INTRODUCTION
Non-compressible torso hemorrhage (NCTH) remains a preventable cause of death from trauma.[1] Currently, early systemic fluid resuscitation or blood transfusion combined with effective hemostatic measures is often recommended to stabilize the physiological state of NCTH patients.[2] Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a readily attainable and effective early in-hospital and pre-hospital intervention for provisionally controlling hemorrhage from NCTH.[3,4]
REBOA is inherently associated with the burden of ischemia-reperfusion injury (IRI).[5] Existing evidence indicates that prolonged complete REBOA (cREBOA) leads to distal organ inflammation and injury.[6] Partial REBOA (pREBOA) can maintain the normal physiological state, reduce the impact of ischemia in the distal organs of the body, and avoid the occurrence of organ failure and prolongation of hospital stay after prolonged blocking time compared with cREBOA.[7,8] However, the overall survival of patients who underwent prolonged pREBOA did not significantly improve. Moreover, previous animal studies did not involve real injury models, present clinical scenarios of human trauma and blood loss, or perform long-term observation and evaluation after injury. Therefore, it is unclear whether the data from the macrovascular injury model can be extrapolated to hemorrhages from solid organ injury caused by an experimental sliding-chamber ballistic gun. Moreover, whether pREBOA improves the survival rate of animals with hemorrhage due to solid organ injury remains unknown.
The main purpose of this research was to compare the feasibility and effectiveness of pREBOA and cREBOA in a swine hemorrhagic shock model of liver penetrating injury. We also aimed to determine the effectiveness of pREBOA in a solid organ injury model and confirm the best pREBOA pattern for solid organ injury hemorrhage.
METHODS
Study design
This study used healthy adult, evirate male or nonpregnant female Landrace pigs weighing 55±10 kg. This study complied with the principles of the laboratory animal welfare and the guidelines for the protection and use of experimental animals of the National Research Council. Approval was obtained from the ethics committee of Tianjin Bairong Experimental Animal Breeding Technology Co., Ltd., before the start of the experiment (authorization number 2022001).
Animals were randomized into control (no aortic occlusion) (n=5), intervention with complete REBOA (cREBOA) (n=5), continuous pREBOA (C-pREBOA) (n=5), and sequential pREBOA (S-pREBOA) (n=5) groups. The animals were subjected to identical solid organ injury with uncontrolled hemorrhage and resuscitation.
Animal preparation
All animals were fasted for 12 h before the initiation of the experiment with free access to water. The animals were premedicated with 0.02 mg/kg atropine sulfate via intramuscular injection. After 30 min, anesthesia was induced via an intramuscular injection of Zoletil 50 (5 mg/kg; Virbac, France). Following endotracheal intubation, general anesthesia was maintained via intravenous infusion of Zoletil 50 (50 mg/h). The core temperature was maintained throughout the experiment (36.5-37.5°C) with a warming blanket. A gastric tube was inserted prior to the procedure.
The animals were placed in the supine position after the induction of anesthesia. The bilateral neck and inguinal areas and pectoral, liver, and renal regions were cleaned and depilated. Under ultrasound guidance (Philips, CX50, Netherlands), an artery catheter (Arrow, ES-04701, USA) was inserted at the left internal carotid artery for proximal blood pressure monitoring and proximal arterial blood sample collection. A jugular 8.5-F sheath (Edwards, 1300F85, USA) was inserted in the right internal jugular to allow access for Swan-Ganz pulmonary artery catheter (Edwards, 744F75, USA) placement, resuscitation, and proximal venous blood sample collection; the right femoral artery was intubated with a 14-F sheath (Cook, RCF-14.0-38-J, USA) to allow placement of a REBOA catheter (Cook, CODA-2-10.0-35-120-32, USA) and monitor distal blood pressure. After external measurement (from the femoral artery to the subxiphoid), the REBOA catheter was pushed to the level of the proximal descending branch of the thoracic aorta. Then, the monitor (Mindray, BeneVision N17, China) was connected.
Injury and intervention
The experiment was performed according to the defined procedure (supplementary Figure 1). After preparations were complete, a baseline blood sample was collected after the animals had stabilized for 30 min. The process of injury in animals has been described.[9] An ultrasound scan was performed to locate the lower edge of the liver at the end of exhalation and the lower border of the right rib cage at the end of inhalation; then, a line was drawn between them. The shooting point lied in this arc. The relative height between the shooting point and the highest point of the body surface on the arc (relative to the ground) was recorded as H (H=6 cm) (supplementary Figure 2). An experimental sliding-chamber ballistic gun was used for injury. The diameter and weight of the fragment simulation projectile were 6 mm and 1.1 g, respectively, and the initial velocity of the fragment was 785 m/s. The distance between the muzzle and the shooting point was 1.2 m. After shooting, the wound surface was covered with sterile dressing without pressure dressing. If the mean arterial pressure (MAP) decreased by 30% or more than the baseline value, the swine model of hemorrhagic shock caused by penetrating liver injury was successfully established.
