INTRODUCTION
Heatstroke is a clinical syndrome characterized by imbalanced body temperature modulation, water/electrolyte disturbance, and nervous system dysfunction.[1] Heatstroke can be divided into classic heatstroke and exertional heatstroke (EHS). EHS occurs more often in workers, athletes, and military personnel engaged in heavy physical activity, and it is often accompanied by rhabdomyolysis (RM). Myoglobin (Mb) released as the result of RM has a critical effect on EHS, which is closely related to major organ functions.[2] Research shows that EHS accompanied by RM[3] usually presents comorbidities such as acute kidney injury (AKI),[4] acute hepatic injury (AHI),[5] diffuse intravascular coagulation (DIC),[6] or multiple organ dysfunction syndrome (MODS), with mortality and disability rates of 40%-70% and 30%, respectively.[1,7] Recent studies have shown that the mechanisms of organ damage include pyroptosis and ferroptosis.[8,9] In both pyroptosis and ferroptosis, a large number of damage-related molecular pattern (DAMP) molecules are released, causing systemic inflammatory reactions. Therefore, in the early stages of EHS, it is difficult to distinguish between intense inflammatory reactions triggered by RM and secondary infection.
Recently, C-reactive protein (CRP), white blood cells (WBCs), and procalcitonin (PCT) have been used to assess whether a patient is coinfected with bacteria and to guide antibiotic use.[10] However, other studies have shown that elevated serum PCT values can also be detected in the absence of bacterial infection in EHS.[11,12] Similarly, elevated serum PCT levels were not found in some severely infected patients. Therefore, the factors associated with elevated PCT levels and the relationship between dynamic PCT levels and organ function are not fully understood.
To avoid antibiotic overuse, it is important that in EHS patients admitted to the emergency department (ED), there is a distinction between an elevated PCT due to a secondary infection or an inflammatory response triggered by RM. Therefore, this retrospective study focused on the dynamic changes of biomarkers for inflammation and RM at four time points, namely, admission, 24 h and 48 h after admission, as well as discharge and outcomes of EHS patients, with the goal of better understanding the value of PCT in RM following EHS.
METHODS
Study design and subjects
Between January 2008 and June 2019, patients admitted to the intensive care unit (ICU) at the General Hospital of Southern Theatre Command of People’s Liberation Army were enrolled in this study. EHS patients were included based on the following criteria:[3,4] a history of strenuous exercise, exposure to a high temperature/humidity, nervous system impairment (such as coma, cognitive impairment, delirium), and an ultrahigh body temperature (core temperature > 40 °C). Patients who met the following criteria were excluded:[4] (1) dead or discharged 24 h postadmission; (2) insufficient data for extraction; (3) insufficient data on outcome measures acquired through telephone follow-up; or (4) a history of skeletal muscle disease.
Patient and public involvement
This study was approved by the Research Ethics Committee of General Hospital of Southern Theatre Command of People’s Liberation Army (HE-2020-09). The Ethics Committee waived the requirement for informed consent. During telephone follow-up, each patient was given detailed information about this research.
Research process
Patient data, including Glasgow Coma Scale (GCS) score, Sequential Organ Failure Assessment (SOFA) score, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, organ function assessments, biomarkers for inflammation and RM at admission, and 24 h and 48 h after admission, were extracted. Patients were classified into RM or non-RM groups based on whether Mb ≥1,000 ng/mL was present.[3] The basic clinical features, organ function injury, 90-day mortality, and inflammatory markers were examined. The relationship between PCT and other inflammatory markers, critical illness score, and outcomes in EHS was compared between the two groups.
Definitions
DIC:[12] International Society for Thrombosis and Hemostasis (ISTH) standard: an ISTH score ≥5 points.
AKI:[13] Kidney Disease: Improving Global Outcomes (KDIGO) standard: serum creatinine (Scr) increase to ≥26.5 µmol/L (≥0.3 mg/dL) in 48 h or ≥1.5-fold baseline value in 7 d, or urine amount <0.5 mL/(kg·h) for a 6-hour period.
Acute hepatic injury (AHI):[14] plasma international normalized ratio (INR) ≥1.5 and total bilirubin (TBIL) ≥34.2 µmol/L, accompanied by varying degrees of hepatic encephalopathy.
