World Journal of Emergency Medicine ›› 2013, Vol. 4 ›› Issue (2): 98-106.doi: 10.5847/wjem.j.issn.1920-8642.2013.02.003
• Original Articles • Previous Articles Next Articles
W. Scott Russell1( ), Judith Rosen Farrar2, Richard Nowak3, Daniel P. Hays4, Natalie Schmitz5, Joseph Wood6, Judi Miller7
), Judith Rosen Farrar2, Richard Nowak3, Daniel P. Hays4, Natalie Schmitz5, Joseph Wood6, Judi Miller7
Received:2013-01-16
Accepted:2013-05-02
Online:2013-06-15
Published:2013-06-15
Contact:
W. Scott Russell
E-mail:ruscott@musc.edu
W. Scott Russell, Judith Rosen Farrar, Richard Nowak, Daniel P. Hays, Natalie Schmitz, Joseph Wood, Judi Miller. Evaluating the management of anaphylaxis in US emergency departments: Guidelines vs. practice[J]. World Journal of Emergency Medicine, 2013, 4(2): 98-106.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn//EN/10.5847/wjem.j.issn.1920-8642.2013.02.003
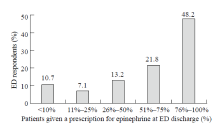
Figure 3.
Percentage of patients seen in the ED for anaphylaxis who were discharged with a prescription for self-injectable epinephrine. Respondents answered the question: What percentage of patients treated for anaphylaxis in your ED is discharged with a prescription for self-injectable epinephrine? (n=197).
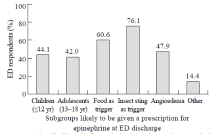
Figure 4.
The likelihood of anaphylaxis patient subgroups being discharged with a prescription for self-injectable epinephrine. Respondents answered the question: Are there particular patient populations you are more likely to prescribe self-injectable epinephrine to at discharge? (n=188).
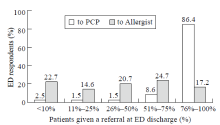
Figure 5.
Percentage of patients seen in the ED for anaphylaxis, who were given a referral to see a physician at discharge. Respondents answered the question,What percentage of patients treated for anaphylaxis in your ED are discharged with a referral to a primary care physician (PCP) and/or to an allergist? (n=198 respondents).
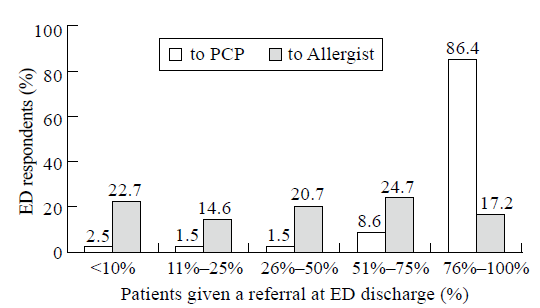
Table 1
Clinical criteria for the diagnosis of acute anaphylactic episode:[3,4,5,6,7] Anaphylaxis is highly likely when any one of the following 3 criteria is fulfilled
| Either criteria 1 | Or criteria 2 | Or criteria 3 |
|---|---|---|
| Acute onset (min-several hr) of an illness involving the skin, mucosal tissue, or both (e.g., generalized hives, pruritus or flushing, swollen lips-tongue-uvula) and at least 1 of the following: a. Respiratory compromise (e.g., dyspnea, wheeze-bronchospasm, stridor, reduced PEF, hypoxemia) b. Reduced BP or associated Sx of end-organ dysfunction (e.g., hypotonia, syncope) | Two or more of the following occurring rapidly (min-several hr) after exposure to a likely allergen for the patient: a. Involvement of the skin-mucosal tissue (e.g., generalized hives, itch-flush, swollen lips-tongue-uvula) b. Respiratory compromise (e.g., dyspnea, wheeze-bronchospasm, stridor, reduced PEF, hypoxemia) c. Reduced BP or associated Sx of end-organ dysfunction (e.g., hypotonia, syncope) d. Before persistent: persistent GI Sx (e.g., cramps, abdominal pain, vomiting) | Reduced BP occurring rapidly (min-several hr) after exposure to a known allergen for the patient: a. Infants and children: low systolic BP (age-specific) or >30% decrease in systolic BP b. Adults: systolic BP<90mm Hg or >30% decrease from baseline |
Table 2
Gaps where clinical practice differs from guideline recommendations for managing the anaphylaxis in the ED, indirectly suggested by studies of the incidence or management of anaphylaxis at US EDs. All studies evaluated US data only and used a definition of anaphylaxis based on current guideline criteria. Gaps in diagnosis, ED treatment, and discharge are noted.
