Dear editor,
The neck is rich in blood vessels. Abnormal origins are rarely seen in clinical practice, but some are found accidentally during relevant imaging examinations, autopsy, and surgery. Abnormal neck vessels are mostly asymptomatic; however, approximately 10% of patients with abnormal blood vessels may have clinical manifestations due to the compression of adjacent tissues and organs.[1] The innominate artery is a short artery branching off from the right side of the main arch obliquely to the upper right behind the right sternoclavicular joint; it divides into the right common carotid artery (RCCA) and the right subclavian artery (RSA). Variations in the location and distortions of the innominate artery and its branches are rare. We encountered a case of distortion and malformation of the RCCA resulting in compression of the trachea, as reported by Madan et al.[2]
CASE
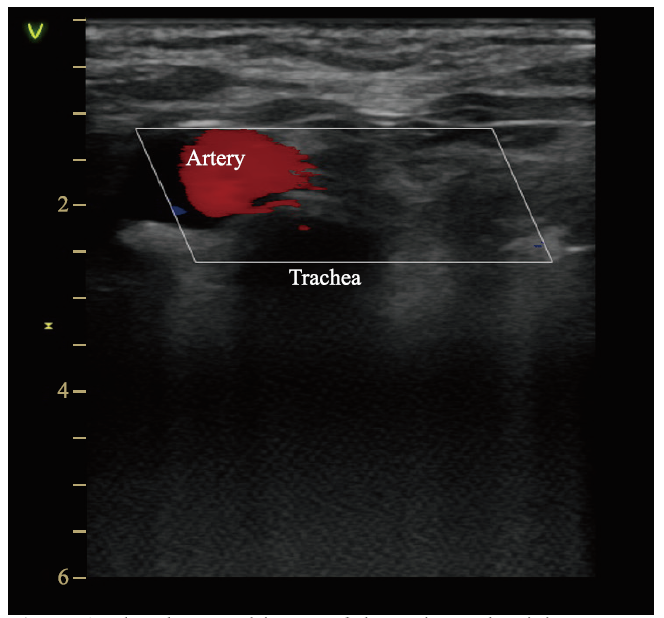
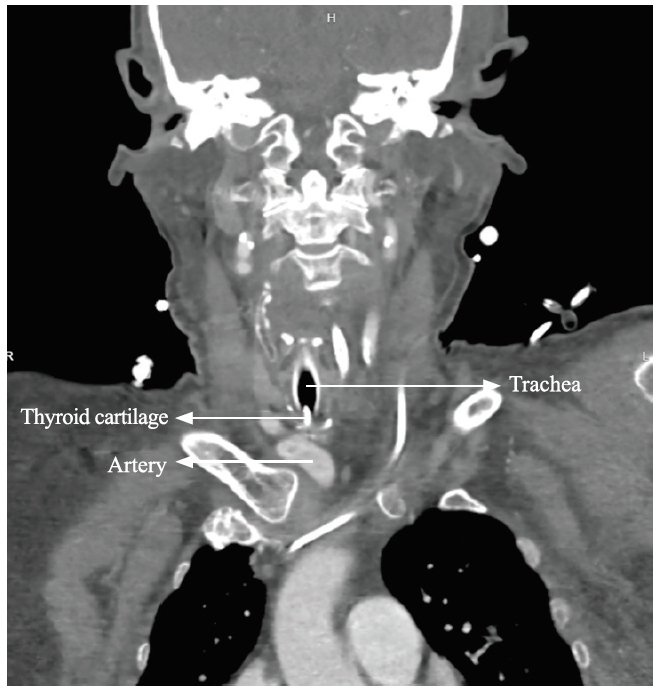
A 78-year-old female (body mass index [BMI] 24.9 kg/m2) was admitted to our hospital after being found unconscious. The diagnosis was hypoxic ischemic encephalopathy. To clear airway secretions and maintain vital signs, percutaneous dilatational tracheostomy (PDT) was considered. At the site of tracheostomy, pulsation on the cricoid cartilage was evident, and ultrasound was performed immediately. The RCCA was found to run on the right side of the trachea, crossing the trachea anteriorly below the cricoid cartilage and descending posteriorly, as shown in Figure 1. The decision was made to suspend the tracheostomy, and carotid angiography was performed on the same day. The family denied any history of congenital vascular malformation. Combined with the patient's long history of hypertension and carotid atherosclerosis, the carotid artery was considered to be distorted and deformed. A coronal view revealed that the trachea was shifted to the right, potentially due to traction from surrounding tissues; the innominate artery transversely covered the position between the 1st and 2nd tracheal rings, as shown in Figure 2. The tracheostomy method was changed the next day. After the RCCA was separated under direct vision, tracheostomy was performed, and a tracheal cannula was implanted. The whole operation was carried out under electrocardiogram (ECG), blood pressure and blood oxygen saturation monitoring, and there was no obvious bleeding during or after the operation. Later, the patient was successfully weaned off the ventilator and transferred out of the emergency intensive care unit (EICU). Ultimately, the patient's family could not afford the expensive rehabilitation treatment and abandoned treatment.
