Dear editor,
Deep vein thrombosis (DVT) is a common peripheral vascular disease, causing pulmonary embolism, post-venous thrombosis syndrome, chronic thrombotic pulmonary hypertension, and other complications.[1] The inferior vena cava filter (IVCF) implantation combined with adequate anticoagulation could lower the incidence of fatal PE to <1%.[2] In clinical practice, the double inferior vena cava (IVC) malformation along with lower extremity DVT (LEDVT) is rarely seen, and poor perception towards this disease easily leads to misdiagnosis and mistreatment. This report summarized the diagnosis and treatment of a case with double IVC who underwent IVCF implantation, and also discussed relevant literature in order to improve the understanding of double IVC malformation.
CASE
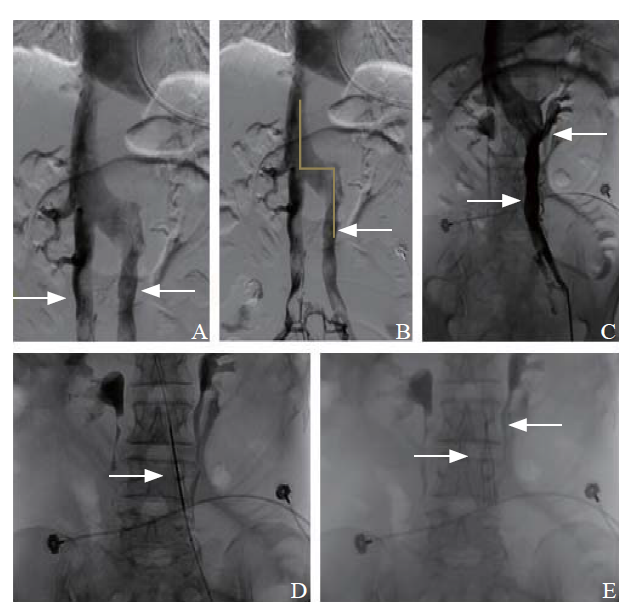
A 60-year-old female, who had a history of cervical carcinoma and radiotherapy two years ago, was admitted to our hospital due to vaginal bleeding along with edema of the left lower limb for one day. Arteriovenous B-ultrasonography of both lower extremities showed thrombosis in the left superficial femoral vein and deep femoral vein. The blood flow in the remaining veins of the left lower limb was slow. Unobstructed blood flow was observed in deep veins of the right lower limb. However, color Doppler ultrasound was not used to diagnose the IVC. Abdominal computed tomography (CT) scan indicated intestinal obstruction and a small volume of pelvic effusion. The D-dimer test was positive. This patient had several risk factors for pulmonary embolism, including cancer, long-term bedrest, and DVT. Due to vaginal bleeding, anticoagulant treatment was contraindicated, so an IVCF was inserted to prevent pulmonary embolism. Next, under topical anesthesia, the right femoral vein was percutaneously punctured using Seldinger puncture technique, and a 6F vascular sheath was indwelled into the vein. Angiography of the right femoral vein displayed malformation of the IVC. However, due to the high vertical positioning at the point of confluence, the double IVC was invisible (Figure 1A). The left lower extremity DVT could not be blocked effectively. If the IVCF was placed through the internal jugular vein, the opening angle of the left IVC was too large, thereby increasing the difficulty (Figure 1B). Preoperative B-ultrasound indicated no obvious thrombosis in the left common femoral vein, and the approach of the left common femoral vein was straighter. Therefore, the left femoral vein was punctured to indwell a 6F vascular sheath. Intraoperative angiography illustrated patency of left common iliac vein (LCIV) and IVC (Figure 1C). The ostium of the left renal vein was localized near the upper edge of the third lumbar vertebrae, and the guide wire and catheter were coordinated to enter the IVC, followed by retrieval of the catheter and vascular sheath, and placement of an ARGON IVCF (Figure 1D). The filter was adjusted and positioned below the level of left renal vein and then released (Figure 1E). Intraoperative angiography displayed unobstructed LCIV and IVC. One month and six months after surgery, ultrasound examinations of lower extremity deep vein indicated disappearance of DVT, and repeat computed tomography pulmonary angiography (CTPA) showed no pulmonary embolism.
