Dear editor,
Salbutamol is a common medication used in a variety of clinical settings. While there have been many reported cases of orally ingested salbutamol toxicity, there have only been a few reports of inhaled salbutamol overdose. We describe a case of acute inhaled salbutamol toxicity with a combination of clinical findings that have not been previously reported together in a single case. Given the ubiquitous use of salbutamol, many patients may experience symptoms of overdose on a spectrum that ranges from mild side effects to severe toxicity, which may be under-recognized by emergency physicians. We believe that it is important for all emergency clinicians to be aware of and recognize the syndrome of β2-agonist toxicity.
CASE
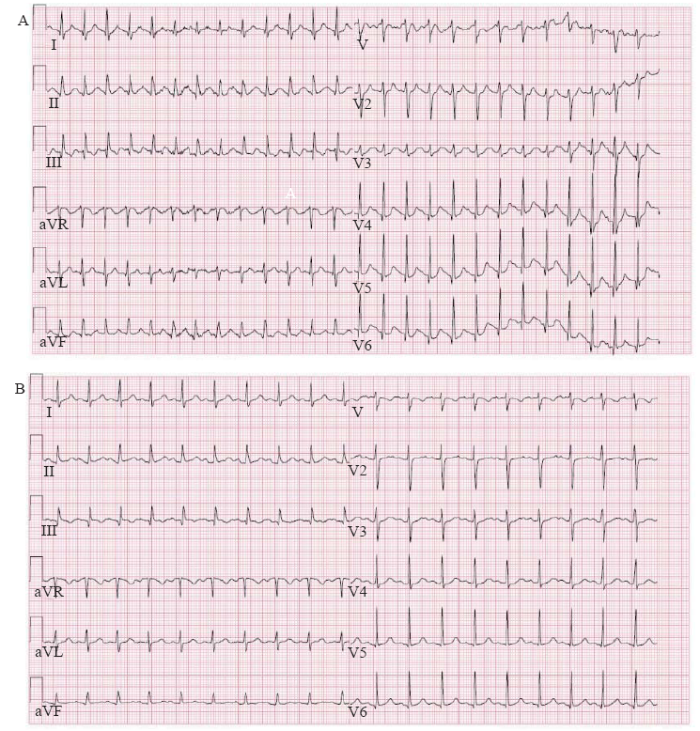
A 16-year-old female was brought to the emergency department (ED) for altered level of consciousness. Cardiac monitors and electrocardiogram (ECG) showed supraventricular tachycardia at 160 beats per minute with a prolonged corrected QT interval (QTc 525 ms) (Figure 1A). Her respiratory rate was 35 breaths per minute. The remaining vital signs were normal: oxygen saturation on room air 100%, blood pressure 110/84 mmHg (1 mmHg=0.133 kPa), temperature 36.7 °C, and point-of-care glucose 7.0 mmol/L. Her initial Glasgow Coma Scale (GCS) was 14.
Figure 1.
Figure 1.
Serial electrocardiograms of a 16-year-old patient with acute salbutamol toxicity. A: initial electrocardiogram at presentation showing supraventricular tachycardia at 160 beats per minute; movement artifact was due to intermittent tremors; B: repeat electrocardiogram 1.5 hours after initial presentation and treatment with diltiazem showing sinus tachycardia at 115 beats per minute.
The patient’s medical history was significant for asthma and her only medication was a salbutamol (Ventolin HFA, GlaxoSmithKline) inhaler. The patient reported experiencing an “asthma attack” a few hours before presenting to the ED and using her salbutamol inhaler approximately 15 times during that time. She also reported taking two tablets of acetaminophen but denied any other ingestions.
On physical examination, the patient was agitated, with no increased work of breathing or airway compromise. The patient’s chest was clear to auscultation, with no wheezes or crackles. Cardiac exam revealed a fast and regular rhythm, with no murmurs. Abdominal and screening neurologic exams were unremarkable.
The patient was given diltiazem (20 mg intravenously) for her supraventricular tachycardia and 1 L normal saline.
An initial venous blood gas (VBG) revealed respiratory alkalosis with metabolic acidosis and lactate 8.1 mmol/L. Other significant findings on bloodwork included potassium 2.9 mmol/L, phosphate 0.43 mmol/L (reference range 0.92-1.55 mmol/L), and acetaminophen level 86 μmol/L. The anion gap was 17 mmol/L and the osmolal gap was normal. Creatine kinase and troponin were normal. Serum salicylate and ethanol levels were undetectable. Serum β-human chorionic gonadotropin was negative. Chest radiograph and non-contrast computed tomography of the head were unremarkable.
On clinical reassessment 1.5 hours after her initial presentation, the patient was oriented and ambulatory, and had no complaints. Repeat ECG showed sinus tachycardia at 115 beats per minute (QTc 473 ms) (Figure 1B). Serial VBGs showed improvement of her lactic acidosis. The four-hour acetaminophen level was undetectable. Six hours after her initial presentation, the patient was discharged home from the ED with instructions about proper use and dosing of her salbutamol inhaler.
DISCUSSION
We describe a case of inhaled salbutamol toxicity presenting with supraventricular tachycardia, QTc prolongation, hypokalemia, and marked lactic acidosis. There are only a few reports of inhaled salbutamol toxicity and no previous case has reported the combination of clinical findings that we have described.[1,2,3,4]