| Citation | Study | Gaps | |||||
|---|---|---|---|---|---|---|---|
| Design | Description | Population | Definition/Dx | Treatment in ED | At discharge | ||
| Adult studies | |||||||
| Campbell et al, 2011[ | Retrospective, consecutive cohort study | Compared dx and tx of ED patients ≥ 50 years and < 50 years who met NAID/FAAN dx criteria for anaphylaxis between 4/2008 and 6/2010 | n=220 patients | Anaphylaxis was often not dx in ED patients presenting with allergic reactions despite multisystem organ involvement (authors suggested this related to 1) lack of universally accepted dx criteria; 2) low recognition of "vague" sx as part of dx, (eg, shortness of breath, light-headedness); 3) lack of sensitive/ specific biomarkers) | Prescription for epinephrine, 63.8%, overall; 40.7% for patients ≥ 50 yr, and 32.1% for patients ≥ 65 yr Post-ED allergist evaluation, 36.4% | ||
| Campbell et al, 2008[ | Retrospective medical record review | Assessed incidence of anaphylaxis (1990-2000)based on dx criteria in random sample of 2 442 patients at tertiary care AMC and community hospital EDs in Olmsted Co, Minn* | n=848 patients: 248 with ICD-9 (or HICDA) codes related to anaphylaxis; 600 with associated dx | Patients meeting criteria for anaphylaxis: 157 of 248 with ICD-9 codes; 54 600 with associated dx (authors suggested variability due to the lack of universally accepted definition of anaphylaxis) | Prescription for epinephrine, 36.6% (more likely in patients who received epinephrine in ED) Referral to allergist, 31.3% (more likely for prescribed epinephrine at discharge) | ||
| Clark et al, 2004[ | Retrospective cohort study) | Evaluated ED visits for physician-dx'd, food-related acute allergic reactions over a 1-yr period in 21 North American AMCs (the Multicenter Airway Research Collaboration) | n=678 patients randomly selected from 5 296 identified charts using food allergy codes and less specific related ICD-9 codes | Epinephrine, 16% Diphenhydramine, 90% Parenteral CCS, 50% | Prescription for epinephrine, 16% (more likely in patients who received epinephrine in the ED) Referral to allergist, 12% Written instructions for avoidance, 40% Wide variability in discharge plans noted | ||
| Clark et al, 2005[ | Retrospective cohort study | Evaluated ED visits for physician-dx'd insect sting allergic reactions over a 1-yr period in 15 North American AMCs (the Multicenter Airway Research Collaboration) | n=617 patients randomly selected from 1 523 identified charts using specific allergy codes and less specific related ICD-9 codes | For patients with anaphylaxis: Epinephrine, 16% Antihistamines, 70% Parenteral CCS, 49% | Patients with systemic reactions (i.e., anaphylaxis or at risk of anaphylaxis): Prescription for epinephrine, 27% Referral to allergist, 20% Written instructions for avoidance, 15% | ||
| Gaeta et al, 2007[ | Retrospective review of nationally representative sample of ED visits using the National Hospital Ambulatory Medical Care Survey | Assessed national trends in ED visits for/managementof anaphylaxis (1993-2004)using ICD-9 codes for acute allergic reactions and anaphylaxis | n=12.4 million ED visits | Epinephrine, 11% Most ED physicians relied on 2nd line agents, particularly H1 antagonists, to tx acute allergic reactions Substantial controversy about how/when to use epinephrine for acute allergic reactions in ED | |||
