Airway management of morbidly obese patients is challenging due to inherent anatomical and physiological variations.[1] The frequent association of compromised hemodynamics, hypoxemia, or acidosis in an emergency department (ED) setting adds to the difficulty of the procedure. Rapid airway management position (RAMP), awake fiber-optic guided intubation, use of intubating laryngeal mask airway (ILMA), and video-laryngoscope are a few techniques that have been described to tackle difficult airways in these patients.[2] Studies have shown that the availability of fiber-optic scopes (3%-60%), video-laryngoscopes (39%-88%), and laryngeal mask airways (LMA) (65%-83%) varies in different ED settings.[3,4] Furthermore, a lack of adequate training and the need for time-bound resuscitation make implementation of the above techniques challenging. Supraglottic airway devices (SADs) are potential rescue airway devices with a fast-learning curve. Point-of-care ultrasound (POCUS) is an easily available, convenient adjunct for airway management in emergency and critical care settings. Various studies have shown the utility of POCUS in the confirmation of correct endotracheal tube placement in real time.[5,6]
We describe a technique of intubation using the LMA bougie ultrasonography (L-B-US) technique in a morbidly obese patient.
CASE
A 36-year-old woman, morbidly obese (estimated body mass index [BMI] >40 kg/m2), was referred to our center for management of urosepsis, septic shock, and multiorgan dysfunction syndrome (MODS). During transfer to our center, the patient had a seizure, and a LMA (AMBU LMA size 4; AMBU®, Denmark) was placed by the paramedic for airway control. On arrival to the ED, the initial assessment revealed a first-generation LMA in situ, respiratory rate of 32 breaths/min, oxygen saturation of 98% (on 100% fraction of inspiration O2 [FiO2]) and bilateral crepitation on auscultation. Heart rate was 136 beats/ min, and blood pressure was 100/40 mmHg (1 mmHg=0.133 kPa). Her Glasgow Coma Scale was E2VTM5. Conjunctival chemosis, icterus, and bleeding from the oro-nasal cavity (probably mucosal) were other findings on examination. Initial blood gas indicated mixed metabolic and respiratory acidosis with pH 7.16, PCO2 57 mmHg, bicarbonate 18 mmol/L, and PO2 51 mmHg. Taking into consideration the risk of aspiration, hemodynamic instability, and need for optimizing ventilation, a decision was made to intubate the patient.
Obesity, short neck, large tongue, restricted mouth opening, and oral bleeding made the procedure an anatomically difficult airway; coexisting hemodynamic instability, acidosis, and hypoxia made it a physiologically difficult airway with a high risk of peri-intubation arrest. Furthermore, the short neck and propensity for bleeding make it a potentially difficult surgical airway in cases of failed endotracheal intubation.
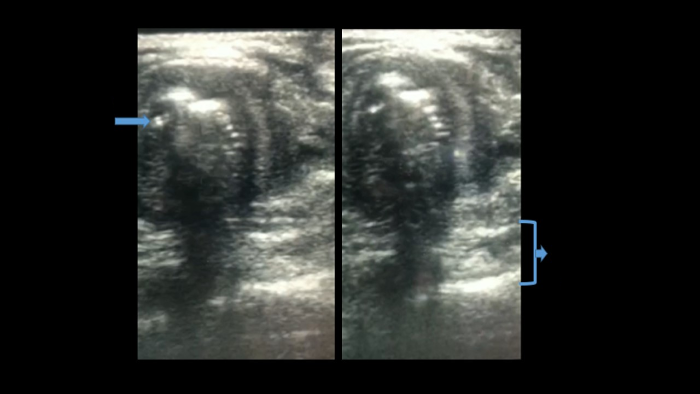
The intubating team consisted of a physician and an emergency nurse trained in POCUS (Figure 1). For ultrasonography, a high-frequency linear probe was used (HFL38x, 13-6 MHz bandwidth, Sonosite M-Turbo®; FUJIFILM Sonosite®, USA). Initial screening ultrasound of the airway was performed to look for any aberrant vessels in the neck and mark the cricothyroid membrane. The patient was placed in the ramped position. Thorough suctioning of the oral cavity was performed. Preoxygenation was continued via the LMA with the ventilator. Injection ketamine 50 mg and rocuronium 50 mg were used as the induction and paralysing agents, respectively. The ultrasound probe was placed horizontally just above the suprasternal notch to view the airway at the level of the upper tracheal rings and esophagus in the same axial plane. It is important to note that the air in the LMA cuff may obscure visibility at the level of the glottis. A bougie was inserted through the LMA. POCUS was used for dynamic tracking of the bougie passing through the trachea, which appeared as a bright dot on