INTRODUCTION
World Health Organization (WHO) data suggest that between 1999 and 2019, the global burden of ischemic and hemorrhagic stroke increased significantly, with the absolute incidence of stroke and epidemic stroke increasing by 70% and 85%, respectively.[1] Ischemic stroke is one of the major causes of mortality, long-term disability, and the development of cognitive disorder.[2,3] Reperfusion therapy (RT) is the primar treatment for acute ischemic stroke (AIS). An earlier administration of RT is associated with a lower risk of in-hospital mortality and hemorrhagic transformation and better functional outcomes at 90 d after onset.[4] The 2019 American Heart Association and American Stroke Association guidelines recommend education and training for providers to ensure the timely use of thrombolysis and thrombectomy in ischemic stroke patients to improve patient outcomes and explore process improvement programs to optimize patient throughput.[5] One study has demonstrated that multidisciplinary cooperation with regular training and debriefing might also shorten the door-to-needle time (DNT), even during the coronavirus disease pandemic.[6] Most AIS patients receive treatment in the emergency department (ED) in China. Therefore, improving the organizational and emergency response abilities of ED staff is pivotal.
In situ simulation (ISS) enables teams to practice in a clinical environment in which genuine care is provided.[7] It has been shown to be a powerful tool for identifying and correcting latent safety threats and process improvement.[8] ISS is useful not only for optimizing flow but also for improving both technical and non-technical skills of healthcare workers. Prior work has shown that emergency medicine residents improved the checklist scoring of ventilator management in simulated critically ill patients after participating in an in situ simulation. This improvement persisted for eight months after the educational intervention.[9] Another study showed that the in situ simulation training improved the confidence and team cooperation skills of ED staff.[10]
ISS has been successfully used in all areas of medicine, including emergency medicine, obstetrics, and pediatrics. Ajmi et al[11] recently examined the use of ISS in the management of patients with acute stroke. The results showed that the implementation of a revised treatment protocol in combination with in situ simulation-based team training sessions could shorten the DNT from 27 min to 13 min and remained consistent after 13 months. Simultaneously, the proportion of patients who died or were bedridden decreased after 90 d. By implementing a dedicated program, Hassan et al[12] reduced the door-to-recanalization time by approximately 30%. Previous studies have optimized the workflow of patients with acute stroke using the ISS and achieved certain effects. However, patients with complications prior to RT were excluded.
Hypoxemia was defined as a desaturation nadir of SpO2 <90%, and severe hypoxemia was defined as SpO2 <70%.[13] Patients with acute stroke are at risk of respiratory compromise due to aspiration, upper airway obstruction, hypoventilation, and neurogenic pulmonary edema. The combination of poor perfusion and hypoxemia exacerbates and extends ischemic brain injury and has been associated with worse outcomes.[14] Early recognition of imminent airway loss and the timely administration of mechanical ventilation may prevent secondary neuronal injury due to hypoxemia. However, if it occurs before thrombolysis, it can result in delayed RT. Improving the emergency response capacity of healthcare workers is critical for shortening reperfusion time in patients with complications prior to thrombolysis.
Therefore, this study aimed to develop a comprehensive, high-simulation, multidisciplinary stroke simulation exercise to train emergency physicians, nurses, neurologists, and radiologists. In addition to assessing medical knowledge and technical skills, the simulation was designed to assess and reinforce teamwork and communication skills and to identify areas for improvement within our healthcare system. The goal was to shorten the reperfusion time for acute stroke patients with hypoxemia who required endotracheal intubation before thrombolysis.
METHODS
Setting and population
This study was conducted at a tertiary hospital in China in March 2021. During emergency interventions for acute stroke patients, the usual response teams include ED physicians, neurologists, ED nurses, and radiologists. This study included ED physicians, neurologists, nurses, and radiologists (n=53). Participants who had attended acute stroke training within the past 4 weeks were excluded. All participants volunteered to participate in this study.
Study design
This study had a pretest-posttest quasi-experimental design without a control group. The researchers obtained the baseline demographic data of the participants, including age, job tenure, and employment type. Participants underwent a self-reported comfort survey for emergency management (hypoxemia and endotracheal intubation) of acute stroke patients before simulation training. An educational intervention based on in situ simulation was then conducted, followed by an assessment of participants’ self-reported comfort and subjective experience after simulation training. In addition, the tracheal intubation time and door-to-image time on the first and second days of simulation training were recorded, and the door-to-image time was tracked in acute stroke patients at 4 months after the completion of simulation training. The time from a verbalized decision to intubation to the final endotracheal tube insertion and completion of the ventilator connection to leave the emergency room was considered the total intubation time.
