Hemorrhagic shock is a life-threatening disease often encountered in emergency departments (EDs). Hemorrhagic shock caused by extensive bleeding from multiple sites is often associated with high mortality and morbidity. In recent years, resuscitative endovascular balloon occlusion of the aorta (REBOA) has been widely used in traumatic hemorrhagic shock and is considered to be an effective resuscitation measure.[1] Some studies reported that REBOA was also effective for non-traumatic hemorrhage.[2,3] In this study, we report a case of hemorrhagic shock caused by acute upper gastrointestinal bleeding that was successfully treated and received REBOA to obtain a transition time. This report may provide feasible options for emergency physicians, gastroenterologists, or surgeons to more actively treat refractory gastrointestinal bleeding.
CASE
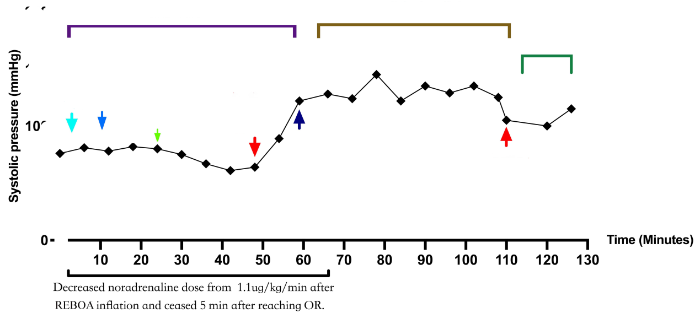
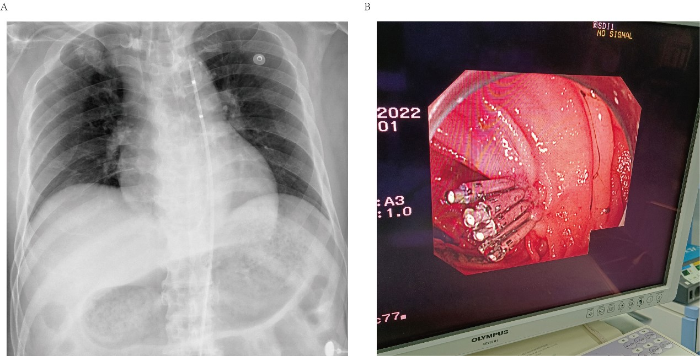
A 60-year-old male presented to the ED of our hospital complaining of melena for 1 d and had a few years of medication history of oral clopidogrel for treating coronary heart disease. Two weeks ago, the patient underwent duodenoscopic adenoma resection at a local hospital. The adenoma was 1.5 cm in size and was clamped with three titanium clips. There was no obvious postoperative discomfort. One day ago, the patient presented with massive melena, approximately 4,000 mL. He was unconscious, with a Glasgow Coma Scale (GCS) score of 8. In the ED, the patient developed hemorrhagic shock. His blood pressure was maintained at 81/45 mmHg (1 mmHg=0.133 kPa) with norepinephrine (0.45 μg/[kg·min]), and his heart rate was 135 beats/min. Endotracheal intubation was performed for assisted ventilation, and intravenous access was established for fluid resuscitation and transfusion of blood products. Then, the patient received approximately 1,100 mL of crystalline liquid, 1,200 units of prothrombin complex (PC), 400 mL of fresh frozen plasma, 2 units of red blood cells (RBCs), and 4 g of fibrinogen. However, the patient’s blood pressure was difficult to maintain and dropped to 65/42 mmHg, and his heart rate decreased to 65 beats/min (Figure 1). Considering that the situation was critical and the patient could have suffered cardiac arrest, we opted for the immediate use of REBOA. We inserted a 10F Coda balloon catheter (COOK Medical, USA) into the right femoral artery. The catheter was inserted 44 cm using surface positioning. The location of the balloon was confirmed to be in zone I using X-ray, and 8 mL of normal saline was injected into the balloon (Figure 2A). During this procedure, partial blockade was conducted to block the bleeding with an aortic balloon for a total of 71 min. The systolic blood pressure immediately rose to 85 mmHg, and the heart rate was 124 beats/min. One minute later, the systolic blood pressure of the patient was 135 mmHg. Bedside ultrasound was used to assess the blood flow below the balloon occlusion, and a weak pulse was palpable on both sides of the dorsum of the foot. Vasoactive drugs were gradually reduced, and laboratory tests revealed that hemoglobin was 39 g/L and lactic acid was 10.9 mmol/L. The patient was prepared for emergency endoscopy, and digital subtraction angiography (DSA) embolization and exploratory laparotomy were configured. Emergency gastroscopy showed a 1.5-cm rupture at the descending and horizontal parts of the