The animals were subsequently randomized into a control group and three REBOA groups. The control group did not inflate the balloon. The MAP difference between proximal and distal was calculated in real time in the REBOA groups, which can judge the degree of aortic occlusion. cREBOA was attained using an aortic occlusion catheter inflated until the right femoral artery waveform disappeared. C-pREBOA was achieved using a standard aortic occlusion catheter inflated until the distal blood pressure gradually decreased by 60%-70% of the pressure gradient (water injection speed, 0.5 mL/min). In the cREBOA and C-pREBOA groups, the balloon was inflated for 60 min. In the S-pREBOA group, the balloon was then maximally inflated for 15 min to achieve full aortic occlusion; afterward, the balloon was slowly deflated until the distal blood pressure gradually decreased by 60%-70% of the pressure gradient and continued to decrease for 45 min. Then, the balloons were slowly deflated until distal arterial waveforms appeared. When the balloon was inflated, 1 mL of normal saline was pushed into the balloon every minute, and when the balloon was deflated, 0.5 mL of normal saline was discharged every minute.
Resuscitation was performed only after the completion of liver injury and shock. When the MAP decreased by 40% or more than the baseline value, fluid replacement therapy of 20 mL/kg was carried out. This scheme involved 250 mL colloids of hydroxyethyl starch 130/0.4 sodium chloride that were initially infused, and the rest was filled with 0.9% sodium chloride injection. The experiment was concluded when MAP < 30 mmHg (1 mmHg=0.133 kPa) or 180-min survival was achieved.
Data collection and analysis
Physiological indices, including heart rate, proximal and distal aortic pressure, and core temperature, and electrocardiography (ECG) were continuously monitored and recorded. Laboratory assessment was performed at baseline, shock after injury, and every 60 min after shock, including measurements of arterial blood gas, hematocrit (Hct), biochemical indicators, and serum cytokines. Immediately after animal euthanasia, tissue samples from the myocardium, liver, kidneys, and duodenum were collected for histological assessment using hematoxylin and eosin staining.
Statistical analysis
All data were statistically analyzed using SPSS version 22 (IBM Corp., USA). The distribution of continuous data was assessed using the Shapiro-Wilk test. Continuous variables with normal distribution were analyzed using analysis of variance or Student’s t-test. Variables with a nonnormal distribution were analyzed using the Mann-Whitney U-test or Kruskal-Wallis test as appropriate. The log-rank test was used for survival analysis. A P-value of less than 0.05 was considered significant.
RESULTS
The baseline characteristics of the animals were not significantly different (Table 1), similar to the baseline hemodynamic and metabolic indices (all P>0.05) (supplementary Table 1). All animals had penetrating liver injury and a similar degree of shock (P=0.77) (Table 1), and no significant differences were observed in the hemodynamic and laboratory values at various shock time points (all P >0.05) (supplementary Table 1). Without intervention, the condition of the animals deteriorated rapidly after liver injury, and the mean survival time was 57.60 min.
Table 1. Descriptive statistics of the physiological characteristics, injury status, and recovery status of all groups
| Parameters | Control (n=5) | cREBOA (n=5) | C-pREBOA (n=5) | S-pREBOA (n=5) | P-value |
|---|---|---|---|---|---|
| Weight, kg | 53.80±7.39 | 53.80±5.81 | 54.84±3.42 | 53.6±4.93 | 0.98 |
| Sex (male: female) | 2:3 | 4:1 | 4:1 | 3:2 | 0.74 |
| Total volume of blood loss, mL | 1136.30±270.07 | 493.14±127.31 | 882.88±202.49 | 852.11±68.57 | <0.01 |
| Shock index | 1.37±0.06 | 1.34±0.05 | 1.34±0.02 | 1.35±0.05 | 0.77 |
| Time to death, min | 57.60±32.69 | 161.00±42.49 | 129.60±73.56 | 145.00±50.50 | 0.03 |
Values are expressed as mean±standard deviation. The P values shown are the results of the analysis of variance with Bonferroni’s post hoc values. REBOA: resuscitative endovascular balloon occlusion of the aorta.
Table 1 also shows the features of the animals and responses to damage and intervention in terms of total volume of blood loss and time to death. The total blood loss volume was statistically lower in the cREBOA group compared with the other three groups (P<0.01). A marked difference was observed in the time of death among the four treatment groups (P=0.03). The average survival time after shock in the cREBOA group was 161.00 min, which was significantly longer than that in the control group.
