World Journal of Emergency Medicine ›› 2013, Vol. 4 ›› Issue (4): 298-303.doi: 10.5847/wjem.j.issn.1920-8642.2013.04.011
• Original Articles • Previous Articles Next Articles
Yi Han1, Zhen-ju Song1, Chao-yang Tong1( ), Chun-sheng Li2
), Chun-sheng Li2
Received:2013-05-12
Accepted:2013-10-20
Online:2013-12-15
Published:2013-12-15
Contact:
Chao-yang Tong
E-mail:tong.chaoyang@zs-hospital.sh.cn
Yi Han, Zhen-ju Song, Chao-yang Tong, Chun-sheng Li. Effects of hypothermia on the liver in a swine model of cardiopulmonary resuscitation[J]. World Journal of Emergency Medicine, 2013, 4(4): 298-303.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn//EN/10.5847/wjem.j.issn.1920-8642.2013.04.011

Figure 1.
Changes of temperature, CO, CPP, SVR and DO2, VO2, ERO2 at baseline and each time point after ROSC in the LT and NT groups. Temperature in the LT group began to decrease at 10 minutes after ROSC, and was significantly lower than that in the NT group from 30 minutes to 4 hours after ROSC; CO in the LT group was significantly decreased from 30 minutes to 1 hour after ROSC, while there were no differences in the NT group; SVR in the LT and NT groups was not obviously changed before and after ROSC. DO2 in the LT group was decreased compared to the NT group, while VO2 in the LT group was more descent, ERO2 in the LT group increased more significantly than that in the NT group after ROSC, which was comparable to the result 2 hours after ROSC.
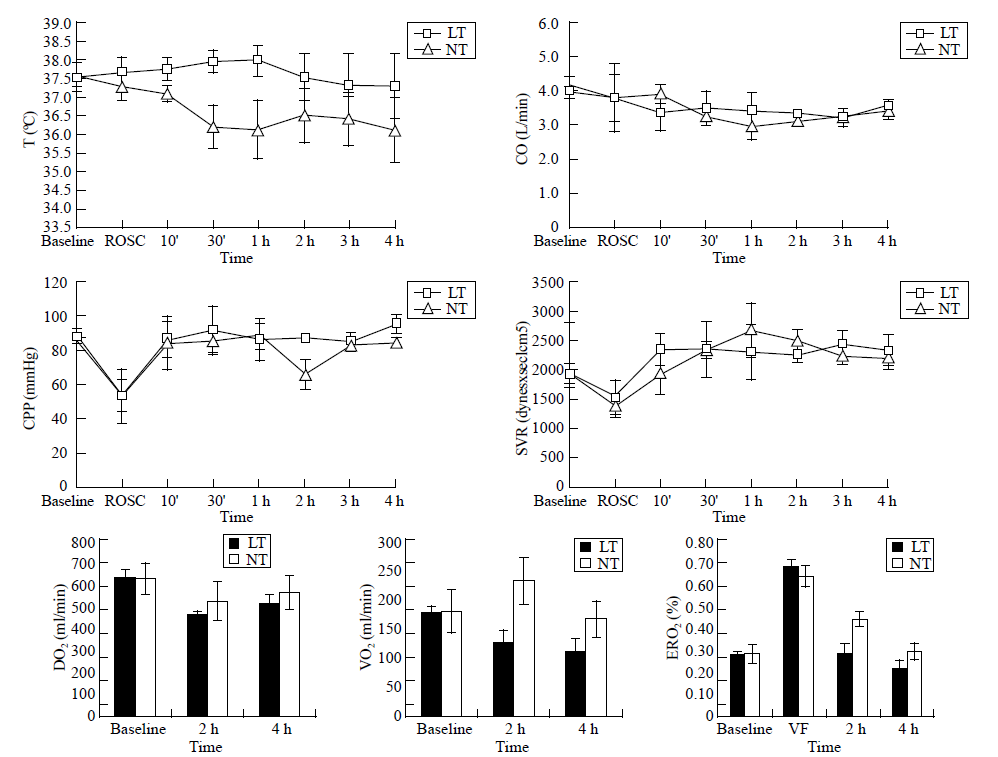
Table 1
Changes of AST, ALT and LDH in the LT and NT groups after CPR (mean±SD)
| Parameters | n | Baseline | ROSC | ||
|---|---|---|---|---|---|
| 10 min | 2 h | 4 h | |||
| AST (U/L) | |||||
| NT | 5 | 66.00±8.60 | 116.25±15.65* | 141.75±8.14# | 175.00±14.31# |
| LT | 5 | 69.50±12.04 | 114.75±3.82# | 119.75±6.95# | 126.25±11.15#? |
