Several factors can contribute to the formation of aneurysms, including hemodynamic changes, polyarteritis nodosa, bacterial endocarditis, vasculitis, fibromuscular dysplasia, vascular malformation, and cystic medial necrosis.[1,2] Surgery is recommended for splenic artery aneurysms (SAAs) greater than 25 mm in diameter, and several surgical approaches are used, including open surgery, laparoscopic surgery, and percutaneous embolization. Laparoscopic surgery might be associated with an increased risk of pancreatic leakage compared to the open surgery approach. Open surgery without complete aneurysm resection should be preferred for patients with large SAAs in close contact with the pancreas. Here, we report a patient with two splenic artery aneurysms.
CASE
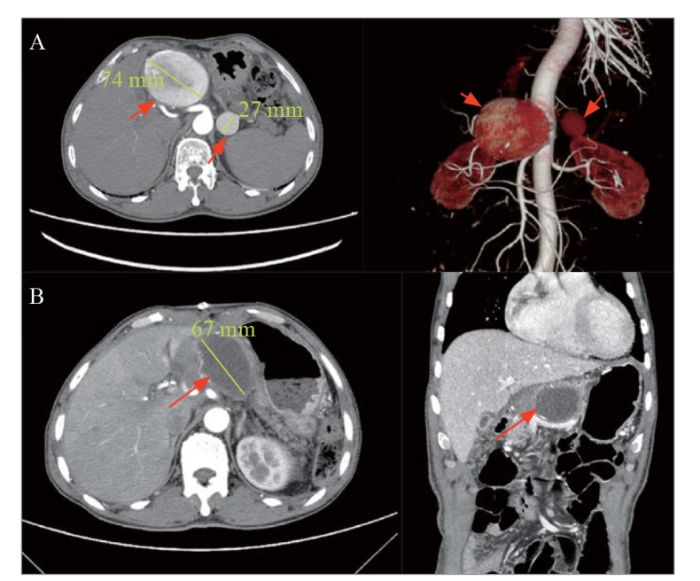
A 70-year-old male patient, a native resident of Hangzhou, was admitted to the emergency department with acute abdominal pain. He had a three-year history of hypertension that was treated with valsartan. During physical examination, a large pulsatile mass in the left upper abdomen and mild abdominal tenderness in the left abdomen were noted. Laboratory tests, including routine blood examination, electrolytes, amylase, liver function tests, X-rays, and electrocardiogram, were normal. However, computed tomography angiography (CTA) revealed a rare anatomical variation of the splenic artery arising from the hepatic artery. Additionally, one SAA measuring 74 mm in diameter in the proximal splenic artery and another SAA measuring 27 mm in diameter in the middle of the hepatic artery were found (Figure 1A). Both SAAs were saccular without calcifications or thrombosis.
Figure 1.
Figure 1.
Results of computed tomographic angiography. A: two separate splenic artery aneurysms, measuring 74 mm and 27 mm in diameter, anomalously originating from the hepatic artery; B: the splenic aneurysm was completely occluded with no blood inflow at the 1-year follow-up.
Considering the risk of rupture and the irregularity and narrowness of the vessel structure, open surgery was chosen. Median laparotomy was performed, and large pulsating masses were observed in the abdomen (supplementary Figure 1). After careful consideration, the SAAs were ligated at the proximal and distal ends. The SAAs were very large, and the splenic artery ran to the left along the superior margin of the pancreas; therefore, separating the SAAs from the surrounding tissues was associated with a high risk of pancreatic damage and bleeding. The dissection of the SAAs revealed blood flow from several branch arteries into the aneurysm sac. The branch arteries were ligated with 5-0 prolene sutures from the inside of the aneurysm walls, and human fibrin sealant was applied to occlude the aneurysms. However, the vascular supply of the entire spleen was compromised, and the spleen turned black 30 min after the completion of the procedure while the patient was under observation. Ischemic necrosis of the spleen was considered, and splenectomy was performed, followed by closure of the laparotomy incision.
Pathologic examination revealed mucoid degeneration and hyalinization of the arterial wall of the aneurysm (supplementary Figure 2). The patient recovered without postoperative complications. Blood tests one week after surgery revealed a platelet count of 480×109/L, and 100 mg/d aspirin was initiated. At the 1-year follow-up evaluation, the patient was in good clinical condition. CTA showed that both SAAs were occluded with no blood flow, and the aneurysms had shrunk (Figure 1B).
DISCUSSION