duodenum with active bleeding. After using 5 more titanium clips, the patient’s blood pressure rose significantly, reaching a maximum of 155 mmHg (Figure 2B). The balloon was gradually released, and the patient’s systolic blood pressure decreased to 105 mmHg, then gradually to a minimum of 100 mmHg and remained stable thereafter. Emergency colonoscopy showed numerous dark red blood clots in the colon with no apparent active bleeding. During the whole process, 8 units of RBCs, 800 mL of fresh frozen plasma, and a large amount of PC and fibrinogen were infused.
Figure 1.
Figure 1.
Schematic diagram of the treatment. INN: norepinephrine; REBOA: resuscitative endovascular balloon occlusion of the aorta; PC: prothrombin complex; FIB: fibrinogen; RBC: red blood cells; FFP: fresh frozen plasma.
Figure 2.
Figure 2.
X-rays and DSA images. A: a 10F Coda balloon catheter inserted into the right femoral artery; B: during emergency gastroscopy, 5 titanium clips used to stop the bleeding.
After the operation, the patient’s vital signs were stable, endotracheal intubation was removed the next day, and the patient was transferred to the gastroenterology ward. On the 5th day, the patient was discharged after successful resuscitation and treatment.
DISCUSSION
REBOA is an auxiliary measure to temporarily stabilize hemodynamics before carrying out deterministic hemostatic measures during hemorrhagic shock. REBOA is a transitional phase between temporary hemostasis and resuscitation. Although it is able to stabilize hemodynamics and temporarily control bleeding, it also puts the patient at risk for ischemia-reperfusion injury in the lower parts after blockage and restoration of blood flow. REBOA is mainly used in the resuscitation of hemorrhagic shock patients with severe trauma by temporarily controlling bleeding and stabilizing hemodynamics. A few studies have been performed on the application of REBOA in upper gastrointestinal bleeding, but only some related cases have been reported. In a recent case, REBOA was successfully used in a patient with cardiac arrest caused by upper gastrointestinal bleeding. Spontaneous circulation was restored, and hemostasis was successfully achieved by DSA embolization.[4] In a similar case of hemorrhagic cardiac arrest caused by hemorrhagic shock from a bleeding giant gastric ulcer, REBOA temporarily controlled the bleeding and quickly restored spontaneous circulation. As the bleeding could not be stopped endoscopically, emergency surgical exploration was performed to stop the bleeding. A recent retrospective study of REBOA in upper gastrointestinal bleeding showed significant hemodynamic improvement after balloon deployment in zone I in all cases, with a mortality rate of approximately 25%.[5] However, with the prolongation of the blocking time, the ischemia-reperfusion injury of the blocked distal tissue was significantly aggravated. Therefore, it has been proposed that partial balloon occlusion can significantly reduce ischemia-reperfusion injury in distal organs.[6] In a retrospective study of occlusion duration in Japan, 78 patients underwent partial REBOA for 58 min, and 37 patients underwent complete REBOA for 33 min. There was no difference in the 24-hour and 30-day mortality between the complete and partial REBOA groups.[7] This suggests that partial balloon occlusion has very broad clinical application prospects. Another study reported the use of a combination of complete and partial balloon occlusion at zone I of the aorta.