Lymphocytopenia:[15] absolute lymphocyte count <0.8×109/L observed more than two consecutive times during hospitalization.
Statistical analysis
Interquartile ranges (IQRs) were used to represent ordinal and enumeration data. To compare enumeration data, multiple independent samples of nonparametric Kruskal-Wallis H tests were used, while nonparametric Mann-Whitney U-tests were used to compare measurement data. The two-piecewise linear regression model and curve fitting were used to examine the relationship between PCT and RM. Statistical analysis was performed using SPSS 23.0 (SPSS Inc., USA), R (http://www.R-project.org) software, and Empower (R) (http://www.empowerstats.com, X&Y solutions, Inc., USA). Statistical significance was defined as P<0.05 (two-tailed).
RESULTS
Baseline characteristics and outcome
There were 162 patients in total, with the RM (n=56) and non-RM (n=106) groups having similar ages (24.0 [21.0-34.0] years vs. 20.0 [19.0-25.0] years, P=0.004), respectively (supplementary Figure 1). Due to their special occupations, most patients were male and physically healthy and had no inflammatory diseases. After admission, patients were treated according to the diagnosis and treatment principles of severe heatstroke. If patients had concurrent infections, antibiotics were added. Patients with RM had higher serum creatine kinase (CK), creatine kinase isoenzyme MB (CK-MB), and Mb levels, SOFA/APACHE II scores, and lower GCS scores than the non-RM group patients at the four time points (P<0.01). The incidence rates of AKI (75.0% vs. 26.9%, P<0.001), AHI (94.4% vs. 65.7%, P<0.001), DIC (57.8% vs. 25.8%, P<0.001) and 90-day mortality (33.9% vs. 2.8%, P<0.001) were all higher in the RM group than in the non-RM group (supplementary Table 1).
Dynamic changes in inflammatory markers
Among the different inflammatory markers, including lymphocytes, platelets, neutrophils, WBCs, PCT, and CRP, only PCT was associated with RM at the four time points (all P<0.001) (Table 1).
Table 1. Dynamic changes in inflammatory markers in EHS patients with or without RM
| Variables | Non-RM group (n=106) | RM group (n=56) | P-value |
|---|---|---|---|
| Admission | |||
| WBC, ×109/L, median (IQR) | 10.4 (8.6-13.7) | 13.2 (8.9-15.8) | 0.030 |
| Neutrophil, ×109/L, median (IQR) | 8.8 (6.5-11.1) | 10.0 (6.8-13.5) | 0.072 |
| Lymphocyte, ×109/L, median (IQR) | 1.1 (0.6-1.9) | 0.8 (0.5-1.8) | 0.398 |
| Platelets, ×109/L, median (IQR) | 169.0 (95.0-219.0) | 90.0 (51.2-166.2) | <0.001 |
| CRP, mg/dL, median (IQR) | 3.3 (1.1-6.7) | 3.4 (3.1-4.5) | 0.785 |
| PCT, ng/mL, median (IQR) | 1.4 (0.6-3.5) | 2.9 (1.4-4.8) | 0.004 |
| 24 h | |||