| ALT (U/L) | |||||
| NT | 5 | 44.25±7.37 | 49.75±3.10 | 50.25±4.99 | 52.00±5.89 |
| LT | 5 | 40.00±6.68 | 42.50±10.38 | 42.75±9.54 | 46.00±8.76? |
| LDH (U/L) | |||||
| NT | 5 | 672.25±90.60 | 829.25±74.20 | 1010.75±143.87* | 1240.00±116.62# |
| LT | 5 | 640.75±52.81 | 699.00±82.00 | 705.75±51.33? | 984.00±68.72? |
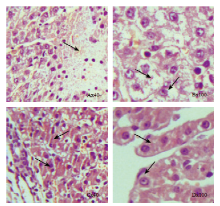
Figure 2.
Hepatic pathology of the LT and NT groups after CPR. NT: A, B; LT: C, D. A: Pyknosis and necrosis of hepatic cells; B: Narrowing hepatic sinusoid, extensive infiltration and adherence of inflammatory cells in the hepatic lobule; C: Hepatic cells were tight; D: Hepatic cells were tight.
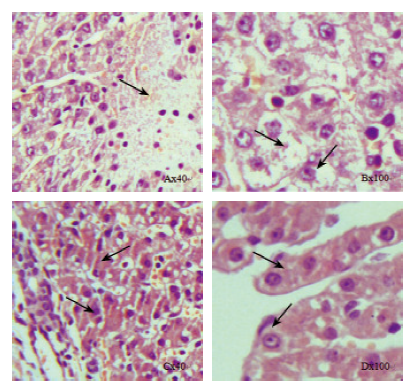
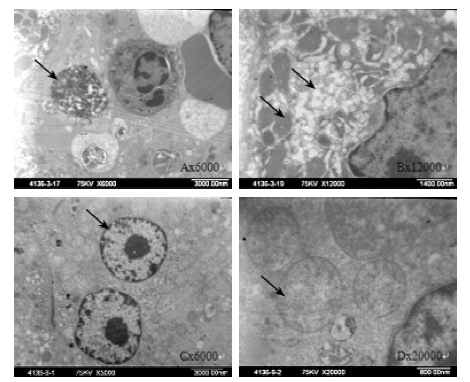
Figure 3.
Hepatic ultra microstructure of the LT and NT groups after CPR. NT: A, B; LT: C, D. A: A necrotic hepatic cell; B: The morphous of mitochondria in hepatic cell was irregular, and electron density increased; C: A normal hepatic cell; D: The morphous of mitochondria was regular, with mitochondrial crista.
| 1 |
Geocadin RG, Ritzl EK. Seizures and status epilepticus in post cardiac arrest syndrome: therapeutic opportunities to improve outcome or basis to withhold life sustaining therapies? Resuscitation 2012; 83:791-792.
pmid: 22513351 |
| 2 |
Zeiner A, Holzer M, Sterz F, Behringer W, Schörkhuber W, Müllner M, et al. Mild resuscitative hypothermia to improve neurological outcome after cardiac arrest. A clinical feasibility trial. Hypothermia After Cardiac Arrest (HACA) Study Group. Stroke 2000; 31:86-94.
doi: 10.1161/01.str.31.1.86 pmid: 10625721 |
| 3 |
Choi S, Noh J, Hirose R, Ferell L, Bedolli M, Roberts JP, et al. Mild hypothermia provides significant protection against ischemia/reperfusion injury in livers of obese and lean rats. Ann Surg 2005; 241:470-476.