[8] The combination of intermittent complete occlusion and partial occlusion has also been reported to have significant hemodynamic advantages in animal studies compared with partial balloon occlusion alone. That is, distal tissue perfusion is significantly more stable, with no difference in mortality and vasoactive drug use.[9] Our case was a patient with upper gastrointestinal bleeding, severe hemorrhagic shock with extremely unstable hemodynamics and critically low heart rate at the time, and impending cardiac arrest. In this case, we chose to implement partial REBOA to keep the cardiac afterload stable, maintain hemodynamic stability, and protect distal organs. This patient suffered no complications related to organ ischemia. Therefore, we performed REBOA in zone I of the aorta, and immediate hemodynamic improvement was observed; the heart rate increased, and cardiac arrest was successfully prevented. Abdominal contrast-enhanced computed tomography could not be performed because of the large amount of blood in his stool, unclear etiology, and hemodynamic instability. Emergency gastroscopy was performed immediately, and considering that the time required for endoscopic treatment and possible exploratory laparotomy may be longer than 30 min, we performed partial occlusion for 71 min. After gastroscopy, there was no distal organ ischemia-reperfusion injury. This suggests that partial balloon occlusion is a promising method of resuscitation for patients with severe hemorrhagic shock caused by upper gastrointestinal bleeding.
This may be the first report of partial balloon occlusion for upper gastrointestinal bleeding and the first time that partial balloon occlusion has been used to prevent cardiac arrest due to severe hemorrhagic shock from upper digestive bleeding. There were no ischemia-related complications in the intestine and distal limbs reported after partial occlusion for 90 min.
CONCLUSION
REBOA could stabilize the hemodynamics of the patients and prevent cardiac arrest at the time of admission. Similar to traumatic hemorrhage, massive transfusion and partial REBOA might extend the occlusion duration of endoscopic hemostasis. More extensive use of REBOA in severe shock caused by upper gastrointestinal bleeding could be considered.
Funding: The study was supported by a grant from Health Commission of Zhejiang Province “optimization study on partial balloon occlusion of the aorta in traumatic hemorrhagic shock patients (2023KY774)”.
Ethical approval: The study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine.
Contributors: LYL and JYW contributed equally to this article. WH, TS, and KL: writing original draft; SXX: review and editing. All authors approved the final version.
Conflicts of interest: The authors declare that there are no conflicts of interest regarding the publication of this article.
Reference
Resuscitative endovascular balloon occlusion of the aorta (REBOA) in patients with major trauma and uncontrolled haemorrhagic shock: a systematic review with meta-analysis
DOI:10.1186/s13017-020-00345-w
[Cited within: 1]

Little is known about the effect of under triage on early mortality in trauma in a pediatric population. Our objective is to describe the effect of under triage on 24-h mortality after major pediatric trauma in a regional trauma system.