Simulation scenario
Team Strategies & Tools to Enhance Performance & Patient Safety (Team STEPPS), an evidence-based framework for improving healthcare delivery, was used as the conceptual framework in this study to maximize team performance in healthcare delivery, with patient safety as the primary desired outcome (supplementary Figure 1).[15] The design of the simulation cases was based on the International Nursing Association Clinical Simulation and Learning standards of best practice.[16] All scenarios and learning objectives of the simulation case were developed and reviewed by a multidisciplinary team of neurologists, ED physicians, nurses, and radiologists to ensure accuracy, authenticity, and realism. Learning objectives, including medical knowledge, patient care, teamwork, and communication, were determined prior to simulation.
The simulation was conducted in an ED. Volunteers were trained in the role of standardized patients, who would show corresponding complaints and clinical symptoms at different stages of the visit according to pre-designed simulation cases, such as nausea, vomiting, seizures, and altered consciousness. The simulated scenarios included stroke patients admitted to the hospital due to limb hemiplegia, coma, hypoxemia, requiring urgent tracheal intubation, and complete computed tomography (CT) imaging after intubation. In addition, participants were also required to complete the evaluation of stroke patients in time after completing CT imaging to determine recanalization treatment options and shorten the recanalization time. The Noelle endotracheal intubation mannequin simulator (GaumardScience, USA) was used to facilitate participants to simulate tracheal intubation.
A total of 53 participants were divided into eight groups and received a two-day simulation training course with roles set according to typical staffing of six to seven people each, including two ED nurses, one ED physician, one neurologist, one radiologist, and one to two family members. The second day of training was mainly to repeat the simulation scenario as in the first day to optimize the simulation team training and improve the technical and non-technical skills of the participants. To determine the need for simulation training, participants were pre-tested, and their self-reported comfort scores in dealing with stroke patients and emergencies (hypoxemia and endotracheal intubation) were recorded. Participants were rated on a 5-point Likert scale ranging from 1 (very uncomfortable) to 5 (very comfortable). Participants were evaluated during the simulation by observers from key areas (emergency, neurology, and nursing) using standardized assessment forms with medical and teamwork/communication actions. The simulation training was preceded by debriefing using the advocacy-investigative reporting theoretical framework.[17] In addition, observers recorded the endotracheal intubation tiem and door-to-image time on the first and second days of simulation training. RT included thrombolytic drugs, interventional therapy, and surgery, and the emergency procedures were inconsistent between different treatments; however, CT examination was required for all stroke patients admitted to the hospital to confirm the diagnosis. Therefore, this study analyzed the difference in door-to-image time in stroke patients before and after simulation to shorten the overall reperfusion time.
Following the simulation, all teams were debriefed in a standardized format. Participants and observers shared observations regarding patient care, medical knowledge, teamwork, communication, and process improvement. Participants received didactic information on key medical topics following the simulation. At the conclusion of the debriefing sessions, participants completed voluntary, anonymous surveys regarding their simulation experience, comfort in managing the clinical scenarios (hypoxemia and endotracheal intubation) before and after training, and additional feedback and suggestions for the exercise.
Statistical analysis
All statistical analyses were performed using SPSS 25.0. The participants’ demographic data were described as the frequency and percentage of participants’ demographic data, and the tracheal intubation time and door-to-image time were described using mean±standard deviation. A paired-sample t-test was used to compare the mean self-reported comfort scores of participants, as well as the endotracheal intubation time and door-to-image time on the first and second days of in situ simulation training. The door-to-image time of acute stroke patients with hypoxemia requiring urgent endotracheal intubation was tracked before and after the simulation training to monitor temporal trends. P-values<0.05 were considered statistically significant.
RESULTS
Fifty-three participants responded to the questionnaires, of which 34 (64.2%) were ED nurses, eight (15.1%) ED physicians, nine (17.0%) neurologists, and two (3.8%) radiologists. The job tenure of the participants (n=53) ranged from two to 17 years. The age of the participants (n=53) ranged from 23 to 40 years.
Participants’ self-reported comfort scores before and after simulated training in response to emergencies (hypoxemia and tracheal intubation) are shown in Table 1. The difference is statistically significant before and after the simulated training.
