Dear editor,
A 41-year-old male with liver cirrhosis suffered from abdominal fullness due to massive ascites. A 16-gauge needle catheter was inserted by Z-tract technique[1] into the right lower quadrant, and 3,000 mL of straw-colored ascites was drained. A pressure bandage was applied. There was no evidence of bleeding. The patient tolerated the procedure well and was discharged stable (blood pressure 124/72 mmHg [1 mmHg=0.133 kPa]; pulse rate 83 beats/minute). It was observed that the patient suffered from right lower quadrant pain and cold sweating when he revisited the emergency department at 13 hours after he was discharged. He was afebrile.
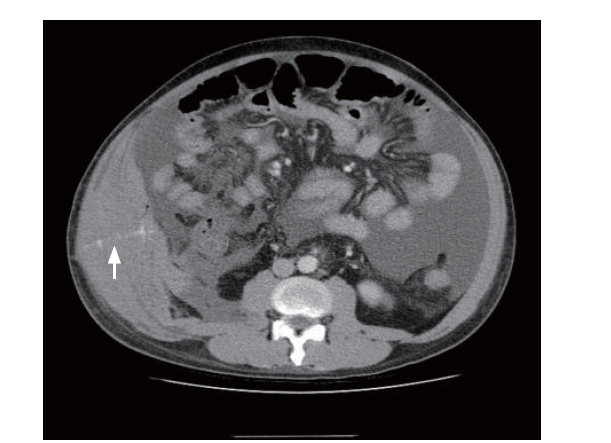
Reassessment revealed right lower quadrant tenderness. Neither leukocytosis nor elevation of C-reactive protein was noted. His blood pressure dropped to 93/52 mmHg with a compensatory pulse rate above 100 beats/minute. His hemoglobin dropped drastically from 9.2 g/dL to 4.7 g/dL within 13 hours. He denied hematemesis or hematochezia. Prothrombin time was prolonged with an international normalized ratio of 2.5. Abdominal computed tomography (CT) disclosed an abdominal wall hematoma with contrast medium leaking into a transmural needle-tract (Figure 1). Hemoperitoneum was confirmed by diagnostic fine-needle paracentesis. His condition was eventually stabilized after aggressive fluid resuscitation and blood transfusion.
Figure 1.
Figure 1.
Contrast medium extravasation into a needle-tract after abdominal paracentesis (arrow).
Although paracentesis is considered a relatively safe procedure,[2] abdominal wall hematomas occur in less than 2% of punctures, and significant bleeding in less than 0.2%.[3,4] A reasonable length of time for close observation of hemodynamic changes after the procedure, instead of a prompt discharge, is a simple safeguarded measure for early detection of occult hemorrhage.
Funding: None.
Ethical approval: Not needed.
Conflicts of interests: The authors have no competing interests relevant to the present study.
Contributors: CSL wrote the study. All authors read and approved the final manuscript.
Reference
Paracentesis of ascitic fluid. A safe procedure
PMID:2946271
[Cited within: 1]

A prospective study of 229 abdominal paracenteses performed on 125 patients with ascites revealed only two major complications (transfusion-requiring abdominal wall hematomas) in a single patient (0.9% of paracenteses and 0.8% of patients), and two minor complications (non-transfusion-requiring hematomas) in two patients (0.9% of paracenteses and 1.6% of patients). No paracentesis resulted in bacterial peritonitis or death. Abdominal paracentesis in patients with ascites is a safe procedure. Fear of complications of the procedure should not preclude performing a paracentesis, provided certain precautions are taken.
Severe hemorrhage following abdominal paracentesis for ascites in patients with liver disease
DOI:10.1111/apt.2005.21.issue-5 URL [Cited within: 1]
Lack of increased bleeding after paracentesis and thoracentesis in patients with mild coagulation abnormalities
DOI:10.1046/j.1537-2995.1991.31291142949.x URL [Cited within: 1]