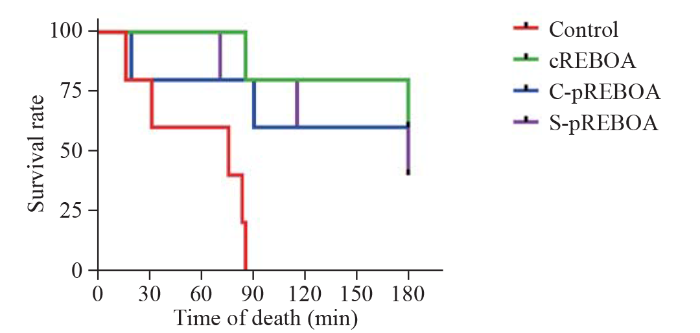
The Kaplan-Meier curves indicated overall survival (Figure 1). Compared with the control group, the survival rate of the REBOA groups was prominently improved (all P<0.05). Most of the animals in the control group died within 90 min after liver injury. No significant differences were found in the survival time among the REBOA groups.
Figure 1.
Figure 1.
Kaplan-Meier survival curve. REBOA: resuscitative endovascular balloon occlusion of the aorta.
Table 2 shows the hemodynamic and laboratory indices at various time points. At 60 min before the balloon was deflated, the REBOA groups had higher proximal blood pressure, lower pH, and higher Lac than the control group (all P<0.05). The Hct count was lower at 60 min in the control group and S-pREBOA group compared to that in the cREBOA group (all P<0.05). The alanine aminotransferase (ALT) at 60 min was significantly lower in the cREBOA group than in the control group (P<0.05). The creatinine concentration was lower at 60 min in the control group compared with the cREBOA or S-pREBOA group (all P<0.05). Compared with the C-pREBOA group, the final pH was significantly lower after 180 min in the cREBOA and S-pREBOA groups (P<0.05). The Hct count was higher in the cREBOA group than in the C-pREBOA and S-pREBOA groups at 120 min (all P<0.05). Compared to the cREBOA group, the ALT was higher at 120 min in the S-pREBOA group (P=0.039). At 120 min, the blood urea nitrogen was lower in the C-pREBOA group than in the cREBOA group (P<0.05).
Table 2. Comparison of hemodynamic and laboratory values among the four treatment groups
| Parameters | Control | cREBOA | C-pREBOA | S-pREBOA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 60 min | 60 min | 120 min | 180 min | 60 min | 120 min | 180 min | 60 min | 120 min | 180 min | ||||
| Hemodynamics | |||||||||||||
| HR, beats/min | 152.67±10.02 | 140.60±20.67 | 153.75±28.55 | 144.00±17.26 | 136.75±12.61 | 123.67±15.04 | 150.33±13.58 | 126.80±11.37 | 156.33±34.85 | 147.00±20.30 | |||
| SBP, mmHg | 86.33±17.95 | 138.40±18.04* | 94.00±21.56 | 100.00±28.55 | 145.75±6.99* | 94.33±26.31 | 100.33±16.50 | 134.60±14.01* | 103.00±19.70 | 103.67±13.01 | |||
| DBP, mmHg | 50.33±10.07 | 104.80±5.45* | 49.00±17.57 | 50.50±18.91 | 111.50±11.45* | 44.67±13.05 | 50.67±8.51 | 100.40±13.24* | 56.00±15.13 | 51.67±16.17 | |||
| MAP, mmHg | 65.67±10.50 | 115.80±8.87* | 63.50±19.30 | 66.75±21.48 | 123.00±9.49* | 61.33±17.79 | 67.00±11.14 | 111.20±11.19* | 71.33±12.10 | 69.00±14.00 | |||
| CVP, mmHg | 3.57±2.70 | 4.80±3.11 | 4.38±3.20 | 6.50±2.12 | 4.75±3.59 | 3.00±2.65 | 3.67±1.15 | 7.30±1.30 | 6.33±3.79 | 6.67±4.04 | |||
| CO, L/min | 1.88±0.92 | 3.36±1.11 | 4.00±1.46 | 3.25±0.33 | 4.15±1.29 | 4.37±2.87 | 3.93±2.51 | 4.74±2.20 | 3.57±0.67 | 2.70±1.40 | |||
| SVR, d·s-1·cm5 | 3470.0±1833.9 | 2642.2±1122.8 | 1182.3±345.1 | 1462.5±477.6 | 2430.5±1256.7 | 1488.0±875.1 | 1742.7±963.8 | 2223.2±1427.6 | 1622.0±342.2 | 2312.3±1080.0 | |||
| Laboratory indices | |||||||||||||
| pH | 7.44±0.05 | 7.19±0.09* | 7.14±0.07 | 7.13±0.08# | 7.24±0.11* | 7.21±0.02 | 7.30±0.02† | 7.14±0.07* | 7.19±0.03 | 7.21±0.03† | |||
| Lac, mg/dL | 9.97±3.62 | 14.24±2.02* | 17.15±1.49 | 17.73±1.64 | 14.45±1.19* | 15.33±1.47 | 14.00±3.40 | 16.18±1.51* | 15.87±2.11 | 16.27±1.54 | |||
| Hct, % | 25.33±2.08 | 32.40±2.70*ǃ | 34.00±1.41#ǃ | 28.00±4.08 | 27.50±4.43 | 26.00±2.65 | 28.67±3.79 | 25.80±3.42 | 29.00±3.46 | 29.33±5.51 | |||
