Acute aortic occlusion (AAO) has been very rarely reported in the literature and is a potentially life-threatening emergency.[1⇓⇓⇓-5] AAO mostly occurs in cardiac disease patients,[1⇓⇓-4,6,7] and leads to cardiac complications.[1,2,5,6] Suprarenal aortic occlusion (SAO) is a very rare type of AAO, and infrarenal aortic occlusion (IAO) accounts for 75.8%-97.8%.[1,3,5⇓-7] SAO is different from IAO in some clinical manifestations, treatment strategies, and prognoses.[3,6⇓-8] SAO with cardiac disease will make the condition more complex and could easily cause a delay in diagnosis and portend worse outcomes with amputation and mortality rates.[1,3,6] Early and fast diagnosis and positive revascularization treatment are necessary to prevent cases from becoming fatal.[1⇓-3] Herein, we present a case series of SAO with cardiac disease.
CASE 1
A 73-year-old man was referred to the emergency department (ED) because of anasarca for 2 months and bilateral leg pain for 10 d, and the patient’s condition was aggravated and complicated with anuria for 1 d. His medical history included left hip surgery due to a car accident 5 years ago. Physical examination at admission showed blood pressure (BP) 187/98 mmHg (1 mmHg=0.133 kPa) and respiratory rate (RR) 20 breaths/min with 85% peripheral capillary oxygen saturation (SpO2) in room air. There were wet rales in both lungs. Pitting edema was observed in both lower limbs, with a strength of 1/5 degree. He also had weak femoral pulses on both sides. The laboratory and electrocardiogram data are shown in supplementary Table 1 (including data from cases 2 and 3). Computed tomography angiography (CTA) revealed total aortic occlusion of the superior mesenteric artery extending to the lumens of the caudal side of the iliac arteries and extensive collateralization (Figure 1A). The patient was diagnosed with SAO, heart failure, and multiple organ failure. Because the patient refused the operation and invasive treatment, heparin anticoagulation and supportive treatment were given. However, conservative treatments were insufficient to resolve the symptoms. The patient’s family asked for discharge several days later. The exterior changes in the lower limbs are shown in supplementary Figure 1.
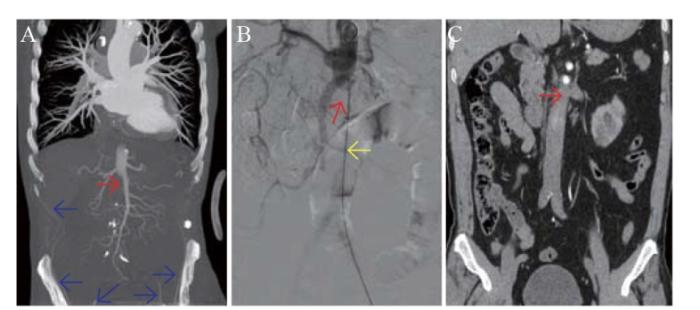
Figure 1.
Figure 1.
Arteriography in the three cases. A: coronal image from CTA in case 1 showing SAO and extensive collateralization; B: CTA in case 2 showing SAO; C: coronal image from CTA in case 3 showing SAO. The red arrows represent the SAO; the blue arrows represent the collateral vasculature; and the yellow arrow represents the guide wire. CTA: computed tomography angiography; SAO: suprarenal aortic occlusion.
CASE 2
A 43-year-old man visited the ED with sudden chest and abdominal pain for 5 h complicated by pain in both lower limbs. The patient had a medical history of hypertension, diabetes, and coronary artery disease (CAD). The patient underwent percutaneous coronary intervention two times (8 years and 10 d prior). He also had a left ventricular thrombus and right femoral vein thrombosis 1 month prior and had taken warfarin until the present time. Physical examination at admission showed BP 166/99 mmHg and RR 26 breaths/min with 85% SpO2 in room air. Wet rales were heard in both lungs. He had weak femoral pulses, and dorsalis pedis pulses were absent on both sides. In addition, both lower limbs had a low skin temperature, hypoactive function, numbness, and distending limb pain. Acute myocardial infarction (AMI) was added as a differential diagnosis, and emergency coronary arteriography was performed for diagnosis and treatment. We punctured the right femoral artery, but the guide wire could not be advanced from the bifurcation to the aorta, which led us to suspect the presence of AAO. Coronary arteriography from the left brachial artery indicated a diffuse lesion of multivessel stenosis and complete aortic occlusion of the suprarenal segment extending to the lumens of the common iliac arteries (Figure 1B). Then, CTA further verified the diagnosis of SAO. The patient had thrombophilia. The PROS1 gene had the NM-000313.3:exon2:c.234+1G>C mutation. The patient was given immediate endovascular treatment (EVT). He underwent successful Fogarty thrombectomy via femoral arteries and renal arterial stenting. He also received continuous intravenous infusion of heparin, antiplatelet therapy with aspirin 100 mg/d and clopidogrel 75 mg/d, continuous renal replacement therapy, antibiotics, and basic supportive care as postoperative therapy. Postoperative pathology verified that SAO was caused by ventricular thrombosis. The patient was discharged 1 month later.
