
| Fibrinogen pre-ECMO | 0.690 | 0.575-0.805 | 1.96 | 0.321 | 63.9 | 68.2 | 16.8 | 94.9 | 0.003 |
| INR pre-ECMO | 0.681 | 0.571-0.790 | 2.68 | 0.314 | 45.5 | 85.9 | 25.6 | 93.6 | 0.005 |
| PLT transfusion | 0.667 | 0.551-0.783 | 0.77 | 0.342 | 72.7 | 61.5 | 16.8 | 95.5 | 0.010 |
| FFP transfusion | 0.671 | 0.542-0.801 | 2.07 | 0.294 | 45.5 | 83.9 | 23.3 | 93.5 | 0.008 |
| Minimum PLT count | 0.716 | 0.604-0.828 | 29 | 0.357 | 45.5 | 90.2 | 33.3 | 93.9 | <0.001 |
| GWR | 0.788 | 0.701-0.876 | 1.27 | 0.503 | 72.7 | 77.6 | 25.8 | 96.4 | <0.001 |
Table 4.
Univariate and multivariate logistic regression analyses of risk factors for intracerebral hemorrhage in adult patients receiving ECMO
| Variables | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| OR | 95%CI | P-value | OR | 95%CI | P-value | ||
| Age | 0.978 | 0.952-1.004 | 0.096 | - | - | - | |
| GWR | 0.891 | 0.843-0.942 | <0.001 | 0.894 | 0.841-0.951 | <0.001 | |
| MAP pre-ECMO | 0.988 | 0.972-1.004 | 0.136 | - | - | - | |
| Fibrinogen pre-ECMO | 0.645 | 0.455-0.916 | 0.014 | - | - | - | |
| INR pre-ECMO | 1.168 | 0.931-1.466 | 0.178 | - | - | - | |
| Stroke | 3.032 | 0.902-10.184 | 0.073 | 4.265 | 1.052-17.291 | 0.042 | |
| PLT transfusion | 1.185 | 1.012-1.388 | 0.035 | - | - | - | |
| FFP transfusion | 1.274 | 1.108-1.465 | 0.001 | 1.208 | 1.037-1.408 | 0.015 | |
| Minimum PLT count | 0.973 | 0.956-0.990 | 0.002 | 0.977 | 0.958-0.996 | 0.019 | |