Life-threatening gastrointestinal bleeding from splenic artery pseudoaneurysm due to gastric ulcer penetration treated by surgical hemostasis with resuscitative endovascular balloon occlusion of the aorta: a case report
Aortic balloon occlusion in distal zone 3 reduces blood loss from obstetric hemorrhage in placenta accreta spectrum
Case report: lifesaving hemostasis with resuscitative endovascular balloon occlusion of the aorta in a patient with cardiac arrest caused by upper gastrointestinal hemorrhage
Resuscitative endovascular balloon occlusion of the aorta for uncontrollable nonvariceal upper gastrointestinal bleeding
DOI:10.1186/s13017-016-0076-3
PMID:27213011
[Cited within: 1]

Background: Although resuscitative endovascular balloon occlusion of the aorta (REBOA) in various clinical settings was found to successfully elevate central blood pressure in hemorrhagic shock, this intervention is associated with high mortality and may represent a last-ditch option for trauma patients. We conducted a retrospective study of patients with nonvariceal upper gastrointestinal bleeding (UGIB) who underwent REBOA to identify the effectiveness of REBOA and reviewed published literatures. Methods: REBOA were performed by trained acute care physicians in the emergency room and intensive care unit. The deployment of balloon catheters was positioned using ultrasonography guidance. Collected data included clinical characteristics, hemorrhagic severity, blood cultures, metabolic values, blood transfusions, REBOA-related complications and mortality. A literature search using PUBMED to include "aortic occlusion" and "gastrointestinal bleeding" was conducted. Results: REBOA was attempted in eight patients among 140 patients with UGIB and median age was 66 years. Systolic blood pressure significantly increased after REBOA (66 +/- 20 vs. 117 +/- 45 mmHg, p < 0.01) and the total occlusion time of REBOA was 80 +/- 48 min. Strong positive correlations were found between total occlusion time of REBOA and lactate concentration (Spearman's r=0.77), clinical Rockwall score (Spearman's r=0.80), and age (Spearman's r=0.88), respectively. Conclusion: REBOA can be performed with a high degree of technical success and is effective at improving hemodynamic in patients with UGIB. Correlations between total occlusion time and high lactate levels, clinical Rockall score, and age may be important for successful use of REBOA.
Extending the golden hour: partial resuscitative endovascular balloon occlusion of the aorta in a highly lethal swine liver injury model
DOI:10.1097/TA.0000000000000940
PMID:26670114
[Cited within: 1]

Combat-injured patients may require rapid and sustained support during transport; however, the prolonged aortic occlusion produced by conventional resuscitative endovascular balloon occlusion of the aorta (REBOA) may lead to substantial morbidity. Partial REBOA (P-REBOA) may permit longer periods of occlusion by allowing some degree of distal perfusion. However, the ability of this procedure to limit exsanguination is unclear. We evaluated the impact of P-REBOA on immediate survival and ongoing hemorrhage in a highly lethal swine liver injury model.Fifteen Yorkshire-cross swine were anesthetized, instrumented, splenectomized, and subjected to rapid 10% total blood loss followed by 30% liver amputation. Coagulopathy was created through colloid hemodilution. Randomized swine received no intervention (control), P-REBOA, or complete REBOA (C-REBOA). Central mean arterial pressure (cMAP), carotid blood flow, and blood loss were recorded. Balloons remained inflated in the P-REBOA and C-REBOA groups for 90 minutes followed by graded deflation. The study ended at 180 minutes from onset of hemorrhage or death of the animal. Survival analysis was performed, and data were analyzed using repeated-measures analysis of variance with post hoc pairwise comparisons.Mean survival times in the control, P-REBOA, and C-REBOA groups were, 25 ± 21, 86 ± 40, and 163 ± 20 minutes, respectively (p < 0.001). Blood loss was greater in the P-REBOA group than the C-REBOA or control groups, but this difference was not significant (4,722 ± 224, 3,834 ± 319, 3,818 ± 37 mL, respectively, p = 0.10). P-REBOA resulted in maintenance of near-baseline carotid blood flow and cMAP, while C-REBOA generated extreme cMAP and prolonged supraphysiologic carotid blood flow. Both experimental groups experienced profound decreases in cMAP following balloon deflation.In the setting of severe ongoing hemorrhage, P-REBOA increased survival time beyond the golden hour while maintaining cMAP and carotid flow at physiologic levels.