| WBC, ×109/L, median (IQR) | 9.2 (6.7-11.4) | 11.1 (7.8-14.3) | 0.007 |
| Neutrophil, ×109/L, median (IQR) | 6.9 (4.7-9.5) | 9.0 (6.7-12.8) | <0.001 |
| Lymphocyte, ×109/L, median (IQR) | 1.3 (1.0-1.9) | 0.7 (0.4-1.5) | <0.001 |
| Platelets, ×109/L, median (IQR) | 144.5 (88.5-186.5) | 57.0 (45.2-110.5) | <0.001 |
| CRP, mg/dL, median (IQR) | 3.4 (3.2-10.9) | 3.4 (3.2-7.4) | 0.415 |
| PCT, ng/mL, median (IQR) | 1.6 (0.8-3.0) | 3.4 (1.8-5.1) | <0.001 |
| 48 h | |||
| WBC, ×109/L, median (IQR) | 7.7 (6.2-9.7) | 6.8 (5.0-8.5) | 0.202 |
| Neutrophil, ×109/L, median (IQR) | 5.4 (4.2-7.5) | 6.8 (5.0-8.5) | 0.014 |
| Lymphocyte, ×109/L, median (IQR) | 1.4 (1.0-1.9) | 0.6 (0.3-1.4) | <0.001 |
| Platelets, ×109/L, median (IQR) | 136.0 (90.0-180.0) | 65.0 (45.0-104.0) | <0.001 |
| CRP, mg/dL, median (IQR) | 3.7 (3.3-13.0) | 3.4 (3.2-8.1) | 0.204 |
| PCT, ng/mL, median (IQR) | 1.1 (0.4-2.0) | 2.8 (1.5-4.8) | <0.001 |
| Discharge | |||
| WBC, ×109/L, median (IQR) | 6.7 (6.9-8.2) | 6.4 (5.7-10.4) | 0.700 |
| Neutrophil, ×109/L, median (IQR) | 4.2 (3.3-5.1) | 4.0 (3.3-8.0) | 0.443 |
| Lymphocyte, ×109/L, median (IQR) | 1.9 (1.4-2.3) | 1.7 (1.2-2.0) | 0.078 |
| Platelets, ×109/L, median (IQR) | 206.0 (161.2-273.2) | 217.0 (61.0-312.0) | 0.286 |
| CRP, mg/dL, median (IQR) | 3.4 (2.5-11.0) | 3.4 (3.2-17.4) | 0.635 |
| PCT, ng/mL, median (IQR) | 0.3 (0.1-0.7) | 2.9 (0.2-13.1) | <0.001 |
RM: rhabdomyolysis; WBC: white blood cell; CRP: C-reactive protein; PCT: procalcitonin; IQR: interquartile range.
Relationships between PCT and other inflammatory markers, critical illness score, and outcomes
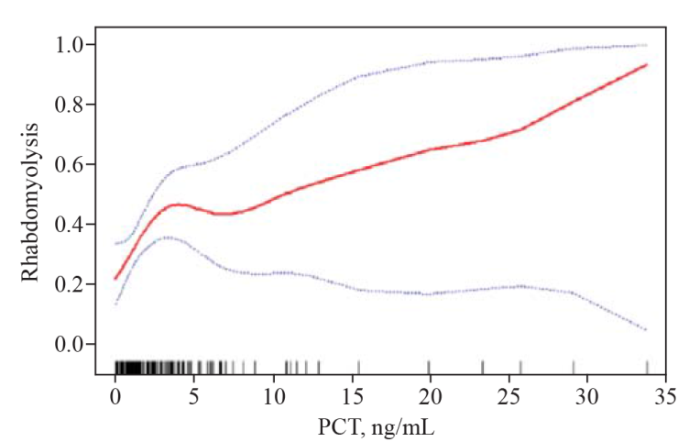
RM (Mb≥1,000 ng/mL), AHI, DIC, SOFA score and APACHE II score were all positively correlated with serum PCT level, with correlation coefficients of 0.214, 0.237, 0.285, 0.454, and 0.368, respectively (all P<0.05) (supplementary Table 2). The results of curve fitting revealed a nonlinear relationship between PCT and RM (Figure 1).
Figure 1.
Figure 1.
Curve fitting of PCT and RM in patients with EHS.
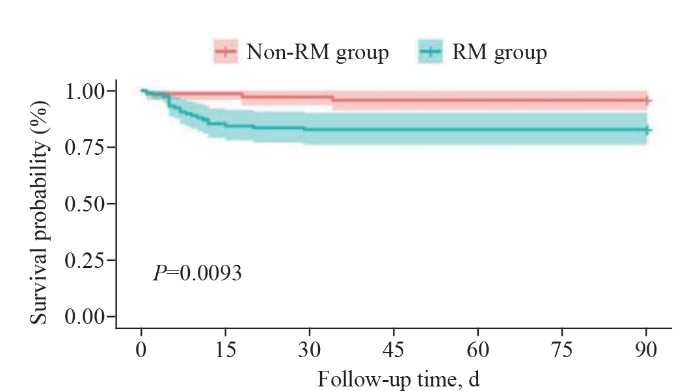
Using a two-piecewise linear regression model, there was a linear correlation in PCT and RM in Model I (odds ratio [OR] 1.1, 95% confidence interval [95% CI] 1.0-1.2, P=0.023) and a positive relationship between PCT level and RM only when PCT <4.6 ng/mL, with effect size (OR 1.3, 95% CI 1.0-1.6, P=0.049), and there were no effects in them when PCT ≥4.6 ng/mL (OR 1.0, 95% CI 1.0-1.1, P=0.352) (supplementary Table 3). The relationships between survival probability and PCT levels showed that RM patients had higher PCT levels and higher mortality than non-RM patients (P=0.0093) (Figure 2).