| LDH, U/L | 2252.0±377.6 | 1752.4±415.2 | 2225.0±689.0 | 2168.8±518.2 | 1303.8±320.2* | 1867.7±539.3 | 2387.3±733.6 | 1830.2±520.4 | 2266.0±690.1 | 3030.3±532.6 | |||
| ALT, U/L | 35.00±10.00 | 17.80±4.60* | 27.00±10.30ǃ | 33.25±20.34 | 20.50±3.00 | 33.67±10.02 | 36.33±24.21 | 23.00±9.90 | 58.33±19.55 | 48.33±14.57 | |||
| Cr, mg/dL | 1.70±0.26 | 2.32±0.31* | 2.40±0.24 | 2.40±0.26 | 1.95±0.24 | 2.07±0.15 | 2.07±0.25 | 2.34±0.30* | 2.37±0.40 | 2.50±0.61 | |||
| BUN, mg/dL | 11.67±3.06 | 13.60±3.21 | 16.75±1.71# | 17.75±2.87 | 10.50±1.92 | 12.67±1.53 | 13.67±1.53 | 11.60±4.22 | 13.67±2.08 | 14.33±5.77 |
Values are expressed as mean±standard deviation. All REBOA groups compared with the control group using Dunnett’s t-test at 60 min (*P<0.05). Comparison between cREBOA and both C-pREBOA and S-pREBOA values at the respective time points using Student’s t-test (#P<0.05 for C-pREBOA, ǃP<0.05 for S-pREBOA); comparisons between C-pREBOA and S-pREBOA using t-test; †P<0.05. REBOA: resuscitative endovascular balloon occlusion of the aorta; HR: heart rate; bpm: beats per minute; SBP: systolic blood pressure; DBP: diastolic blood pressure; MAP: mean arterial pressure; CVP: central venous pressure; CO: cardiac output; SVR: systemic vascular resistance; Lac: lactate; Hct: hematocrit; LDH: lactate dehydrogenase; ALT: alanine aminotransferase; Cr: creatinine; BUN: blood urea nitrogen.
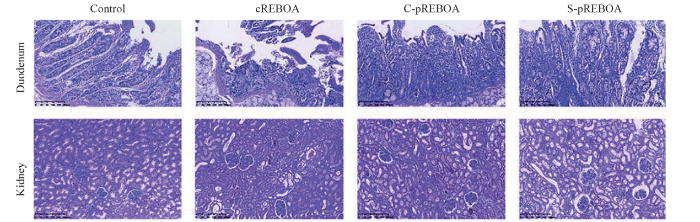
Under the light microscope, the kidney and duodenum showed ischemic injury with tissue loss in all REBOA groups. Representative kidney and duodenum samples harvested from all four groups are displayed in Figure 2. The duodenum tissue of the cREBOA group exhibited significant injury, as evidenced by villus hemorrhage and denudation and lamina propria inflammatory cell infiltration, compared with that in the pREBOA groups. The control group only showed patch disruption of the epithelial cells in the villi. The kidney tissue in the cREBOA group showed more necrotic areas with increased interstitial inflammatory cell infiltration compared to the specimen obtained from the pREBOA groups.
Figure 2.
Figure 2.
Standard histological examination of kidney and duodenum samples harvested with hematoxylin and eosin staining and magnified ×10. REBOA: resuscitative endovascular balloon occlusion of the aorta.
DISCUSSION
With the advancement of REBOA techniques for NCTH treatment, the complications of aortic occlusion are increasingly well known.[10] To overcome these complications, novel strategies are needed to maintain MAP while minimizing distal ischemia. However, the anatomical categories of NCTH are diverse;[2] hence, the specific causes of NCTH should be considered when studying the dispositions and adjunctive treatments, such as REBOA. Most animal studies related to REBOA have used vascular injury models, which may manifest differently when compared with models using other familiar causes of NCTH, such as solid organ injury or serious pelvic fractures. Therefore, this study used a swine model of liver injury and hemorrhage shock caused by an experimental sliding-chamber ballistic gun to analyze the effect of pREBOA and evaluate the situation 3 h after injury. The results suggested that pREBOA was able to improve the survival of subjects with solid organ injury while minimizing IRI after undergoing cREBOA. The C-pREBOA group showed a reduction in the severity of acidosis and end-organ injury.