cross-section. Position was also confirmed by simultaneous absence of post echoic shadowing at the esophagus indicated by an intact hyperechoic line of the transverse process of the cervical vertebra behind the esophagus (Figure 2 and supplementary video). Following this, the LMA was removed, keeping the bougie in situ. Laryngoscopy was performed (Cormack-Lehanne Grade 3), and a size 7 endotracheal tube (ETT) was railroaded over the bougie. The position of the ETT was again confirmed with ultrasound. The double tract sign, which is a sign of esophageal intubation, was absent. Right mainstem bronchus intubation was ruled out by the presence of left-lung sliding. The ventilator circuit was connected to the ETT, and correct placement was reconfirmed with the end-tidal carbon dioxide (ETCO2) curve.
Figure 1.
Figure 1.
A “representative” image depicting the setup during the L-B-US technique.
Figure 2.
Figure 2.
Tracking of bougie placement and confirmation with airway ultrasonography.
DISCUSSION
In this case, we discussed the combination of the use of LMA bougie and ultrasound for the management of a difficult airway in a morbidly obese patient.
Intubation in critically ill patients with challenging neck anatomy and compromised physiological reserves[7] aggravates the risk of peri-intubation deterioration, making rapid first-pass intubation success crucial. SADs have proven to be very effective and easy-to-use equipment with a relatively high success rate, especially in difficult airway situations.[8] It holds the advantage of providing adequate oxygenation and ventilation and can be utilized for preoxygenation and further as a conduit for endotracheal intubation. Various techniques have been described for the same, of which the highest success rates have been obtained by using a flexible fiber-optic bronchoscope inserted through an already placed LMA.[9] Other techniques, such as blind bougie insertion or the use of intubation guides (airway exchange catheters -Cook medical®; Cook Medical LLC®, USA) via SADs, have had just approximately 50% first-pass success rates.[10,11] The use of ultrasound as a guide for bougie placement has been previously described in pediatric patients with anticipated difficult airways.[12] The nonavailability of fiber optic bronchoscope and obscured visibility led us to use this novel combination of adjuncts for management of the difficult airway. ILMA is another alternative that has been used in obese patients with a reasonable success rate.[13] However, studies have shown that the first-pass success with blind intubation with ILMA is up to 90%, which reduces further in novice users; there may be up to 8% risk of esophageal intubation with the blind technique.[14,15] The time taken for tracheal intubation and maneuvers may be significantly longer when using conventional polyvinylchloride tracheal tubes with ILMA. These may be the perceived advantages when considering the L-B-US technique described by us, where the risk of esophageal intubation may be avoided. However, further study in a larger cohort is required to test the ease of use, learning curve and time to intubation using this technique.
CONCLUSIONS
This report highlights the use of a combination of a simple LMA, bougie, and ultrasound for effective preoxygenation and safe intubation in morbidly obese patients with a difficult airway. The technique utilizes existing equipment available in most EDs.
Funding: None.
Ethical approval: The Institutional Ethics Committee provided waiver of consent for case reports with no direct patient identifiers.
Conflicts of interest: The authors have no conflicts of interest.
Contributors: RB: conceptualization, writing original draft; PY: draft writing; JB: case image acquisition; AN: conceptualization, collecting case data; SKN: review of draft, intellectual inputs; PRM: review of draft.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
The crashing obese patient
DOI:10.5811/westjem.2018.12.41085
PMID:30881553
[Cited within: 1]