Figure 2.
Figure 2.
Survival analysis of the RM and non-RM groups.
DISCUSSION
PCT is a peptide precursor of calcitonin and is considered to be an inflammatory stressor that leads to systemic immune responses and increased protein production in the acute phase. Therefore, PCT is widely used in diseases such as infection, trauma and tumors. Especially in infected patients, PCT has been used to guide antibiotic use and predict patient prognosis.[10,11] However, whether PCT can be used to determine whether a patient with EHS has a secondary infection upon admission remains controversial. For example, some studies have suggested that EHS patients with elevated PCT on admission are associated with bacterial infection, and such patients are empirically treated with antibiotics based on PCT values. Other studies have suggested that elevated PCT in heatstroke patients does not indicate a coexisting bacterial infection. In our study, 34.6% of EHS were associated with RM, and PCT levels were significantly elevated in the RM group but not the CPR, a finding consistent with previous studies showing that elevated PCT in patients with heatstroke does not indicate that the patient is infected with bacteria.[16,17]
Data from this study showed that serum CK, CK-MB, Mb level, SOFA score and APACHE II score were higher in RM patients than in non-RM patients, and the incidence of AKI, AHI, DIC and 90-day mortality was also higher. This indicates that EHS patients with RM have serious organ damage. The main mechanisms include Mb released by RM directly blocking renal tubules, renal injury mediated by oxidative stress and released HMGB1 and H3 mediating liver cell injury and coagulation disorder, eventually leading to more serious organ injury or even death.[1,18,19]
Further analysis also found that PCT was associated with RM (Mb≥1,000 ng/mL), DIC, AHI, SOFA score and APACHE II score but not with lymphocytopenia, AKI, or 90-day mortality. The mechanism may be related to the release of intracellular substances into the circulation secondary to RM, which promotes the synthesis of PCT in the liver and leads to severe inflammatory reactions. However, because different tissues have different responses to PCT under the same inflammatory stress and many factors affect the prognosis of patients, the PCT level is related to the characteristics of injured tissues.[20,21]
To further clarify the relationship between PCT and RM, we used curve fitting and found that PCT and RM were not linearly correlated. Therefore, in this study, a piecewise linear regression model was used to find that a cut-off of PCT was 4.6 ng/mL. Therefore, when the PCT level is less than 4.6 ng/mL, the probability of RM occurrence increases with increasing PCT level. However, when the PCT level is greater than 4.6 ng/mL, it can be seen from the curve fitting diagram that the development trend of correlation between PCT and RM still exists, but the slope of the curve decreases. This is similar to the study on PCT and sepsis AKI.[22] These results indicate that PCT is not directly related to organ function injury, and there may be some confounding factors, such as subsequent and secondary infection, ischemia, and shock.
Therefore, for EHS patients in the ED with elevated PCT levels, clinicians should first determine whether RM has occurred and make a comprehensive judgment through detailed medical history inquiries combined with RM and other inflammatory indicators as well as imaging results to avoid the abuse of antibiotics. Second, the PCT level can indirectly reflect the degree of organ damage in patients, and relevant treatment can be given to patients in advance. Finally, we need to pay attention to confounding factors of PCT production and clearance to evaluate patient prognosis.
Limitations
Our study also had some limitations. First, this is a single-center study, which may reduce statistical efficiency. Later multicenter studies with a larger sample size are needed to determine the value of PCT in EHS or classic heatstroke. Second, due to the nature of the unit, our patients were all male, which may have led to statistical deviations. Third, since our study was a retrospective study with a long-time span, only data about WBCs, PCT and CRP were collected, while data about IL-6, IL-1β and TNF-α were not collected because of incomplete data. In the future, we will conduct a prospective study to include these three indicators to obtain more statistical evidence.