| Harduar-Morano et al, 2010[ | Retrospective review of ED data from the Florida Agency for Health Care Admini-stration | Assessed FL anaphylaxis cases (2005-2006) by ICD-9-CM codes or using an algorithm based on the 2ndSymposium criteria | n=3 024 records of anaphylaxis episodes (ICD-9 codes, 1 283; algorithm, 1 741) | Lack of standard definition and dx criteria resulted in cases not dx'd or mis-dx'd: 58% of cases were missed using ICD-9 codes alone | Epinephrine: ICD-9 cases (n=111), 10%; algorithm cases (n=180), 11% | ||
| Ross et al, 2008[ | 2-mo retro-spective review of the National Electronic Injury Surveil-lance System database | Evaluated incidence and severity of food allergic reactions presenting to US EDs | n=173 ED-food allergic events reported at 34 sites | Cases meeting criteria for anaphylaxis: 38% received dx; 62% did not | Epinephrine, 19% Antihistamines, 87% Parenteral CCS, 65% | ||
| Rudders et al, 2010a[ | Retrospective medical record review | Evaluated dx and tx of patients with stinging insect hypersensitivity reactions presenting to 3 EDs in Boston, MA (2001-2006) | n=153 patients | In patients with systemic reactions (i.e., anaphylaxis or at risk of anaphylaxis): Epinephrine, 9% Antihistamines, 76% Parenteral CCS, 55% | In patients with systemic reactions (i.e., anaphylaxis or at risk of anaphylaxis): Prescription for epinephrine, 68% Referral to allergist, 11% Written instructions for avoidance, 3% | ||
| Pediatric studies | |||||||
| Bohlke et al, 2004[ | Retrospective review of dx | Estimated incidence of anaphylaxis in relation to specific dx by ICD-9 codes and by sampling related dx w/o specific codes | n=229 422 patients ≤18 yr enrolled in HMO in WA between 3/1/1991 and 12/31/1997 | In 753 possible cases, 67 anaphylaxis episodes identified by ICD-9 codes and 18 more by sampling related dx (authors suggested this reflected 1) lack of a std case definition; 2) variability among criteria used) | Epinephrine, 79% Parenteral antihistamine, 51% Parenteral CCS, 34% | ||
| Gupta et al, 2011[ | Randomized, population-based, cross-sectional survey of US homes with children ≤ 18 yr | Identified prevalence and severity of childhood food allergy (6/2009-2/2010) | n=38 480 children | Disparities in determining etiology of food allergy related to under dx and underestimates of childhood food allergy in the US | Disparities in management of food allergy in ED noted | Disparities in discharge management of food allergy inoted | |
| Huang et al, 2012[ | Retrospective case review | Evaluated dx and tx of 118 680 anaphylaxis encounters at a pediatric ED (2004-2008) using ICD-9 codes | n=213 anaphylaxis episodes in 192 patients: 62 by ICD-9 code for anaphylaxis and 151 that were coded, allergic reaction, but fulfilled the criteria of anaphylaxis or were tx'd as anaphylaxis | Significant miscoding of anaphylaxis: 71% of episodes received ICD-9 code for allergic rx, not anaphylaxis (confusion related to lack of standard dx criteria) | Epinephrine, overall, 79%: 75% of allergic reactions, 81% of coded anaphylaxis Histamine-1-receptor antagonists, 92% Histamine-2-receptor antagonists, 46% Parenteral CCS, 89% | Prescription for epinephrine at ED discharge, 63% | |
| Rudders et al, 2010b[ | Retrospective medical record review | Evaluated dx and tx of children presenting with food-related anaphylaxis at 3 EDs in Boston, MA (2001-2006) | n=1 255 patients | Epinephrine, 20% | Prescription for epinephrine, 43% Referral to allergist, 22% Written instructions for avoidance, 36% | ||