Figure 1.
Figure 1.
Results of angiography. A: malformation of double inferior vena cava (IVC) was observed (the right femoral vein angiography); B: if the inferior vena cava filter was placed through the internal jugular vein, the opening angle of the left inferior vena cava was too large; C: the ostium of the left renal vein was localized near the upper edge of the third lumbar vertebrae (the left femoral vein angiography); D: implantation of an inferior vena cava filter; E: the IVC was lower than the ostium of the left renal vein (inferior vena cava position).
DISCUSSION
LEDVT is the most common cause of PE. IVCF implantation is an effective prophylactic measure against PE. IVCFs remain the only treatment option for patients with acute (within 2-4 weeks) proximal DVT or pulmonary embolism and an absolute contraindication to anticoagulation.[3]
There are no differences in the all-cause mortality among DVT patients treated with IVCFs compared to those treated with anticoagulation therapy alone. Prophylactic IVCFs are occasionally inserted in patients at high risk of developing venous thromboembolism (VTE), especially if anticoagulation is contraindicated.[4]
The double IVC has been rarely reported. IVC malformation is shown to be asymptomatic in most of the patients, and often found by accident during autopsy or imaging examination. Embryological development of IVC remains complicated and diverse congenital malformations could occur, leading to an incidence of double IVC of about 0.2%-3.0%.[5] Most of the patients with double IVC are asymptomatic.
Anomalous development of vena cava occurs in a small portion of double IVC patients, which presents as vena cava stenosis and poor collateral compensation, resulting in the obstruction of venous drainage. The common clinical complication in this type of malformation is thrombosis in the IVC and lower extremity deep veins, manifesting as lower extremity swelling, pain, and varicosity. In patients with left IVC malformation, the IVC is susceptible to compression and stenosis at the anterior or posterior sites of the aorta above the kidney level when horizontally circumventing it. This in turn causes disturbance in the venous drainage at the distal end of stenosis and venous hypertension, probably resulting in LEDVT, nutcracker syndrome, and pelvic congestion syndrome.[6,7,8,9,10]
Interventions for IVC malformations accompanied by LEDVT are similar to LEDVT, which include anticoagulation, IVCF implantation, catheter-directed thrombolysis (CDT), and thrombus extraction.[11,12,13] When IVC malformations are exposed during operation, a revised surgical approach and IVCF is used to fully exert its effect. The operation guidelines for filter implantation recommend to examine possible vascular malformations before ICVF implantation.[14] Before implantation surgery, any existing vascular malformations of the vena cava are identified by color Doppler ultrasound, enhanced CT, and magnetic resonance imaging (MRI).[15] Nonetheless, given the medical facility conditions and cost, it is not feasible to perform enhanced CT and MRI scan for all patients scheduled for filter implantation, whereas color Doppler ultrasound of the IVC and hepatic vein are considered to be simple and accurate. Therefore, before ICVF implantation, a routine color Doppler ultrasound of IVC should be conducted to clarify the overall IVC condition. For cases without color Doppler ultrasound inspection, intraoperative angiography of the IVC should be performed to determine its condition.
However, a definite guideline or expert consensus on the position of IVCF implantation for double IVC malformation is lacking. According to an analysis on positions of implanted filter for dual IVC, an ICVF could be implanted in each IVC for patients with dual IVC along with bilateral DVT, and the position could be below the level of the renal vein ostia.[16] In this case, the patient developed thrombosis in the left common femoral vein, superficial femoral vein, and deep femoral vein, while no blood flow obstruction or thrombosis was detected in the right lower extremity deep veins. Therefore, we clearly explained the situation to the family members and only placed a filter in the left IVC.