CONCLUSION
EHS patients with RM frequently have AKI, AHI, or DIC, which increases 90-day mortality. RM also has significantly elevated PCT, which should be interpreted cautiously in patients with EHS. High serum PCT levels have been associated with RM following EHS in young, critically ill patients.
Funding: The present study was funded by the National Natural Science Foundation of China (82072143, 81873943, 82360903); Sanming Project of Medicine in Shenzhen (SZSM20162011); Shenzhen Science and Technology Innovation Commission (JCYJ20190806163603504); Shenzhen Second People’s Hospital Clinical Research Fund of Guangdong Province High-level Hospital Construction Project (20203357014, 2023xgyj3357001, 2023yjlcyj022); Guizhou Science and Technology Planning Project (Guizhou Science and Technology Cooperation Support [2021] General 413); and PhD Start-up Fund (GYZYYFY-BS-2023[09]).
Ethical approval: This study was approved by the Research Ethics Committee of General Hospital of Southern Theatre Command of PLA (HE-2020-09).
Conflicts of interest: All authors declared no competing interests.
Contributors: LZ and FFS contributed equally to this work. MW and ZFL contributed to the study conception and design. LZ and CLW contributed to data collection. MW contributed to the statistical analysis. YYL and LZ contributed to manuscript drafting. ZFL and MW contributed to manuscript revision.
Reference
Development and evaluation of a predictive nomogram for survival in heat stroke patients: a retrospective cohort study
DOI:10.5847/wjem.j.1920-8642.2022.092
PMID:36119776
[Cited within: 3]

This study aimed to establish an effective nomogram to predict the survival of heat stroke (HS) based on risk factors.This was a retrospective, observational multicenter cohort study. We analyzed patients diagnosed with HS, who were treated between May 1 and September 30, 2018 at 15 tertiary hospitals from 11 cities in Northern China.Among the 175 patients, 32 patients (18.29%) died before hospital discharge. After the univariate analysis, mechanical ventilation, initial mean arterial pressure <70 mmHg, maximum heart rate, lab results on day 1 (white blood cell count, alanine aminotransferase, creatinine), and Glasgow admission prediction score were included in multivariate analysis. Multivariate Cox regression showed that invasive ventilation, initial mean arterial pressure <70 mmHg (1 mmHg=0.133 kPa), and Glasgow admission prediction score were independent risk factors for HS. The nomogram was established for predicting 7-d and 14-d survival in the training cohort. The nomogram exhibited a concordance index (C-index) of 0.880 (95% confidence interval [95% CI] 0.831-0.930) by bootstrapping validation (B=1,000). Furthermore, the nomogram performed better when predicting 14-d survival, compared to 7-d survival. The prognostic index cut-off value was set at 2.085, according to the operating characteristic curve for overall survival prediction. The model showed good calibration ability in the internal and external validation datasets.A novel nomogram, integrated with prognostic factors, was proposed; it was highly predictive of the survival in HS patients.Copyright: © World Journal of Emergency Medicine.
Association of D-dimer and acute kidney injury associated with rhabdomyolysis in patients with exertional heatstroke: an over 10-year intensive care survey
DOI:10.1080/0886022X.2021.2008975
PMID:34839765
[Cited within: 1]

Patients with rhabdomyolysis (RM) following exertional heatstroke (EHS) are often accompanied by dysfunction of coagulation and acute kidney injury (AKI). The purpose of this study was to investigate the relationship between D-dimer and AKI in patients with RM following EHS. A retrospective study was performed on patients with EHS admitted to the intensive care unit over 10-year. Data including baseline clinical information at admission, vital organ dysfunction, and 90-day mortality were collected. A total of 84 patients were finally included, of whom 41 (48.8%) had AKI. AKI patients had more severe organ injury and higher 90-day mortality (34.1 0.0%, < 0.001) than non-AKI patients. Multivariate logistic analysis showed that D-dimer (OR 1.3, 95% CI 1.1-1.7, = 0.018) was an independent risk factor for AKI with RM following EHS. Curve fitting showed a curve relationship between D-dimer and AKI. Two-piecewise linear regression showed that D-dimer was associated with AKI in all populations (OR 1.3, 95% CI 1.2-1.5, < 0.001) when D-dimer <10.0 mg/L, in RM group (OR 1.3, 95% CI 1.1-1.5, < 0.001) when D-dimer >0.4 mg/L, in the non-RM group (OR 6.4, 95% CI 1.7-23.9, = 0.005) when D-dimer <1.3 mg/L and D-dimer did not increase the incidence of AKI in the non-RM group when D-dimer >1.3 mg/L. AKI is a life-threatening complication of RM following EHS. D-dimer is associated with AKI in critically ill patients with EHS. The relationship between D-dimer and AKI depends on whether RM is present or not.