Figure 1.
Figure 1.
The ultrasound image of the patient. The right common carotid artery found to run on the right side of the trachea.
Figure 2.
Figure 2.
The carotid angiography image of the patient. The innominate artery transversely covered the position between the 1st and 2nd tracheal rings.
DISCUSSION
The great vessels of the human head and neck include the aortic arch, the brachiocephalic trunk (BCT), the left common carotid artery (LCCA) and RCCA, the left and right vertebral arteries, and the left subclavian artery (LSA) and RSA. The aortic arch is one of the three thoracic segments of the aorta and the only segment located in the superior mediastinum (SM). The arch begins with the aorta rising from the pericardium and passing upward, backward, and left across the SM and ends at the level of the T4-T5 vertebrae. Three branches arise from the upper boundary of the artery: the BCT, the LCCA, and the LSA. The BCT divides into the RCCA and the RSA.[3,4] However, it has been reported in the literature that cervical vascular variations and distortions are more common on the left side, with abnormalities on the right side of the neck accounting for less than 1% of the total.[5] In addition, a study of 556 patients with thoracic aortic disease showed that 33.5% (186 patients) demonstrated anomalies of the aortic arch, 6.3% (35 patients) had an isolated left vertebral artery, and 1.8% (10 patients) had an aberrant RSA.[1] PDT is currently an important means of clinical rescue. Although the curative effect is exact and the technique is mature, hemorrhage is a serious complication after this operation. The literature indicates that the mortality rate due to hemorrhage after tracheostomy is high, especially innominate artery hemorrhage, with a mortality rate of 90%.[6]Thus, appropriate indications are required for tracheostomy.[7] Based on the literature and clinical experience, the emergency unit of our institution requires all patients intended to be treated with PDT to undergo a preincision evaluation, except in extreme cases where cricothyroid tracheostomy may be necessary.[8] In cases of BMI 28 kg/m2, vague anatomical landmarks (brevicollis, giant thyroid, after surgery or radiotherapy), neck instability or infection, and hypocoagulability, physicians and surgeons need to decide together whether the patient would benefit from tracheostomy and which technique would be the most suitable. An uncorrected bleeding disorder (platelet count <50,000/mm3 and/or international normalized ratio >1.5 and/or partial thromboplastin time >2 normal) is an absolute contraindication to all surgical procedures.[9,10] We require an ultrasound examination before PDT because it helps identify abnormal blood vessels, and ultrasound during PDT helps prevent tracheal misalignment.[11]This requirement is based on four open randomized studies in a total of 560 patients. We typically used a single dilator in our PDT technique,[10] as this method causes the least bleeding among all methods and tools for PDT (multiple dilator, guide wire dilating forceps, single dilator, rotating dilation, and balloon dilation).
CONCLUSIONS
The incidence of cervical vascular variation is not high in clinical practice, but carelessness during tracheostomy may lead to serious complications and irreparable consequences. PDT can be performed quickly and safely at the bedside with the use of a modified Seldinger technique and bronchoscopic guidance. Compared with the open tracheostomy, this approach is associated with fewer bleeding complications, a shorter operation time, and a decreased incidence of stoma infection and inflammation, but a similar long-term morbidity rate.[10⇓-12] While performing tracheostomy early or late does not affect the prognosis, early tracheostomy seems to reduce the consumption of hypnotic drugs. At our institution, early tracheostomy (after the fourth day of mechanical ventilation) is performed for patients with severe cerebrovascular disease. Therefore, fundamental measures to prevent complications of tracheostomy include standardizing the evaluation and manipulation of the trachea before tracheostomy and strengthening observation and nursing practices after tracheostomy. Based on the treatment involved and summary of this case, we provide a basis for the clinical response to similar cases.
Funding: This research was supported by grants from the Research Foundation of Hwa Mei Hospital, University of Chinese Academy of Sciences, China (2020HMKY22); the Zhejiang Medicine and Health Science and Technology Project (2021424731); and Ningbo Medical Key Discipline (2022-F16).
Ethics approval: The study was approved by the Ethics Committee of Hwa Mei Hospital. Informed written consent was obtained from the patient's legal representative for publication of this report and any accompanying images.