NCTH is defined by high-grade injury present in one or more of the following anatomic domains: pulmonary, solid abdominal organ, major vascular or pelvic trauma; plus hemodynamic instability or the need for immediate hemorrhage control.[2] A limited number of hemostatic materials or facilities have been used in the field and hospital settings for the provisional therapy of NCTH, such as multifarious foaming agents and equipment for blocking the vessel[11] or fibrin sealants for diverse procedures.[12] Among them, REBOA is a temporary aortic hemostatic method for traumatic hemorrhage;[13] patients who underwent REBOA showed improved overall survival and a lower risk of early death compared with patients who underwent resuscitation.[14,15]
However, sustained use of REBOA is associated with IRI; in particular, prolonged zone I inflation to 45 or 60 min was fatal.[16,17] Thus, reducing the complications of zone I REBOA has become a hot topic around REBOA. An animal study found that pREBOA could better maintain the normal physiological status compared with cREBOA, reduce the ischemic load in those with serious hemorrhagic shock, and lessen the risks of metabolic and inflammatory impacts or organ dysfunction after resuscitation, allowing a longer intervention time.[7,18] A clinical study in Japan showed that undelayed deployment of REBOA without presenting impending cardiac arrest with shorter balloon occlusion (<30 min at zone I with partial occlusion) might be related to successful hemodynamic stabilization and improved survival.[19] Clinically, pREBOA might mitigate ischemic-organ injury but is not currently associated with improved survival in prolonged occlusion.[8] Furthermore, it is difficult to determine the specific advantages of pREBOA that can be used to develop more standardized methods. In addition, the ability to achieve renewable and reliable partial blocking using currently available devices is still unknown, and existing devices cannot strictly control flow. In order to accurately achieve pREBOA, we must optimize the strategy to minimize IRI and extend the tolerance time for aortic occlusion in Zone I.
In our study, we explored the practicality of utilizing simple balloon volume adjustment methods to effectively control NCTH. A study found that monitoring distal pressure and titrating percent balloon volume is feasible to manage pREBOA and that 60% balloon volume was enough inflation to elevate central pressure allowing distal perfusion.[20] Our study adopted two different partial methods to control NCTH and utilized proximal and distal MAPs for intervention, monitoring, and guidance. Complete and partial obstructed schedules were obviously beneficial in improving the survival of animals with liver injury at 180 min and the proximal blood pressure compared with the control group. However, no prominent difference was observed in the survival time of the partial groups. Moreover, among the above-mentioned hemostatic strategies, complete strategies can better control bleeding. Although early complete blocking for 15 min in the S-pREBOA group may be beneficial for the formation of clots, the total volume of blood loss did not significantly change compared with the control group. This result may be attributed to the fact that venous and portal bleeding caused by liver injury persisted even after REBOA inflation during the experiment. Alternatively, the sudden changes in blood pressure may have caused the blood clots to dislodge. Finally, marked differences were observed in the severity of organ injury and ischemic changes, with less injury observed in the C-pREBOA group than in the other groups. The severity of acidosis in the C-pREBOA group also showed significant improvement over time. This phenomenon may be due to the persistence of distal blood flow; moreover, the influence of proximal organ ischemia eventually reduced over time.
Limitation
The results demonstrated here are restricted to an animal model and may not be directly suitable for human patients. The study animals were frequently under anesthesia; hence, we were unable to evaluate their long-term outcomes or survival. The currently used devices are insufficient to achieve precise control of aortic occlusion. Finally, considering that long-term REBOA probably requires military-related scenarios, the resuscitation and schedule used were designed to mimic these conditions and are not suitable for dense civilian trauma centers.
CONCLUSION
In this trauma model with liver injury, a 60-minute pREBOA resulted in improved survival rate and was effective in maintaining reliable aortic pressure, despite persistent hemorrhage. Extended tolerance time for aortic occlusion in Zone I for NCTH is feasible with both continuous partial and sequential partial measures, and the significant improvement in the severity of acidosis and distal organ injury was observed in the sequential pREBOA. Although this study has limitations, it provides data that can serve as a reference for more comprehensive REBOA research.
Funding: The study was supported by military logistics scientific research project (AHJ16J004).
Ethical approval: This research was approved by ethics committee of Tianjin Bairong Experimental Animal Breeding Technology Co., Ltd., before the start of the experiment.
Conflicts of interest: The authors declare no conflicts of interest.
Contributors: TSL: study design, critical revision; YS: literature search, study design, data collection, data analysis, data interpretation, writing; YZ: literature search, study design, data collection, data analysis, data interpretation, writing; CCL: literature search, data collection, study conduct; JXG: literature search, data collection, study conduct; GGS: literature search, data collection.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
An online survey of non-compressible torso hemorrhage: training is needed
DOI:10.5847/wjem.j.1920-8642.2022.069 PMID:35837559 [Cited within: 1]
A review of treatments for non-compressible torso hemorrhage (NCTH) and internal bleeding
DOI:10.1016/j.biomaterials.2022.121432 URL [Cited within: 3]
Resuscitative endovascular balloon occlusion of the aorta in the treatment of severe hemorrhagic shock caused by upper gastrointestinal bleeding
Resuscitative endovascular balloon occlusion of the aorta (REBOA): update and insights into current practices and future directions for research and implementation
DOI:10.1186/s13049-020-00807-9
[Cited within: 1]

In this review, we assess the state of Resuscitative Endovascular Occlusion of the Aorta (REBOA) today with respect to out-of-hospital (OOH) vs. inhospital (H) use in blunt and penetrating trauma, as well as discuss areas of promising research that may be key in further advancement of REBOA applications.