| Russell et al, 2010[ | Retrospective cross-sectional descriptive study | Evaluated anaphylaxis dx and tx of patients ≤21 yr (2002-2006) in pediatric ED (Children's Hospital of Alabama; Birmingham, AL); patients were identified using ICD-9 code for allergic rx and by 2ndSymposium criteria | n=124 cases from 740 patient visits with ICD-9 code related to allergic rx | Substantial lack of agreement on criteria used to define and identify anaphylaxis | Epinephrine, 51% Antihistamines, 92% Parenteral CCS, 78% | Prescription for epinephrine, 63% Referral to allergist, 33% | |
| Current Survey of US ED Providers | |||||||
| Russell et al, 2013 | Cross-sectional survey of US ED health care providers | Initial assessment of concordance between how US EDs manage aanaphylaxis and current guideline recommendations for diagnosis, treatment, discharge | n=207 EM providers (nurses, physician assistants, physicians) | Respondents reporting that in their EDs: No definition of anaphylaxis: 90% Definition of anaphylaxis based on current guidelines: 9% | Respondents reporting that in their EDs: Majority (>75%) of patients received epinephrine in ED: 42% ≤50% of patients received epinephrine in ED: 40% Antihistamines preferred in some EDs as first-line treatment | Respondents reporting that in their EDs: Majority (>75%) of patients received prescription for epinephrine: 48%; ≤50% of patients received prescription for epinephrine: 31% Referral to allergist for >50% of patients: 42%; for >75% of patients: 17% Written information about anaphylaxis: 95%; anaphylaxis action plan: 71% | |
| 1 |
Bohlke K, Davis RI, DeStefano F, Marcy SM, Braun MM, Thompson RS, et al. Epidemiology of anaphylaxis among children and adolescents enrolled in a health maintenance organization. J Allergy Clin Immunol 2004; 113:536-542.
doi: 10.1016/j.jaci.2003.11.033 pmid: 15007358 |
| 2 | Clark S, Camargo CA Jr. Epidemiology of anaphylaxis. Immunol Allergy Clin N Am 2007; 27:145-163. |
| 3 | Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World Allergy Organization guidelines for the assessment and management of anaphylaxis. J Allergy Clin Immunol 2011; 127: 593.e1-e22. |
| 4 | Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, et al. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol 2010; 126:477-480. |
| 5 |
Sampson HA, Munoz-Furlong A, Campbell R, Adkinson NF Jr, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report. Ann Emerg Med 2006; 47:373-380.
pmid: 16546624 |
| 6 |
Simons FE, Ardusso LRF, Bilo MB, Dimov V, Ebisawa M, El-Gamal YM, et al. 2012 update: World Allergy Organization Guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol 2012; 12:389-399.
doi: 10.1097/ACI.0b013e328355b7e4 pmid: 22744267 |
| 7 | Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: Report of the NIAID-sponsored expert panel. J Allergy Clin Immunol 2010; 126(suppl 1):S1-58. |
| 8 |
Russell S, Lozano D, Monroe K, Losek JD. Anaphylaxis management in the pediatric emergency department. Opportunities for improvement. Pediatr Emerg Care 2010; 26:71-76.
pmid: 20094000 |
| 9 |
Clark S, Bock SA, Gaeta TJ, Brenner BE, Cydulka RK, Camargo CA Jr. Muticenter study of emergency department visits for food allergies. J Allergy Clin Immunol 2004; 113:347-352.
