Traumatic injuries range from simple to complicated multiple injuries. The identification of patients with critical injuries and disrupted organ perfusion is essential to prevent tissue hypoxia. A study estimated that a fast and accurate response to thoracic trauma should reduce the mortality by 30%.[1] The tissue perfusion value is an essential indicator of mortality and morbidity for patients admitted to the hospital with thoracic trauma. Thus, this study aimed to show the role of the perfusion index (PI) in predicting the prognosis of patients admitted to the emergency department for thoracic trauma.
METHODS
This study was conducted prospectively on 187 patients who were admitted to the emergency clinic of a tertiary university hospital between January 1, 2019, and December 1, 2020. Ethics committee approval was obtained (Accept no. 20.478.486//01/15/2020).
Patients older than 8 years who were admitted for thoracic trauma and whose PI values were measured on admission and 2 h after admission were included in the study. Patients with a known peripheral vascular disease, penetrating injuries, or positive COVID-19 polymerase chain reaction test, were excluded from the study. Masimo Radical-7 pulse oximeters (Masimo Corporation, USA) were used to measure the PI.
The patients were assessed for their sex, age, triage codes on admission, Glasgow Coma Scale (GCS), Injury Severity Score (ISS), Revised Trauma Scores (RTS), systolic and diastolic blood pressures, pulse rates, fingertip oxygen saturation (SPO2), respiration rates, PI, presence of intubation, diagnoses, and outcomes (discharge, transfer to a department/intensive care unit [ICU], or exitus).
SPSS Statistics for Windows, version 21.0 (IBM Corp., USA) was used to perform the analyses. Categorical variables are shown as numbers and percentages, and continuous numeric variables are shown as mean with standard deviations or means with range. The normality of continuous numerical variables was tested by the Shapiro-Wilk test. Analysis of variance was used to compare continuous numerical variables that matched the normal distribution between more than two groups, and the Kruskal-Wallis test was used to compare parameters that did not match the normal distribution. To determine the significant groups, Bonferroni correction was performed to calculate the P-values. The Pearson Chi-square test was used to compare categorical variables among the groups. The correlation was determined by the Spearman correlation test. Logistic regression analysis was used to determine the factors that affected the results. Receiver operating characteristic analysis was performed to determine the sensitivity and specificity for the predictability of the PI, and a P-value <0.05 was considered statistically significant.
RESULTS
Based on the selection criteria, 37 patients were excluded from the study, and 150 patients were included. Moreover, 22% (n=33) of the patients were female, whereas 78% (n=117) were male. We observed isolated thoracic trauma in 29.3% (n=44) and multiple traumas accompanied by thoracic trauma in 70.7% (n=106) of the patients.
Red triaged patients accounted for 69.3% of all patients, 12.7% of the cases were intubated. According to outcomes, 22.0% of the cases were discharged (the patients who had one rib fracture with or without minimal radiological lung contusion, non-surgical extremity fracture treated with splint, soft tissue injuries, GCS 15, or RTS 12), 26.7% were hospitalized, 50.0% were sent to the ICU, and 1.3% died. We recorded thorax-head-neck injuries in 29.2% (n=31), thorax-abdomen injuries in 25.5% (n=27), thorax-abdomen-head-neck injuries in 19.8% (n=21), and thorax-abdomen-head-neck-extremity injuries in 25.5% (n=27) of patients with multiple traumas. In addition, we observed pneumothorax (16.0%), hemothorax (11.3%), rib fractures (58.7%), contusions (52.0%), hemopneumothorax (1.3%), and flail chest (0.7%) in thoracic trauma cases.
In this study, the GCS, ISS, RTS scores, and PI readings on admission and 2 h thereafter significantly affected the final outcomes (P<0.05) (Table 1).
Table 1. Distribution of age, coma, risk scores, and vital parameters in patients
| Variables | Termination status (outcomes) | P-value | ||
|---|---|---|---|---|
| Discharged group (n=33) | Hospitalized group (n=40) | ICU and exitus group (n=77) | ||
| Age, years | 47.24±19.24 | 47.53±15.87 | 42.22±17.69 | 0.174 |
| Glasgow Coma Scale | 15.00±0.00 | 15.00±1.00 | 12.65±4.39 | <0.001 |
| Injury Severity Score | 2.70±1.67 | 5.90±2.47 | 9.77±3.53 | <0.001 |
| Revised Trauma Score | 12.00±0.00 | 12.00±1.00 | 11.21±1.66 | <0.001 |
| Systolic blood pressure, mmHg | ||||
| Arrival | 129.00±12.40 | 130.43±13.65 | 114.90±21.28 | <0.001 |
| 2nd hour | 71.76±9.49 | 74.98±8.25 | 68.36±14.15 | 0.009 |
| Diastolic blood pressure, mmHg | ||||
| Arrival | 128.52±10.07 | 131.58±12.51 | 118.40±16.67 | <0.001 |
| 2nd hour | 74.91±7.40 | 77.08±6.42 | 72.10±10.26 | 0.040 |
| Heart rate, beats/min | ||||
| Arrival | 85.48±11.01 | 91.43±11.02 | 99.56±19.68 | 0.001 |
| 2nd hour | 84.18±8.18 | 86.88±9.27 | 93.17±14.58 | 0.001 |
| Finger probe SPO2, % | ||||
| Arrival | 97.18±1.26 | 95.63±2.50 | 94.34±6.13 | 0.001 |
| 2nd hour | 97.79±0.96 | 97.05±1.34 | 97.14±2.61 | 0.093 |
| Respiration rate, breaths/min | ||||
| Arrival | 15.91±1.47 | 15.78±1.72 | 16.75±2.23 | 0.023 |
| 2nd hour | 15.64±1.54 | 15.63±1.55 | 15.61±1.48 | 0.996 |
| Perfusion index | ||||
| Arrival | 2.92±1.51 | 1.90±1.13 | 0.88±0.40 | <0.001 |
| 2nd hour | 3.18±1.39 | 2.37±0.98 | 1.44±0.54 | <0.001 |
A P-value <0.05 was considered as significant. SPO2: oxygen saturation; ICU: intensive care unit.