Table 1. Comparison of self-reported comfort scores before and after simulated training in different clinical situations (n=53)
| Clinical situation | Self-reported comfort scores | t P-value | ||
|---|---|---|---|---|
| Pre-training | Post-training | |||
| Hypoxemia | 3.62±0.69 | 4.53±0.64 | -11.046 | <0.001 |
| Tracheal intubation | 3.43±0.72 | 3.98±0.72 | -6.940 | <0.001 |
The self-reported comfort scores of the participants with different employment types before and after the simulated training in response to emergencies (hypoxemia and tracheal intubation) are presented in Table 2.
Table 2. Comparison of self-reported comfort scores of different employment types of participants before and after simulated training in response to hypoxemia and endotracheal intubation
| Employment types | Hypoxemia | t | P-value | Endotracheal intubation | t | P-value | ||
|---|---|---|---|---|---|---|---|---|
| Pre-training | Post-training | Pre-training | Post-training | |||||
| Emergency department nurses (n=34) | 3.48±0.76 | 4.52±0.68 | -10.109 | <0.001 | 3.39±0.70 | 4.03±0.62 | -6.062 | <0.001 |
| Emergency department physicians (n=8) | 3.86±0.38 | 5.00±0.00 | -8.000 | <0.001 | 4.14±0.90 | 4.43±0.98 | -1.549 | 0.172 |
| Neurologists (n=9) | 4.13±0.35 | 4.63±0.52 | -2.646 | 0.033 | 3.13±0.35 | 3.88±0.35 | -4.583 | 0.003 |
| Radiologists (n=2) | 3.40±0.55 | 3.80±0.84 | -1.633 | 0.178 | 3.20±0.45 | 3.20±0.45 | / | / |
During the two-day simulation training, the endotracheal intubation time and door-to-image time were recorded. On the first day, the time for endotracheal intubation was 15.38±2.50 min, and the door-to-image time was 25.38±2.51 min. On the second day of simulation, the time for endotracheal intubation was reduced to 12.25±2.38 min (t=2.818, P=0.026), and the door-to-image time was reduced to 20.25±2.38 min (t=4.621, P=0.002).
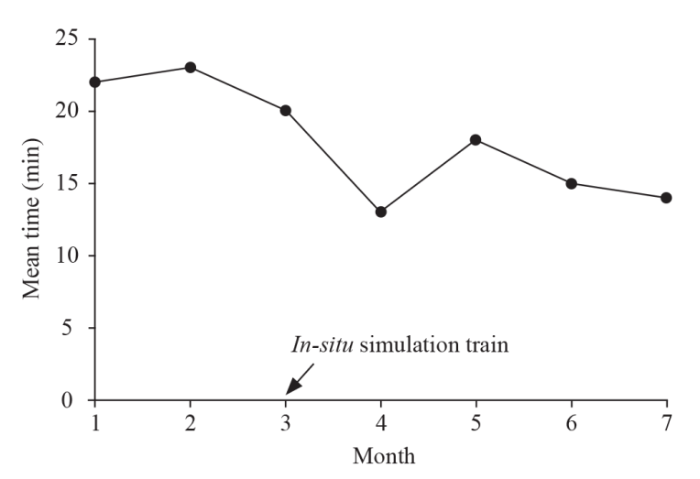
The door-to-image time was monitored for 4 months before initiating the simulation training and 4 months after the simulation training on patients with acute stroke complicated with hypoxemia who needed endotracheal intubation. We observed a decreasing trend in the door-to-image time, which continued after initiating the simulation training, as shown in Figure 1.
Figure 1.
Figure 1.
Linear trend of the door-to-image time.
Findings based on subjective outcomes showed that almost all participants rated simulated training as helpful, particularly in relation to the assessment system and communication/team cooperation components. Only radiologists believed that participating in this simulated training did not significantly improve their abilities during the exercise, and many participants became aware of areas of improvement in teamwork, communication, and first-aid processes. Participants and observers will be required to complete similar training exercises more frequently in the future. Overall, the simulation maintained a high degree of realism, with many participants reporting that they felt “stressed” during the patient’s endotracheal intubation, and many comments conveying that those participants considered the simulation to be very realistic.