CONCLUSIONS
IVC malformation is usually misdiagnosed and mistreated. IVCF implantation for double IVC complicated by LEDVT is rarely reported, but this operation can effectively prevent the occurrence of PE caused by acute LEDVT, and is perceived to be an effective and reliable therapy. Nonetheless, a comprehensive and effective examination and assessment should be conducted before surgery. During IVCF implantation, bilateral renal vein angiography should be performed to exclude the possibility of congenital IVC variants or malformations, thereby accomplishing accurate implantation of IVCF and PE-preventing effects. In patients whose confluences of the two IVCs are higher than the openings of bilateral renal veins, if no DVT is found in one side of the lower extremity, the IVCF need not be placed on this side.
Funding: This study was funded by the Science and Technology program of Jinhua Science and Technology Bureau (2020-4-114).
Ethical approval: The study protocol was reviewed and approved by the Institutional Review Board of the Fourth Affiliated Hospital of Zhejiang University School of Medicine.
Conflicts of interests: The authors declare no conflicts of interest regarding the publication of this paper.
Contributors: LJ proposed the study, and wrote the first draft. All authors have read and approved the final version.
Reference
The postthrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies: a scientific statement from the American Heart Association
DOI:10.1161/CIR.0000000000000130 URL [Cited within: 1]
Photothermal ablation with the excimer laser sheath technique for embedded inferior vena cava filter removal: initial results from a prospective study
DOI:10.1016/j.jvir.2011.01.459 URL [Cited within: 1]
Inferior vena cava filters
DOI:10.1111/jth.13564
PMID:28019712
[Cited within: 1]

Use of inferior vena cava (IVC) filters has increased dramatically in recent decades, despite a lack of evidence that their use has impacted venous thromboembolism (VTE)-related mortality. This increased use appears to be primarily driven by the insertion of retrievable filters for prophylactic indications. A growing body of evidence, however, suggests that IVC filters are frequently associated with clinically important adverse events, prompting a closer look at their role. We sought to narratively review the current evidence on the efficacy and safety of IVC filter placements. Inferior vena cava filters remain the only treatment option for patients with an acute (within 2-4 weeks) proximal deep vein thrombosis (DVT) or pulmonary embolism and an absolute contraindication to anticoagulation. In such patients, anticoagulation should be resumed and IVC filters removed as soon as the contraindication has passed. For all other indications, there is insufficient evidence to support the use of IVC filters and high-quality trials are required. In patients where an IVC filter remains, regular follow-up to reassess removal and screen for filter-related complications should occur.© 2016 International Society on Thrombosis and Haemostasis.
Double inferior vena cava and its implications during endovascular and surgical interventions: a word of caution
Left-sided and duplicate inferior vena cava: a case series and review
DOI:10.1002/ca.v26.8 URL [Cited within: 1]
Embryogenetic malformations of the inferior vena cava, and their manifestations in adults
Inferior vena cava obstruction and collateral circulation as unusual manifestations of hepatobiliary cystadenocarcinoma
DOI:10.1016/S1499-3872(13)60052-1 URL [Cited within: 1]
Compressive symptoms due to thrombosed or hypertrophic collateral circulation in infrarenal inferior vena cava agenesis
Chronic venous insufficiency in patients with absence of the inferior vena cava
Long-term efficacy of two vena cava filter implants for congenital duplicated inferior vena cava
DOI:10.1016/j.acvd.2008.06.009 PMID:19233113 [Cited within: 1]
Mechanical and pharmacologic catheter-directed thrombolysis treatment of severe, symptomatic, bilateral deep vein thrombosis with congenital absence of the inferior vena cava
DOI:10.1016/j.jvs.2011.02.012 URL [Cited within: 1]
Treatment of venous thromboembolism
DOI:10.1001/jama.2014.65 URL [Cited within: 1]
The consensus among Chinese interventional experts on the standard of inferior vena cava filter insertion and retrieval
The complications due to inferior vena cava abnormality and their interventional management
Duplicate inferior vena cava filters: more is not always better
DOI:10.1016/j.ajem.2015.04.083 URL [Cited within: 1]