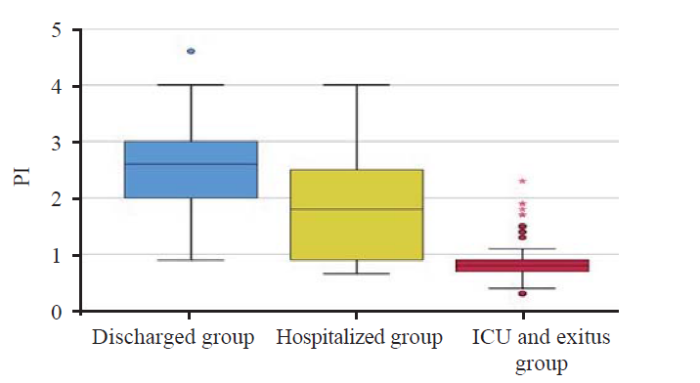
The PI on admission was 2.92±0.51 for the discharged group, 1.90±1.13 for the hospitalized group, and 0.88±0.40 for the ICU and exitus group. As the clinical severity of the cases increased, the PI decreased significantly (P<0.001) (Figure 1).
Figure 1.
Figure 1.
Graphical representation of the distribution of the PI value measured at admission among the outcome groups. PI: perfusion index; ICU: intensive care unit.
The ISS (odds ratio [OR] 2.077, 95% confidence interval [95% CI] 1.493-2.890) and the PI recorded on admission (OR 0.112, 95% CI 0.037-0.340) significantly affected ICU admission and exitus regardless of other variables (P<0.001)(supplementary Table 1).
The PI was 83.6% sensitive and 81.8% specific at a cut-off value of 0.95 in determining ICU admission or death (area under the curve [AUC] 0.896, 95% CI 0.846-0.946, P<0.001). The PI on admission correlated positively with the GCS, RTS, systolic blood pressure, and fingertip SPO2 and negatively with the ISS, pulse rate, and respiration rate at a significant level (P<0.05) (supplementary Table 2).
DISCUSSION
Ozakin et al[2] reported the predictability of hypovolemic shock by PI in trauma cases. According to them, PI was 78% sensitive and 97.6% specific at the most ideal at a cut-off value of 1. In our study, a similarly disrupted peripheral PI value at a cut-off value of 0.95 (83.6% sensitive, 81.8% specific) was significant in determining whether the patient needed ICU care.
All studies about the correlation between the PI and prognosis underline the association of a drop in PI with a poor prognosis. There is a clearly significant correlation between the drop in perfusion and mortality in a review of 26 studies and the correlation between peripheral PI and mortality in sepsis.[4] Hariri et al[5] similarly reported that PI was a key indicator of serious organ failure and mortality risk.
Few studies have compared PI with other clinical scores in trauma cases. In our study, we analyzed RTS, ISS, and PI for their capability to predict prognosis for thoracic trauma cases, and we found that PI and ISS were superior to RTS in this regard. Akhavan Akbari and Mohammadian[6] reported that ISS predicted mortality, survival probability, and period of ICU stay and that ISS was a more accurate score for trauma cases. In a similar study, Wang et al[7] assessed the predictive capacity of GCS, RTS, and ISS and reported that ISS was a better scoring system than RTS and GCS in predicting both early and delayed mortality. We found that PI and ISS were independently related to ICU stay and mortality. Considering the purpose of ISS, it is an indicator of the severity of injury in trauma cases; hence, it is related to prognosis. A few studies have reported that ISS could predict a poor prognosis in thoracic trauma cases.[8,9] Moreover, in a study comparing the uses of RTS and PI in trauma cases, Ozakin et al[2] reported a significant negative correlation between PI and RTS, arguing that PI was superior to RTS in trauma cases. Considering the outcomes of the studies on trauma scores and PI and our findings, PI and ISS can be more accurate predictors than RTS in determining prognosis in trauma cases. However, the lack of studies that have compared ISS with PI and the fact that we did not notice any superiority between the two parameters in our study limit our ability to comment on choosing between ISS and PI in predicting prognoses in trauma cases.