DISCUSSION
In this study, we conducted a simulation training program for patients with hypoxemia-complicated AIS. During the implementation process, the ED of our hospital was selected to provide the participants with a real clinical setting. Medical students played the role of standardized patients, and the medical staff did not need to play other roles. In the context of anticipated simulation, this can help healthcare institutions improve their preparedness efforts, ultimately enhancing their response capabilities. At the end of the simulation training, the observer guided the participants to review the events, reflect, and give feedback to the participants to help them improve their knowledge and skills, establish clinical thinking, and optimize the process. By collecting subjective feedback from participants, we found that all participants had a high degree of recognition of the method of training, the degree of simulation, and the achievement of training goals. This finding supports previous research showing that adult learners retain more experience than they do in classrooms.[18]
In our study, neurologists and ED nurses reported higher self-reported comfort scores in dealing with hypoxemia and endotracheal intubation after in situ simulation training. ED physicians only had high self-reported comfort scores in managing hypoxemia after simulation training, and there was no difference in the management of endotracheal intubation. This may be related to the fact that ED physicians perform endotracheal intubation more frequently than other specialists. However, there was no significant difference in self-reported comfort scores between radiologists before and after the simulation. Their feedback on subjective experience showed that they felt pressure during the simulation process. This indicated that the simulation training program increased participants’ ability and confidence in dealing with changes in the disease. Similar results have been reported by other authors.[19]
In addition, we noted statistically significant improvements in in situ team performance. In this study, the endotracheal intubation time and door-to-image time after training were shorter than those before training. On the second day of simulation training, the door-to-image time of acute stroke patients with hypoxemia was shortened to 20.25±2.38 min. Previous guidelines have recommended that door-to-image time should be controlled within 25 min for patients with acute stroke.[4] When patients with hypoxemia required endotracheal intubation, this requirement was met in our simulation training. Thus, this length of time proves that our in situ simulation training scheme is effective.
Our study identified several areas of quality improvement. In the process of simulation training, not all physicians could accurately evaluate the actual and impending airway compromise and start the emergency response system in time. In addition, we found that not all nurses in EDs were able to prepare the equipment for endotracheal intubation correctly and cooperate well with physicians. One reason for this could be unfamiliarity with the process. We also found that the success rate of the first-time tracheal intubation among junior medical staff was low. Our future work will focus on strengthening airway management training.
After the simulation training, we found that the door-to-image time of acute stroke patients with hypoxemia required emergency endotracheal intubation decreased, and this trend continued after the simulation training. Although we cannot attribute this change entirely to the results of our simulation training, it is undeniable that the closed-loop communication, cooperation, and disease-reporting ability of team members have been significantly improved through the simulation training. This is important for EDs, in which patient conditions change rapidly.
This study has some limitations. First, this was an uncontrolled before-and-after intervention; there was no control group to compare the teaching methods, and the interval between the two simulation training sessions was short. Second, since this study partially relied on self-reported data, there could be a self-reporting bias. Additionally, we cannot completely attribute the reduction in the door-to-image time to our simulation.
CONCLUSIONS
This study demonstrated that the implementation of ISS training in an actual clinical environment with a multidisciplinary approach may improve the ability and confidence of stroke-team members, optimize the first-aid process, and effectively shorten the door-to-image time of stroke patients with emergency complications. Considering the low cost of running the simulations with the available resources and the positive feedback from the participants, ISS should be implemented extensively as a useful educational technique.
Funding: This study was supported by Hangzhou Construction Fund of Key Medical Disciplines (OO20200265); Zhejiang Medical and Health Science and Technology Plan Project (2020KY687); Hangzhou Science and Technology Development Project (20200401B04); Hangzhou Biomedical and Health Industry Development Supporting Technology Projects (2021WJCY256).
Ethical approval: The study was approved by the Ethics Committee of the Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine.
Conflicts of interest: The authors declare that they have no conflicts of interests.