Sequential Organ Failure Assessment score for prediction of mortality of patients with rhabdomyolysis following exertional heatstroke: a longitudinal cohort study in Southern China
Clinical characteristics and risk factors associated with acute kidney injury inpatient with exertional heatstroke: an over 10-year intensive care survey
Characteristics and outcome of exertional heatstroke patients complicated by acute hepatic injury
DOI:10.14218/JCTH.2021.00307 PMID:34722174 [Cited within: 1]
Clinical characteristics and outcomes of patients with severe heatstroke complicated with disseminated intravascular coagulation: a case-control study
DOI:10.1016/j.thromres.2020.11.009 PMID:33212378 [Cited within: 1]
Disseminated intravascular coagulation in heat stroke: a hot topic
DOI:10.1097/CCM.0b013e31823d785d PMID:22425849 [Cited within: 1]
Heatstroke induces liver injury via IL-1β and HMGB1-induced pyroptosis
DOI:10.1016/j.jhep.2015.04.010
PMID:25931416
[Cited within: 1]

Liver injury is a common complication of heat stroke (HS), and often constitutes a direct cause for patient death. The cellular and molecular mechanism underlying HS-induced liver injury remains unclear. Recent evidence indicates that inflammasome plays an important role in mediating sterile inflammation triggered by tissue damage. Using a rat HS model, we identified a novel mechanism by which inflammasome-dependent interleukin-1β (IL-1β) activation and hepatocyte pyroptosis mediate HS-induced liver injury.To induce HS, rats were subjected to heat exposure. Inhibition of inflammasomes was achieved by RNA silencing and pharmacologic inhibitor prior to heat exposure. Inflammasome assembly, caspase-1 activation, histological changes, as well as serum levels of liver enzymes were measured.We demonstrated that the onset of HS activated inflammasome in the liver as evidenced by increased capase-1 activity and the association of inflammasome components NOD-like receptor family pyrin domain containing 3 (Nlrp3) and apoptosis speck-like protein containing a caspase-recruitment domain (ASC); and the activated inflammasome, in turn, induced IL-1β activation and hepatocyte pyroptosis, and subsequent augmented liver injury. HS-induced hepatocyte inflammasome activation seems to be high-mobility group box 1 (HMGB1) dependent. Inhibition of Nlrp3, caspase-1, or HMGB1 prevented HS-induced liver inflammation and ameliorated liver injury.These findings demonstrate an important role of HMGB1 in mediating inflammasome activation in the development of liver injury following HS, and suggest that targeting inflammasome may represent a novel therapeutic strategy to limit cell death and prevent liver failure after HS.Copyright © 2015 European Association for the Study of the Liver. All rights reserved.
Serum myoglobin modulates kidney injury via inducing ferroptosis after exertional heatstroke
Diagnostic value of PCT and CRP for detecting serious bacterial infections in patients with fever of unknown origin: a systematic review and meta-analysis
DOI:10.1097/PAI.0000000000000552
URL
[Cited within: 2]

It is vital to recognize the cause of an infection to enable earlier treatment. Studies have shown that procalcitonin (PCT) and C-reactive protein (CRP) have very high sensitivity and specificity for diagnosing serious bacterial infections (SBIs), with PCT performing better than CRP.
