Subdiaphragmatic abscess is the accumulation of pus in the space between the diaphragm and the transverse colon and its mesentery.[1] Subdiaphragmatic abscess is clinically characterized by fever and local pain. Its clinical manifestations are often vague and diverse, and its symptoms and signs together constitute thoracoabdominal syndrome, leading to delayed diagnosis and a high incidence rate and mortality.[2]Subdiaphragmatic abscess is often secondary to acute peritonitis or remote infection with hematogenous dissemination. The bacteriological characteristics of these abscesses include aerobic and facultative bacteria, such as Escherichia coli, group D Enterococcus and Staphylococcus aureus, as well as less common anaerobic organisms, such as Bacteroides.[3] In 1938, Ochsner and DeBakey recognized chest complications of subdiaphragmatic abscesses, including empyema, bronchial fistula, and pericarditis, in their classic review of subdiaphragmatic abscesses. Because of the structural characteristics of the diaphragm, there are fewer complications of diaphragm perforation.[4] Especially now, with the use of antibiotics, these complications have become more rare. Here, we report a case of purulent pericarditis caused by Klebsiella pneumonia, secondary to subdiaphragmatic abscess extending through the diaphragm.
CASE
A 57-year-old male was transferred to the emergency department (ED) of our hospital with a 7-hour history of continuous pain under the xiphoid process. Two hours before admission, he went to other hospitals with a temperature of 38.5 ℃. Echocardiography at other hospitals showed pericardial effusion, and computed tomography (CT) of the abdomen suggested a left lobe cyst of the liver. He was treated with dexamethasone, cefoperazone sulbactam sodium, and morphine, but the symptoms were not relieved and gradually aggravated, accompanied by shortness of breath, sweating, and weakness. He was transferred to the ED of our hospital. The patient suffered from varicose veins in his left lower limb for 30 years. He received surgical treatment for left shoulder fracture and antibiotic treatment for anal fistula in other hospitals six years ago and four months ago, respectively. Three months ago, he had fever and runny nose, but recovered without treatment. He denied having any other medical history.
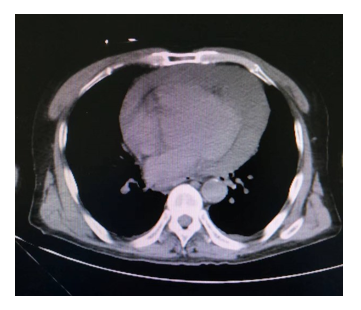
At admission to our hospital, the patient had a painful appearance, shortness of breath, general weakness, intermittent shivering, and a small amount of sweating. He was also hypotensive and tachycardic. During the examination, faint heart sounds, clear lungs, and diffuse abdominal pain were noted. Electrocardiography (ECG) showed sinus tachycardia, diffuse ST-segment elevation, and PR-segment depression (except for aVR lead), consistent with acute pericarditis (supplementary Figure 1). Chest CT revealed pericardial effusion (Figure 1). Abdominal CT showed space occupying the lateral segment of the left lobe of the liver (supplementary Figure 2), and the boundary between the local part and the diaphragm was unclear (supplementary Figure 3). Emergency bedside echocardiography showed a large amount of pericardial effusion (there was a dark area of fluid in the pericardium with a maximum depth of 20 mm, but the image was not saved). Abdominal ultrasound showed that 7.4 cm × 8.0 cm heterogeneous irregular shape low echo could be seen next to the left lobe of the liver.
Figure 1.
Figure 1.
Chest computed tomography showing pericardial effusion (white arrow).
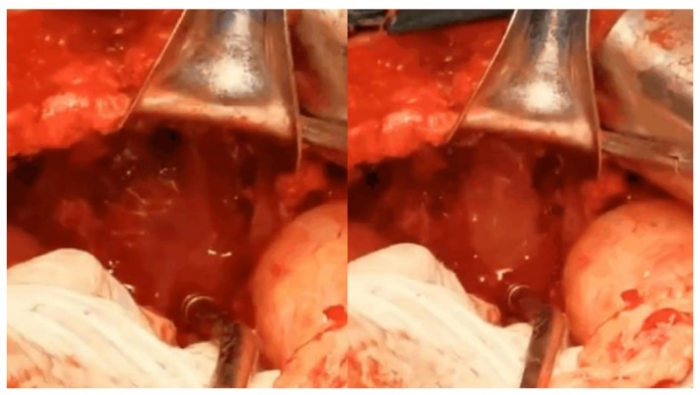
The diagnosis was pericarditis and peritonitis, and there were indications for laparotomy. Emergency exploratory laparotomy was performed. During the operation, a 15 cm × 12 cm tumor near the left lateral lobe of the liver was seen, which was irregular and hard. The tumor adhered to the left lateral lobe of the liver and diaphragm, and the tumor was wrapped by omentum. After removal of the free omentum, the tumor was considered an abscess. After absorbing approximately 300 mL of yellow pus, a 0.5-cm perforation of the diaphragm could be seen, and yellow pus overflowed from the pericardium (Figure 2 and specific video in the supplementary file). The pericardium and subdiaphragmatic area were rinsed, drainage tubes were placed, and pus was left for pathogenic culture, which was positive for Klebsiella pneumonia. In the first stage, vancomycin combined with meropenem was used for empirical treatment. In the second stage, vancomycin combined with meropenem was changed to cefoperazone-sulbactam anti-infection treatment according to the susceptibility test for antibiotics. At the same time, pericardial drainage, subdiaphragmatic abscess drainage, organ support, and nutritional support were performed. After surgical drainage, the patient’s condition improved, and then the drainage tube was removed. After 16 d of clinical treatment, the patient was discharged. We followed up with the patient for 180 d, and CT showed that the pericardial effusion subsided and the size of subdiaphragmatic abscess decreased (supplementary Figures 4 and 5). The patient gave written informed consent before we collected clinical information.