Mechanisms
Salbutamol stimulates β2-adrenergic receptors to provide rapid bronchodilation through cyclic adenosine monophosphate (cAMP)-mediated bronchial smooth muscle relaxation.[5] While salbutamol is relatively selective for β2-adrenergic receptors, it has been shown to have β1-receptor effects in the myocardium.[5] In addition, β1- and β2-adrenergic receptors coexist in the heart.[6] Stimulation of cardiac β2-receptors increases both chronotropy and inotropy and increases myocardial oxygen demand. In overdose, receptor specificity may be lost and β2-agonists may cause tachycardia, cardiac ischemia, and arrhythmias such as atrial fibrillation, supraventricular tachycardia, and ventricular tachycardia.[6]
Salbutamol causes hypokalemia primarily through β2-stimulation of the Na+/K+-ATPase pump in skeletal muscle, which shifts potassium intracellularly.[7] Hypokalemia caused by β2-agonists can be significant enough to produce ECG changes such as QT prolongation and U-waves. During exacerbations of chronic obstructive lung disease, concomitant hypoxemia and alterations in plasma pH may further increase the risk of cardiac arrhythmias.[3]
Acute salbutamol toxicity may also cause lactic acidosis. β2-adrenergic stimulation is thought to increase cAMP-mediated gluconeogenesis and lipolysis.[4] This causes increased plasma glucose, leading to increased conversion to pyruvate and lactate. This mechanism is in keeping with salbutamol also having been shown to cause transient hyperglycemia.[1]
Diagnosis and management
The diagnosis of salbutamol toxicity can be made based on clinical and laboratory findings as illustrated in our case. At high therapeutic doses, salbutamol can cause tachycardia, tremors, and hypokalemia. In overdose, salbutamol can additionally cause hyperglycemia, lactic acidosis, and cardiac arrhythmias.
Management of salbutamol toxicity is mainly supportive. Ramoska et al[8] reported that β-blockers may be considered for highly symptomatic patients in the absence of contraindications. Cardiac arrhythmias should be managed according to Advanced Cardiac Life Support Guidelines. Salbutamol-induced hypokalemia should be treated judiciously, if at all, since the underlying mechanism is transcellular shift and not a total body deficit.[3] While lactic acidosis is a known side effect of salbutamol overdose, clinicians should also carefully assess for other underlying causes of lactic acidosis.[4] Hyperventilation is a common finding among patients with metabolic acidosis. In the context of salbutamol toxicity, hyperventilation is typically a compensatory mechanism for metabolic acidosis as opposed to a sign of worsening respiratory distress that requires more β2-agonist therapy.[4]
CONCLUSIONS
Inhaled salbutamol overdose is uncommon, but the syndrome of β2-agonist toxicity is an important presentation to recognize. The diagnosis can be made based on clinical and laboratory findings. Key features include tremors, hypokalemia, hyperglycemia, lactic acidosis, and cardiac arrhythmias. The management is mainly supportive, including discontinuation of the offending agent and β-blockers for symptomatic treatment. Given the ubiquitous use of salbutamol and other β2-agonists, emergency physicians should be familiar with the diagnosis and management of β2-agonist toxicity.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval: The study was approved by the Ethics Committee of the hospital.
Conflicts of interest: The authors declare that they have no competing interests.
Contributors: All authors contributed substantially to the writing and revision of this manuscript and approved of its contents.
Reference
Unintentional oral beta agonist overdose: case report and review of the literature
DOI:10.1097/MJT.0b013e3182002f2d
URL
PMID:21317628
[Cited within: 2]

