Dear editor,
Pancreatic carcinoma is highly malignant and is mainly characterized by a low rate of eligibility for curative-intent resection, rapid metastases and/or local relapses even after surgery.[1,2,3] Imaging examinations like enhanced computed tomography (CT)/magnetic resonance imaging (MRI), and positron emission tomography-computed tomography (PET-CT), play an important role in detecting tumor recurrence or residual after radical resection of pancreatic cancer. However, these detection platforms are increasingly reported to have insufficient sensitivity and specificity.[4,5] Here we report a pancreatic cancer patient who had progressively increased carbohydrate antigen 19-9 (CA199) level one year and three months after surgery; however, none of the above imaging methods were able to identify the cause. After our investigations, we discovered mediastinal metastasis using endoscopic ultrasonography (EUS) and confirmed by EUS-guided fine needle aspiration (EUS-FNA).
CASE
A 49-year-old asymptomatic male patient was found to have progressively increased CA199 level within three months. He had partial pancreatectomy (pancreatic body and tail) and cholecystectomy due to pancreatic carcinoma one year and three months ago. From one month after surgery, the patient received preventative chemotherapy treatments (gemcitabine hydrochloride 1 g/m2, qw) for ten episodes (three months). A few nodules were found in the patient's lung when his pancreatic carcinoma was diagnosed. However, the nodules were stable and were not treated. Ten months after surgery, a routine CT scan indicated that one of the nodules had suspicious enlargement. Radiofrequency ablation was performed to remove the nodule. Three months ago, the patient's serum CA199 level was 48 U/mL, only a little higher than normal upper limits (40 U/mL). However, in the next two to three months, the CA199 level progressively rose to 129 U/mL. After that, the patient was arranged for chest and abdominal CT, abdominal MRI, and systematic PET-CT in a local hospital, but no obvious lesions were found. The patient was subsequently transferred to our hospital for further examination. Upon examination the patient was observed to have normal vital signs and nutritional status, with body mass index (BMI) 24.96 kg/m2. No abnormal signs were observed.
Laboratory results were as follows: platelets 373×109/L (normal [100-300]×109/L), blood glucose 9.89 mmol/L (normal 3.89-6.10 mmol/L), glycosuria test 3+; other parameters were within the normal range, such as white and red blood cell counts, blood electrolytes, aminopherase, bilirubin, amylase, and renal function. We tested many serum tumor markers such as alpha fetoprotein (AFP), carcinoembryonic antigen (CEA), carbohydrate antigen 12-5 (CA 125), carbohydrate antigen 50 (CA50), cytokeratin fragment 21-1 (CYFRA 21-1), carbohydrate antigen 72-4 (CA724), total prostate specific antigen (TPSA), free prostate specific antigen (FPSA), and neuron-specific enolase (NSE). CA199 and CA50 levels were higher than normal levels (CA199 136.2 U/mL, normal 0-35 U/mL; CA50 43.97 ng/mL, normal 0-25 ng/mL).
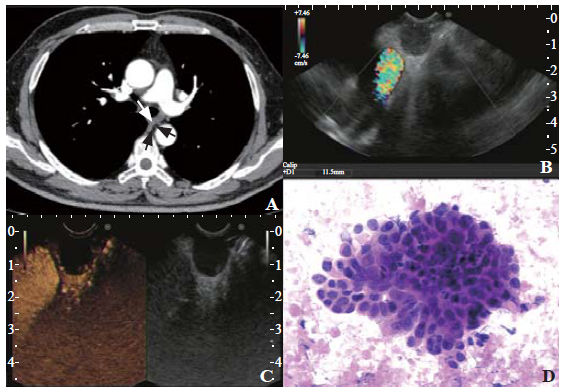
Because CA199 is commonly implicated in pancreatic cancer, we wanted to investigate the reason for increased CA199. Therefore, we arranged for chest, abdomen, and pelvis enhanced CT scan for the patient in our hospital. The CT scan did not find any abnormal lesions, except a small nodule in the right lower lung which remained the same size as previously scan. Importantly, no enlarged lymph nodes were observed in the pulmonary hilar and mediastinal areas (Figure 1A). Following these observations, our initial suspicion was that the rising levels of CA199 were due to residual cancer and remnant pancreas recurrence. Considering EUS is one of the best tools to discover small pancreatic cancer lesions (≤1 cm), we arranged the EUS for the patient. No abnormalities were found in his pancreas through EUS examination. However, with additional examination of mediastinum, we found a few low-echo lesions, and one of them was under suspicion of metastasis (Figure 1B). This lesion was close to the esophagus and was located among the esophagus, the thoracic aorta, and the spine, about 1 cm below the trachea carina. After intravenous injection of SonoVue, the lesion didn't show any enhancement (Figure 1C). To confirm diagnosis, we performed EUS-FNA of the mediastinum lesion. Soon, adenocarcinoma cells in the patient's specimen were detected. This was consistent with the reports from our pathologist which suggested the presence of metastasis of pancreatic cancer (Figure 1D). The patient was prepared to receive further radiotherapy and chemotherapy treatments, and the follow-up procedures were scheduled.