Conflicts of interests: The authors have no conflicts of interest.
Contributors: LWD wrote the study. All authors have made substantial contributions to the acquisition, analysis, or interpretation of data for the work and drafting the work or revising it critically for important intellectual content, and provided final approval of the version to be published.
Reference
Atypical aortic arch branching variants: a novel marker for thoracic aortic disease
DOI:10.1016/j.jtcvs.2015.02.019
PMID:25802134
[Cited within: 2]

To examine the potential of aortic arch variants, specifically bovine aortic arch, isolated left vertebral artery, and aberrant right subclavian artery, as markers for thoracic aortic disease (TAD).We screened imaging data of 556 patients undergoing surgery due to TAD for presence of aortic arch variations. Demographic data were collected during chart review and compared with a historical control group of 4617 patients.Out of 556 patients with TAD, 33.5% (186 patients) demonstrated anomalies of the aortic arch, compared with 18.2% in the control group (P <.001). Three hundred seventy (66.5%) had no anomaly of the aortic arch. Bovine aortic arch emerged as the most common anomalous branch pattern with a prevalence of 24.6% (n = 137). Thirty-five patients (6.3%) had an isolated left vertebral artery, and 10 patients (1.8%) had an aberrant right subclavian artery. When compared with the control group, all 3 arch variations showed significant higher prevalence in patients with TAD (P <.001). Patients with aortic aneurysms and anomalous branch patterns had hypertension less frequently (73.5% vs 81.8%; P =.048), but had a higher rate of bicuspid aortic valve (40.8% vs 30.6%; P =.042) when compared with patients with aneurysms but normal aortic arch anatomy. Patients with aortic branch variations were significantly younger (58.6 ± 13.7 years vs 62.4 ± 12.9 years; P =.002) and needed intervention for the aortic arch more frequently than patients with normal arch anatomy (46% vs 34.6%; P =.023).Aortic arch variations are significantly more common in patients with TAD than in the general population. Atypical branching variants may warrant consideration as potential anatomic markers for future development of TAD.Copyright © 2015 The American Association for Thoracic Surgery. Published by Elsevier Inc. All rights reserved.
Right aortic arch with aberrant left innominate artery in a 4-week-old infant: contrast-enhanced magnetic resonance angiography findings with three-dimensional reconstructions
DOI:10.1007/s00246-010-9706-9 URL [Cited within: 1]
Aberrant left innominate artery from the left descending aorta in right aortic arch: echocardiographic diagnosis
An additional challenge for head and neck radiologists: anatomic variants posing a surgical risk - a pictorial review
DOI:10.1186/s13244-019-0794-7 URL [Cited within: 1]
Diverse presentation of aberrant origin of the right subclavian artery: two case reports
PMID:9404777
[Cited within: 1]

Aberrant origin of the right subclavian artery occurs in up to 1% of the population and can result in a wide range of symptoms. In this report, two cases of this anomaly are presented. In the first case, a patient developed fatal group A streptococcal aortitis. In the second case, the patient complained of chronic cough and intermittent dyspnea. The embryologic genesis of this abnormality is discussed and the current literature is summarized. Although relatively uncommon, it is important to consider this vascular anomaly in the differential diagnosis of patients with dysphagia, dyspnea, chest pain, fever, or mediastinal widening evidenced on chest roentgenography.