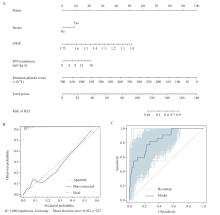
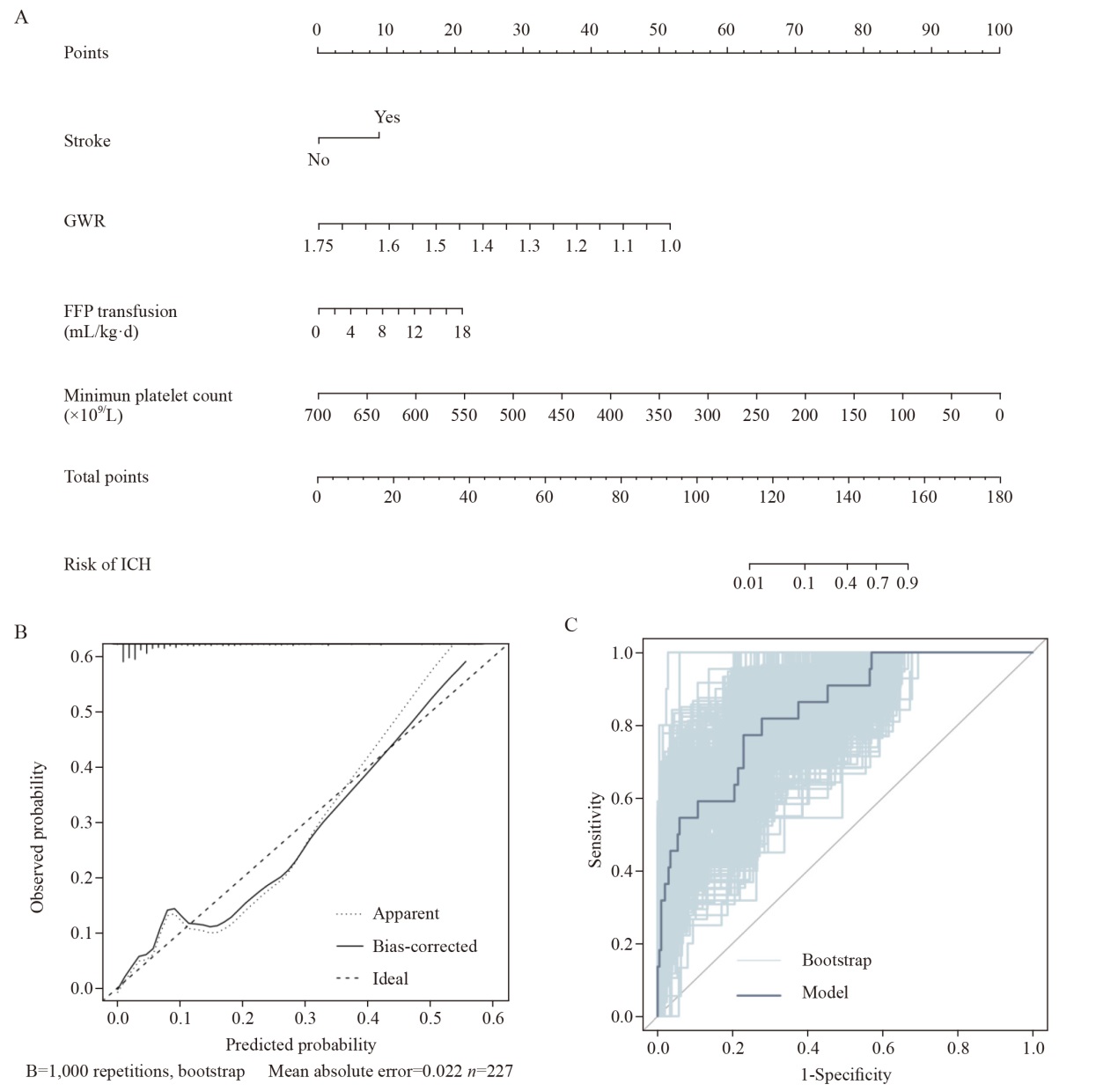
Figure 3.
The establishment and evaluation of the predictive model for ICH. (A) the nomogram for predicting ICH in adults receiving ECMO; (B) the calibration curve of the predictive model; (C) the AUROC of model and the internal validation using the bootstrap method (resampling=1,000). GWR: grey-white-mater ratio; FFP: fresh frozen plasma; ECMO: extracorporeal membrane oxygenation; ICH: intracranial hemorrhage.
| 1 |
Schrage B, Becher PM, Bernhardt A, Bezerra H, Blankenberg S, Brunner S, et al. Left ventricular unloading is associated with lower mortality in patients with cardiogenic shock treated with venoarterial extracorporeal membrane oxygenation: results from an international, multicenter cohort study. Circulation. 2020; 142(22): 2095-106.
doi: 10.1161/CIRCULATIONAHA.120.048792 pmid: 33032450 |
| 2 | Inoue A, Hifumi T, Sakamoto T, Okamoto H, Kunikata J, Yokoi H, et al. Extracorporeal cardiopulmonary resuscitation in adult patients with out-of-hospital cardiac arrest: a retrospective large cohort multicenter study in Japan. Crit Care. 2022; 26(1): 129. |
| 3 |
Chen ZS, Mondal NK, Zheng SR, Koenig SC, Slaughter MS, Griffith BP, et al. High shear induces platelet dysfunction leading to enhanced thrombotic propensity and diminished hemostatic capacity. Platelets. 2019; 30(1): 112-9.