Figure 1.
Figure 1.
Results of computed tomography (CT) and endoscopic ultrasonography (EUS). A: no abnormal lesions were found by CT scan where EUS found the metastasis lesion (arrows); B: a low-echo lesion in mediastinum was found and suspicious of metastasis using EUS; C: no enhancement in the lesion was found after intravenous injection of SonoVue; D: malignant lesion was supported by cell samples from EUS-FNA, showing large variations in size and chromatin unevenly distributed with rough granules (magnification, ×100).
DISCUSSION
Pancreatic carcinoma is one of the life-threaten diseases. Even after multimodality therapy with surgical resection, the five-year overall survival rate can only reach 25% to 30%.[6] With this dreadful disease, about 80% of post-surgical patients promptly develop metastases and/or local relapses.[2] So, for a better prognosis of pancreatic carcinoma, it is very important to predict early metastasis and/or local relapse. CA199 and multiple imaging methods (e.g., enhanced CT/MRI) are usually considered to be the common tools for postoperative surveillance of patients after curative therapy.[1] However, these methods often fail to discover the lesion, especially when the lesion is small.[5] EUS has been well accepted as a preferable tool to detect the early small pancreatic carcinoma lesion (≤1 cm). However, its value in detecting metastases after curative therapy is not thoroughly investigated. In our study, we reported one patient suspicious of metastasis and/or relapse indicated by high rising CA199, who was finally confirmed by EUS.
In this study, the 49-year-old patient had radical surgery for pancreatic cancer more than one year ago with a rising serous CA199 level. It is important to distinguish cancer relapse and metastasis, because if relapse is confirmed, additional surgery may be a fundamental solution. In case of the subject reported in this study, none of contrast CT, MRI or PET-CT found the cause. At last, thanks to EUS, the metastasis lesion was found in mediastinum, and specimen from EUS-FNA samples confirmed the malignant nature.
The follow-up procedures after pancreatectomy are still controversial. Using cost-effective analyses, some studies concluded that increasing the frequency and intensity of postoperative surveillance after curative therapy is beyond clinical evaluation and CA 199 testing every six months increases cost but confers no clinically significant survival benefit.[7] Beyond follow-up procedures, eligible tools with enough sensibility for detecting tumor relapse and/or metastasis are also important. CA199 has been considered to be the best serum biomarker for postoperative follow-up, but not perfect for sensitivity.[8,9] Enhanced CT and MRI were the frequently used methods for follow-up survey, but with insufficient specificity and sensitivity.[4] There are relatively fewer studies on PET-CT follow-up value for pancreatic cancer. The conclusion indicates that PET-CT has a high sensitivity for pancreatic cancer recurrence and metastasis, and can be a supplementary to enhanced CT[9] but with less sensitivity for lymphatic metastasis.[10] EUS is a good tool to detect biliopancreatic disease, and it is reported that EUS is helpful to diagnose synchronous primary pancreatic adenocarcinoma.[11] However, its follow-up value of pancreatic cancer is not known yet. Our case study showed an important role of EUS in finding mediastinal metastasis which was not found by CT or PET-CT. We consider that EUS may be an optional choice to diagnose relapse and/or metastasis.
There are many interesting questions we have not revealed in our case. For instance, did the mediastinal lesion exist there before and become larger? Or was the lesion formed recently? If the former, we need to investigate thoroughly before surgery. And if the latter, we need to study the mechanism to intervene tumorigenesis. There are also many problems we need to resolve in the further study, e.g., the procedure of EUS checking in post-surgery patients and value of the enhanced EUS in the metastasis.
CONCLUSIONS
For investigating suspicious cancer relapse and/or metastasis, EUS is helpful to confirm the diagnosis. We also suggest that EUS should play an important role in detecting the metastasis and/or relapse in specific pancreatic cancer patients after surgery.
Funding: This study was supported by Group Medical Aid Project of the Tibet Autonomous Region Natural Science Foundation (XZ2020ZR-ZY28[Z]).
Ethical approval: Not needed.
Conflicts of interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors: HTW wrote the main body of the report. All authors approved the final version.