Serum procalcitonin predicting mortality in exertional heatstroke
Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation
DOI:10.1055/s-0037-1616068 URL [Cited within: 2]
Is procalcitonin a marker of critical illness in heatstroke?
DOI:10.1007/s00134-008-1083-y URL [Cited within: 1]
Characteristics and outcome of exertional heatstroke patients complicated by acute hepatic injury: a cohort study
DOI:10.14218/JCTH.2021.00084
PMID:34722180
[Cited within: 1]

Exertional heatstroke (EHS) is associated with strenuous physical activity in hot environments. The present study aimed to investigate dynamic changes of hepatic function indices in EHS patients and determine risk factors for death.This single-center retrospective cohort study considered all patients with EHS admitted to the intensive care unit at the General Hospital of Southern Theater Command of PLA from October 2008 to May 2019. Data on general characteristics, organ function parameters, and the 90-day outcome of enrolled patients were collected. Hepatic indices were collected dynamically, and patients with acute hepatic injury (AHI) were identified by plasma total bilirubin (TBIL) ≥34.2 µmol/L and an international normalized ratio ≥1.5, or with any grade of hepatic encephalopathy.In patients who survived, TBIL, alanine aminotransferase and aspartate aminotransferase were increased at 24 h, peaked at 2-3 days, and began to decrease at 5 days. In non-survivors, TBIL continuously increased post-admission. The area under the receiver operating characteristic curve for the prediction of mortality based on sequential organ failure assessment (SOFA) scores was 89.8%, and the optimal cutoff value was 7.5. Myocardial injury and infection were identified as independent risk factors for death in EHS patients with AHI.In EHS patients, hepatic dysfunction usually occurred within 24 h. Patients with AHI had more severe clinical conditions, and significantly increased 90-day mortality rates. SOFA scores over 7.5, complicated with myocardial injury or infection, were found to be risk factors for death in EHS patients with AHI.© 2021 Authors.
Sepsis pathophysiology, chronic critical illness, and persistent inflammation-immunosuppression and catabolism syndrome
DOI:10.1097/CCM.0000000000002074
PMID:27632674
[Cited within: 1]

To provide an appraisal of the evolving paradigms in the pathophysiology of sepsis and propose the evolution of a new phenotype of critically ill patients, its potential underlying mechanism, and its implications for the future of sepsis management and research.Literature search using PubMed, MEDLINE, EMBASE, and Google Scholar.Sepsis remains one of the most debilitating and expensive illnesses, and its prevalence is not declining. What is changing is our definition(s), its clinical course, and how we manage the septic patient. Once thought to be predominantly a syndrome of over exuberant inflammation, sepsis is now recognized as a syndrome of aberrant host protective immunity. Earlier recognition and compliance with treatment bundles has fortunately led to a decline in multiple organ failure and in-hospital mortality. Unfortunately, more and more sepsis patients, especially the aged, are suffering chronic critical illness, rarely fully recover, and often experience an indolent death. Patients with chronic critical illness often exhibit "a persistent inflammation-immunosuppression and catabolism syndrome," and it is proposed here that this state of persisting inflammation, immunosuppression and catabolism contributes to many of these adverse clinical outcomes. The underlying cause of inflammation-immunosuppression and catabolism syndrome is currently unknown, but there is increasing evidence that altered myelopoiesis, reduced effector T-cell function, and expansion of immature myeloid-derived suppressor cells are all contributory.Although newer therapeutic interventions are targeting the inflammatory, the immunosuppressive, and the protein catabolic responses individually, successful treatment of the septic patient with chronic critical illness and persistent inflammation-immunosuppression and catabolism syndrome may require a more complementary approach.
Markers for sepsis diagnosis: what is useful?
PMID:16893736
[Cited within: 1]

Timely diagnosis of the different severities of septic inflammation is potentially lifesaving because therapies that have been shown to lower mortality should be initiated early. Sepsis and severe sepsis are accompanied by clinical and laboratory signs of systemic inflammation but patients with inflammation caused by noninfectious causes may present with similar signs and symptoms. It is important to identify markers for an early diagnosis of sepsis and organ dysfunction. This article presents currently interesting sepsis biomarkers. Other novel markers and their potential role are discussed.