CASE 3
A 71-year-old man who was referred to the ED presented with pain in both lower limbs and fatigue for 3 h. The patient had a medical history of hypertension, hypertensive cardiopathy, atrial fibrillation (AF), and cerebral infarction. His vital signs were within the normal range, except for BP, which was elevated at 189/119 mmHg. Femoral and pedal pulses were absent on both sides. The patient’s skin was pale over the lower limbs with coldness and mottled cyanosis, and the patient had sensory-motor deficits and gastrocnemius tenderness. Doppler ultrasound showed embolism of the lower limb arteries and arteriosclerosis on both sides, and CTA revealed total aortic occlusion extending from the level of the celiac trunk to the caudal side of the iliac arteries (Figure 1C). Fogarty thrombectomy was performed promptly. The postoperative therapy was the same as in case 2. Unfortunately, because of right leg necrosis, the patient underwent amputation 20 d later. The patient was discharged uneventfully 2 months after admission.
DISCUSSION
AAO is an emergent vascular condition. The etiologies are associated with embolism (especially cardiac large embolism), thrombosis, hypercoagulable states (such as AF), atherosclerosis, thrombophilia, and low cardiac output.[2⇓⇓-5,7,8] AAO occurs mostly in older patients with a history of cardiac disease and hypertension.[1⇓⇓-4,6,7] In our patients, case 2 involved CAD, large cardiac embolism, and hypertension, and case 3 involved hypertension, hypertensive cardiopathy, and AF. Grip et al[4] reported 715 AAO patients in a nationwide cohort study over a 20-year period and mentioned that cardiac disease (59.5%) and hypertension (56.6%) were the most frequent comorbidities. Furthermore, cardiac disease may be partly responsible for the high mortality.[4,7]
Clinical presentation and severity depend on the level and size of the aortic occlusion.[3,6⇓-8] The AAO symptoms are mainly lower limb ischemia represented by the classic 6-P signature (pain, paresthesia, paralysis, pulselessness, pallor, and poikilothermia).[2,3] SAO presents with more internal organ ischemia symptoms than IAO.[3,6⇓-8] Hence, SAO often presents with hypertensive crisis or uncontrolled hypertension, heart failure, chest pain, renal failure, and mesenteric ischemia.[3,6⇓-8] Heart failure and hypertension, which were present in case 1, are common cardiac symptoms/complications.[1,5,6]
CTA is the gold standard for the diagnosis of AAO.[2,5] Once AAO was suspected, CTA was performed immediately. CTA is sometimes delayed because of issues including vital instability, severe cardiac disease, contrast allergies, and renal inadequacy.[5,6] Ultrasound, especially point-of-care ultrasound, facilitates the early recognition of AAO. Hyperechoic intraluminal content and the absence of blood flow, representing thrombi, can be shown in ultrasound images.[2,5]
The management of AAO varies depending on etiology, age, cardiac comorbidities, and the location and size of the occluded vessel.[2,7] Treatment relies on anticoagulation and urgent surgery, such as EVT, axillo-bifemoral bypass, or aorto-bifemoral bypass.[2,7,8] Anticoagulation is initiated after the diagnosis and continued during and after the operation.[2,7,8] Permanent anticoagulation is suggested in patients with embolic AAO.[7] With increased availability and expertise in endovascular techniques, EVT is the first-line approach, especially in cases involving advanced age and cardiovascular comorbidities.[4,8] EVT performed in two of our patients achieved excellent technical success; it also resulted in a short recovery time and length of hospital stay. If adequate reperfusion via EVT is not possible, axillo-bifemoral bypass should be recommended.[2] For SAO, aorto-bifemoral bypass with branched grafts to the visceral arteries is suitable, especially in younger patients with lower rates of cardiac comorbidities.[2,3,6] SAO also requires additional operative interventions, such as limb amputations and renal reconstructions.[6,7]
CONCLUSION
AAO mostly occurs in cardiac disease patients. SAO is less common but is more severe and often leads to cardiac complications. The diagnosis of AAO should be suspected when there is sudden onset of lower limb ischemia symptoms in patients with cardiac disease or cardiac complications. EVT should be considered for SAO patients of advanced age who have cardiovascular comorbidities.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The author(s) declare no potential conflicts of interest.