Tracheoinnominate artery fistula after laryngotracheal separation: prevention and management
DOI:10.1016/j.jpedsurg.2011.11.029 URL [Cited within: 1]
Outcome predictors for severely brain-injured patients directly admitted or transferred from emergency departments to a trauma center
DOI:10.5847/wjem.j.1920-8642.2020.02.010 PMID:32076479 [Cited within: 1]
Percutaneous dilatational tracheotomy in high-risk ICU patients
DOI:10.1186/s13613-021-00906-5
PMID:34319491
[Cited within: 1]

Percutaneous dilatational tracheotomy (PDT) has become an established procedure in intensive care units (ICU). However, the safety of this method has been under debate given the growing number of critically ill patients with high bleeding risk receiving anticoagulation, dual antiplatelet therapy (DAPT) or even a combination of both, i.e. triple therapy. Therefore, the purpose of this study, including such a high proportion of patients on antithrombotic therapy, was to investigate whether PDT in high-risk ICU patients is associated with elevated procedural complications and to analyse the risk factors for bleeding occurring during and after PDT.PDT interventions conducted in ICUs at 12 European sites between January 2016 and October 2019 were retrospectively analysed for procedural complications. For subgroup analyses, patient stratification into clinically relevant risk groups based on anticoagulation and antiplatelet treatment regimens was performed and the predictors of bleeding occurrence were analysed.In total, 671 patients receiving PDT were included and stratified into four clinically relevant antithrombotic treatment groups: (1) intravenous unfractionated heparin (iUFH, prophylactic dosage) (n = 101); (2) iUFH (therapeutic dosage) (n = 131); (3) antiplatelet therapy (aspirin and/or P2Y receptor inhibitor) with iUFH (prophylactic or therapeutic dosage) except for triple therapy (n = 290) and (4) triple therapy (DAPT with iUFH in therapeutic dosage) (n = 149). Within the whole cohort, 74 (11%) bleedings were reported to be procedure-related. Bleeding occurrence during and after PDT was independently associated with low platelet count (OR 0.73, 95% CI [0.56, 0.92], p = 0.009), chronic kidney disease (OR 1.75, 95% CI [1.01, 3.03], p = 0.047) and previous stroke (OR 2.13, 95% CI [1.1, 3.97], p = 0.02).In this international, multicenter study bronchoscopy-guided PDT was a safe and low-complication airway management option, even in a cohort of high risk for bleeding on cardiovascular ICUs. Low platelet count, chronic kidney disease and previous stroke were identified as independent risk factors of bleeding during and after PDT but not triple therapy.© 2021. The Author(s).
Death after percutaneous dilatational tracheostomy: a systematic review and analysis of risk factors
DOI:10.1186/cc13085 URL [Cited within: 1]
Tracheotomy in the intensive care unit: guidelines from a French expert panel
DOI:10.1186/s13613-018-0381-y
PMID:29546588
[Cited within: 3]

Tracheotomy is widely used in intensive care units, albeit with great disparities between medical teams in terms of frequency and modality. Indications and techniques are, however, associated with variable levels of evidence based on inhomogeneous or even contradictory literature. Our aim was to conduct a systematic analysis of the published data in order to provide guidelines. We present herein recommendations for the use of tracheotomy in adult critically ill patients developed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method. These guidelines were conducted by a group of experts from the French Intensive Care Society (Societe de Reanimation de Langue Francaise) and the French Society of Anesthesia and Intensive Care Medicine (Societe Francaise d'Anesthesie Reanimation) with the participation of the French Emergency Medicine Association (Societe Francaise de Medecine d'Urgence), the French Society of Otorhinolaryngology. Sixteen experts and two coordinators agreed to consider questions concerning tracheotomy and its practical implementation. Five topics were defined: indications and contraindications for tracheotomy in intensive care, tracheotomy techniques in intensive care, modalities of tracheotomy in intensive care, management of patients undergoing tracheotomy in intensive care, and decannulation in intensive care. The summary made by the experts and the application of GRADE methodology led to the drawing up of 8 formal guidelines, 10 recommendations, and 3 treatment protocols. Among the 8 formal guidelines, 2 have a high level of proof (Grade 1+/-) and 6 a low level of proof (Grade 2+/-). For the 10 recommendations, GRADE methodology was not applicable and instead 10 expert opinions were produced.
Safety and efficacy of ultrasonography before and during percutaneous dilatational tracheostomy in adult patients: a systematic review
PMID:23230879
[Cited within: 2]

A systematic review to examine the safety and efficacy of ultrasound before and/or during percutaneous dilatational tracheostomy (PDT).Systematic searches of MEDLINE, PubMed, EMBASE, and the Cochrane Central Register of Controlled Trials were undertaken to identify trials reporting on safety and efficacy of using ultrasound guidance before and/or during PDT.Ultrasound before PDT: no controlled trials; two observational studies suggested a possible benefit in avoiding serious complications by identifying vulnerable vascular structures. Real-time ultrasound during PDT: one controlled study, which retrospectively compared real-time ultrasound guidance with the landmark-guided technique and found it to be superior in avoiding cranial misplacement; it appeared to be safe and effective in two observational studies.There are currently no randomised controlled trials to establish the safety or efficacy of preprocedural and/or real-time intraprocedural ultrasound guidance during PDT compared with the current standard of care. One study supports the use of real-time ultrasound guidance during PDT in preventing cranial tracheostomy tube misplacement. Observational data suggest that preprocedural ultrasound may help prevent vascular complications and that real-time ultrasound guidance during PDT is likely safe, with a high success rate. A prospective randomised controlled trial evaluating its safety and efficacy compared with the traditional landmarkguided technique is required to establish its role in clinical practice.
Percutaneous tracheostomy
DOI:10.1056/NEJMvcm2014884 URL [Cited within: 1]