doi: 10.1080/09537104.2017.1384542 pmid: 29182470 |
| 4 | Fletcher-Sandersjöö A, Bartek J Jr, Thelin EP, Eriksson A, Elmi-Terander A, Broman M, et al. Predictors of intracranial hemorrhage in adult patients on extracorporeal membrane oxygenation: an observational cohort study. J Intensive Care. 2017; 5: 27. |
| 5 | Lüsebrink E, Zimmer S, Schrage B, Dabboura S, Majunke N, Scherer C, et al. Intracranial haemorrhage in adult patients on venoarterial extracorporeal membrane oxygenation. Eur Heart J Acute Cardiovasc Care. 2022; 11(4): 303-11. |
| 6 |
Lockie CJA, Gillon SA, Barrett NA, Taylor D, Mazumder A, Paramesh K, et al. Severe respiratory failure, extracorporeal membrane oxygenation, and intracranial hemorrhage. Crit Care Med. 2017; 45(10): 1642-9.
doi: 10.1097/CCM.0000000000002579 pmid: 28727576 |
| 7 | Wu XJ, Li M, Cai Y, Zhai TS, Zhang Y, Zhan QY, et al. Risk factors for intracranial hemorrhage and mortality in adult patients with severe respiratory failure managed using veno-venous extracorporeal membrane oxygenation. Chin Med J (Engl). 2022; 135(1): 36-41. |
| 8 |
Arachchillage DRJ, Passariello M, Laffan M, Aw TC, Owen L, Banya W, et al. Intracranial hemorrhage and early mortality in patients receiving extracorporeal membrane oxygenation for severe respiratory failure. Semin Thromb Hemost. 2018; 44(3): 276-86.
doi: 10.1055/s-0038-1636840 pmid: 29566407 |
| 9 |
Metter RB, Rittenberger JC, Guyette FX, Callaway CW. Association between a quantitative CT scan measure of brain edema and outcome after cardiac arrest. Resuscitation. 2011; 82(9): 1180-5.
doi: 10.1016/j.resuscitation.2011.04.001 pmid: 21592642 |
| 10 |
Choi SP, Park HK, Park KN, Kim YM, Ahn KJ, Choi KH, et al. The density ratio of grey to white matter on computed tomography as an early predictor of vegetative state or death after cardiac arrest. Emerg Med J. 2008; 25(10): 666-9.
doi: 10.1136/emj.2007.053306 pmid: 18843066 |
| 11 | Scheel M, Storm C, Gentsch A, Nee J, Luckenbach F, Ploner CJ, et al. The prognostic value of gray-white-matter ratio in cardiac arrest patients treated with hypothermia. Scand J Trauma Resusc Emerg Med. 2013; 21: 23. |
| 12 |
Hunsicker O, Beck L, Krannich A, Finger T, Prinz V, Spies C, et al. Timing, outcome, and risk factors of intracranial hemorrhage in acute respiratory distress syndrome patients during venovenous extracorporeal membrane oxygenation. Crit Care Med. 2021; 49(2): e120-e129.
doi: 10.1097/CCM.0000000000004762 pmid: 33323749 |
| 13 |
Hwang J, Caturegli G, White B, Chen L, Cho SM. Cerebral microbleeds and intracranial hemorrhages in adult patients on extracorporeal membrane oxygenation-autopsy study. Crit Care Explor. 2021; 3(3): e0358.
doi: 10.1097/CCE.0000000000000358 pmid: 33681814 |
| 14 |
Chandler WL. Platelet, red cell, and endothelial activation and injury during extracorporeal membrane oxygenation. ASAIO J. 2021; 67(8): 935-42.
doi: 10.1097/MAT.0000000000001320 pmid: 33606391 |
| 15 |
Prinz V, Manekeller L, Menk M, Hecht N, Weber-Carstens S, Vajkoczy P, et al. Clinical management and outcome of adult patients with extracorporeal life support device-associated intracerebral hemorrhage-a neurocritical perspective and grading. Neurosurg Rev. 2021; 44(5): 2879-88.
doi: 10.1007/s10143-020-01471-4 pmid: 33483801 |
| 16 |
Jiritano F, Serraino GF, Ten Cate H, Fina D, Matteucci M, Mastroroberto P, et al. Platelets and extra-corporeal membrane oxygenation in adult patients: a systematic review and meta-analysis. Intensive Care Med. 2020; 46(6): 1154-69.
doi: 10.1007/s00134-020-06031-4 pmid: 32328725 |
| 17 |
Streitberger KJ, Endisch C, Ploner CJ, Stevens R, Scheel M, Kenda M, et al. Timing of brain computed tomography and accuracy of outcome prediction after cardiac arrest. Resuscitation. 2019; 145: 8-14.