Splenic artery aneurysms with a diameter of ≥5 cm are considered rare, whereas two coincidental SAAs are rarer, potentially life-threatening presentations. SAAs can cause jaundice, abdominal pain, portal hypertension, or hemorrhage, depending on the location of the aneurysm.[3] Surgery is recommended for SAAs larger than 25 mm in diameter, those with symptomatic SAAs,[4] and those with rapid growth due to the increased rupture risk, which is associated with 20%-30% mortality.[5] Except in cases of rupture, the diagnosis of SAA is difficult due to the nonspecific symptoms.
Moreover, patients may benefit from treatment regardless of the sac size for aneurysms in specific arterial territories. In the present case, the treatment strategy was based on the site and the morphologic and anatomic characteristics of the SAAs as well as the need for occlusion of large efferent vessels emerging from the aneurysms. In addition, clinical presentation, general health status, and comorbidities were considered to determine the treatment approach.
Treatment approaches for this disease are classic surgical approaches,[6] including aneurysmal resection with or without vascular reconstruction, laparoscopy,[7] and endovascular treatment such as percutaneous embolization or stent implantation.[8] A previous study reported an endovascular approach with coil embolization for the treatment of huge hepatic artery aneurysms.[9] Coil embolization of large SAAs with a very wide neck tends to be extremely troublesome due to the limited length of inflow and outflow arteries.[10] Moreover, embolization of large aneurysms is associated with increased cost. In large saccular aneurysms, coil embolization is associated with poor long-term prognosis, as the coils may not be stable, increasing the risk of displacement and migration. Locating SAAs, separating the surrounding tissue, and dissecting the aneurysm are time-consuming procedures associated with an increased risk of postoperative complications, such as pancreatic leakage. Therefore, in the present case, open surgery was performed to ligate the distal and proximal ends of the aneurysms, which were occluded using human fibrin sealant to reduce the risk of pancreatic leakage and bleeding. During the long evolution of SAAs, multiple collaterals may develop, which can increase the splenic blood supply. In fact, the development of splenic ischemia following dissection and ligation of the SAAs in the present case required eventual removal of the spleen. For that patient, a laparoscopic approach may be minimally invasive. However, the present patient had two large SAAs, which were far apart, and the laparoscopic approach had difficulty in achieving precise manipulation and may cause a high risk of pancreatic injury. D’Errico et al[11] reported a patient with symptomatic double SAAs in the proximal and distal sections of the splenic artery who was successfully treated with surgery. Median laparotomy could provide a better view and more precise manipulation.
CONCLUSION
In patients with large SAAs in close contact with the pancreas, open surgery without complete aneurysm resection could be preferred to minimize pancreatic complications.
Funding: This study was funded by the Natural Science Foundation of Zhejiang Province (LQ20H020006).
Ethical approval: The patient provided informed consent, and all procedures performed followed the ethical standards of our hospital.
Conflicts of interest: The authors declare that they have no competing interests.
Contributors: All authors contributed substantially to the writing and revision of this manuscript and approved its contents.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
A ruptured splenic artery aneurysm treated by transcatheter arterial embolization using n-butyl cyanoacrylate-Lipiodol-Iopamidol
DOI:10.1016/j.radcr.2023.04.005 URL [Cited within: 1]
Congenital portosystemic shunt with multiple splenic artery aneurysms: reversing pulmonary hypertension and preventing aneurysm rupture
DOI:10.4103/apc.apc_142_21
PMID:36589645
[Cited within: 1]