Emergency physicians (EP) frequently resuscitate and manage critically ill patients. Resuscitation of the crashing obese patient presents a unique challenge for even the most skilled physician. Changes in anatomy, metabolic demand, cardiopulmonary reserve, ventilation, circulation, and pharmacokinetics require special consideration. This article focuses on critical components in the resuscitation of the crashing obese patient in the emergency department, namely intubation, mechanical ventilation, circulatory resuscitation, and pharmacotherapy. To minimize morbidity and mortality, it is imperative that the EP be familiar with the pearls and pitfalls discussed within this article.
The crashing obese patient
DOI:10.1016/j.emc.2020.06.013 URL [Cited within: 1]
Human and equipment resources for difficult airway management, airway education programs, and capnometry use in Japanese emergency departments: a nationwide cross-sectional study
DOI:10.1186/s12245-017-0155-6
PMID:28905252
[Cited within: 1]

Although human and equipment resources, proper training, and the verification of endotracheal intubation are vital elements of difficult airway management (DAM), their availability in Japanese emergency departments (EDs) has not been determined. How ED type and patient volume affect DAM preparation is also unclear. We conducted the present survey to address this knowledge gaps.This nationwide cross-sectional study was conducted from April to September 2016. All EDs received a mailed questionnaire regarding their DAM resources, airway training methods, and capnometry use for tube placement. Outcome measures were the availability of: (1) 24-h in-house back-up; (2) key DAM resources, including a supraglottic airway device (SGA), a dedicated DAM cart, surgical airway devices, and neuromuscular blocking agents; (3) anesthesiology rotation as part of an airway training program; and (4) the routine use of capnometry to verify tube placement. EDs were classified as academic, tertiary, high-volume (upper quartile of annual ambulance visits), and urban.Of the 530 EDs, 324 (61.1%) returned completed questionnaires. The availability of in-house back-up coverage, surgical airway devices, and neuromuscular blocking agents was 69.4, 95.7, and 68.5%, respectively. SGAs and dedicated DAM carts were present in 51.5 and 49.7% of the EDs. The rates of routine capnometry use (47.8%) and the availability of an anesthesiology rotation (38.6%) were low. The availability of 24-h back-up coverage was significantly higher in academic EDs and tertiary EDs in both the crude and adjusted analysis. Similarly, neuromuscular blocking agents were more likely to be present in academic EDs, high-volume EDs, and tertiary EDs; and the rate of routine use of capnometry was significantly higher in tertiary EDs in both the crude and adjusted analysis.In Japanese EDs, the rates of both the availability of SGAs and DAM carts and the use of routine capnometry to confirm tube placement were approximately 50%. These data demonstrate the lack of standard operating procedures for rescue ventilation and post-intubation care. Academic, tertiary, and high-volume EDs were likely to be well prepared for DAM.
Difficult airway equipment in English emergency departments
PMID:10792145
[Cited within: 1]

The need for tracheal intubation in the emergency department is often unpredictable and precipitous in nature. When compared with the operating room, a higher incidence of difficult intubation is observed. There are currently no accepted guidelines with respect to the stocking of difficult airway equipment in the emergency department. We have conducted a telephone survey to determine the availability of equipment for the management of the difficult airway in English emergency departments. Overall, the majority of units held a curved laryngoscope blade (100%), gum elastic bougie (99%) and surgical airway device (98%). Of alternative devices for ventilation, a laryngeal mask airway was kept by 65% of departments, a needle cricothyroidostomy kit by 63% and an oesophageal-tracheal twin-lumen airway (Combitube) by 18%. Of alternative devices for intubation, fewer than 10% held a retrograde intubating kit, intubating laryngeal mask, bronchoscope or lighted stylet. Seventy-four per cent of departments held an end-tidal carbon dioxide detector.
Integration of point-of-care ultrasound during rapid sequence intubation in trauma resuscitation
DOI:10.4103/JETS.JETS_56_17
PMID:29937637
[Cited within: 1]

Airway and breathing management play critical role in trauma resuscitation. Early identification of esophageal intubation and detection of fatal events is critical. Authors studied the utility of integration of point-of-care ultrasound (POCUS) during different phases of rapid sequence intubation (RSI) in trauma resuscitation.It was prospective, randomized single-centered study conducted at the Emergency Department of a level one trauma center. Patients were divided into ultrasonography (USG) and clinical examination (CE) arm. The objectives were to study the utility of POCUS in endotracheal tube placement and confirmations and identification of potentially fatal conditions as tracheal injury, midline vessels, paratracheal hematoma, vocal cord pathology, pneumothorax, and others during RSI. Patient >1 year of age were included. Time taken for procedure, number of incorrect intubations, and pathologies detected were noted. The data were collected in Microsoft Excel spread sheets and analyzed using Stata (version 11.2, Stata Corp, Texas, U. S. A) software.One hundred and six patients were recruited. The mean time for primary survey USG versus CE arm was (20 ± 10.01 vs. 18 ± 11.03) seconds. USG detected four pneumothorax, one tracheal injury, and one paratracheal hematoma. The mean procedure time USG versus CE arm was (37.3 ± 21.92 vs. 58 ± 32.04) seconds. Eight esophageal intubations were identified in USG arm by POCUS and two in CE arm by EtCO2 values.Integration of POCUS was useful in all three phases of RSI. It identified paratracheal hematoma, tracheal injury, and pneumothorax. It also identified esophageal intubation and confirmed main stem tracheal intubation in less time compared to five-point auscultation and capnography.
Endotracheal tube placement confirmation by ultrasonography: a systematic review and meta-analysis of more than 2500 patients
DOI:S0736-4679(20)30346-2
PMID:32553512
[Cited within: 1]