Contributors: SQC, YLL, WJH, WXS and JNY were involved in the conception and design of the study. JZC, YLL and QC drafted the manuscript, JNY, WNS and QC drew the figures, and YLL, JZC, WJH and SQC were the major contributors in writing and revising the manuscript. All the authors have read and approved the final version of the manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Risk factors for perioperative mortality after revascularization for acute aortic occlusion
DOI:S0741-5214(18)30996-0
PMID:29945836
[Cited within: 9]

Acute aortic occlusion (AAO) is a life-threatening event necessitating prompt revascularization to the pelvis and lower extremities. Because of its uncommon nature, outcomes after revascularization for AAO are not well characterized. Our aim was to describe the perioperative morbidity and mortality associated with revascularization and to identify the patients at highest risk.A retrospective chart review was performed of patients who presented to our institution from 2006 to 2017 with acute distal aortic occlusion. Patients with a prior aortofemoral bypass were excluded, but those with aortoiliac stents were included. Baseline demographics and comorbidities, preoperative clinical presentation and imaging, procedural details, and postoperative hospital course were reviewed. The primary outcome was 30-day mortality, and major complications were evaluated as secondary outcomes. Logistic regression models were constructed to identify factors associated with 30-day mortality.We identified 65 patients who underwent revascularization for AAO. Median age was 63 years (range, 35-89 years), and 64.6% were male; 56.4% of patients presented within 24 hours of symptom onset, and 43.8% were treated within 6 hours of presentation. There were particularly high rates of prior coronary artery disease (62.3%) and chronic obstructive pulmonary disease (41.0%); 18.5% had prior iliac stents. Preoperative imaging in 44 patients showed occlusion of the inferior mesenteric artery in 36.0% and both internal iliac arteries in 34.7%. Treatments for revascularization included axillobifemoral bypass (55.4%), aortoiliac thromboembolectomy (15.4%), aortobifemoral bypass (13.9%), and aortoiliac stenting (15.4%). Overall 30-day mortality was 27.7% and was not affected by treatment modality. Mortality was highest in patients older than 60 years (40.5% vs 10.7%; P =.01) and those presenting with lactate elevation (45.5% vs 5.9%; P =.004) or motor deficit in at least one extremity (36.6% vs 9.5%; P =.03). Univariate predictors of 30-day mortality were age ≥60 years (odds ratio [OR], 5.68; 95% confidence interval [CI], 1.45-22.26; P =.01), presentation with motor deficit (OR, 5.48; 95% CI, 1.12-26.86; P =.04), presentation with elevated lactate level (OR, 13.33; 95% CI, 1.58-11.57; P =.02), history of prior stroke (OR, 4.80; 95% CI, 1.21-18.97; P =.03), and bilateral internal iliac artery occlusion (OR, 7.11; 95% CI, 1.54-32.91; P = .01). At least one postoperative complication was observed in 78.5% of patients, including acute kidney injury (56.9%, with 21.5% requiring hemodialysis), respiratory complications (46.2%), cardiovascular complications (33.9%), major amputation (15.4%, bilateral in 7.7%), and bowel ischemia (10.8%).Even with prompt revascularization and despite the chosen treatment modality, AAO carries high risk of mortality and numerous life-threatening complications. Older patients presenting with elevated lactate levels, motor deficit, and bilateral internal iliac artery occlusions are at the highest risk of perioperative mortality. These factors may aid in risk stratification and managing expectations in this critically ill population.Copyright © 2018 Society for Vascular Surgery. Published by Elsevier Inc. All rights reserved.
New appropriate use criteria for aortic stenosis patients
DOI:10.1016/j.jacasi.2023.02.003 URL [Cited within: 14]
A modern series of acute aortic occlusion
DOI:10.1016/j.jvs.2013.10.080
PMID:24393282
[Cited within: 15]

Acute aortic occlusion (AAO) is a rare condition associated with substantial morbidity and mortality. The most recent large series was published over 15 years ago and included patients from the 1980s. Previous studies reported up to 50% of AAOs are caused by embolization, with a mortality rate approaching 50%. We reviewed our recent experience with AAOs to identify current etiologies and outcomes in a contemporary series of patients with AAOs.Current Procedural Terminology codes and data from a prospectively maintained vascular surgical database were used to identify patients with acute occlusion of the native aorta between 2005 and July 2013. AAOs secondary to trauma, dissection, or graft occlusion were excluded.We identified 29 patients with AAOs treated at our institution. Twenty-three patients were transferred from referring hospitals with a mean transfer time of 3.9 hours (range, 0.5-7.5 hours). Twenty-two presented with occlusion below the renal arteries and seven with occlusion extending above the renal arteries. Resting motor/sensory lower extremity deficits were noted in 17 patients. Eight patients presented with complete paraplegia. Etiology was felt to be aortoiliac thrombosis in 22 cases, embolic occlusion in 2, and indeterminate in 5. Surgical revascularization was performed in 26 cases (extra-anatomic bypass in 18, thromboembolectomy in 5, and aortobifemoral bypass in 3 patients. Three patients had no intervention. Acute renal failure developed in 15 patients and rhabomyolysis in 10 patients. Fasciotomy was performed in 19 extremities. Nine extremities were amputated in six patients. Overall mortality was 34% with a 30-day mortality of 24% and a postprocedure mortality of 15%.AAO is an infrequent but devastating event. The dominant etiology of AAOs is now thrombotic occlusion. Despite advances in vascular surgery and critical care over the past 2 decades, associated morbidity and mortality remain substantial with high rates of limb loss, acute renal failure, rhabdomyolysis, and death. Mortality may be improved with expeditious extra-anatomic bypass.Copyright © 2014 Society for Vascular Surgery. Published by Mosby, Inc. All rights reserved.