The inflammatory sequelae of aortic balloon occlusion in hemorrhagic shock
DOI:10.1016/j.jss.2014.04.012
PMID:24836421
[Cited within: 1]

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a hemorrhage control and resuscitative adjunct that has been demonstrated to improve central perfusion during hemorrhagic shock. The aim of this study was to characterize the systemic inflammatory response associated and cardiopulmonary sequelae with 30, 60, and 90 min of balloon occlusion and shock on the release of interleukin 6 (IL-6) and tumor necrosis factor alpha.Anesthetized female Yorkshire swine (Sus scrofa, weight 70-90 kg) underwent a 35% blood volume-controlled hemorrhage followed by thoracic aortic balloon occlusion of 30 (30-REBOA, n = 6), 60 (60-REBOA, n = 8), and 90 min (90-REBOA, n = 6). This was followed by resuscitation with whole blood and crystalloid over 6 h. Animals then underwent 48 h of critical care with sedation, fluid, and vasopressor support.All animals were successfully induced into hemorrhagic shock without mortality. All groups responded to aortic occlusion with a rise in blood pressure above baseline values. IL-6, as measured (picogram per milliliter) at 8 h, was significantly elevated from baseline values in the 60-REBOA and 90-REBOA groups: 289 ± 258 versus 10 ± 5; P = 0.018 and 630 ± 348; P = 0.007, respectively. There was a trend toward greater vasopressor use (P = 0.183) and increased incidence of acute respiratory distress syndrome (P = 0.052) across the groups.REBOA is a useful adjunct in supporting central perfusion during hemorrhagic shock; however, increasing occlusion time and shock results in a greater IL-6 release. Clinicians must anticipate inflammation-mediated organ failure in post-REBOA use patients.Published by Elsevier Inc.
Distal organ inflammation and injury after resuscitative endovascular balloon occlusion of the aorta in a porcine model of severe hemorrhagic shock
DOI:10.1371/journal.pone.0242450
URL
[Cited within: 1]

Resuscitative Endovascular Balloon Occlusion of Aorta (REBOA) has emerged as a potential life-saving maneuver for the management of non-compressible torso hemorrhage in trauma patients. Complete REBOA (cREBOA) is inherently associated with the burden of ischemia reperfusion injury (IRI) and organ dysfunction. However, the distal organ inflammation and its association with organ injury have been little investigated. This study was conducted to assess these adverse effects of cREBOA following massive hemorrhage in swine.
Partial resuscitative endovascular balloon occlusion of the aorta in swine model of hemorrhagic shock
DOI:10.1016/j.jamcollsurg.2016.04.037 URL [Cited within: 2]
A feasibility study of partial REBOA data in a high-volume trauma center
DOI:10.1007/s00068-020-01561-4 [Cited within: 2]
Establishment of a high-velocity fragment-induced penetrating liver injury model in Landrace pigs
The complications associated with resuscitative endovascular balloon occlusion of the aorta (REBOA)
DOI:10.1186/s13017-018-0181-6 [Cited within: 1]
Surgical adjuncts to noncompressible torso hemorrhage as tools for patient blood management
Advances in topical hemostatic agent therapies: a comprehensive update
DOI:10.1007/s12325-020-01467-y
PMID:32813165
[Cited within: 1]

Severe hemorrhage causes significant metabolic and cellular dysfunction secondary to deficient tissue perfusion and oxygen delivery. If bleeding continues, hemodynamic destabilization, hypoxemia, multiple organ failure, and death will occur. Techniques employed to promote hemostasis include surgical suture ligatures, cautery, chemical agents, self-assembling nanoparticles, and physical methods, like mechanical pressure. Improved understanding of the natural clotting cascade has allowed newly designed agents to become more targeted for clinical and military use. Topically-applied hemostatic agents have enormous clinical applications in achieving hemostasis. This manuscript describes currently available and developing topical hemostatic materials, including topical active agents, mechanical agents, synthetic/hemisynthetic hemostatic agents, and external hemostatic dressings for clinical practice.
What’s new for trauma haemorrhage management?