We found that PI and ISS on admission can predict ICU stay and mortality regardless of the other parameters examined. A low PI in patients who sustained hemothorax and pneumothorax improved rapidly after tube thoracostomy. While the average PI of these cases was 0.58±0.13 on admission, the PI rose to 0.98±0.22 after 2 h, indicating a 69% increase. Moreover, intubation increased the PI value. This explains why patients who were triaged red had a PI of 0.88±0.40 on admission but had a PI of 1.44±0.54 after 2 h.
In our study, although the number of patients with multitrauma was high, the ISS was low (7.18±4.11), and the GCS score was high (13.79±3.35). This is because our hospital is the reference hospital for thoracic surgery in the region, and patients are transferred to our hospital regardless of the ISS. Although 29.3% (n=44) of our isolated chest trauma patients had a low PI value, the cause was thought to be pulmonary parenchymal damage rather than multitrauma.
CONCLUSIONS
PI in combination with ISS may be easily used for determining the prognosis of patients with thoracic trauma, especially those with lung parenchymal injury.
Funding: None.
Ethical approval: Ethics committee approval was obtained (Accept no. 20.478.486//01/15/2020).
Conflicts of interest: None declared.
Contributors: All authors contributed to the conception or design of the work or the acquisition, analysis, or interpretation of data for the study.
All the supplementary files in this paper are available at http://wjem.com.cn.
Reference
Trauma score systems for quality assessment
DOI:10.1007/s00068-002-0170-y URL [Cited within: 1]
Perfusion index measurement in predicting hypovolemic shock in trauma patients
DOI:S0736-4679(20)30341-3
PMID:32439257
[Cited within: 3]

Perfusion index (PI) derived from pulse oximeter shows the ratio of the pulsatile blood flow to the nonpulsatile blood flow or static blood in peripheral tissue.The aim of this study was to investigate the relationship between PI and blood transfusion necessity in 24 h and stage of hemorrhagic shock, as well as the utility of PI according to laboratory and clinical parameters, and determining the major risk of hemorrhage.PI was measured with a pulse oximeter in 338 patients (235 males, average age 41.8 ± 17.94 years). Laboratory parameters (hemoglobin, hematocrit, lactate, base deficits, pH) and clinical parameters (pulse rate, respiratory rate, SpO, systolic blood pressure [SBP] and diastolic blood pressure [DBP]), shock index (SI) and revised trauma score (RTS) were recorded. Univariate analysis was used to determine major risk for bleeding, and the receiver operating characteristic curves were performed to compare parameters.PI was < 1 in 39 (11.5%) patients. Positive correlation between PI and hemoglobin (p < 0.001; r: 0.320), hematocrit (p < 0.001; r: 0.294), base deficit (p < 0.001; r: 0.315), pH (p < 0.05; r: 0.235), SBP (p < 0.001; r: 0.146), DBP (p < 0.001; r: 0.259), SpO (p < 0.001; r: 0.197), RTS (p < 0.001; r: 0.344), and negative correlation with lactate (p < 0.05; r: -0.117), pulse (p < 0.001; r: -0.326), respiratory rate (p < 0.001; r: -0.231), and SI (p < 0.001; r: -0.257) were detected. A difference was detected between class 1 and 2, and class 1 and 3 (both p < 0.05) in hemorrhagic shock. Thirty-one with PI < 1 had blood transfusion within 24 h (p < 0.001; odds ratio 111.98, sensitivity 75.6%, specificity 97.3, positive predictive value 79.5%, negative predictive value 96.7%). The main risk factors of the need for blood transfusions were PI, pulse rate, and SpO. PI was more significant than lactate, base deficit, RTS, and SI measurements.PI might be beneficial in the detection and exclusion of critical patients and blood transfusion needs in the emergency department. PI can be used with vital signs and shock parameters in the early diagnosis of hemorrhage.Copyright © 2020 Elsevier Inc. All rights reserved.
Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion
DOI:10.1097/00003246-200206000-00006 URL [Cited within: 1]
Association between peripheral perfusion, microcirculation and mortality in sepsis: a systematic review
Narrative review: clinical assessment of peripheral tissue perfusion in septic shock
DOI:10.1186/s13613-019-0511-1 URL [Cited within: 1]
Comparison of the RTS and ISS scores on prediction of survival chances in multiple trauma patients
Predictors of early versus late mortality in pelvic trauma patients
DOI:10.1186/s13049-016-0220-9 URL [Cited within: 1]
The thorax trauma severity score and the trauma and injury severity score: do they predict in-hospital mortality in patients with severe thoracic trauma? : a retrospective cohort study
DOI:10.1097/MD.0000000000008317 URL [Cited within: 1]
Factors affecting mortality in patients with thorax trauma
DOI:10.5505/tjtes.2011.76158 URL [Cited within: 1]
Lung contusion: a clinico-pathological entity with unpredictable clinical course
Pulmonary contusion
DOI:10.21037/jtd.2018.11.53 URL [Cited within: 1]