The integration of point-of-care ultrasound in endotracheal tube placement confirmation has been focus of many recent studies.We sought to determine the diagnostic accuracy of ultrasonography in confirmation of endotracheal intubation compared with standard confirmatory methods.We completed an extensive search of PubMed, EMBASE, Cochrane Central, Web of Science, and bibliographies of the selected articles from inception to October 2019. The search was limited to prospective studies conducted in human adults that compared the accuracy of ultrasonography in confirming the endotracheal tube position with a reference standard. The methodologic quality of studies was assessed using the Quality Assessment of Diagnostic Accuracy Studies-2 tool. A bivariate random-effects model summarized diagnostic accuracy statistics. Subgroup analyses by ultrasonographic signs, study location, the operator's specialty, types of transducer, the technique of ultrasound confirmation, and clinical setting (cardiac arrest vs. non-cardiac arrest) were performed.Thirty studies involving 2534 patients were selected for this meta-analysis. The estimated pooled sensitivity and specificity for ultrasonography were 0.982 (95% confidence interval [CI] 0.971-0.988) and 0.957 (95% CI 0.901-0.982), respectively. Subgroup analyses did not reveal significant difference by ultrasonographic sign used, location, the sonographer's specialty, transducer type, or ultrasound technique used. Ultrasound was also found to be a useful adjunct in confirming endotracheal tube position in the subgroup of patients with cardiac arrest, with sensitivity of 0.99 (95% CI 0.98-1.00) and specificity of 0.84 (95% CI 0.67-1.00), respectively.Ultrasonography is a valuable and reliable adjunct for endotracheal tube confirmation, including during cardiac arrest resuscitation.Copyright © 2020 Elsevier Inc. All rights reserved.
The physiologically difficult airway
DOI:10.5811/westjem.2015.8.27467
PMID:26759664
[Cited within: 1]

Airway management in critically ill patients involves the identification and management of the potentially difficult airway in order to avoid untoward complications. This focus on difficult airway management has traditionally referred to identifying anatomic characteristics of the patient that make either visualizing the glottic opening or placement of the tracheal tube through the vocal cords difficult. This paper will describe the physiologically difficult airway, in which physiologic derangements of the patient increase the risk of cardiovascular collapse from airway management. The four physiologically difficult airways described include hypoxemia, hypotension, severe metabolic acidosis, and right ventricular failure. The emergency physician should account for these physiologic derangements with airway management in critically ill patients regardless of the predicted anatomic difficulty of the intubation.
Supraglottic airways in difficult airway management: successes, failures, use and misuse
DOI:10.1111/anae.2011.66.issue-s2 URL [Cited within: 1]
Manikin study of fibreoptic-guided intubation through the classic laryngeal mask airway with the Aintree intubating catheter vs. the intubating laryngeal mask airway in the simulated difficult airway
DOI:10.1111/j.1365-2044.2010.06412.x
PMID:20586746
[Cited within: 1]

In this randomised crossover manikin study of simulated difficult intubation, 26 anaesthetists attempted to intubate the trachea using two fibreoptic-guided techniques: via a classic laryngeal mask airway using an Aintree intubating catheter and via an intubating laryngeal mask airway using its tracheal tube. Successful intubation was the primary endpoint, which was completed successfully in all 26 cases using the former technique, and in 5 of 26 cases using the latter (p < 0.0001). The former technique also proved quicker to reach the vocal cords with the fibrescope (median (IQR [range])) time 18 (14-20 [8-44]) s vs 110 (70-114 [30-118]) s, respectively; p = 0.008); and to first ventilation (93 (74-109 [52-135]) s vs 135 (79-158 [70-160]) s, respectively; p = 0.0038)]. We conclude that in simulated difficult intubation, fibreoptic intubation appears easier to achieve using a classic laryngeal mask airway and an Aintree intubating catheter than through an intubating laryngeal mask airway.
Blind intubation through the laryngeal mask airway in patients with difficult airways
Tracheal intubation through the laryngeal mask airway using a gum elastic bougie: the effect of head position
PMID:11578886
[Cited within: 1]