Reference
Potentially curable pancreatic cancer: American Aociety of Clinical Oncology Clinical Practice Guideline
DOI:10.1200/JCO.2016.67.5553 URL [Cited within: 2]
Potentially curable pancreatic cancer: American Society of Clinical Oncology Clinical Practice Guideline update
DOI:10.1200/JCO.2017.72.4948 URL [Cited within: 2]
Multicenter study of early pancreatic cancer in Japan
DOI:10.1016/j.pan.2017.11.007 URL [Cited within: 1]
Imaging findings of recurrent pancreatic cancer following resection
DOI:10.1007/s00261-017-1397-8
PMID:29198001
[Cited within: 2]

Pancreatic cancer is a challenging malignancy to treat, largely due to aggressive regional involvement, early systemic dissemination, high recurrence rate, and subsequent low patient survival. Generally, 15-20% of newly diagnosed pancreatic cancers are candidates for possible curative resection. Eighty percent of these patients, however, will experience locoregional or distant recurrence in first 2 years. Although there is no strong evidence-based guideline for optimal surveillance after pancreatic cancer resection, careful comparison of surveillance follow-up multi-detector CT (MDCT) studies with a postoperative baseline MDCT examination aids detection of early recurrent pancreatic cancer. In this review article, we describe imaging findings suggestive of recurrent pancreatic cancer and review routine and alternative imaging options.
Metastatic pancreatic cancer: American Society of Clinical Oncology Clinical Practice Guideline
DOI:10.1200/JCO.2016.67.1412 URL [Cited within: 2]
Long-term survival after multidisciplinary management of resected pancreatic adenocarcinoma
DOI:10.1245/s10434-008-0295-2 URL [Cited within: 1]
Frequency and intensity of postoperative surveillance after curative treatment of pancreatic cancer: a cost-effectiveness analysis
DOI:10.1245/s10434-013-2889-6 URL [Cited within: 1]
Biomarkers in pancreatic adenocarcinoma: current perspectives
DOI:10.2147/OTT URL [Cited within: 1]
Utility of (18) F-FDG PET/CT and CECT in conjunction with serum CA 19-9 for detecting recurrent pancreatic adenocarcinoma
DOI:10.1007/s00261-017-1316-z
PMID:28900703
[Cited within: 2]

The roles of different cross-sectional imaging in evaluating the recurrence of pancreatic adenocarcinoma are not well established. We evaluated the utility of F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) and contrast-enhanced computed tomography (CECT) in the diagnosis of recurrent pancreatic adenocarcinoma in conjunction with the tumor marker CA 19-9.We retrospectively reviewed the records of patients who underwent CECT and FDG PET/CT along with serum CA 19-9 measurement as a follow-up or on a clinical suspicion of recurrent disease after initial surgery for pancreatic adenocarcinoma. Two observers blinded to the other imaging modality results retrospectively reviewed and interpreted the images in consensus using a three-point scale (negative, equivocal, or positive). Pathologic analysis by biopsy or further clinical and radiologic follow-up determined the true status of the suspected recurrences. The imaging results were compared with CA 19-9 levels and true disease status.Thirty-nine patients were included in the study. Thirty-three patients (85%) had proven recurrent cancer and six patients (15%) had no evidence of disease. Twenty-four patients had elevated CA 19-9 and 15 patients had normal CA 19-9. Sensitivity, specificity, and accuracy for recurrence were 90.9%, 100.0%, and 92.3% for PET/CT and 72.2%, 66.6%, and 71.7% for CECT, respectively. Sensitivity for locoregional recurrence was 94.4% for PET/CT but only 61.1% for CECT. PET/CT detected recurrence in 12 patients who had normal levels of CA 19-9. PET/CT showed lesions not visible on CECT in five (15%) patients. Although the sensitivity and specificity of PET/CT were higher than those of CECT, they were not statistically significant (p = 0.489 and p = 0.1489, respectively).FDG PET/CT has a high sensitivity for pancreatic cancer recurrence. Normal CA 19-9 does not necessarily exclude these recurrences. FDG PET/CT is useful when CECT is equivocal and can detect recurrence in patients with normal CA 19-9.
FDG-PET in diagnosis, staging and prognosis of pancreatic carcinoma: a meta-analysis
DOI:10.3748/wjg.v19.i29.4808 URL [Cited within: 1]
Endoscopic ultrasound fine-needle aspiration diagnosis of synchronous primary pancreatic adenocarcinoma and effects on staging and resectability
DOI:10.1016/j.cgh.2016.08.009 URL [Cited within: 1]