DOI:10.12968/hmed.2019.80.5.268
PMID:31059346
[Cited within: 1]

Uncontrolled haemorrhage is the leading cause of preventable death from injury and is a major contributor to the global burden of disease. The majority of deaths resulting from bleeding occur within the first 3 hours of hospital admission, and the window for meaningful intervention is therefore extremely small. Resuscitative efforts during active bleeding should focus on maintaining haemostatic function with blood product transfusion and early administration of tranexamic acid. Achieving control of haemorrhage is the overarching treatment priority and may require temporising measures before definitive surgical or radiological intervention. This review summarizes the contemporary approaches to resuscitation of bleeding trauma patients, options for achieving haemorrhage control, and current areas of active research including organ protective resuscitation and suspended animation.
Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage
DOI:10.1097/TA.0000000000000809
PMID:26402524
[Cited within: 1]

Hemorrhage remains the leading cause of death in trauma patients. Proximal aortic occlusion, usually performed by direct aortic cross-clamping via thoracotomy, can provide temporary hemodynamic stability, permitting definitive injury repair. Resuscitative endovascular balloon occlusion of the aorta (REBOA) uses a minimally invasive, transfemoral balloon catheter, which is rapidly inserted retrograde and inflated for aortic occlusion, and may control inflow and allow time for hemostasis. We compared resuscitative thoracotomy with aortic cross-clamping (RT) with REBOA in trauma patients in profound hemorrhagic shock.Trauma registry data was used to compare all patients undergoing RT or REBOA during an 18-month period from two Level 1 trauma centers.There was no difference between RT (n = 72) and REBOA groups (n = 24) in terms of demographics, mechanism of injury, or Injury Severity Scores (ISSs). There was no difference in chest and abdominal Abbreviated Injury Scale (AIS) scores between the groups. However, the RT patients had lower extremity AIS score as compared with REBOA patients (1.5 [0-3] vs. 4 [3-4], p < 0.001). Of the 72 RT patients, 45 (62.5%) died in the emergency department, 6 (8.3%) died in the operating room, and 14 (19.4%) died in the intensive care unit. Of the 24 REBOA patients, 4 (16.6%) died in the emergency department, 3 (12.5%) died in the operating room, and 8 (33.3%) died in the intensive care unit. In comparing location of death between the RT and REBOA groups, there were a significantly higher number of deaths in the emergency department among the RT patients as compared with the REBOA patients (62.5% vs. 16.7%, p < 0.001). REBOA had fewer early deaths and improved overall survival as compared with RT (37.5% vs. 9.7%, p = 0.003).REBOA is feasible and controls noncompressible truncal hemorrhage in trauma patients in profound shock. Patients undergoing REBOA have improved overall survival and fewer early deaths as compared with patients undergoing RT.Therapeutic study, level IV.
Temporal changes in REBOA utilization practices are associated with increased survival: an analysis of the AORTA registry
DOI:10.1097/SHK.0000000000001586 URL [Cited within: 1]
Aortic branch vessel flow during resuscitative endovascular balloon occlusion of the aorta
DOI:10.1097/TA.0000000000002075
PMID:30252777
[Cited within: 1]

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a torso hemorrhage control adjunct. Aortic branch vessel flow (BVF) during REBOA is poorly characterized and has implications for ischemia-reperfusion injury. The aim of this study is to quantify BVF in hypovolemic shock with and without REBOA.Female swine (79-90 kg) underwent anesthesia, 40% controlled hemorrhage and sonographic flow monitoring of the carotid, hepatic, superior mesenteric, renal, and femoral arteries. Animals were randomized to REBOA (n = 5) or no-REBOA (n = 5) for 4 hours, followed by full resuscitation and balloon deflation for 1 hour.All animals were successfully induced into hemorrhagic shock with a mean decrease of flow in all vessels of 50% from baseline (p < 0.001). Deployment of REBOA resulted in a 200% to 400% increase in carotid flow, but near complete abolition of BVF distal to the balloon. The no-REBOA group saw recovery of BVF to 100% of baseline in all measured vessels, except the hepatic at 50% to 75%. two-way analysis of variance confirmed a significant difference between the groups throughout the protocol (p < 0.001). During resuscitation, the REBOA group saw BVF restore to between 25% and 50%, but never achieving baseline values. The lactate at 4 hours was significantly higher in the REBOA versus no-REBOA group (17.2 ± 0.1 vs. 4.9 ± 1.4; p < 0.001).REBOA not only abolishing BVF during occlusion, but appears to have a post-REBOA effect, reducing visceral perfusion. This may be a source of REBOA associated ischemia-reperfusion injury and warrants further investigation in order to mitigate this effect.