Acute aortic occlusion
DOI:10.1161/CIRCULATIONAHA.118.036420 PMID:30615512 [Cited within: 7]
Point-of-care ultrasound diagnosis of acute abdominal aortic occlusion
DOI:10.5811/cpcem.2019.11.44311
PMID:32064433
[Cited within: 8]

Acute aortic occlusion is an emergent vascular condition not encountered routinely. Given its varied presentations, including neurovascular deficits and mimicking an acute abdomen, the diagnosis is often delayed causing increased morbidity and mortality. We present a case of acute abdominal aortic occlusion masquerading as sudden onset lower extremity pain and weakness in an 86-year-old female requiring emergent thrombectomy. This is only the second case report to discuss the use of point-of-care ultrasound to expedite diagnosis and management.1.Copyright: © 2020 Bloom et al.
Suprarenal aortic occlusion
PMID:8377231
[Cited within: 14]

This report was designed to elucidate the clinical manifestations of suprarenal aortic occlusion (SRAO) and determine the efficacy of surgical treatment.A retrospective review of 135 patients with aortic occlusion was undertaken from which the 16 patients (12%) with SRAO were found.Analysis yielded two subsets of patients based on the time-frame over which SRAO developed. Group I (n = 13) had chronic aortic occlusion with proximal propagation of thrombus to involve the suprarenal aorta. They had uncontrolled hypertension and claudication. Surgical treatment included 16 renal reconstructions (nine patients), two nephrectomies, 10 aortobifemoral bypasses, and three extra-anatomic procedures. The operative mortality rate was 23%. In contrast, group II (n = 3) had acute SRAO, manifest by profound lower extremity ischemia and acute renal failure after cardiac dysrhythmias. Two patients were moribund and died shortly after extraanatomic "salvage" procedures. One patient survived aortobifemoral and bilateral renal artery bypass.Chronic SRAO should be suspected in patients with absent femoral pulses and refractory hypertension. Aortic and renal reconstruction offers long-term improvement in hypertension control and relief of claudication. Acute SRAO is a multisystem disorder that is ineffectively managed with extraanatomic "salvage" procedures.
Acute aortic occlusion—factors that influence outcome
DOI:10.1016/s0741-5214(95)70188-5
PMID:7707562
[Cited within: 16]

The purpose of this study was to report our experience in the management of acute aortic occlusion and to analyze factors that influenced the outcome.This was a retrospective analysis of 48 patients with acute aortic occlusion treated over a 19-year period. Presentation included limb ischemia in 34, acute abdomen in four, spinal cord compression-like symptoms in eight, and sudden onset of hypertension in two patients. Thrombosis was the cause of acute aortic occlusion in 44, and embolus in four patients. Acute thrombosis was associated with underlying atherosclerotic occlusive disease in 36 patients. In these, thrombosis was due to low-flow state caused by cardiac dysfunction or severe volume depletion. Thrombosed aneurysms caused aortic occlusion in two patients. Hypercoagulable state caused thrombosis of relatively normal aorta in six patients. Angiography in 39 patients revealed occlusion to be juxtarenal or infrarenal in 37 and suprarenal in two. Left ventricular function (LVF) was assessed in 42 patients. Circulation was restored in 45 (aortofemoral bypass in 22, axillofemoral bypass in 12, and thromboembolectomy in 11). This was not feasible in three patients. Additional surgical procedures were required in 29 patients (64%).The overall mortality rate was 52% (25 of 48). Of the 20 patients with severely compromised LVF, 17 died (85%). In contrast, only five (23%) deaths occurred among 22 with good LVF. Among 29 patients who required additional operations, 18 died (62%). All four patients with embolic occlusion survived. Patients with normal LVF but hypercoagulable state had dismal outcome--only one of the six survived.Acute aortic occlusion is infrequent. Presentation may be varied, thus delaying diagnosis. Poor LVF, thrombosis of arteries below the inguinal ligament or of visceral arteries, and "hypercoagulable state" portend ominous prognosis.
Successful endovascular treatment for aortic thrombosis due to primary antiphospholipid syndrome: a case report and literature review