Contributors: GYH drafted the manuscript. All authors had substantial contributions to the acquisition, analysis, or interpretation of data for the work; revising the work critically for important intellectual content; and final approval of the version to be published.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Orolingual angioedema during thrombolysis in acute ischemic stroke: A case report
Stroke in China: advances and challenges in epidemiology, prevention, and management
DOI:S1474-4422(18)30500-3
PMID:30878104
[Cited within: 1]

With over 2 million new cases annually, stroke is associated with the highest disability-adjusted life-years lost of any disease in China. The burden is expected to increase further as a result of population ageing, an ongoing high prevalence of risk factors (eg, hypertension), and inadequate management. Despite improved access to overall health services, the availability of specialist stroke care is variable across the country, and especially uneven in rural areas. In-hospital outcomes have improved because of a greater availability of reperfusion therapies and supportive care, but adherence to secondary prevention strategies and long-term care are inadequate. Thrombolysis and stroke units are accepted as standards of care across the world, including in China, but bleeding-risk concerns and organisational challenges hamper widespread adoption of this care in China. Despite little supporting evidence, Chinese herbal products and neuroprotective drugs are widely used, and the increased availability of neuroimaging techniques also results in overdiagnosis and overtreatment of so-called silent stroke. Future efforts should focus on providing more balanced availability of specialised stroke services across the country, enhancing evidence-based practice, and encouraging greater translational research to improve outcome of patients with stroke.Copyright © 2019 Elsevier Ltd. All rights reserved.
Significant contribution of aortogenic mechanism in ischemic stroke: observation of aortic plaque rupture by angioscopy
DOI:10.1016/j.jacasi.2022.07.009
PMID:36444317
[Cited within: 1]

Although embolic stroke accounts for most cerebral infarction, examinations to identify the embolic source have been insufficient. Nonobstructive general angioscopy (NOGA) has developed to allow the detailed observation of atheromatous changes of the aorta.The purpose of this study was to clarify the importance of the aortogenic mechanism in the development of ischemic stroke.We examined 114 consecutive patients whose aorta was observed by NOGA and who subsequently underwent brain magnetic resonance imaging to detect ischemic stroke lesions. In the evaluation of the aorta, the presence and location of spontaneously ruptured aortic plaque (SRAP) were determined. The aorta was observed from the origin to the arch (proximal aorta [PAo]) and the proximal descending aorta.Forty-nine of 114 patients had SRAP observed by NOGA. Among these, 24 had SRAP in the PAo, and 43 had SRAP in the descending aorta. Thirty-three patients had ischemic stroke lesions, including 6 with a clinical neurologic deficit. The frequency at which SRAP was detected in these patients was significantly higher in comparison to 81 patients without ischemic stroke (69% vs 33%; < 0.01). The sensitivity and specificity of the presence of SRAP for ischemic stroke were 0.70 and 0.68, respectively. The presence of SRAP in PAo was significantly correlated with ischemic stroke (odds ratio: 14.3; < 0.001).In the treatment of ischemic stroke, attention should be paid to SRAP, especially that in the PAo. (STROKE-NOGA [SponTaneously Ruptured aOrtic plaques as a potential cause of embolic stroKEs visualized by Non-Obstructive General Angioscopy] Study; UMIN000034588).© 2022 The Authors.
Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials
DOI:10.1016/S0140-6736(14)60584-5
PMID:25106063
[Cited within: 2]

Alteplase is effective for treatment of acute ischaemic stroke but debate continues about its use after longer times since stroke onset, in older patients, and among patients who have had the least or most severe strokes. We assessed the role of these factors in affecting good stroke outcome in patients given alteplase.We did a pre-specified meta-analysis of individual patient data from 6756 patients in nine randomised trials comparing alteplase with placebo or open control. We included all completed randomised phase 3 trials of intravenous alteplase for treatment of acute ischaemic stroke for which data were available. Retrospective checks confirmed that no eligible trials had been omitted. We defined a good stroke outcome as no significant disability at 3-6 months, defined by a modified Rankin Score of 0 or 1. Additional outcomes included symptomatic intracranial haemorrhage (defined by type 2 parenchymal haemorrhage within 7 days and, separately, by the SITS-MOST definition of parenchymal type 2 haemorrhage within 36 h), fatal intracranial haemorrhage within 7 days, and 90-day mortality.Alteplase increased the odds of a good stroke outcome, with earlier treatment associated with bigger proportional benefit. Treatment within 3·0 h resulted in a good outcome for 259 (32·9%) of 787 patients who received alteplase versus 176 (23·1%) of 762 who received control (OR 1·75, 95% CI 1·35-2·27); delay of greater than 3·0 h, up to 4·5 h, resulted in good outcome for 485 (35·3%) of 1375 versus 432 (30·1%) of 1437 (OR 1·26, 95% CI 1·05-1·51); and delay of more than 4·5 h resulted in good outcome for 401 (32·6%) of 1229 versus 357 (30·6%) of 1166 (OR 1·15, 95% CI 0·95-1·40). Proportional treatment benefits were similar irrespective of age or stroke severity. Alteplase significantly increased the odds of symptomatic intracranial haemorrhage (type 2 parenchymal haemorrhage definition 231 [6·8%] of 3391 vs 44 [1·3%] of 3365, OR 5·55, 95% CI 4·01-7·70, p<0·0001; SITS-MOST definition 124 [3·7%] vs 19 [0·6%], OR 6·67, 95% CI 4·11-10·84, p<0·0001) and of fatal intracranial haemorrhage within 7 days (91 [2·7%] vs 13 [0·4%]; OR 7·14, 95% CI 3·98-12·79, p<0·0001). The relative increase in fatal intracranial haemorrhage from alteplase was similar irrespective of treatment delay, age, or stroke severity, but the absolute excess risk attributable to alteplase was bigger among patients who had more severe strokes. There was no excess in other early causes of death and no significant effect on later causes of death. Consequently, mortality at 90 days was 608 (17·9%) in the alteplase group versus 556 (16·5%) in the control group (hazard ratio 1·11, 95% CI 0·99-1·25, p=0·07). Taken together, therefore, despite an average absolute increased risk of early death from intracranial haemorrhage of about 2%, by 3-6 months this risk was offset by an average absolute increase in disability-free survival of about 10% for patients treated within 3·0 h and about 5% for patients treated after 3·0 h, up to 4·5 h.Irrespective of age or stroke severity, and despite an increased risk of fatal intracranial haemorrhage during the first few days after treatment, alteplase significantly improves the overall odds of a good stroke outcome when delivered within 4·5 h of stroke onset, with earlier treatment associated with bigger proportional benefits.UK Medical Research Council, British Heart Foundation, University of Glasgow, University of Edinburgh.Copyright © 2014 Emberson et al. Open Access article distributed under the terms of CC BY. Published by Elsevier Ltd. All rights reserved.
Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association
Shortening door-to-needle time by multidisciplinary collaboration and workflow optimization during the COVID-19 pandemic
DOI:10.1016/j.jstrokecerebrovasdis.2021.106179 URL [Cited within: 1]
Role of in situ simulation for training in healthcare: opportunities and challenges
DOI:10.1097/ACO.0000000000000514
PMID:28968283
[Cited within: 1]

Simulation has now been acknowledged as an important part of training in healthcare, and most academic hospitals have a dedicated simulation center. In-situ simulation occurs in patient care units with scenarios involving healthcare professionals in their actual working environment. The purpose of this review is to describe the process of putting together the components of in-situ simulation for training programs and to review outcomes studied, and challenges with this approach.In-situ simulation has been used to 'test-drive' new centers, train personnel in new procedures in existing centers, for recertification training and to uncover latent threats in clinical care areas. It has also emerged as an attractive alternative to traditional simulations for institutions that do not have their own simulation center.In-situ simulation can be used to improve reliability and safety especially in areas of high risk, and in high-stress environments. It is also a reasonable and attractive alternative for programs that want to conduct interdisciplinary simulations for their trainees and faculty, and for those who do not have access to a fully functional simulation center. Further research needs to be done in assessing effectiveness of training using this method and the effect of such training on clinical outcomes.
The use of in situ simulation to detect latent safety threats in paediatrics: a cross-sectional survey
DOI:10.1136/bmjstel-2015-000037
URL
[Cited within: 1]

In situ simulation (ISS) has been reported as an innovative method to identify and mitigate latent safety threats (LSTs) in healthcare. Little is known about the current utilisation of ISS across academic simulation programmes.