Resuscitative endovascular balloon occlusion of the aorta: review of the literature and applications to veterinary emergency and critical care
DOI:10.3389/fvets.2019.00197
PMID:31275952
[Cited within: 1]

While hemorrhagic shock might be the result of various conditions, hemorrhage control and resuscitation are the corner stone of patient management. Hemorrhage control can prove challenging in both the acute care and surgical settings, especially in the abdomen, where no direct pressure can be applied onto the source of bleeding. Resuscitative endovascular balloon occlusion of the aorta (REBOA) has emerged as a promising replacement to resuscitative thoracotomy (RT) for the management of non-compressible torso hemorrhage in human trauma patients. By inflating a balloon at specific levels (or zones) of the aorta to interrupt blood flow, hemorrhage below the level of the balloon can be controlled. While REBOA allows for hemorrhage control and augmentation of blood pressure cranial to the balloon, it also exposes caudal tissue beds to ischemia and the whole body to reperfusion injury. We aim to introduce the advantages of REBOA while reviewing known limitations. This review outlines a step-by-step approach to REBOA implementation, and discusses common challenges observed both in human patients and during translational large animal studies. Currently accepted and debated indications for REBOA in humans are discussed. Finally, we review possible applications for veterinary patients and how REBOA has the potential to be translated into clinical veterinary practice.
Blood pressure targeting by partial REBOA is possible in severe hemorrhagic shock in pigs and produces less circulatory, metabolic and inflammatory sequelae than total REBOA
DOI:S0020-1383(18)30556-4
PMID:30301556
[Cited within: 1]

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is an effective adjunct in exsanguinating torso hemorrhage, but causes ischemic injury to distal organs. The aim was to investigate whether blood pressure targeting by partial REBOA (pREBOA) is possible in porcine severe hemorrhagic shock and to compare pREBOA and total REBOA (tREBOA) regarding hemodynamic, metabolic and inflammatory effects.Eighteen anesthetized pigs were exposed to induced controlled hemorrhage to a systolic blood pressure (SBP) of 50 mmHg and randomized into three groups of thoracic REBOA: 30 min of pREBOA (target SBP 80-100 mmHg), tREBOA, and control. They were then resuscitated by autologous transfusion and monitored for 3 h. Hemodynamics, blood gases, mesenteric blood flow, intraperitoneal metabolites, organ damage markers, histopathology from the small bowel, and inflammatory markers were analyzed.Severe hemorrhagic shock was induced in all groups. In pREBOA the targeted blood pressure was reached. The mesenteric blood flow was sustained in pREBOA, while it was completely obstructed in tREBOA. Arterial pH was lower, and lactate and troponin levels were significantly higher in tREBOA than in pREBOA and controls during the reperfusion period. Intraperitoneal metabolites, the cytokine response and histological analyses from the small bowel were most affected in the tREBOA compared to the pREBOA and control groups.Partial REBOA allows blood pressure titration while maintaining perfusion to distal organs, and reduces the ischemic burden in a state of severe hemorrhagic shock. Partial REBOA may lower the risks of post-resuscitation metabolic and inflammatory impacts, and organ dysfunction.Copyright © 2018. Published by Elsevier Ltd.
Partial occlusion, conversion from thoracotomy, undelayed but shorter occlusion: resuscitative endovascular balloon occlusion of the aorta strategy in Japan
DOI:10.1097/MEJ.0000000000000466
PMID:28328730
[Cited within: 1]

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a viable alternative to resuscitative thoracotomy (RT) in refractory hemorrhagic patients. We evaluated REBOA strategies using Japanese multi-institutional data.The DIRECT-IABO investigators registered trauma patients requiring REBOA from 18 hospitals. Patients' characteristics, outcomes, and time in initial treatment were collected and analyzed.From August 2011 to December 2015, 106 trauma patients were analyzed. The majority of patients were men (67%) (median BMI of 22 kg/m, 96% blunt injured). REBOA occurred in the field (1.9%, all survived >30 days), emergency department (75%), angiography suite (17%), and operating room (1.9%). Initial deployment was at zone I in 93% and partial occlusion in 70% of cases. RT and REBOA were combined in 30 patients (RT+REBOA group) who showed significantly higher injury severity score (44 vs. 36, P=0.001) and chest abbreviated injury scale (4 vs. 3; P<0.001) than the REBOA-alone group (n=76). Frequent cardiopulmonary resuscitation (73%), longer prothrombin time-international normalised ratio, lower pH, and higher lactate were observed in the RT+REBOA. Among 24 h nonsurvivors (n=30) of the REBOA alone, preocclusion systolic blood pressure was lower (43 vs. 72 mmHg; P=0.002), indicating impending cardiac arrest, and duration of occlusion was longer (60 vs. 31 min; P=0.010). In the RT+REBOA (n=30), six survived beyond 24 h, three beyond 30 days, and achieved survival discharge.Partial occlusion was performed in 70% of patients. Undelayed deployment of REBOA without presenting impending cardiac arrest with shorter balloon occlusion (<30 min at zone I with partial occlusion) might be related to successful hemodynamic stabilization and improved survival. Further evaluation should be performed prospectively.
Distal pressure monitoring and titration with percent balloon volume: feasible management of partial resuscitative endovascular balloon occlusion of the aorta (P-REBOA)
DOI:10.1007/s00068-019-01257-4 [Cited within: 1]