doi: 10.1097/01.sla.0000154259.73060.f1 pmid: 15729070 |
| 4 |
Kulstad EB, Courtney MD, Waller D. Induction of therapeutic hypothermia via the esophagus: a proof of concept study. World J Emerg Med 2012; 3:118-122.
pmid: 25215049 |
| 5 |
Stadlbauer KH, Rheinberger K, Wenzel V, Raedler C, Krismer AC, Strohmenger HU, et al. The effects of nifedipine on ventricular fibrillation mean frequency in a porcine model of prolonged cardiopulmonary resuscitation. Anesth Analg 2003; 97:226-230.
pmid: 12818971 |
| 6 |
Nordmark J, Rubertsson S. Induction of mild hypothermia with infusion of cold (4 degrees C) fluid during ongoing experimental CPR. Resuscitation 2005; 66:357-365.
doi: 10.1016/j.resuscitation.2005.04.002 pmid: 16081199 |
| 7 |
Kulstad EB, Courtney DM, Waller D. Induction of therapeutic hypothermia via the esophagus: a proof of concept study. World J Emerg Med 2012; 3:118-122.
doi: 10.5847/wjem.j.issn.1920-8642.2012.02.007 pmid: 25215049 |
| 8 |
Post H, Schmitto JD, Steendijk P, Christoph J, Holland R, Wachter R, et al. Cardiac function during mild hypothermia in pigs: increased inotropy at the expense of diastolic dysfunction. Acta Physiol (Oxf) 2010; 199:43-52.
doi: 10.1111/aps.2010.199.issue-1 |
| 9 |
Vijlbrief DC, Benders MJ, Kemperman H, van Bel F, de Vries WB. Cardiac biomarkers as indicators of hemodynamic adaptation during postasphyxial hypothermia treatment. Neonatology 2012; 102:243-248.
doi: 10.1159/000339117 pmid: 22907615 |
| 10 |
Gundersen Y, Vaagenes P, Pharo A, Valø ET, Opstad PK. Moderate hypothermia blunts the inflammatory response and reduces organ injury after acute haemorrhage. Acta Anaesthesiol Scand 2001; 45:994-1001.
doi: 10.1034/j.1399-6576.2001.450812.x pmid: 11576051 |
| 11 |
Westermann S, Vollmar B, Thorlacius H, Menger MD. Surface cooling inhibits tumor necrosis factor-alpha-induced microvascular perfusion failure, leukocyte adhesion, and apoptosis in the striated muscle. Surgery 1999; 126:881-889.
pmid: 10568188 |
| 12 |
Zhang C, Gao GR, Jiang HY, Lv CG, Zhang BL, Xie MS, et al. Effects of environmental hypothermia on hemodynamics and oxygen dynamics in a conscious swine model of hemorrhagic shock. World J Emerg Med 2012; 3:128-134.
doi: 10.5847/wjem.j.issn.1920-8642.2012.02.009 pmid: 25215051 |
| 13 |
Hildebrand F, Giannoudis PV, van Griensven M, Chawda M, Pape HC. Pathophysiologic changes and effects of hypothermia on outcome in elective surgery and trauma patients. Am J Surg 2004; 187:363-371.
doi: 10.1016/j.amjsurg.2003.12.016 pmid: 15006564 |
| 14 |
Peliowski-Davidovich A; Canadian Paediatric Society, Fetus and Newborn Committee. Hypothermia for newborns with hypoxic ischemic encephalopathy. Paediatr Child Health 2012; 17:41-46.
pmid: 23277757 |
| 15 |
Lauriat S, Linas SL. The role of neutrophils in acute renal failure. Semin Nephrol 1998; 18:498-504.