doi: 10.1016/j.jaci.2003.10.053 pmid: 14767453 |
| 10 |
Clark S, Long AA, Gaeta TJ, Kamarthi GS, Camargo CA Jr. Multicenter study of emergency department visits for insect sting allergy. J Allergy Clin Immunol 2005; 116:643-649.
doi: 10.1016/j.jaci.2005.06.026 pmid: 16159637 |
| 11 | Beno SM, Nadel FM, Alessandri EA. A survey of emergency department management of acute urticaria in children. Pediatr Emerg Care 2007; 23:862-868. |
| 12 |
Klein JS, Yocum MW. Underreporting of anaphylaxis in a community emergency room. J Allergy Clin Immunol 1995; 95:637-638.
pmid: 7852677 |
| 13 | Camargo CA Jr. Potter Stewart and the definition of anaphylaxis. J Allergy Clin Immunol 2012; 129:753-754. |
| 14 |
Kastner M, Harada L, Waserman S. Gaps in anaphylaxis management at the level of physicians, patients, and the community: a systematic review of the literature. Allergy 2010; 65:435-444.
pmid: 20028373 |
| 15 | Arroabarren E, Lasa EM, Olaciregui I, Sarasqueta C, Munoz JA, Perez-Yarza EG. Improving anaphylaxis management in a pediatric emergency department. Ped Allergy Immunol 2010; 22:708-714. |
| 16 |
Grabenhenrich L, Hompes S, Gough H, Rueff F, Scherer K, Pfohler C, et al. Implementation of anaphylaxis management guidelines: A register-based study. PLOS one 2012; 7:e35778.
doi: 10.1371/journal.pone.0035778 pmid: 22590513 |
| 17 | Nowak R, Farrar JR, Brenner BE, Lewis L, Silverman RA, Emerman C, et al. Customizing anaphylaxis guidelines for emergency medicine. J Emerg Med 2013; Available at http://dx.doi.org/10.1016/j.jemermed.2013.01.018. |
| 18 |
Kemp SF, Lockey RF, Simons FER, on behalf of the World Allergy Oraganization ad hoc Committee on Epinephrine in Anaphylaxis. Epinephrine: the drug of choice for anaphylaxis. A statement of the World Allergy Organization. Allergy 2008; 63:1061-1070.
doi: 10.1111/j.1398-9995.2008.01733.x pmid: 18691308 |
| 19 |
Harduar-Morano L, Simon MR, Watkins S, Blackmore C. Algorithm for the diagnosis of anaphylaxis and its validation using population-based data on emergency department visits for anaphylaxis in Florida. J Allergy Clin Immunol 2010; 126:98-104.
doi: 10.1016/j.jaci.2010.04.017 pmid: 20541247 |
| 20 | Gaeta TJ, Clark S, Pelletier AJ, Camargo CA Jr. National study of US emergency department visits for acute allergic reactions 1993-2004. Ann Allergy Asthma Immunol 2007; 98:360-365. |
| 21 | Davis JE, Norris RL Jr. Allergic emergencies in children: the pivotal role of epinephrine. Ped Emerg Med Pract 2007; 4:1-28. |
| 22 |
Simons FER. Anaphylaxis. J Allergy Clin Immunol 2010; 125:S161-181.
pmid: 20176258 |
| 23 |
Pumphrey RSH. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy 2000; 30:1144-1150.
doi: 10.1046/j.1365-2222.2000.00864.x pmid: 10931122 |
| 24 |
Sicherer SH, Simons ER, the Section on Allergy and Immunology. Self-injectable epinephrine for first-aid management of anaphylaxis. Pediatrics 2007; 119:638-646.
doi: 10.1542/peds.2006-3689 pmid: 17332221 |
| 25 |
Bock SA, Munoz-Furlong A, Sampson HA. Fatalaties due to anaphylactic reactions to food. J Allergy Clin Immunol 2001; 107:191-193.