Figure 2.
Figure 2.
Yellow pus in the pericardium. A: a 0.5-cm perforation of the diaphragm (white arrow); B: yellow pus overflowed from the pericardium (white arrow).
DISCUSSION
Acute pericarditis is a rare but potentially fatal complication of subdiaphragmatic abscess. In our report, we describe a rare case of purulent pericarditis caused by Klebsiella pneumonia, secondary to subdiaphragmatic abscess extending through the diaphragm. Inflammation of the diaphragm and pericardium was confirmed during the operation. Early surgical treatment and antibiotic treatment may have prevented pericarditis from developing into more severe pericardial tamponade.
The purulent pericarditis extending through the diaphragm may form pathological channels due to the acute inflammation of the abscess and the inflammatory reaction of the diaphragm. Among them, liver pericardial fistula is more frequently reported and is mostly related to bacterial liver abscess and amebic liver abscess,[5⇓-7] and pericarditis caused by subdiaphragmatic abscess is extremely rare. Subdiaphragmatic abscess is often secondary to acute peritonitis or intraperitoneal surgery.[8] This patient had no history of abdominal surgery or related manifestations, such as abdominal organ perforation, before the onset of disease. However, he had upper respiratory tract infection three months ago and a history of anal fistula four months ago. Because the lymphatic network of the diaphragm and the lymphatic vessels of the surrounding organs overlap with each other, chest and abdominal infection can lead to infection under the diaphragm. This patient may have a subdiaphragmatic abscess due to chest and abdominal infection, but the symptoms were not obvious, so he did not seek medical advice. Finally, the abscess gradually penetrated the diaphragm and formed a pericardial abscess.
Purulent pericarditis caused by diaphragmatic extension is usually accompanied by tachycardia, septic shock, and even cardiac tamponade. If not treated in time, it may be fatal. Therefore, early identification is very important. Its treatment mainly includes pericardiocentesis, surgical pericardial drainage or pericardiectomy, surgical resection of the abscess, and antibiotic treatment.
CONCLUSION
In our case, subdiaphragmatic abscess may have been caused by infection of the chest and abdomen. This patient had indications for surgical exploration, so he received surgical treatment, and the treatment was effective. In conclusion, purulent pericarditis is a rare but fatal complication of abscess that can result from diaphragmatic extension. Early diagnosis, evaluation, and timely treatment can reduce the risk of death.
Funding: None.
Ethical approval: Written informed consent was obtained from the patient.
Contributors: SY and CC contributed equally to this study. SY drafted the manuscript. CC contributed to the manuscript revision. All authors read and approved the final manuscript.
Conflicts of interest: All authors have disclosed no conflicts of interest.
Reference
Cardiac tamponade provoked by a subphrenic abscess
DOI:10.2169/internalmedicine.8697-16 URL [Cited within: 1]
Intra-abdominal, retroperitoneal, and visceral abscesses in children
PMID:15343468
[Cited within: 1]

This review describes the microbiology, diagnosis, and management of intra-abdominal abscesses (including subphrenic, hepatic, splenic, and retroperitoneal abscesses) in children. They often occur as a complication of local or generalized peritonitis, commonly secondary to appendicitis, necrotizing enterocolitis, pelvic inflammatory disease, and tubo-ovarian infection, surgery or trauma. The original infection generally occurs because of the entry of enteric microorganisms into the peritoneal cavity through a defect in the wall of the intestine or other viscus as a result of obstruction, infarction, or direct trauma. Mixed aerobic and anaerobic flora can be recovered from most abscesses. The predominant aerobic isolates are Escherichia coli, Staphylococcus aureus, and Enterococcus spp. and the main anaerobic bacteria are Bacteroides fragilis group Peptostreptococcus spp., Fusobacterium spp., and Clostridium spp. The treatment of intraabdominal abscesses includes drainage, surgical correction of pathology, and administration of antimicrobials effective against both aerobic and anaerobic microorganisms.
Pericarditis with effusion and tamponade complicating left subdiaphragmatic abscesses
A rare case of pericarditis and pleural empyema secondary to transdiaphragmatic extension of pyogenic liver abscess
DOI:10.1186/s12879-018-2953-8
PMID:29334903
[Cited within: 1]

Background: Transdiaphragmatic extension of pyogenic liver abscess is the rarest cause of pericarditis and pleural empyema. It is a rapidly progressive and highly lethal infection with mortality rates reaching 100% if left untreated. However, the transmission route, treatment methods and prognosis have not been well studied.Case presentation: A 65-year-old male patient presented with a fever, dyspnea, and right upper quadrant abdominal pain. Computed tomography of the chest and abdomen showed huge liver abscess without full liquefaction in the left lobe, large amount of left pleural effusion, and mild pericardial effusion, and the patient was treated with parenteral antibiotics and pigtail insertion at the left pleura. However, four days later, cardiac tamponade was developed and surgical drainage of the abscess and pericardium was performed. Klebsiella pneumonia was isolated from pleural empyema. Twenty-five days after surgery, the patient was discharged without any complications.Conclusions: Herein, we report a rare case of pleural empyema and pericarditis in that resulted from the extension of huge pyogenic liver abscess. Early surgical treatment may have prevented progression of the pericarditis to the more dismal purulent pericarditis. We also review pertinent English literature on pericarditis as a complication of PLA.
Transdiaphragmatic rupture of hepatic abscess producing purulent pericarditis and pericardial tamponade
Hepato-pericardial fistula revealed by a massive pericardial effusion: a case report of an exceptional complication of the hydatid liver cyst
Endoscopic ultrasound-guided transmural drainage for subphrenic abscess: report of two cases and a literature review