An 18-month-old male infant with oral albuterol intoxication was admitted to our pediatric emergency medicine unit with agitation, moderate hypokalemia (2.36 mEq/L), and hyperglycemia (180 mg/dL). His initial electrocardiogram showed sinus tachycardia with a low-amplitude T waves. He was admitted for observation, intravenous hydration was started with added potassium, blood glucose levels were closely monitored along with serum potassium and magnesium, and serial electrocardiography was performed. It should be stressed that as an oral bronchodilator, albuterol does not improve symptoms of asthma, and it can lead to severe complications, which can be avoided when this drug is delivered by inhalation or by a metered dose inhaler.
Recalcitrant supraventricular tachycardia: occult albuteral toxicity due to a factitious disorder
DOI:10.1016/j.jemermed.2015.05.007
URL
PMID:26162766
[Cited within: 1]

BACKGROUND: We report a case of a factitious disorder presenting with recurrent episodes of supraventricular tachycardia (SVT). CASE REPORT: A 26-year-old woman presented with recurrent episodes of SVT. Medical history included SVT, asthma, anxiety, depression, type 2 diabetes, and migraine headaches. The patient had frequent emergency department (ED) visits with complaints of chest pain, palpitations, and heart rates typically between 130 and 150 beats/min. Electrocardiograms revealed sinus tachycardia; laboratory studies were consistently normal except for periodic episodes of hypokalemia. Over the 3 years, the patient had more than 50 visits for health care and underwent multiple diagnostic evaluations, including comprehensive laboratory testing, echocardiography, Holter monitoring, and event monitoring. Given the constellation of clinical features, a plasma albuterol concentration was obtained during an ED visit for SVT, which was 17 ng/mL (reference range for peak plasma concentration after 0.04-0.1-mg inhaler dose = 0.6-1.4 ng/mL). A subsequent ED visit with a similar presentation revealed a plasma albuterol level of 11 ng/mL. The patient adamantly denied using this medication. Due to concerns about a factitious disorder, a multidisciplinary hospital discussion was planned for subsequent interventions; however, the patient was lost to follow-up. WHY SHOULD AN EMERGENCY PHYSICIAN BE AWARE OF THIS?: This is a compelling case report of a factitious disorder and occult albuterol abuse resulting in recalcitrant SVT with numerous ED visits and interventions. Patients with factitious disorders can have multiple visits for emergency care and are challenging to evaluate and treat. Albuterol toxicity can present with pronounced sinus tachycardia, fine tremor, and often with transient hypokalemia.
Hypokalemia in an asthmatic child from abuse of albuterol metered dose inhaler
DOI:10.1097/00006565-199804000-00015
URL
PMID:9583400
[Cited within: 3]

A case of albuterol abuse by a pediatric patient with the development of hypokalemia with electrocardiographic changes is presented. The hypokalemic effects of beta2-agonists are discussed in regard to the production of significant cardiac symptoms. Additionally, guidance regarding the evaluation of similar patients presenting in the emergency department is provided.
Metabolic acidosis due to inhaled salbutamol toxicity: a hazardous side effect complicating management of suspected cases of acute severe asthma
DOI:10.1016/j.mjafi.2011.10.002
URL
PMID:24532877
[Cited within: 4]

Metabolic acidosis has seldom been reported during treatment of asthma with use of beta agonist but not with much clinical consequence. We report two cases of metabolic acidosis with hyperventilation as a direct effect of salbutamol that caused difficulty in assessment and management of their respiratory symptoms which resolved with appropriate tapering of beta agonist.
A review of the toxicology of salbutamol (albuterol)
DOI:10.1007/s002040050059
URL
PMID:8067892
[Cited within: 2]

This paper reviews the published toxicology of salbutamol. Salbutamol is a relatively selective beta 2-adrenoreceptor stimulant with rapid, potent bronchodilator activity and only minor inotropic or chronotropic effects. It was not found to be mutagenic. LD50 values and other acute studies indicated low toxicity. Findings published for repeat dose studies were mainly uneventful. Tachycardia and flushing of the skin were observed in dogs. There were several findings peculiar to the rat--growth of the salivary gland, enlargement of the Harderian gland, an increase in colloid in the pituitary, and mesovarian leiomyomas. Increases in heart weights associated with inflammation, hypertrophy of muscle fibres, focal myocardial necrosis and fibrosis were seen in rats. Malformation, in the form of cleft palate, was reported in mice but not in rats or rabbits. These treatment related effects reported for salbutamol are not compound-related but rather are class-related. They are an expression of pharmacological activity brought about by the excessive beta stimulant action of high dosage with the drug.
Acute clenbuterol overdose resulting in supraventricular tachycardia and atrial fibrillation
Hypokalemia After pediatric albuterol overdose: a case series
DOI:10.1016/0735-6757(94)90202-x
URL
PMID:8285977
[Cited within: 1]

Sympathomimetic use results in a triad of hypokalemia, hyperglycemia, and elevated white blood cell count. Transient hypokalemia results from activation of the Na+/K+ pump and transport of potassium intracellularly. Increased serum glucose and insulin may also contribute to the intracellular shift of potassium after sympathomimetic use. Four cases of accidental pediatric albuterol ingestion with significant hypokalemia are reported. Four children between 1 and 6 years of age presented to the emergency department within 5 hours of ingesting 3.0, 1.1, 3.7, and 1.7 mg/kg albuterol, respectively. All four presented alert and oriented in no apparent distress. The most common findings were vomiting, sinus tachycardia, and hypokalemia (2.3, 2.5, 2.8, and 2.5 mmol/L, respectively). Each child received a single dose of activated charcoal and intravenous potassium replacement. All patients recovered uneventfully within 12 to 24 hours with supportive care only. These cases demonstrated that significant depressions in serum potassium can occur after pediatric albuterol overdose. Although transient, the dose-response relationship and duration of effect is unknown. Although significant hypokalemia can occur after ingestion of oral sympathomimetics, replacement should be managed on an individual basis until further studies are completed.
Propranolol treatment of albuterol poisoning in two asthmatic patients
URL PMID:8363123 [Cited within: 1]