doi: 10.1067/mai.2001.112031 |
| 26 |
Andrews Al, Teufel RJ II, Basco WT Jr. Low rates of controller medication initiation and outpatient follow-up after emergency department visits for asthma. J Pediatr 2012; 160:325-330.
pmid: 21885062 |
| 27 |
Campbell RL, Luke A, Weaver Al, Decker WW, Kanthala AR, Bellolio MF, et al. Prescriptions for self-injectable epinephrine and follow-up referral in emergency department patients presenting with anaphylaxis. Ann Allergy Asthma Immunol 2008; 101:631-636.
doi: 10.1016/S1081-1206(10)60227-X pmid: 19119708 |
| 28 |
Campbell RL, Hagan JB, Li JT, Vukov SC, Kanthala AR, Smith VD, et al. Anaphylaxis in emergency department patients 50 or 65 years or older. Ann Allergy Asthma Immunol 2011; 106:401-406.
doi: 10.1016/j.anai.2011.01.011 pmid: 21530872 |
| 29 |
Decker WW, Campbell RL, Manivannan V, Luke A, St Sauver JL, Weaver A, et al. The etiology and incidence of anaphylaxis in Rochester Minnesota: A report from the Rochester Epidemiology Project. J Allergy Clin Immunol 2008; 122:1161-1165.
doi: 10.1016/j.jaci.2008.09.043 pmid: 18992928 |
| 30 |
Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics 2011; 128:e9-e17.
doi: 10.1542/peds.2011-0204 |
| 31 |
Huang F, Chawla K, Jarvinen KM, Nowak-Wegzyn. Anaphylaxis in a New York City pediatric emergency department: Triggers, treatments, and outcomes. J Allergy Clin Immunol 2012; 129:162-168.
doi: 10.1016/j.jaci.2011.09.018 pmid: 22018905 |
| 32 |
Ross MP, Ferguson M, Street D, Klontz K, Schroeder T, Luccioli S. Analysis of food-allergic and anaphylactic events in the National Electronic Injury Surveillance System. J Allergy Clin Immunol 2008; 121:166-171.
doi: 10.1016/j.jaci.2007.10.012 pmid: 18206508 |
| 33 |
Rudders SA, Banerji A, Katzman DP, Clark S, Camargo CA Jr. Multiple epinephrine doses for stinging insect hypersensitivity reactions treated in the emergency department. Ann Allergy Asthma Immunol 2010; 105:85-93.
doi: 10.1016/j.anai.2010.05.004 pmid: 20642208 |
| 34 |
Rudders SA, Banerji A, Corel B, Clark S, Camargo CA Jr. Multicenter study of repeat epinephrine treatments for food-related anaphylaxis. Pediatrics 2010; 125:e711-718.
doi: 10.1542/peds.2009-2832 pmid: 20308215 |
| [1] | Lori Stolz, Elaine Situ-LaCasse, Josie Acuña, Matthew Thompson, Nicolaus Hawbaker, Josephine Valenzuela, Uwe Stolz, Srikar Adhikari. What is the ideal approach for emergent pericardiocentesis using point-of-care ultrasound guidance? [J]. World Journal of Emergency Medicine, 2021, 12(3): 169-173. |
| [2] | Kasım Turgut, Erdal Yavuz, Mine Kayacı Yıldız, Mehmet Kaan Poyraz. Violence toward emergency physicians: A prospective-descriptive study [J]. World Journal of Emergency Medicine, 2021, 12(2): 111-116. |
| [3] | Marin Pavlov, Lucija Klobučar, Iva Klobučar, Kristina Žgela, Vesna Degoricija. Does shifting to professional emergency department staffing affect the decision for chest radiography? [J]. World Journal of Emergency Medicine, 2021, 12(2): 87-92. |
| [4] | Hady Zgheib, Aline El Zakhem, Cynthia Wakil, Mohamad Ali Cheaito, Rola Cheaito, Antoine Finianos, Ralphe Bou Chebl, Rima Kaddoura, Nader Al Souky, Imad El Majzoub. Role of urine studies in asymptomatic febrile neutropenic patients presenting to the emergency department [J]. World Journal of Emergency Medicine, 2021, 12(2): 99-104. |