Fewer REBOA complications with smaller devices and partial occlusion: evidence from a multicentre registry in Japan
DOI:10.1136/emermed-2016-206383
PMID:28860179
[Cited within: 1]

Resuscitative endovascular balloon occlusion of the aorta (REBOA) performed by emergency physicians has been gaining acceptance as a less invasive technique than resuscitative thoracotomy.To evaluate access-related complications and duration of occlusions during REBOA.Patients with haemorrhagic shock requiring REBOA, from 18 hospitals in Japan, included in the DIRECT-IABO Registry were studied. REBOA-related characteristics were compared between non-survivors and survivors at 24 hours. 24-Hour survivors were categorised into groups with small (≤8 Fr), large (≥9 Fr) or unusual sheaths (oversized or multiple) to assess the relationship between the sheath size and complications. Haemodynamic response, occlusion duration and outcomes were compared between groups with partial and complete REBOA.Between August 2011 and December 2015, 142 adults undergoing REBOA were analysed. REBOA procedures were predominantly (94%) performed by emergency medicine (EM) physicians. The median duration of the small sheath (n=53) was 19 hours compared with 7.5 hours for the larger sheaths (P=0.025). Smaller sheaths were more likely to be removed using external manual compression (96% vs 45%, P<0.001). One case of a common femoral artery thrombus (large group) and two cases of amputation (unusual group) were identified. Partial REBOA was carried out in more cases (n=78) and resulted in a better haemodynamic response than complete REBOA (improvement in haemodynamics, 92% vs 70%, P=0.004; achievement of stability, 78% vs 51%, P=0.007) and allowed longer occlusion duration (median 58 vs 33 min, P=0.041). No statistically significant difference in 24-hour or 30-day survival was found between partial and complete REBOA.In Japan, EM physicians undertake the majority of REBOA procedures. Smaller sheaths appear to have fewer complications despite relatively prolonged placement and require external compression on removal. Although REBOA is a rarely performed procedure, partial REBOA, which may extend the occlusion duration without a reduction in survival, is used more commonly in Japan.© Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted.
Use of an intra-aortic balloon catheter tamponade for controlling intra-abdominal hemorrhage in man
Not ready for prime time: intermittent versus partial resuscitative endovascular balloon occlusion of the aorta for prolonged hemorrhage control in a highly lethal porcine injury model
DOI:10.1097/TA.0000000000002558
PMID:31996655
[Cited within: 1]

Partial resuscitative endovascular balloon occlusion of the aorta (pREBOA) and intermittent REBOA (iREBOA) are techniques to extend the therapeutic duration of REBOA by balloon titration for distal flow or cyclical balloon inflation/deflation to allow transient distal flow, respectively. We hypothesized that manually titrated pREBOA would reduce blood losses and ischemic burden when compared with iREBOA.Following 20% blood volume controlled hemorrhage, 10 anesthetized pigs underwent uncontrolled hemorrhage from the right iliac artery and vein. Once in hemorrhagic shock, animals underwent 15 minutes of complete zone 1 REBOA followed by 75 minutes of either pREBOA or iREBOA (n = 5/group). After 90 minutes, definitive hemorrhage control was obtained, animals were resuscitated with the remaining collected blood, and then received 2 hours of critical care.There were no differences in mortality. Animals randomized to iREBOA spent a larger portion of the time at full occlusion when compared with pREBOA (median, 70 minutes; interquartile range [IQR], 70-80 vs. median, 20 minutes; IQR, 20-40, respectively; p = 0.008). While the average blood pressure during the intervention period was equivalent between groups, this was offset by large fluctuations in blood pressure and significantly more rescue occlusions for hypotension with iREBOA. Despite lower maximum aortic flow rates, the pREBOA group tolerated a greater total amount of distal aortic flow during the intervention period (median, 20.9 L; IQR, 20.1-23.0 vs. median, 9.8 L; IQR, 6.8-10.3; p = 0.03) with equivalent abdominal blood losses. Final plasma lactate and creatinine concentrations were equivalent, although iREBOA animals had increased duodenal edema on histology.Compared with iREBOA, pREBOA reduced the time spent at full occlusion and the number of precipitous drops in proximal mean arterial pressure while delivering more distal aortic flow but not increasing total blood loss in this highly lethal injury model. Neither technique demonstrated a survival benefit. Further refinement of these techniques is necessary before clinical guidelines are issued.