pmid: 9754602 |
| [1] | Xue-jie Dong, Lin Zhang, Yue-lin Yu, Shu-xiao Shi, Xiao-chen Yang, Xiao-qian Zhang, Shuang Tian, Helge Myklebust, Guo-hong Li, Zhi-jie Zheng. The general public’s ability to operate automated external defibrillator: A controlled simulation study [J]. World Journal of Emergency Medicine, 2020, 11(4): 238-245. |
| [2] | Ye-cheng Liu, Yan-meng Qi, Hui Zhang, Joseph Walline, Hua-dong Zhu. A survey of ventilation strategies during cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2019, 10(4): 222-227. |
| [3] | Alexei Birkun, Yekaterina Kosova. Social attitude and willingness to attend cardiopulmonary resuscitation training and perform resuscitation in the Crimea [J]. World Journal of Emergency Medicine, 2018, 9(4): 237-248. |
| [4] | Alexei Birkun, Maksim Glotov, Herman Franklin Ndjamen, Esther Alaiye, Temidara Adeleke, Sergey Samarin. Pre-recorded instructional audio vs. dispatchers’ conversational assistance in telephone cardiopulmonary resuscitation: A randomized controlled simulation study [J]. World Journal of Emergency Medicine, 2018, 9(3): 165-171. |
| [5] | Alexei Birkun, Maksim Glotov. Education in cardiopulmonary resuscitation in Russia: A systematic review of the available evidence [J]. World Journal of Emergency Medicine, 2017, 8(4): 245-252. |
| [6] | Chennappa Kalvatala Krishna, Hakim Irfan Showkat, Meenakshi Taktani, Vikram Khatri. Out of hospital cardiac arrest resuscitation outcome in North India — CARO study [J]. World Journal of Emergency Medicine, 2017, 8(3): 200-205. |
| [7] | Ji Ung Na, Sang Kuk Han, Pil Cho Choi, Dong Hyuk Shin. Effect of metronome rates on the quality of bag-mask ventilation during metronome-guided 30:2 cardiopulmonary resuscitation: A randomized simulation study [J]. World Journal of Emergency Medicine, 2017, 8(2): 136-140. |
| [8] | Gan-nan Wang, Xu-feng Chen, Li Qiao, Yong Mei, Jin-ru Lv, Xi-hua Huang, Bin Shen, Jin-song Zhang. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A meta-analysis of 2 260 patients with cardiac arrest [J]. World Journal of Emergency Medicine, 2017, 8(1): 5-11. |
| [9] | Marion Leary, David G. Buckler, Daniel J. Ikeda, Daiane A. Saraiva, Robert A. Berg, Vinay M. Nadkarni, Audrey L. Blewer, Benjamin S. Abella. The association of layperson characteristics with the quality of simulated cardiopulmonary resuscitation performance [J]. World Journal of Emergency Medicine, 2017, 8(1): 12-18. |
| [10] | Chik Leung Ho, Ka Wai Cheng, Tze Hang Ma, Yau Hang Wong, Ka Lok Cheng, Chak Wah Kam. Characterization of available automated external defibrillators in the market based on the product manuals in 2014 [J]. World Journal of Emergency Medicine, 2016, 7(2): 138-146. |
| [11] | Tomoya Okazaki, Toru Hifumi, Arisa Manabe, Hikari Matsumura, Satoshi Egawa, Hideyuki Hamaya, Nastuyo Shinohara, Koshiro Takano, Hajime Shishido, Yuko Abe, Kenya Kawakita, Masanobu Hagiike, Yasuhiro Kuroda. Invasive group B streptococcal infection in a patient with post splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension [J]. World Journal of Emergency Medicine, 2016, 7(1): 68-70. |
| [12] | Audrey L. Blewer, David G. Buckler, Jiaqi Li, Marion Leary, Lance B. Becker, Judy A. Shea, Peter W. Groeneveld, Mary E. Putt, Benjamin S. Abella. Impact of the 2010 resuscitation guidelines training on layperson chest compressions [J]. World Journal of Emergency Medicine, 2015, 6(4): 270-276. |
| [13] | Jian-ping Gao, Ke-jing Ying. Thrombolysis during extended cardiopulmonary resuscitation for autoimmune-related pulmonary embolism [J]. World Journal of Emergency Medicine, 2015, 6(2): 153-156. |
| [14] | Shou-quan Chen. Advances in clinical studies of cardiopulmonary resuscitation [J]. World Journal of Emergency Medicine, 2015, 6(2): 85-93. |
| [15] | Li Yan, Yi Huang, Shu-sheng Li. Cardiac arrest: a case-based review [J]. World Journal of Emergency Medicine, 2014, 5(3): 171-174. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