| [5] | William Gilliam, Jackson F. Barr, Brandon Bruns, Brandon Cave, Jordan Mitchell, Tina Nguyen, Jamie Palmer, Mark Rose, Safura Tanveer, Chris Yum, Quincy K. Tran. Factors associated with refractory pain in emergency patients admitted to emergency general surgery [J]. World Journal of Emergency Medicine, 2021, 12(1): 12-17. |
| [6] | Rebekah Shaw, Erica Popovsky, Alyssa Abo, Marni Jacobs, Nicole Herrera, James Chamberlain, Andrea Hahn. Improving antibiotic prescribing in the emergency department for uncomplicated community-acquired pneumonia [J]. World Journal of Emergency Medicine, 2020, 11(4): 199-205. |
| [7] | Hai-jiang Zhou, Tian-fei Lan, Shu-bin Guo. Outcome prediction value of National Early Warning Score in septic patients with community-acquired pneumonia in emergency department: A single-center retrospective cohort study [J]. World Journal of Emergency Medicine, 2020, 11(4): 206-215. |
| [8] | Chuan-qi Ding, Yu-ping Zhang, Yu-wei Wang, Min-fei Yang, Sa Wang, Nian-qi Cui, Jing-fen Jin. Death and do-not-resuscitate order in the emergency department: A single-center three-year retrospective study in the Chinese mainland [J]. World Journal of Emergency Medicine, 2020, 11(4): 231-237. |
| [9] | Maybritt I. Kuypers, Adinda Klijn, Nieke E. Mullaart-Jansen, Frans B. Plötz. Availability and quality of procedural sedation and analgesia in emergency departments without emergency physicians: A national survey in the Netherlands [J]. World Journal of Emergency Medicine, 2020, 11(2): 69-73. |
| [10] | Emily Shao, Chantelle Judge, Erin McMeniman, Tina Bazianas, Rob Eley. Presenting patterns of dermatology conditions to an Australian emergency department [J]. World Journal of Emergency Medicine, 2020, 11(2): 74-78. |
| [11] | Zhenghong Liu, Mingwei Ng, Dinesh V. Gunasekeran, Huihua Li, Kishanti Ponampalam, R Ponampalam. Mobile technology: Usage and perspective of patients and caregivers presenting to a tertiary care emergency department [J]. World Journal of Emergency Medicine, 2020, 11(1): 5-11. |
| [12] | Wirachin Hoonpongsimanont, Preet Kaur Sahota, Yanjun Chen, Maria Nguyen, Christine Louis, Jonathan Pena, Andrew Wong, Maxwell Jen. Emergency department patient experience: Same location, same provider, different scores by different survey methods [J]. World Journal of Emergency Medicine, 2019, 10(3): 138-144. |
| [13] | Chang Pan, Xiao-ran Huang, Jiao-jiao Pang, Kai Cheng, Feng Xu, Yu-guo Chen. Trends in mortality of emergency departments patients in China [J]. World Journal of Emergency Medicine, 2019, 10(3): 152-155. |
| [14] | Rakesh Gupta, Isaac Siemens, Sam Campbell. The use of outcome feedback by emergency medicine physicians: Results of a physician survey [J]. World Journal of Emergency Medicine, 2019, 10(1): 14-18. |
| [15] | Elaine Situ-LaCasse, Ryan W. Grieger, Stephen Crabbe, Anna L. Waterbrook, Lucas Friedman, Srikar Adhikari. Utility of point-of-care musculoskeletal ultrasound in the evaluation of emergency department musculoskeletal pathology [J]. World Journal of Emergency Medicine, 2018, 9(4): 262-266. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