In situ simulation for ventilator management in emergency medicine
DOI:10.1002/aet2.v4.4 URL [Cited within: 1]
Interdisciplinary in situ simulation-based medical education in the emergency department of a teaching hospital in Nepal
DOI:10.1186/s12245-019-0235-x
PMID:31455223
[Cited within: 1]

Simulation is well established as an effective strategy to train health care professionals in both technical and nontechnical skills and to prevent errors. Despite its known efficacy, adequate implementation is restricted due to the financial burden in resource-limited settings like ours. We therefore pursued to introduce cost-effective in situ simulation (ISS) in the emergency department (ED) to explore its impact on perception and learning experience among multidisciplinary health care professionals and to identify and remediate the latent safety threats (LST).This is a prospective cross-sectional study with a mixed method research design, which was conducted in the ED of Dhulikhel Hospital-Kathmandu University Hospital. The pretest questionnaire was used to determine baseline knowledge, attitude, and confidence of the staff. The ISS with minimal added cost was conducted involving multidisciplinary healthcare workers. The LSTs were recorded and appropriate remediation was performed. Voluntary post simulation feedback was collected after the sessions.Overall 56 staff participated in at least one of the 35 simulation sessions, among which 45 (80%) responded to the questionnaires`. Twenty participants (45.5%) were reluctant to use the defibrillator. The self-reported confidence level of using defibrillator was low 29 (64.6%). The knowledge score ranged from 0 to 8 with the median score of 3 and a mean of 3.29 ± 1.8. There was no statistically significant difference in knowledge scores among participants of different occupational backgrounds, previous training, duration of work experience, and previous use of a defibrillator. A total of 366 LSTs {individual (43%), medication (17%), equipment (4%), and system/team (36%)} were identified (10.45 LST per ISS). The overall feedback from the participants was positive. Eighty percent of participants reported increased skills to use a defibrillator, and 82% reported increased confidence for managing such cases. They also agreed upon the need and continuity of such type of simulation in their workplace.The baseline knowledge score and the confidence level of the staff were low. Self-reported feedback suggested increased confidence level and teamwork skills after ISS. It promoted identification and remediation of latent safety threats. ISS serves as a cost-effective powerful educational model that can be implemented even in settings where finances and space are limited.
Reducing door-to-needle times in stroke thrombolysis to 13 min through protocol revision and simulation training: a quality improvement project in a Norwegian stroke centre
DOI:10.1136/bmjqs-2018-009117
PMID:31256015
[Cited within: 1]

In eligible patients with acute ischaemic stroke, rapid revascularisation is crucial for good outcome. At our treatment centre, we had achieved and sustained a median door-to-needle time of under 30 min. We hypothesised that further improvement could be achieved through implementing a revised treatment protocol and in situ simulation-based team training sessions. This report describes a quality improvement project aiming to reduce door-to-needle times in stroke thrombolysis.All members of the acute stroke treatment team were surveyed to tailor the interventions to local conditions. Through a review of responses and available literature, the improvement team suggested changes to streamline the protocol and designed in situ simulation-based team training sessions. Implementation of interventions started in February 2017. We completed 14 simulation sessions from February to June 2017 and an additional 12 sessions from November 2017 to March 2018. Applying Kirkpatrick's four-level training evaluation model, participant reactions, clinical behaviour and patient outcomes were measured. Statistical process control charts were used to demonstrate changes in treatment times and patient outcomes.A total of 650 consecutive patients, including a 3-year baseline, treated with intravenous thrombolysis were assessed. Median door to needle times were significantly reduced from 27 to 13 min and remained consistent after 13 months. Risk-adjusted cumulative sum charts indicate a reduced proportion of patients deceased or bedridden after 90 days. There was no significant change in balancing measures (stroke mimics, fatal intracranial haemorrhage and prehospital times).Implementing a revised treatment protocol in combination with in situ simulation-based team training sessions for stroke thrombolysis was followed by a considerable reduction in door-to-needle times and improved patient outcomes. Additional work is needed to assess sustainability and generalisability of the interventions.© Author(s) (or their employer(s)) 2019. No commercial re-use. See rights and permissions. Published by BMJ.
STEPS-T program improves endovascular treatment outcomes of acute ischemic stroke: a 6-year study
DOI:10.3389/fneur.2019.01251
PMID:32116978
[Cited within: 1]

Early endovascular recanalization of occluded vessels in acute ischemic stroke (AIS) is a major contributor to good clinical outcome. We report the analysis of all AIS patients throughout a 6-year experience following the deployment of a quality initiative aiming at improving care, speed and maintaining quality for AIS treatment. Using a prospectively collected endovascular database at a comprehensive stroke center between 2012 and 2017, workflow/outcomes were recorded. There were no exclusion criteria. During the first year, a quality program employing "digital-object" technology, staff education, and workflow improvement was implemented to reduce time-to-treatment. Using electronic recording, workflow times were collected for onset (T), CT (T), door (T), angiography-suite (T), groin puncture (T), DSA (T), and recanalization (T). Recanalization time (T-T) and workflow intervals were compared at Year 1 and 6. Analysis of 382 patients (aged 71.3 ± 12.9) undergoing mechanical thrombectomy for AIS (206 male and 176 female) was performed. Recanalization time was significantly reduced from 82 min in 2012 to 34 min by 2017 (IQR 52-117 min and 23-49 min), a 59% reduction (< 0.001). Further, consistent year-over-year reductions in setup time (T-T) (44% improvement) and T to T times were observed. During the same period, clinical outcome significantly improved year-over-year as measured with the modified Rankin Scale 0-2 (33, 37, 38, 41, 53, and 58%). Significant improvements were observed following the deployment of a quality initiative enabling iterative evidence-based process improvements, thereby sustaining significant reductions in time-to-treat and improved clinical outcomes for AIS patients.Copyright © 2020 Hassan, Rabah, Preston and Tekle.