doi: S0300-9572(19)30636-7 pmid: 31585185 |
| 18 |
Chae MK, Ko E, Lee JH, Lee TR, Yoon H, Hwang SY, et al. Better prognostic value with combined optic nerve sheath diameter and grey-to-white matter ratio on initial brain computed tomography in post-cardiac arrest patients. Resuscitation. 2016; 104: 40-5.
doi: 10.1016/j.resuscitation.2016.04.001 pmid: 27143123 |
| 19 | Arbelaez A, Castillo M, Mukherji SK. Diffusion-weighted MR imaging of global cerebral Anoxia. AJNR Am J Neuroradiol. 1999; 20(6): 999-1007. |
| 20 |
Takahashi S, Higano S, Ishii K, Matsumoto K, Sakamoto K, Iwasaki Y, et al. Hypoxic brain damage: cortical laminar necrosis and delayed changes in white matter at sequential MR imaging. Radiology. 1993; 189(2): 449-56.
doi: 10.1148/radiology.189.2.8210374 pmid: 8210374 |
| 21 |
Bashir RA, Vayalthrikkovil S, Espinoza L, Irvine L, Scott J, Mohammad K. Prevalence and characteristics of intracranial hemorrhages in neonates with hypoxic ischemic encephalopathy. Am J Perinatol. 2018; 35(7): 676-81.
doi: 10.1055/s-0037-1608927 pmid: 29220856 |
| 22 | Zotzmann V, Rilinger J, Lang CN, Duerschmied D, Benk C, Bode C, et al. Early full-body computed tomography in patients after extracorporeal cardiopulmonary resuscitation (eCPR). Resuscitation. 2020; 146: 149-54. |
| 23 |
von Heymann C, Keller MK, Spies C, Schuster M, Meinck K, Sander M, et al. Activity of clotting factors in fresh-frozen plasma during storage at 4 degrees C over 6 days. Transfusion. 2009; 49(5): 913-20.
doi: 10.1111/j.1537-2995.2008.02063.x pmid: 19159416 |
| 24 |
McMichael ABV, Zimmerman KO, Kumar KR, Ozment CP. Evaluation of effect of scheduled fresh frozen plasma on ECMO circuit life: a randomized pilot trial. Transfusion. 2021; 61(1): 42-51.
doi: 10.1111/trf.16164 pmid: 33269487 |
| [1] | Fei Zeng, Lingyun Cai, Luyao Guo, Meijuan Lan, Jiangshuyuan Liang, Peipei Gu. Pulmonary rehabilitation protocols in urgent lung transplantation patients [J]. World Journal of Emergency Medicine, 2024, 15(1): 47-51. |
| [2] | Cong-ying Song, Jian-yong Zhu, Wei Huang, Yuan-qiang Lu. Development and validation of a predictive model for the assessment of potassium-lowering treatment among hyperkalemia patients [J]. World Journal of Emergency Medicine, 2023, 14(3): 198-203. |
| [3] | Quincy K. Tran, Francis O’Connell, Andrew Hakopian, Marwa SH Abrahim, Kamilla Beisenova, Ali Pourmand. Patient care during interfacility transport: a narrative review of managing diverse disease states [J]. World Journal of Emergency Medicine, 2023, 14(1): 3-9. |
| [4] | Jia-ying Tang, Xiu-qin Feng, Xiao-xia Huang, Yu-ping Zhang, Zhi-ting Guo, Lan Chen, Hao-tian Chen, Xiao-xiao Ying. Development and validation of a predictive model for patients with post-extubation dysphagia [J]. World Journal of Emergency Medicine, 2023, 14(1): 49-55. |
| [5] | David Vandroux, Thomas Aujoulat, Bernard-Alex Gaüzère, Bérénice Puech, Bertrand Guihard, Olivier Martinet. Predicting factors for the need of extracorporeal membrane oxygenation for suicide attempts by cardiac medication: a single-center cohort study [J]. World Journal of Emergency Medicine, 2022, 13(4): 283-289. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