We report an unusual occurrence of multiple splenic artery aneurysms and splenomegaly in a young woman with severe pulmonary hypertension, secondary to a congenital portosystemic shunt (CPS). The splenic artery was occluded using an Amplatzer Duct Occluder-II device, and closure of the large intrahepatic CPS was achieved using a muscular ventricular septal defect occluder. There was resolution of splenomegaly with normal pulmonary artery pressures, a few months after the procedure.Copyright: © 2022 Annals of Pediatric Cardiology.
A systematic review and meta-analysis of the management of visceral artery aneurysms
DOI:S0741-5214(19)30361-1
PMID:31126761
[Cited within: 1]

The evidence supporting management decisions of visceral artery aneurysms (VAAs) is sparse. Practice guidelines are needed to help patients and surgeons choose between endovascular and open surgery approaches.We searched MEDLINE, EMBASE, Cochrane databases, and Scopus for studies of patients with VAAs. Studies were selected and appraised by pairs of independent reviewers. Meta-analysis was performed when appropriate.We included 80 observational studies that were mostly noncomparative. Data were available for 2845 aneurysms, comprising 1279 renal artery, 775 splenic artery, 359 hepatic artery, 226 pancreaticoduodenal and gastroduodenal arteries, 95 superior mesenteric artery, 87 celiac artery, 15 jejunal, ileal and colic arteries, and 9 gastric and gastroepiploic arteries. Differences in mortality between open and endovascular approaches were not statistically significant. The endovascular approach was used more often by surgeons. The endovascular approach was associated with shorter hospital stay and lower rates of cardiovascular complications but higher rates of reintervention. Postembolization syndrome rates ranged from 9% (renal) to 38% (splenic). Coil migration ranged from 8% (splenic) to 29% (renal). Otherwise, access site complication were low (<5%). Pseudoaneurysms tended to have higher mortality and reintervention rates.This systematic review provides event rates for outcomes important to patients with VAAs. Despite the low certainty warranted by the evidence, these rates along, with surgical expertise and anatomic feasibility, can help patients and surgeons in shared-decision making.Copyright © 2019 Society for Vascular Surgery. Published by Elsevier Inc. All rights reserved.
The Society for Vascular Surgery clinical practice guidelines on the management of visceral aneurysms
DOI:10.1016/j.jvs.2020.01.039
PMID:32201007
[Cited within: 1]

These Society for Vascular Surgery Clinical Practice Guidelines describe the care of patients with aneurysms of the visceral arteries. They include evidence-based size thresholds for repair of aneurysms of the renal arteries, splenic artery, celiac artery, and hepatic artery, among others. Specific open surgical and endovascular repair strategies are also discussed. They also describe specific circumstances in which aneurysms may be repaired at smaller sizes than these size thresholds, including in women of childbearing age and false aneurysms. These Guidelines offer important recommendations for the care of patients with aneurysms of the visceral arteries and long-awaited guidance for clinicians who treat these patients.Copyright © 2020 Society for Vascular Surgery. Published by Elsevier Inc. All rights reserved.
Current management strategies for visceral artery aneurysms: an overview
DOI:10.1007/s00595-019-01898-3
PMID:31620866
[Cited within: 1]

Visceral artery aneurysms (VAAs) are rare and affect the celiac artery, superior mesenteric artery, and inferior mesenteric artery, and their branches. The natural history of VAAs is not well understood as they are often asymptomatic and found incidentally; however, they carry a risk of rupture that can result in death from hemorrhage in the peritoneal cavity, retroperitoneal space, or gastrointestinal tract. Recent advances in imaging technology and its availability allow us to diagnose all types of VAA. VAAs can be treated by open surgery, laparoscopic surgery, endovascular therapy, or a hybrid approach. However, there are still no specific indications for the treatment of VAAs, and the best strategy depends on the anatomical location of the aneurysm as well as the clinical presentation of the patient. This article reviews the literature on the etiology, clinical features, diagnosis, and anatomic characteristics of each type of VAA and discusses the current options for their treatment and management.
Endovascular and open surgical management in splenic artery aneurysm: an updated meta-analysis of comparative studies
The laparoscopic isolation of a splenic artery aneurysm: a case report
Ruptured splenic artery aneurysms in pregnancy and usefulness of endovascular treatment in selective patients: a case report and review of literature
Lessons in IR: splenic infarct after splenic aneurysm embolization
DOI:10.1016/j.jvir.2023.01.028 PMID:36739085 [Cited within: 1]
Treatment of visceral artery aneurysms using novel neurointerventional devices and techniques
DOI:S1051-0443(19)30001-6
PMID:31036460
[Cited within: 1]

The presence of branching vessels, a wide aneurysm neck, and/or fusiform morphology represents a challenge to conventional endovascular treatment of visceral artery aneurysms. A variety of techniques and devices have emerged for the treatment of intracranial aneurysms, in which more aggressive treatment algorithms aimed at smaller and morphologically diverse aneurysms have driven innovation. Here, modified neurointerventional techniques including the use of compliant balloons, scaffold- or stent-assisted coil embolization, and flow diversion are described in the treatment of visceral aneurysms. Neurointerventional devices and their mechanisms of action are described in the context of their application in the peripheral arterial system.Copyright © 2019 SIR. Published by Elsevier Inc. All rights reserved.
Surgical treatment of a double splenic artery aneurysm
PMID:20380278
[Cited within: 1]

Splenic artery aneurysms account for the majority of splanchnic artery aneurysms. These constitute a uncommon pathology, but with a mortality rate greater 70%. We report a case of a double symptomatic aneurysm of the splenic artery with a proximal and distal localization. The patient was a 65-year-old woman with chronic abdominal pain of the left hypochondrium, irradiating to the ipsilateral iliac fossa. In this case, the particular anatomical characteristics, which prevented a conservative endovascular treatment, were well suited to surgical treatment, performed successfully. In conclusion, in the case of a low-risk patient, in the presence of aneurysms with favourable anatomical characteristics one should prefer surgical rather than endovascular treatment, despite the widespread use of the latter.