Association between hypoxemia and anemia following arthroplasty: a pilot clinical study
PMID:27168828
[Cited within: 1]

Hypoxia and anemia are common complications following joint arthroplasty. Whether hypoxia indicates that a patient is anemic and whether anemia causes a decline in arterial oxygen pressure accompanied by hypoxemia are not completely understood. The aim of the present study was to determine the association between hypoxemia and anemia following arthroplasty. A total of 135 patients who underwent arthroplasty at the China-Japan Friendship Hospital between January and May 2013 were retrospectively analyzed. The patients were divided into five groups depending on the type of arthroplasty they had experienced: Unilateral total knee arthroplasty (TKA), bilateral TKA, unilateral total hip arthroplasty (THA), bilateral THA or unilateral unicompartmental knee arthroplasty. Perioperative peripheral oxygen saturation (SpO2) and hemoglobin (Hb) levels were assessed, and the associations between the changes in SpO2 (ΔSpO2) and hemoglobin (ΔHb) levels on the first and third postoperative days (PODs) were analyzed using Pearson's correlation test for each group. The perioperative SpO2 curves for the various groups were typically at their lowest on the day of surgery. Significant hypoxemia was observed on POD 0-2, although a stable recovery curve was observed on POD 3-5. Trends in ΔHb were observed among the 5 groups, with the lowest Hb value observed predominantly on POD 2 and 3. By POD 4 and 5 Hb levels had recovered, with a steadily and consistently increasing curve. There was no statistically significant correlation between ΔSpO2 and decrease in Hb levels (P>0.05). SpO2 levels should not serve as a clinical indicator of the incidence and severity of anemia in patients who have undergone primary arthroplasty. To a point, the degree of postoperative anemic status does not affect SpO2 levels.
Association between physiological homeostasis and early recovery after stroke
PMID:11022093 [Cited within: 1]
TeamSTEPPS™: team strategies and tools to enhance performance and patient safety
Available at: https://www.ncbi.nlm.nih.gov/books/NBK43686/
INACSL standards of best practice for simulation: past, present, and future
PMID:26521497
[Cited within: 1]

To describe the historical evolution of the International Nursing Association for Clinical Simulation and Learning's (INACSL) Standards of Best Practice: Simulation.The establishment of simulation standards began as a concerted effort by the INACSL Board of Directors in 2010 to provide best practices to design, conduct, and evaluate simulation activities in order to advance the science of simulation as a teaching methodology.A comprehensive review of the evolution of INACSL Standards of Best Practice: Simulation was conducted using journal publications, the INACSL website, INACSL member survey, and reports from members of the INACSL Standards Committee.The initial seven standards, published in 2011, were reviewed and revised in 2013. Two new standards were published in 2015. The standards will continue to evolve as the science of simulation advances.As the use of simulation-based experiences increases, the INACSL Standards of Best Practice: Simulation are foundational to standardizing language, behaviors, and curricular design for facilitators and learners.
Debriefing with good judgment: combining rigorous feedback with genuine inquiry
The case for simulation as part of a comprehensive patient safety program
DOI:10.1016/j.ajog.2011.09.012
PMID:22000670
[Cited within: 1]

Simulation in obstetrics allows us to practice in a safe environment. Simulations can improve the performance of individuals and obstetric teams. The evidence is overwhelming that, with simulated practice, obstetricians improve their technical and communication skills. Evidence is emerging that simulation ultimately may improve clinical outcomes. It stands to reason that simulation in obstetrics should be incorporated into comprehensive patient safety programs.Copyright © 2012 Mosby, Inc. All rights reserved.
Simulation-based outreach program improves rural hospitals’ team confidence in neonatal resuscitation