Diagnostic value of procalcitonin in patients with heat stroke
HMGB1-activatied NLRP3 inflammasome induces thrombocytopenia in heatstroke rat
DOI:10.7717/peerj.13799
URL
[Cited within: 1]

Thrombocytopenia, an early common complication in heatstroke (HS), has been widely considered as a mortality predictor of HS. The mechanism underlying thrombocytopenia in HS remains unknown. It is not known whether NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome is activated in HS platelet, which, in turn, induces platelet activation and thrombocytopenia. This study tried to clarify the activation of the NOD-like receptor signaling pathway under HS conditions and investigate its roles in mediating HS-induced thrombocytopenia.
Prognostic value of plasma exosomal levels of histone H3 protein in patients with heat stroke
DOI:10.3892/etm.2021.10354
PMID:34335883
[Cited within: 1]

Heat stroke (HS) is a condition that can lead to multiple organ dysfunction syndrome and death; however, there is no reliable method for stratifying mortality risk in HS. The abundance of exosomes in the circulation and their contents may be used as potential biomarkers of HS. The present study aimed to examine whether histone H3 levels in plasma exosomes could be used to determine HS prognosis. Blood samples were collected from patients with HS (36 survivors and 8 non-survivors) at admission to the intensive care unit and 4 days after admission. Blood samples were additionally collected from 15 healthy volunteers. Plasma exosomes were isolated using high-speed differential centrifugation. Correlation between histone H3 level and organ function and disease severity was examined. The results suggested differential expression and enrichment of histone H3 in the plasma exosomes of patients with HS (survivors, 249.3±04.6; non-survivors, 500.4±216.8; healthy controls, 161.1±52.49 pg/100 µg; P<0.05). The increased expression of histone H3 was associated with increased disease severity and duration. Plasma exosomal levels of histone H3 were significantly correlated with both organ dysfunction and disease severity (P<0.0001) and were significantly different between non-survivors and survivors (area under the receiver operating characteristic curve, 0.9668). A cutoff value of 307 pg/100 µg demonstrated optimized sensitivity (95%) and specificity (91.67%) for predicting mortality risk, suggesting that histone H3 levels in plasma exosomes may be a reliable biomarker for HS prognosis.Copyright: © Li et al.
Expert consensus on the diagnosis and treatment of heat stroke in China
Risk factors for the 90-day prognosis of severe heat stroke: a case-control study
DOI:10.1097/SHK.0000000000001589 URL [Cited within: 1]
Association between procalcitonin and acute kidney injury in patients with bacterial septic shock
DOI:10.1159/000512351
URL
[Cited within: 1]

Objective: The objective of this study was to assess the relationship between serum procalcitonin (PCT) and acute kidney injury (AKI) induced by bacterial septic shock. Methods: A retrospective study was designed which included patients who were admitted to the ICU from January 2015 to October 2018. Multiple logistic regression and receiver operating characteristic (ROC) as well as smooth curve fitting analysis were used to assess the relationship between the PCT level and AKI. Results: Of the 1,631 patients screened, 157 patients were included in the primary analysis in which 84 (53.5%) patients were with AKI. Multiple logistic regression results showed that PCT (odds ratio [OR] = 1.017, 95% confidence interval [CI] 1.009–1.025, p < 0.001) was associated with AKI induced by septic shock. The ROC analysis showed that the cutoff point for PCT to predict AKI development was 14 ng/mL, with a sensitivity of 63% and specificity 67%. Specifically, in multivariate piecewise linear regression, the occurrence of AKI decreased with the elevation of PCT when PCT was between 25 ng/mL and 120 ng/mL (OR 0.963, 95% CI 0.929–0.999; p = 0.042). The AKI increased with the elevation of PCT when PCT was either <25 ng/mL (OR 1.077, 95% CI 1.022–1.136; p = 0.006) or >120 ng/mL (OR 1.042, 95% CI 1.009–1.076; p = 0.013). Moreover, the PCT level was significantly higher in the AKI group only in female patients aged ≤75 years (p = 0.001). Conclusions: Our data revealed a nonlinear relationship between PCT and AKI in septic shock patients, and PCT could be used as a potential biomarker of AKI in female patients younger than 75 years with bacterial septic shock.