To determine the effect of head position on success of tracheal intubation through a Laryngeal Mask Airway (LMA) using a gum elastic bougie.Randomized, controlled study.Anesthesia and operating rooms of the University Hospital, Nottingham, UK.20 patients scheduled to undergo routine elective surgery requiring the use of an LMA for anesthesia.Blind placement of a gum elastic bougie through an LMA in two head positions.Final position of the gum elastic bougie after removal of the LMA as determined by fiberoptic laryngoscopy. The gum elastic bougie was correctly sited in the trachea in the classical intubating position in 4/20 (20%) and in the neutral position in 0/20 (0%). There was no difference in the success of this technique between the two head positions.This technique cannot be recommended as an alternative to direct laryngoscopy following a failed intubation.
Ultrasound-guided bougie insertion during anticipated difficult intubation
DOI:10.1111/pan.2018.28.issue-11 URL [Cited within: 1]
Intubating laryngeal mask airway in morbidly obese and lean patients: a comparative study
PMID:15915021
[Cited within: 1]

The intubating laryngeal mask airway (ILMA) was designed using the characteristics of healthy-weight subjects but was shown to be an effective airway device in morbidly obese patients. The authors compared airway management quality in morbidly obese and lean patients with use of the ILMA.Fifty morbidly obese and 50 lean patients (mean body mass indexes, 42 and 27 kg/m, respectively) were enrolled in this prospective study. After induction of general anesthesia, characteristics of airway management were judged on safety and efficiency parameters, including success rate at ventilation and intubation and airway management quality criteria, such as the number of patients who required adjustment maneuvers, the number of failed tracheal intubation attempts, the total duration of airway management, and an overall difficulty visual analog scale score.The ILMA was successfully inserted and adequate ventilation through the ILMA was achieved in all 100 patients. The success rates of tracheal intubation through the ILMA were similar in obese and lean patients (96% and 94%, respectively). The numbers of failed blind tracheal access attempts and patients who required airway-adjustment maneuvers were significantly reduced in obese patients as compared with lean patients. Four obese patients experienced transient episodes of oxygen desaturation (oxygen saturation < 90%) before adequate bag ventilation was established with the ILMA.The authors confirmed that the ILMA was an efficient airway device for airway management of both lean and obese patients. In the conditions of this study, the authors observed that airway management with the ILMA was simpler in obese patients as compared with lean patients.
Intubation success through I-gel® and intubating laryngeal mask airway®using flexible silicone tubes: a randomised noninferiority trial
Endotracheal intubation through the intubating laryngeal mask airway (LMA-Fastrach™): a randomized study of LMA- Fastrach™ wire-reinforced silicone endotracheal tube versus conventional polyvinyl chloride tracheal tube
DOI:10.4103/0019-5049.108555
PMID:23716761
[Cited within: 1]

A wire-reinforced silicone tube (LMA-Fastrach™ endotracheal tube) is specially designed for tracheal intubation using intubating laryngeal mask airway (ILMA). However, conventional polyvinyl chloride (PVC) tracheal tubes have also been used with ILMA to achieve tracheal intubation successfully.To evaluate the success of tracheal intubation using the LMA-Fastrach™ tracheal tube versus conventional PVC tracheal tube through ILMA.Two hundred adult ASA physical status I/II patients, scheduled to undergo elective surgery under general anaesthesia requiring intubation, were randomly allocated into two groups.The number of attempts, time taken, and manoeuvres employed to accomplish tracheal intubation were compared using conventional PVC tubes (group I) and LMA-Fastrach™ wire-reinforced silicone tubes (group II). Intraoperative haemodynamic changes and evidence of trauma and postoperative incidence of sore throat and hoarseness, were compared between the groups.The data was analyzed using two Student's t test and Chi-square test for demographics and haemodynamic parameters. Mann Whitney U test was used for comparison of time taken for endotracheal tube insertion. Fisher's exact test was used to compare postoperative complications.Rate of successful tracheal intubation and haemodynamic variables were comparable between the groups. Time taken for tracheal intubation and manoeuvres required to accomplish successful endotracheal intubation, however, were significantly greater in group I than group II (14.71±6.21 s and 10.04±4.49 s, respectively (P<0.001), and 28% in group I and 3% in group II, respectively (P<0.05)).Conventional PVC tube can be safely used for tracheal intubation through the ILMA.